Variants of Callous–Unemotional Traits in Middle Childhood: An Investigation of Emotional Regulation, Externalizing Behaviors, and Psychosocial Risk Factors
Abstract
1. Introduction
1.1. Emotional Regulation Deficits and CU Traits
1.2. Psychosocial Risk Factors and CU Traits
1.3. Comorbid Psychopathology
1.4. Summary
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Emotional Regulation Task
2.4. Measures
2.4.1. Group Formation
- Callous–Unemotional Traits
- Anxiety
2.4.2. Psychosocial Risk Factors
- Prenatal Maternal Stress
- Social Adversity
- Exposure to Childhood Abuse and Domestic Violence
- Parent Criminal Behavior
- Neighborhood Collective Efficacy
2.4.3. Externalizing Behavior Measures
- ADHD/ODD/CD symptoms
- Reactive and Proactive Aggression
- Aggression and Delinquency
- Impulsivity and Narcissism
2.5. Psychophysiological Data Acquisition and Reduction
2.5.1. Respiratory Sinus Arrhythmia (RSA)
2.5.2. Pre-Ejection Period (PEP)
2.6. Statistical Analyses
3. Results
3.1. Emotional Regulation Deficits and CU Variants
3.2. Psychosocial Risk Factors and CU Variants
3.3. Externalizing Behaviors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Frick, P.J.; Stickle, T.R.; Dandreaux, D.M.; Farrell, J.M.; Kimonis, E.R. Callous–unemotional traits in predicting the severity and stability of conduct problems and delinquency. J. Abnorm. Child Psychol. 2005, 33, 471–487. [Google Scholar] [CrossRef] [PubMed]
- Lynam, D.R. Early identification of chronic offenders: Who is the fledgling psychopath? Psychol. Bull. 1996, 120, 209–234. [Google Scholar] [CrossRef] [PubMed]
- Kimonis, E.R. The Emotionally Sensitive Child-Adverse Parenting Experiences-Allostatic (Over)Load (ESCAPE-AL) Model for the Development of Secondary Psychopathic Traits. Clin. Child Fam. Psychol. Rev. 2023, 26, 1097–1114. [Google Scholar] [CrossRef] [PubMed]
- Fanti, K.A.; Kimonis, E. Heterogeneity in externalizing problems at age 3: Association with age 15 biological and environmental outcomes. Dev. Psychol. 2017, 53, 1230. [Google Scholar] [CrossRef]
- Ezpeleta, L.; Granero, R.; de la Osa, N.; Domènech, J.M. Developmental trajectories of callous-unemotional traits, anxiety and oppositionality in 3–7 year-old children in the general population. Personal. Individ. Differ. 2017, 111, 124–133. [Google Scholar] [CrossRef]
- Goulter, N.; Kimonis, E.R.; Hawes, S.W.; Stepp, S.; Hipwell, A.E. Identifying stable variants of callous-unemotional traits: A longitudinal study of at-risk girls. Dev. Psychol. 2017, 53, 2364–2376. [Google Scholar] [CrossRef]
- Payot, M.; Monseur, C.; Stievenart, M.; Brianda, M.E. Callous-Unemotional Traits and Co-occurring Anxiety in Preschool and School-age Children: Investigation of Associations with Family’s Socioeconomic Status and Home Chaos. Res. Child Adolesc. Psychopathol. 2024, 52, 819–831. [Google Scholar] [CrossRef]
- McRae, K.; Gross, J.J. Emotion regulation. Emotion 2020, 20, 1–9. [Google Scholar] [CrossRef]
- Gross, J.J. Emotion regulation: Current status and future prospects. Psychol. Inq. 2015, 26, 1–26. [Google Scholar] [CrossRef]
- Thompson, R.A. Emotion dysregulation: A theme in search of definition. Dev. Psychopathol. 2019, 31, 805–815. [Google Scholar] [CrossRef]
- Cicchetti, D. Socioemotional, Personality, and Biological Development: Illustrations from a Multilevel Developmental Psychopathology Perspective on Child Maltreatment. Annu. Rev. Psychol. 2016, 67, 187–211. [Google Scholar] [CrossRef]
- Craig, S.G.; Moretti, M.M. Profiles of primary and secondary callous-unemotional features in youth: The role of emotion regulation. Dev. Psychopathol. 2019, 31, 1489–1500. [Google Scholar] [CrossRef] [PubMed]
- Wilke, J.; Goagoses, N. Morality in middle childhood: The role of callous-unemotional traits and emotion regulation skills. BMC Psychol. 2023, 11, 283. [Google Scholar] [CrossRef]
- Blair, R.J.R.; Colledge, E.; Mitchell, D.G.V. Somatic markers and response reversal: Is there orbitofrontal cortex dysfunction in boys with psychopathic tendencies? J. Abnorm. Child Psychol. 2001, 29, 499–511. [Google Scholar] [CrossRef]
- Musser, E.D.; Galloway-Long, H.S.; Frick, P.J.; Nigg, J.T. Emotion regulation and heterogeneity in attention-deficit/hyperactivity disorder. J. Am. Acad. Child Adolesc. Psychiatry 2013, 52, 163–171.e2. [Google Scholar] [CrossRef] [PubMed]
- Fanti, K.A.; Kyranides, M.N.; Petridou, M.; Demetriou, C.A.; Georgiou, G. Neurophysiological markers associated with heterogeneity in conduct problems, callous unemotional traits, and anxiety: Comparing children to young adults. Dev. Psychol. 2018, 54, 1634–1649. [Google Scholar] [CrossRef] [PubMed]
- Craig, S.; Goulter, N.; Moretti, M. A systematic review of primary and secondary callous-unemotional traits and psychopathy variants in youth. Clin. Child Fam. Psychol. Rev. 2021, 24, 65–91. [Google Scholar] [CrossRef]
- Cecil, C.A.; Lysenko, L.J.; Jaffee, S.R.; Pingault, J.B.; Smith, R.G.; Relton, C.L.; Woodward, G.; McArdle, W.; Mill, J.; Barker, E.D. Environmental risk, Oxytocin Receptor Gene (OXTR) methylation and youth callous-unemotional traits: A 13-year longitudinal study. Mol. Psychiatry 2014, 19, 1071–1077. [Google Scholar] [CrossRef]
- Payot, M.; Monseur, C.; Stievenart, M. Variants of Callous-unemotional traits in childhood: Investigation of attachment profile and hostile attribution bias. Attach. Hum. Dev. 2023, 25, 566–582. [Google Scholar] [CrossRef]
- van IJzendoorn, M.H.; Bakermans-Kranenburg, M.J.; Coughlan, B.; Reijman, S. Annual Research Review: Umbrella synthesis of meta-analyses on child maltreatment antecedents and interventions: Differential susceptibility perspective on risk and resilience. J. Child. Psychol. Psychiatry 2020, 61, 272–290. [Google Scholar] [CrossRef]
- Humayun, S.; Kahn, R.E.; Frick, P.J.; Viding, E. Callous-unemotional traits and anxiety in a community sample of 7-year-olds. J. Clin. Child Adolesc. Psychol. 2014, 43, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Kimonis, E.R.; Fanti, K.A.; Isoma, Z.; Donoghue, K. Maltreatment profiles among incarcerated boys with callous-unemotional traits. Child Maltreat. 2013, 18, 108–121. [Google Scholar] [CrossRef] [PubMed]
- Cecil, C.A.M.; McCrory, E.J.; Barker, E.D.; Guiney, J.; Viding, E. Characterising youth with callous-unemotional traits and concurrent anxiety: Evidence for a high-risk clinical group. Eur. Child Adolesc. Psychiatry 2018, 27, 885–898. [Google Scholar] [CrossRef]
- Todorov, J.J.; Kohls, G.; Pauli, R.; Rogers, J.; Bernhard, A.; Ackermann, K.; Raschle, N.M.; Dugre, J.R.; Fernandez-Rivas, A.; Gonzalez-Torres, M.A. Maltreatment and parenting in youth with primary and secondary callous-unemotional traits: Anxiety matters. JCPP Adv. 2024, 5, e12266. [Google Scholar] [CrossRef]
- Barker, E.D.; Oliver, B.R.; Viding, E.; Salekin, R.T.; Maughan, B. The impact of prenatal maternal risk, fearless temperament and early parenting on adolescent callous-unemotional traits: A 14-year longitudinal investigation. J. Child Psychol. Psychiatry 2011, 52, 878–888. [Google Scholar] [CrossRef]
- Meehan, A.J.; Maughan, B.; Cecil, C.A.M.; Barker, E.D. Interpersonal callousness and co-occurring anxiety: Developmental validity of an adolescent taxonomy. J. Abnorm. Psychol. 2017, 126, 225–236. [Google Scholar] [CrossRef]
- Gluckman, P.D.; Cutfield, W.; Hofman, P.; Hanson, M.A. The fetal, neonatal, and infant environments-the long-term consequences for disease risk. Early Hum. Dev. 2005, 81, 51–59. [Google Scholar] [CrossRef]
- Euler, F.; Jenkel, N.; Stadler, C.; Schmeck, K.; Fegert, J.M.; Kölch, M.; Schmid, M. Variants of girls and boys with conduct disorder: Anxiety symptoms and callous-unemotional traits. J. Abnorm. Child Psychol. 2015, 43, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Fanti, K.A.; Demetriou, C.A.; Kimonis, E.R. Variants of callous-unemotional conduct problems in a community sample of adolescents. J. Youth Adolesc. 2013, 42, 964–979. [Google Scholar] [CrossRef]
- Kimonis, E.R.; Skeem, J.L.; Cauffman, E.; Dmitrieva, J. Are secondary variants of juvenile psychopathy more reactively violent and less psychosocially mature than primary variants? Law Hum. Behav. 2011, 35, 381–391. [Google Scholar] [CrossRef]
- Gao, Y.; Borlam, D.; Zhang, W. The association between heart rate reactivity and fluid intelligence in children. Biol. Psychol. 2015, 107, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Wechsler, D. Wechsler Intelligence Scale for Children–Fourth Edition (WISC-IV); The Psychological Corporation: San Antonio, TX, USA, 2003. [Google Scholar]
- Musser, E.D.; Backs, R.W.; Schmitt, C.F.; Ablow, J.C.; Measelle, J.R.; Nigg, J.T. Emotion regulation via the autonomic nervous system in children with Attention-Deficit/Hyperactivity Disorder (ADHD). J. Abnorm. Child Psychol. 2011, 39, 841–852. [Google Scholar] [CrossRef]
- Bradley, M.M.; Lang, P.J. Measuring emotion: The self-assessment manikin and the semantic differential. J. Behav. Ther. Exp. Psychiatry 1994, 25, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Frick, P.J. Inventory of Callous-Unemotional Traits: Unpublished Rating Scale; University of New Orleans: New Orleans, LA, USA, 2004. [Google Scholar]
- Frick, P.J.; Hare, R.D. Antisocial Process Screening Device (APSD): Technical Manual; Multi-Health Systems: Tonawanda, NY, USA, 2001. [Google Scholar]
- Gao, Y.; Zhang, W. Confirmatory factor analyses of self-and parent-report inventory of callous-unemotional traits in 8- to 10-year-olds. J. Psychopathol. Behav. Assess. 2016, 38, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.M. Manual for the Child Behavior Checklist/4-18 and 1991 Profile; University of Vermont Department of Psychiatry: Burlington, VT, USA, 1991. [Google Scholar]
- Achenbach, T.M.; Dumenci, L.; Rescorla, L.A. DSM-oriented and empirically based approaches to constructing scales from the same item pools. J. Clin. Child Adolesc. Psychol. 2003, 32, 328–340. [Google Scholar] [CrossRef]
- Price, M.; Higa-McMillan, C.; Ebesutani, C.; Okamura, K.; Nakamura, B.J.; Chorpita, B.F.; Weisz, J. Symptom differentiation of anxiety and depression across youth development and clinic-referred/nonreferred samples: An examination of competing factor structures of the Child Behavior Checklist DSM-oriented scales. Dev. Psychopathol. 2013, 25 Pt 1, 1005–1015. [Google Scholar] [CrossRef]
- Sharf, A.; Kimonis, E.R.; Howard, A. Negative life events and posttraumatic stress disorder among incarcerated boys with callous-unemotional traits. J. Psychopathol. Behav. Assess. 2014, 36, 401–414. [Google Scholar] [CrossRef]
- Gao, Y.; Raine, A.; Venables, P.H.; Dawson, M.E.; Mednick, S.A. Association of poor childhood fear conditioning and adult crime. Am. J. Psychiatry 2010, 167, 56–60. [Google Scholar] [CrossRef]
- Raine, A.; Yaralian, P.S.; Reynolds, C.; Venables, P.H.; Mednick, S.A. Spatial but not verbal cognitive deficits at age 3 years in persistently antisocial individuals. Dev. Psychopathol. 2002, 14, 25–44. [Google Scholar] [CrossRef]
- Straus, M.A. Measuring intrafamilial conflict and violence: The Conflict Tactics Scale (CTS). J. Marriage Fam. 1979, 4, 75–86. [Google Scholar] [CrossRef]
- Widom, C.S.; Shepard, R.L. Accuracy of adult recollections of childhood victimization: Part 1, Childhood physical abuse. Psychol. Assess. 1996, 8, 412–420. [Google Scholar] [CrossRef]
- Straus, M.A.; Gelles, R.J. Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8145 Families; Transaction: New Brunswick, NJ, USA, 1990. [Google Scholar]
- Raine, A.; Yang, Y.; Narr, K.L.; Toga, A.W. Sex differences in orbitofrontal gray as a partial explanation for sex differences in antisocial personality. Mol. Psychiatry 2011, 16, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Sampson, R.J.; Raudenbush, S.W.; Earls, F. Neighbourhoods and violent crime: A multilevel study of collective efficacy. Science 1997, 277, 918–924. [Google Scholar] [CrossRef]
- Kofler, L.; Zhang, W.; Gao, Y. Psychopathic Traits and Conduct Problems in Children: Effects of Collective Efficacy, Heart Rate, and Sex. J. Psychopathol. Behav. Assess. 2022, 44, 98–114. [Google Scholar] [CrossRef]
- Shaffer, D.; Fisher, P.; Lucas, C.P.; Dulcan, M.K.; Schwab-Stone, M.E. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 28–38. [Google Scholar] [CrossRef]
- Shaffer, D.; Scott, M.; Wilcox, H.; Maslow, C.; Hicks, R.; Lucas, C.P.; Garfinkel, R.; Greenwald, S. The Columbia Suicide Screen: Validity and reliability of a screen for youth suicide and depression. J. Am. Acad. Child Adolesc. Psychiatry 2004, 43, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Raine, A.; Dodge, K.; Loeber, R.; Gatzke-Kopp, L.; Lynam, D.R.; Reynolds, C.; Stouthamer-Loeber, M.; Liu, J. The reactive-proactive aggression questionnaire: Differential correlates of reactive and proactive aggression in adolescent boys. Aggress. Behav. 2006, 32, 159–171. [Google Scholar] [CrossRef]
- Achenbach, T.M. Manual for the Youth Self-Report and 1991 Profile; University of Vermont Department of Psychiatry: Burlington, VT, USA, 1991. [Google Scholar]
- Vitacco, M.J.; Rogers, R.; Neumann, C.S. The antisocial process screening device: An examination of its construct and criterion-related validity. Assessment 2003, 10, 143–150. [Google Scholar] [CrossRef]
- Grossman, P.; Van Beek, J.; Wientjes, C. A comparison of three quantification methods for estimation of respiratory sinus arrhythmia. Psychophysiology 1990, 27, 702–714. [Google Scholar] [CrossRef]
- Sherwood, A.; Allen, M.T.; Fahrenberg, J.; Kelsey, R.M.; Lovallo, W.R.; Van Doornen, L.J. Methodological guidelines for impedance cardiography. Psychophysiology 1990, 27, 1–23. [Google Scholar]
- Beauchaine, T. Vagal tone, development, and Gray’s motivational theory: Toward an integrated model of autonomic nervous system functioning in psychopathology. Dev. Psychopathol. 2001, 13, 183–214. [Google Scholar] [CrossRef] [PubMed]
- Beauchaine, T.P.; Thayer, J.F. Heart rate variability as a transdiagnostic biomarker of psychopathology. Int. J. Psychophysiol. 2015, 98, 338–350. [Google Scholar] [CrossRef]
- Porges, S.W. The polyvagal perspective. Biol. Psychol. 2007, 74, 116–143. [Google Scholar] [CrossRef]
- Utendale, W.T.; Nuselovici, J.; Saint-Pierre, A.B.; Hubert, M.; Chochol, C.; Hastings, P.D. Associations between inhibitory control, respiratory sinus arrhythmia, and externalizing problems in early childhood. Dev. Psychobiol. 2014, 56, 686–699. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Gao, Y. Interactive effects of social adversity and respiratory sinus arrhythmia activity on reactive and proactive aggression. Psychophysiology 2015, 52, 1343–1350. [Google Scholar] [CrossRef] [PubMed]
- Thomson, N.D.; Aboutanos, M.; Kiehl, K.A.; Neumann, C.; Galusha, C.; Fanti, K.A. Physiological reactivity in response to a fear-induced virtual reality experience: Associations with psychopathic traits. Psychophysiology 2019, 56, e13276. [Google Scholar] [CrossRef]
- Hinnant, J.B.; El-Sheikh, M. Children’s externalizing and internalizing symptoms over time: The role of individual differences in patterns of RSA responding. J. Abnorm. Child Psychol. 2009, 37, 1049–1061. [Google Scholar] [CrossRef]
- Wagner, N.J.; Hastings, P.D.; Rubin, K.H. Callous-Unemotional Traits and Autonomic Functioning in Toddlerhood Interact to Predict Externalizing Behaviors in Preschool. J. Abnorm. Child Psychol. 2018, 46, 1439–1450. [Google Scholar] [CrossRef]
- Wagner, N.J.; Waller, R. Leveraging parasympathetic nervous system activity to study risk for psychopathology: The special case of callous-unemotional traits. Neurosci. Biobehav. Rev. 2020, 118, 175–185. [Google Scholar] [CrossRef]
- Conradt, E.; Degarmo, D.; Fisher, P.; Abar, B.; Lester, B.M.; Lagasse, L.L.; Shankaran, S.; Bada, H.; Bauer, C.R.; Whitaker, T.M.; et al. The contributions of early adverse experiences and trajectories of respiratory sinus arrhythmia on the development of neurobehavioral disinhibition among children with prenatal substance exposure. Dev. Psychopathol. 2014, 26 Pt 1, 901–916. [Google Scholar] [CrossRef]
- Gordis, E.B.; Feres, N.; Olezeski, C.L.; Rabkin, A.N.; Trickett, P.K. Skin conductance reactivity and respiratory sinus arrhythmia among maltreated and comparison youth: Relations with aggressive behavior. J. Pediatr. Psychol. 2010, 35, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Katz, L.F. Domestic violence and vegal reactivity to peer provocation. Biol. Psychol. 2007, 74, 154–164. [Google Scholar] [CrossRef] [PubMed]
- Cardinale, E.M.; Marsh, A.A. The Reliability and Validity of the Inventory of Callous Unemotional Traits: A Meta-Analytic Review. Assessment 2020, 27, 57–71. [Google Scholar] [CrossRef]
- Salekin, R.T.; Andershed, H.; Colins, O.F. Introduction to the special section: What do we know about the psychophysiology of child psychopathy and conduct problems? J. Psychopathol. Behav. Assess. 2022, 44, 1–10. [Google Scholar] [CrossRef]
- Brooker, R.J.; Buss, K.A. Dynamic measures of RSA predict distress and regulation in toddlers. Dev. Psychobiol. 2010, 52, 372–382. [Google Scholar] [CrossRef]
- Kahn, R.E.; Frick, P.J.; Youngstrom, E.A.; Kogos Youngstrom, J.; Feeny, N.C.; Findling, R.L. Distinguishing primary and secondary variants of callous-unemotional traits among adolescents in a clinic-referred sample. Psychol. Assess. 2013, 25, 966. [Google Scholar] [CrossRef]
- Barker, E.D.; Salekin, R.T. Irritable oppositional defiance and callous unemotional traits: Is the association partially explained by peer victimization? J. Child Psychol. Psychiatry 2012, 53, 1167–1175. [Google Scholar] [CrossRef]
| Low CU | High CU | F Χ2 | Pairwise Comparisons (w/Bonferroni Correction) | |||
|---|---|---|---|---|---|---|
| Low Anxiety (Control; “C”, n = 54) | High Anxiety (Anxious; “A”, n = 51) | Low Anxiety/Primary (“P”, n = 44) | High Anxiety/Secondary (“S”, n = 63) | |||
| Male (%) | 42.6 | 39.2 | 56.8 | 41.3 | Χ2= 3.63, p = 0.310 | - |
| Age | 9.18 (0.68) | 8.98 (0.58) | 9.05 (0.60) | 9.07 (0.62) | F (3, 208) = 0.93, p = 0.43, η2 = 0.007 | - |
| IQ | 108.26 (19.07) | 107.20 (19.10) | 98.41 (22.20) | 91.92 (18.66) | F (3, 208) = 8.89, p < 0.001, η2 = 0.11 | A, C > S |
| Prenatal and Postnatal Adversity | ||||||
| Prenatal Maternal Stress | 0.37 (0.73) | 0.60 (0.78) | 0.79 (0.97) | 1.14 (1.34) | F (3, 200) = 5.90, p < 0.001. η2 = 0.08 | S > A, C |
| Social Adversity | 2.61 (1.88) | 3.33 (2.22) | 3.23 (1.94) | 3.32 (2.05) | F (3, 207) = 1.57, p = 0.200, η2 = 0.05 | - |
| Parent White-Collar Crime | 8.50 (5.83) | 8.90 (5.11) | 8.82 (6.31) | 7.94 (6.77) | F (3, 199) = 0.27, p = 0.840, η2 = 0.004 | - |
| Other Parental Crime | 4.05 (4.65) | 5.67 (5.07) | 4.87 (6.26) | 7.13 (7.59) | F (3, 200) = 2.61, p = 0.050, η2 = 0.04 | S > C |
| Neighborhood Collective Efficacy | 34.15 (6.96) | 29.74 (9.14) | 30.55 (8.91) | 27.50 (9.17) | F (3, 150) = 4.37, p = 0.006, η2 = 0.08 | C > S |
| Domestic Violence (Physical) | 0.43 (1.87) | 1.21 (3.31) | 1.88 (5.50) | 3.81 (8.78) | F (3, 191) = 3.55, p = 0.016, η2 = 0.05 | S > C |
| Domestic Violence (Verbal) | 4.57 (5.65) | 5.81 (5.35) | 8.05 (6.73) | 10.90 (6.94) | F (3, 191) = 10.53, p < 0.001, η2 = 0.14 | S > A, C; P > C |
| Childhood Abuse (Physical) | 1.57 (2.47) | 2.45 (2.60) | 3.35 (3.36) | 4.17 (5.40) | F (3, 204) = 5.01, p = 0.002, η2 = 0.12 | S > C |
| Childhood Abuse (Verbal) | 2.69 (3.06) | 5.02 (4.60) | 4.88 (4.48) | 7.33 (5.09) | F (3, 204) = 10.67, p < 0.001, η2 = 0.25 | S > A, P > C |
| Externalizing Behaviors | ||||||
| Aggression (Parent Report) | 1.33 (1.88) | 3.59 (3.75) | 5.84 (4.96) | 8.56 (6.06) | F (3, 208) = 27.14, p < 0.001, η2 = 0.34 | S > P > C; S > A |
| Aggression (Child Report) | 5.00 (3.33) | 8.63 (4.31) | 7.11 (3.53) | 10.08 (5.03) | F (3, 208) = 15.45, p < 0.001, η2 = 0.31 | S, A >C; S > P |
| Delinquency (Parent Report) | 0.69 (1.08) | 1.20 (1.31) | 2.50 (1.85) | 3.86 (3.66) | F (3, 208) = 21.62, p < 0.001, η2 = 0.37 | S > P > A, C |
| Delinquency (Child Report) | 2.65 (1.42) | 3.31 (2.01) | 2.82 (1.87) | 4.29 (2.66) | F (3, 208) = 7.27, p < 0.001, η2 = 0.14 | S > C, P |
| Proactive Aggression | 0.53 (1.05) | 1.08 (2.31) | 1.94 (3.56) | 2.63 (3.62) | F (3, 204) = 5.97, p < 0.001, η2 = 0.11 | S > A, C |
| Reactive Aggression | 4.05 (3.35) | 6.38 (3.40) | 6.18 (4.82) | 7.22 (4.47) | F (3, 304) = 6.17, p < 0.001, η2 = 0.14 | S, A > C |
| ADHD Symptoms | 2.80 (3.06) | 5.04 (3.82) | 6.95 (4.64) | 8.52 (6.07) | F (3, 203) = 16.03, p < 0.001, η2 = 0.28 | S, P > C; S > A |
| ODD Symptoms | 2.59 (2.54) | 2.69 (2.57) | 3.93 (2.98) | 5.18 (3.43) | F (3, 203) = 9.84, p < 0.001, η2 = 0.19 | S > A, C |
| CD Symptoms | 0.30 (0.69) | 0.43 (0.96) | 1.17 (1.71) | 1.13 (1.52) | F (3, 203) = 6.67, p < 0.001, η2 = 0.13 | S, P > A, C |
| Narcissism (Parent Report) | 0.69 (0.85) | 1.28 (1.11) | 2.30 (1.97) | 3.10 (2.51) | F (3, 203) = 19.92, p < 0.001, η2 = 0.34 | S, P > A, C |
| Narcissism (Child Report) | 1.20 (1.47) | 2.08 (1.76) | 2.30 (2.08) | 3.62 (2.94) | F (3, 201) = 11.78, p < 0.001, η2 = 0.20 | S > P, A, C |
| Impulsivity (Parent Report) | 1.48 (1.13) | 1.90 (1.36) | 2.89 (1.81) | 3.64 (1.89) | F (3, 203) = 20.93, p < 0.001, η2 = 0.26 | S, P > A, C |
| Impulsivity (Child Report) | 1.49 (1.45) | 2.34 (1.44) | 2.52 (1.72) | 3.12 (1.94) | F (3, 201) = 8.92, p < 0.001, η2 = 0.19 | S, P > C |
| Low CU | High CU | F | Pairwise Comparisons | |||
|---|---|---|---|---|---|---|
| Low Anxiety (Control; “C”, n = 34–46) | High Anxiety (Anxious; “A”; n = 35–46) | Low Anxiety/Primary (“P”; n = 22–36) | High Anxiety/Secondary (“S”; n = 38–53) | |||
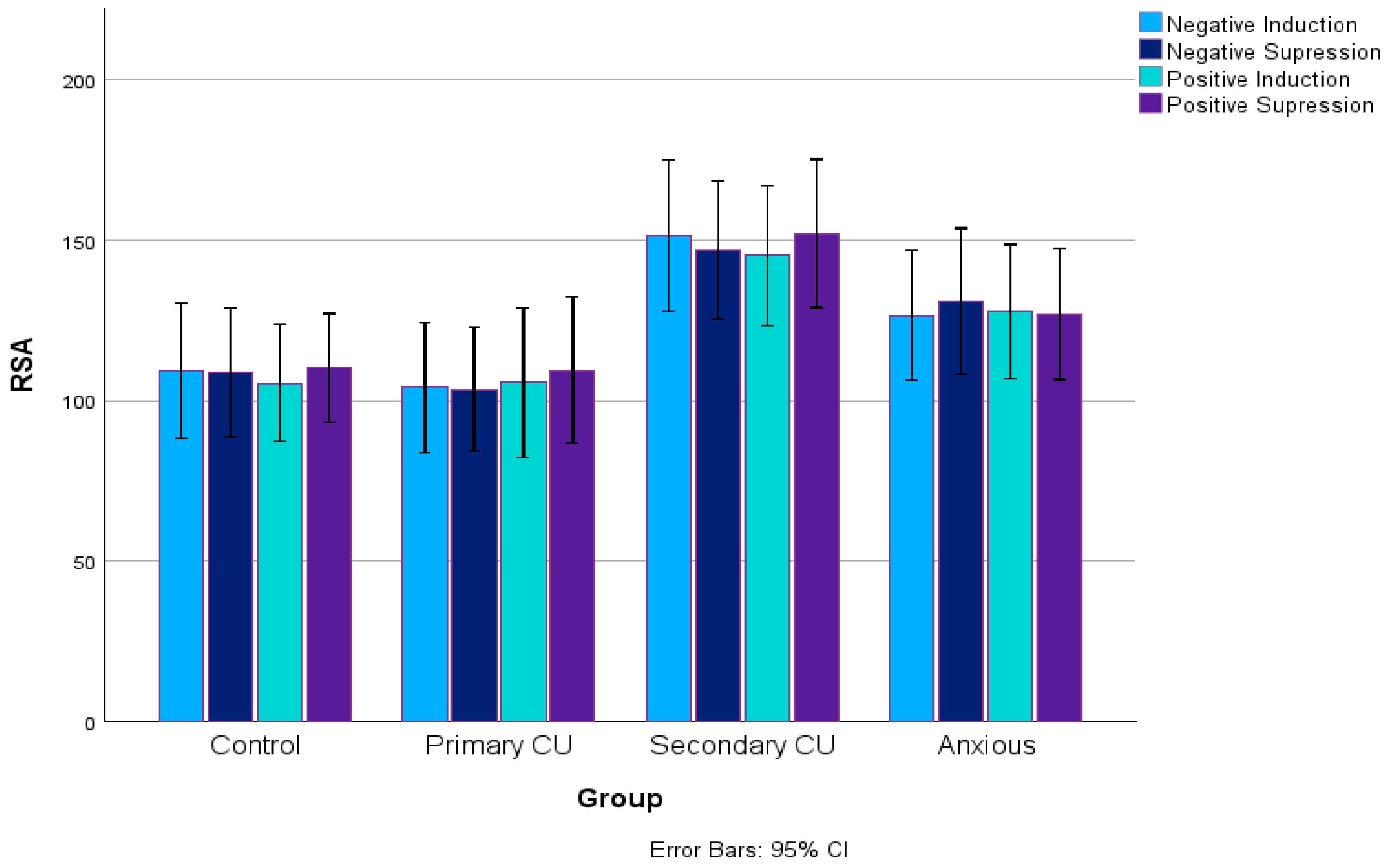
| RSA (Negative Induction) | 109.15 (58.27) | 121.64 (55.05) | 104.17 (45.84) | 145.51 (67.31) | F (3, 125) = 3.28, p = 0.023, η2 = 0.07 | LSD: S > C, P |
| RSA (Negative Suppression) | 108.87 (55.93) | 127.13 (60.17) | 108.87 (49.64) | 144.79 (61.54) | F (3, 124) = 2.89, p = 0.038, η2 = 0.07 | LSD: S > C, P |
| RSA (Positive Induction) | 109.82 (56.71) | 126.79 (56.77) | 110.85 (57.26) | 143.61 (62.41) | F (3, 124) = 2.43, p = 0.069, η2 = 0.06 | - |
| RSA (Positive Suppression) | 113.13 (50.72) | 123.12 (53.31) | 113.96 (54.81) | 146.25 (66.57) | F (3, 128) = 2.52, p = 0.061, η2 = 0.06 | - |
| PEP (Negative Induction) | 77.96 (19.24) | 88.41 (19.76) | 80.50 (22.72) | 83.33 (22.7) | F (3, 175) = 2.04, p = 0.110, η2 = 0.03 | - |
| PEP (Negative Suppression) | 81.44 (20.12) | 88.57 (18.84) | 83.75 (15.7) | 85.21 (24.21) | F (3, 175) = 0.89, p = 0.450, η2 = 0.02 | - |
| PEP (Positive Induction) | 78.38 (19.12) | 90.32 (20.77) | 84.15 (21.79) | 88.08 (21.79) | F (3, 175) = 2.41, p = 0.069, η2 = 0.04 | - |
| PEP (Positive Suppression) | 81.55 (19.00) | 89.16 (19.66) | 83.21 (24.13) | 87.62 (23.44) | F (3, 171) = 1.21, p = 0.309, η2 = 0.07 | - |
| Valence (Negative Induction) | 2.15 (0.97) | 2.10 (0.97) | 2.02 (1.05) | 2.02 (1.09) | F (3, 206) = 0.22, p = 0.870, η2 = 0.003 | - |
| Valence (Negative Suppression) | 2.25 (1.07) | 2.16 (1.06) | 2.64 (1.14) | 1.98 (1.11) | F (3, 206) = 3.14, p = 0.026, η2 = 0.04 | LSD: S, A < P Bonferroni: S < P |
| Valence (Positive Induction) | 4.34 (0.90) | 4.43 (0.82) | 4.23 (0.91) | 4.44 (0.93) | F (3, 205) = 0.61, p = 0.608, η2 = 0.01 | - |
| Valence (Positive Suppression) | 4.65 (0.56) | 4.65 (0.86) | 4.43 (0.85) | 4.56 (0.98) | F (3, 204) = 0.75, p = 0.526, η2 = 0.01 | - |
| Arousal (Negative Induction) | 1.94 (1.06) | 2.16 (1.85) | 2.50 (1.40) | 2.21 (1.44) | F (3, 206) = 1.18, p = 0.318, η2 = 0.02 | - |
| Arousal (Negative Suppression) | 2.47 (1.31) | 2.68 (1.22) | 2.86 (1.34) | 2.49 (1.39) | F (3, 206) = 0.95, p = 0.418, η2 = 0.01 | - |
| Arousal (Positive Induction) | 2.34 (1.41) | 2.14 (1.37) | 2.20 (1.42) | 2.41 (1.59) | F (3, 205) = 0.38, p = 0.765 η2 = 0.01 | - |
| Arousal (Positive Suppression) | 2.17 (1.32) | 2.12 (1.35) | 2.43 (1.56) | 2.11 (1.35) | F (3, 204) = 0.55, p = 0.648 η2 = 0.01 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gao, Y.; Guariguata, I.; Kofler, L. Variants of Callous–Unemotional Traits in Middle Childhood: An Investigation of Emotional Regulation, Externalizing Behaviors, and Psychosocial Risk Factors. Children 2025, 12, 835. https://doi.org/10.3390/children12070835
Gao Y, Guariguata I, Kofler L. Variants of Callous–Unemotional Traits in Middle Childhood: An Investigation of Emotional Regulation, Externalizing Behaviors, and Psychosocial Risk Factors. Children. 2025; 12(7):835. https://doi.org/10.3390/children12070835
Chicago/Turabian StyleGao, Yu, Ines Guariguata, and Liat Kofler. 2025. "Variants of Callous–Unemotional Traits in Middle Childhood: An Investigation of Emotional Regulation, Externalizing Behaviors, and Psychosocial Risk Factors" Children 12, no. 7: 835. https://doi.org/10.3390/children12070835
APA StyleGao, Y., Guariguata, I., & Kofler, L. (2025). Variants of Callous–Unemotional Traits in Middle Childhood: An Investigation of Emotional Regulation, Externalizing Behaviors, and Psychosocial Risk Factors. Children, 12(7), 835. https://doi.org/10.3390/children12070835






