Gross Motor Performance, Participation and Quality of Life After Adapted Physical Activity Interventions in Pediatric Populations with Neuromotor Disability: A Systematic Review
Abstract
1. Introduction
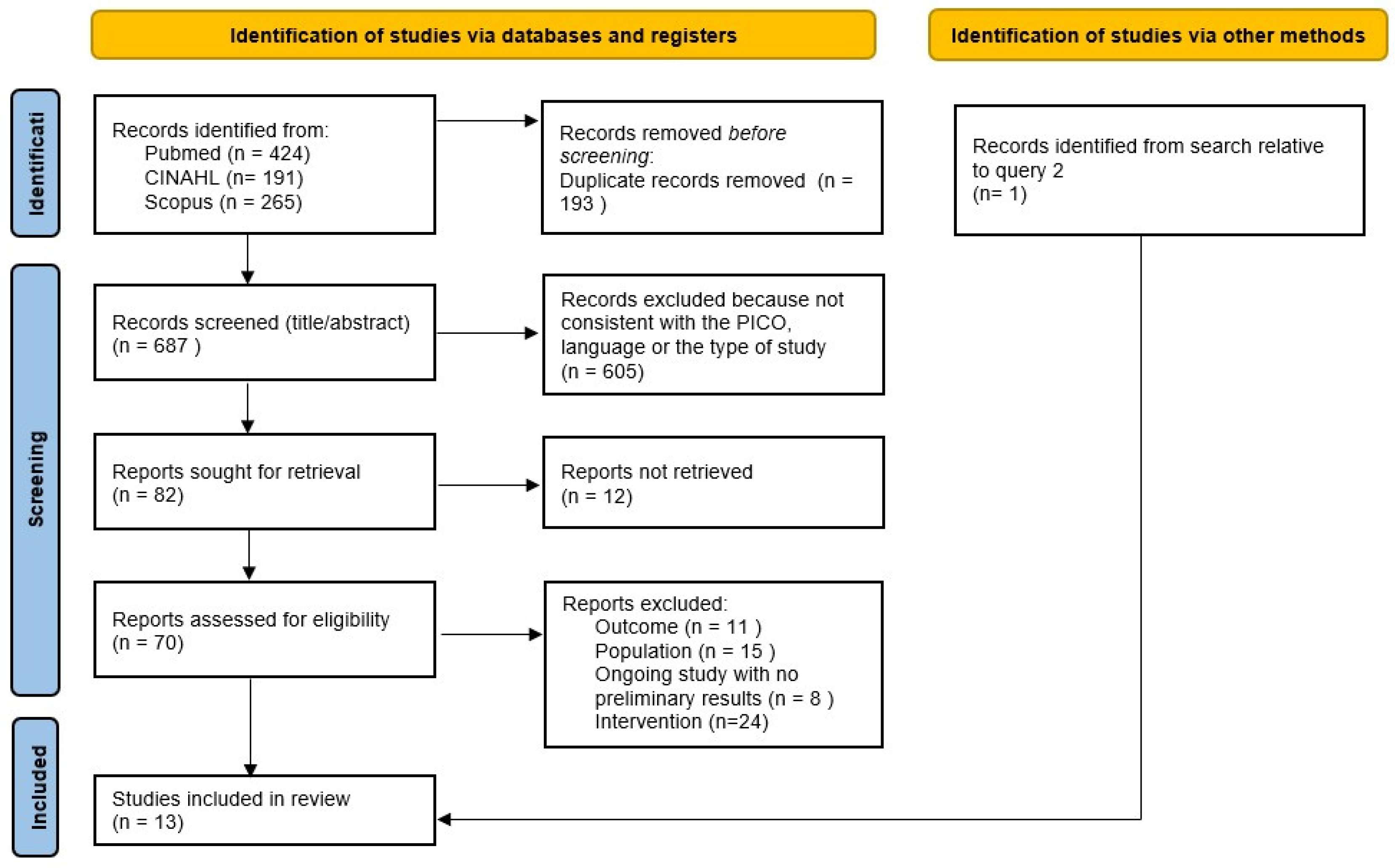
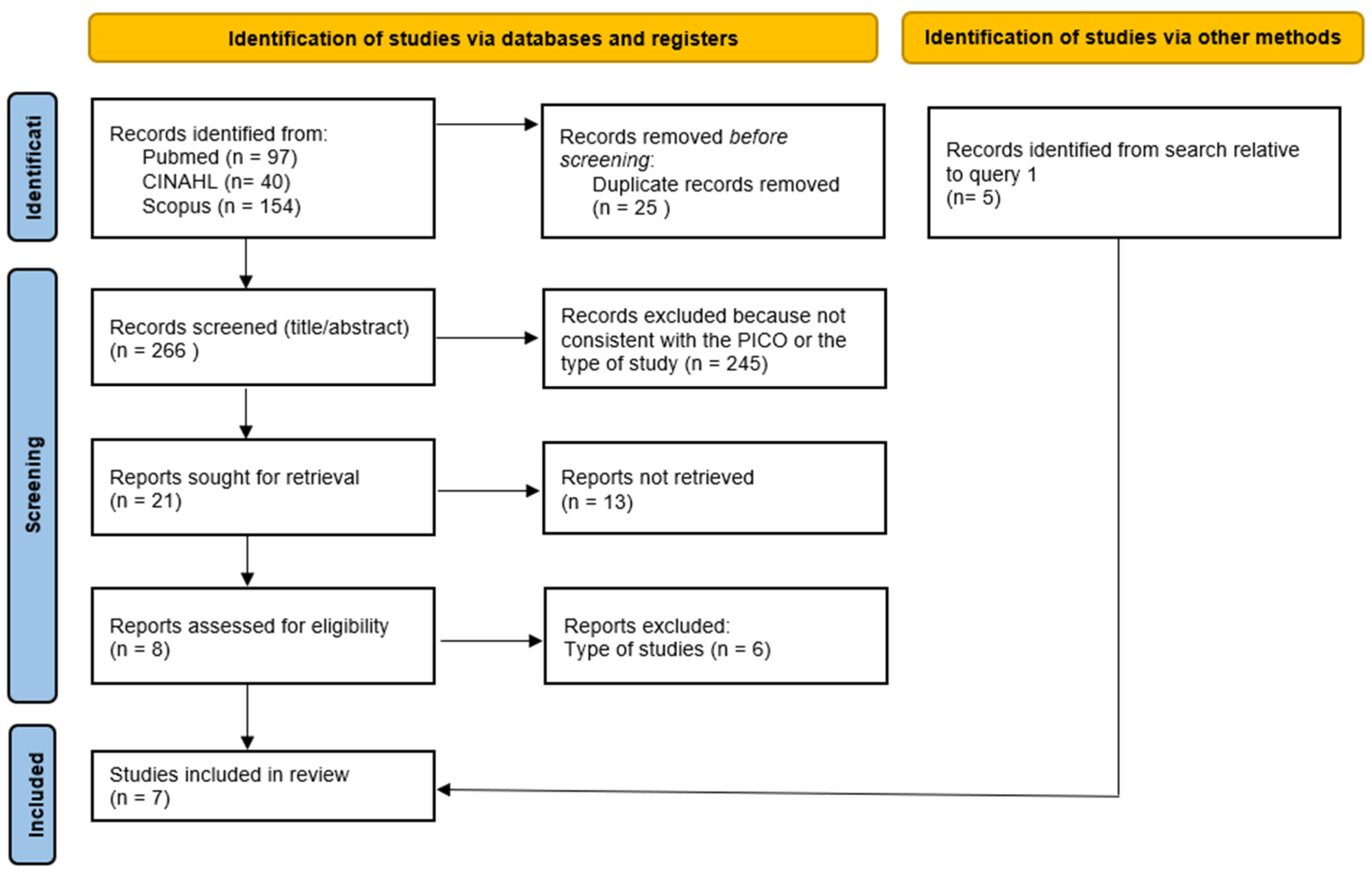
2. Materials and Methods
- P: patients aged 2–18 with cerebral palsy, developmental disabilities, acquired nervous system injury, hereditary spastic paraplegias, pediatric movement disorders or ataxias, any neurometabolic or neuromuscular diseases, congenital, hereditary diseases and abnormalities.
- I: adapted physical activity.
- C: conventional therapy or no treatment.
- O: change in gross motor function, walking, postural control, postural balance, muscle strength, cardiorespiratory and muscular endurance.
- P: patients aged 2–18 with cerebral palsy, developmental disabilities, acquired nervous system injury, hereditary spastic paraplegias, pediatric movement disorders or ataxias, any neurometabolic or neuromuscular diseases, congenital, hereditary diseases and abnormalities.
- I: adapted physical activity.
- C: conventional therapy or no treatment.
- O: change in quality of life and participation.
3. Results
3.1. Quality of Studies and Risk of Bias
3.2. Interventions Relative to Query 1
3.3. Interventions Relative to Query 2
3.4. Outcome Measures
3.5. Side Effects
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Physical Activity. Available online: https://www.who.int/europe/news-room/fact-sheets/item/physical-activity (accessed on 23 April 2025).
- Rimmer, J.H.; Rowland, J.L.; Yamaki, K. Obesity and secondary conditions in adolescents with disabilities: Addressing the needs of an underserved population. J. Adolesc. Health 2007, 41, 224–229. [Google Scholar] [CrossRef]
- Carbone, P.S.; Smith, P.J.; Lewis, C.; LeBlanc, C. Promoting the Participation of Children and Adolescents with Disabilities in Sports, Recreation, and Physical Activity. Pediatrics 2021, 148, e2021054664. [Google Scholar] [CrossRef]
- Rowland, J.L.; Fragala-Pinkham, M.; Miles, C.; O’Neil, M.E. The scope of pediatric physical therapy practice in health promotion and fitness for youth with disabilities. Pediatr. Phys. Ther. 2015, 27, 2–15. [Google Scholar] [CrossRef] [PubMed]
- Tasiemski, T.; Kennedy, P.; Gardner, B.P.; Blaikley, R.A. Athletic Identity and Sports Participation in People with Spinal Cord Injury. Adapt. Phys. Act. Q. 2004, 21, 364–378. [Google Scholar] [CrossRef]
- Willis, C.E.; Reid, S.; Elliott, C.; Rosenberg, M.; Nyquist, A.; Jahnsen, R.; Girdler, S. A realist evaluation of a physical activity participation intervention for children and youth with disabilities: What works, for whom, in what circumstances, and how? BMC Pediatr. 2018, 18, 113. [Google Scholar] [CrossRef] [PubMed]
- Hutzler, Y.; Sherrill, C. Defining adapted physical activity: International perspectives. Adapt. Phys. Act. Q. 2007, 24, 1–20. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning Disability Health: ICF; World Health Organization: Geneva, Switzerland, 2001; Available online: https://iris.who.int/handle/10665/42407 (accessed on 31 May 2025).
- Winter, E.M.; Fowler, N. Exercise defined and quantified according to the Systeme International d’Unites. J. Sports Sci. 2009, 27, 447–460. [Google Scholar] [CrossRef]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar]
- McArdle, W.D.; Katch, F.I.; Katch, V.L. Exercise Physiology: Energy, Nutrition and Human Performance, 6th ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2007. [Google Scholar]
- Morgan, P.; Cleary, S.; Dutia, I.; Bow, K.; Shields, N. Community-based physical activity interventions for adolescents and adults with complex cerebral palsy: A scoping review. Dev. Med. Child Neurol. 2023, 65, 1451–1463. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Munn, Z.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Tufanaru, C.; Qureshi, R.; Mattis, P.; Mu, P. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute’s approach. Int. J. Evid. Based Healthc. 2015, 13, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Schranz, C.; Kruse, A.; Belohlavek, T.; Steinwender, G.; Tilp, M.; Pieber, T.; Svehlik, M. Does Home-Based Progressive Resistance or High-Intensity Circuit Training Improve Strength, Function, Activity or Participation in Children with Cerebral Palsy? Arch. Phys. Med. Rehabil. 2018, 99, 2457–2464.e4. [Google Scholar] [CrossRef]
- Declerck, M.; Verheul, M.; Daly, D.; Sanders, R. Benefits and Enjoyment of a Swimming Intervention for Youth with Cerebral Palsy: An RCT Study. Pediatr. Phys. Ther. 2016, 28, 162–169. [Google Scholar] [CrossRef]
- Böhm, H.; Rammelmayr, M.K.; Döderlein, L. Effects of climbing therapy on gait function in children and adolescents with cerebral palsy—A randomized, controlled crossover trial. Eur. J. Physiother. 2015, 17, 1–8. [Google Scholar] [CrossRef]
- Coman, C.; Meldrum, D.; Kiernan, D.; Malone, A. Pilates-based exercises for gait and balance in ambulant children with cerebral palsy: Feasibility and clinical outcomes of a randomised controlled trial. Disabil. Rehabil. 2023, 45, 2796–2807. [Google Scholar] [CrossRef]
- Toovey, R.A.M.; Harvey, A.R.; McGinley, J.L.; Lee, K.J.; Shih, S.T.F.; Spittle, A.J. Task-specific training for bicycle-riding goals in ambulant children with cerebral palsy: A randomized controlled trial. Dev. Med. Child Neurol. 2022, 64, 243–252. [Google Scholar] [CrossRef] [PubMed]
- Clutterbuck, G.L.; Auld, M.L.; Johnston, L.M. SPORTS STARS: A practitioner-led, peer-group sports intervention for ambulant children with cerebral palsy. Activity and participation outcomes of a randomised controlled trial. Disabil. Rehabil. 2022, 44, 948–956. [Google Scholar] [CrossRef]
- Elnaggar, R.K.; Alghadier, M.; Abdrabo, M.S.; Abonour, A.A. Effect of a structured aqua-plyometric exercise program on postural control and functional ability in children with hemiparetic cerebral palsy: A two-arm randomized controlled trial. NeuroRehabilitation 2022, 51, 247–258. [Google Scholar] [CrossRef]
- Hanssen, B.; Peeters, N.; De Beukelaer, N.; Vannerom, A.; Peeters, L.; Molenaers, G.; van Campenhout, A.; Deschepper, E.; Broeck, C.V.D.; Desloovere, K. Progressive resistance training for children with cerebral palsy: A randomized controlled trial evaluating the effects on muscle strength and morphology. Front. Physiol. 2022, 13, 911162. [Google Scholar] [CrossRef] [PubMed]
- Scholtes, V.A.; Becher, J.G.; Comuth, A.; Dekkers, H.; Van Dijk, L.; Dallmeijer, A.J. Effectiveness of functional progressive resistance exercise strength training on muscle strength and mobility in children with cerebral palsy: A randomized controlled trial. Dev. Med. Child Neurol. 2010, 52, e107–e113. [Google Scholar] [CrossRef]
- Raghupathy, M.K.; Divya, M.; Karthikbabu, S. Effects of Traditional Indian Dance on Motor Skills and Balance in Children with Down syndrome. J. Mot. Behav. 2022, 54, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Gibson, N.; Chappell, A.; Blackmore, A.M.; Morris, S.; Williams, G.; Bear, N.; Allison, G. The effect of a running intervention on running ability and participation in children with cerebral palsy: A randomized controlled trial. Disabil. Rehabil. 2018, 40, 3041–3049. [Google Scholar] [CrossRef]
- Lee, H.K.; Jin, J. Combined Virtual-Reality- and Gym-Based Physical Activity Intervention for Children with a Developmental Disability: Effects on Physical Activity Levels, Motor Skills, and Social Skills. Adapt. Phys. Act. Q. 2024, 41, 513–533. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Huang, P.; Su, M.; Liu, Z.; Liu, Q.; Guo, Y.; Zheng, L. Impact of remote collaboration-based family physical activity on activity levels and quality of life in children with intellectual developmental disabilities. Front. Public Health 2024, 12, 1464099. [Google Scholar] [CrossRef]
- Desmuth, S.K.; Knutson, L.M.; Fowler, E.G. The PEDALS stationary cycling intervention and health-related quality of life in children with cerebral palsy: A randomized controlled trial. Dev. Med. Child Neurol. 2012, 54, 654–661. [Google Scholar] [CrossRef]
- Vitrikas, K.; Dalton, H.; Breish, D. Cerebral Palsy: An Overview. Am. Fam. Physician 2020, 101, 213–220. [Google Scholar]
- McIntyre, S.; Goldsmith, S.; Webb, A.; Ehlinger, V.; Hollung, S.J.; McConnell, K.; Arnaud, C.; Smithers-Sheedy, H.; Oskoui, M.; Khandaker, G.; et al. Global prevalence of cerebral palsy: A systematic analysis. Dev. Med. Child Neurol. 2022, 64, 1494–1506. [Google Scholar] [CrossRef]
- Ryan, J.M.; Cassidy, E.E.; Noorduyn, S.G.; O’Connell, N.E. Exercise interventions for cerebral palsy. Cochrane Database Syst. Rev. 2017, 6, CD011660. [Google Scholar] [CrossRef]
- Faccioli, S.; Sassi, S.; Pagliano, E.; Maghini, C.; Perazza, S.; Siani, M.F.; Sgherri, G.; Farella, G.M.; Foscan, M.; Viganò, M.; et al. Care Pathways in Rehabilitation for Children and Adolescents with Cerebral Palsy: Distinctiveness of the Adaptation to the Italian Context. Children 2024, 11, 852. [Google Scholar] [CrossRef] [PubMed]
- NICE Guidelines: Managing Cerebral Palsy in Under 25s. 2021. Available online: http://pathways.nice.org.uk/pathways/cerebral-palsy (accessed on 31 May 2025).
- NICE Guidelines: Spasticity in Under 19s: Management. 2012–2016. Available online: https://www.nice.org.uk/guidance/cg145 (accessed on 31 May 2025).
- Management of Cerebral Palsy in Children: A Guide for Allied Health Professionals. 2018. Available online: http://www.health.nsw.gov.au/kidsfamilies/ (accessed on 31 May 2025).
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour at a Glance; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
| Reference Study Design Overall RoB | Sample # | Intervention Group (IG) | Control Group (CG) | Assessment | Outcomes | Results Query 1 # § | Results Query 2 # § |
|---|---|---|---|---|---|---|---|
| Bohm H et al., 2014 [19] RCT crossover  | 8 BSCP GMFCS I-II-III mean age 13.9 ± 4.3 (7–18) y | 6 weeks of climbing therapy (CT), 1.5 h × 2/w; 4 w washout period between treatments | PT 1.5 h twice a week (NDT) | Pre- (T0) and post-intervention (T1) | Query 1: Walking speed, GPS, step length, step time | Mean T1-T0 Δ in:
| / |
| Clutterbuck G L et al., 2020 [22] RCT  | 54 CP GMFCS I-II mean age IG 8.9 ± 2 and CG 8.6 ± 2 (6–12) y | Sports Stars: sports-specific gross motor activity training, sports education, teamwork development and confidence building for four sports: soccer, netball, T-ball and cricket; 8 weeks, 1 h × 1/w | Waiting list received standard care: PT mean 1.3 h (0–4 h) in 8 weeks. | Pre-intervention (T0), 8 w post intervention (T1), 12 w Fu (T2) | Query 1: mCOPM-activity, TGMD-2, GMFM-Challenge, TUG, MPST, 10 × 5mST, SBJ, Vertical Jump and Seated Throw. Query 2: m-COPM participation, CAPE-PAC, CP QOL-Child | Group by time effects using a linear mixed model analysis to compare groups: query 1
| Group by time effects using a linear mixed model analysis to compare groups: query 2:
|
| Coman C et al., 2023 [20] RCT  | 46 CP, GMFCS I-II, mean age IG 10y6m ± 2y6m and CG 10 y10 m ± 2y6m (7–17 y) | Pilates-based exercises with supplemental home exercise program, 60 m × 2/w for 4 w (480 m) | Conventional PT | Pre (T0) and 14 d post intervention (T1) | Query 1: 3DGA (speed, GPS, etc.), FWT, BBS, TSLS | Mean IG-CG Δ in T1-T0:
| / |
| Declerck M et al., 2016 [18] RCT  | 14 CP, GMFCS I-II-III mean age IG 8.7 ± 3.4, CG 11.8 ± 3.5 (7–17) y | 10 w swimming program, 40–50 m × 2/w + conventional PT | Conventional PT | Pre (T0) and post (T1) intervention, after the 5 w Fu (T2) | Query 1: 1mFWT, WOTA 2, VAS, rFPS, PedsQL-MFS Query 2: 5-point Likert scale for enjoyment, % of adherence | Query 1: mean T1-T0 and T2-T1 Δ in:
| Query 2:
|
| Desmuth S K et al., 2012 [30] RCT  | 62 CP GMFCS I-II-III, median age IG 10.7 (8.5, 12.3), CG 11.2 (9.8, 13.3) range 7–18 y | Stationary cycling intervention, 1 h, 30 sessions over 12 w | No intervention | Pre (T0) and post intervention (T1) | Query 2: PedsQL, PODCI | / | Mean scores at T0 and T1 in:
|
| Elnaggar R K et al., 2022 [23] RCT  | 56 CP GMFCS I-II mean age IG 13.40 ± 1.37, CG 13.96 ± 1.45 (12–16) y | Aqua-PLYO (10′ low-impact aerobics warmup and cool-down and 25′ mixed exercises in waist-level immersion depth) 45 m × 3/w (2-day recovery in between) for 12 w | Conventional PT45 m × 3/w (non-consecutive days) for 12 w | Pre- (T0) and post-intervention (T1) | Query 1: Postural stability by LOSdynamic (M-DC, ReT, M-Vel, Mx-Exc, EP-Exc). Functional outcomes: 30s-STS, TUDS, DGI. | Mean scores at T0 and T1 in:
| / |
| Gibson N et al., 2017 [27] RCT  | 42 CP GMFCS I-II-III mean age IG 12.4 ± 2.7, CG 12.5 ± 2.8 (9–18) y | Running training at a community therapy organization 1 h × 2/w for 12 w and a home program × 2/w | Conventional PT | Pre (T0) and post intervention (T1) | Query 1: Improvement in running ability assessed by GAS and HLMAT; aerobic fitness by SRT, anaerobic fitness by MPST, agility by 10 × 5-Meter Sprint Test Query 2: PEM-CY | Mean Δ T1-T0 in:
| PEM-CY School: IG > CG 1.2 (1.0–1.4) * |
| Hanssen B et al., 2022 [24] RCT  | 49 CP GMFCS I-II-III Mean age IG 8.3 ± 2.0, CG 8.5 ± 2.1 y. | Progressive resistance home training (PRT) × 3–4/w (non-consecutive days) for 12 w | Conventional PT | Pre- (T0) and post-intervention (T1) | Query 1: Isometric strength KE, KF, PF; LSU, STS, UHR, BHR, SLJ, 1MWT, GMFM | Mean Δ T1-T0 in:
| / |
| Lee HK et al., 2024 [28] RCT  | 25 DD mean age 9 ± 1.6 y | VR + gym-based PA (5 m warm-up, 25 m VR PA, 25 m gym-based PA, 5 m cool-down) × 2/w for 12 w | No treatment | Pre- (T0), post-treatment (T1), 12 w Fu (T2) | Query 1: MVPA using GENEActive, SSRS | Mean Δ between groups at T1:
| / |
| Raghupathy M K et al., 2021 [26] RCT  | 36 DS, mean age IG 7.8 ± 1.3, CG 8.4 ± 1.3 (6–10) y | Indian traditional dance 1 h × 3/w for 6 w | Neuromuscular training 1 h × 3/w for 6 w | Pre- (T0) and post-intervention (T1) | Query 1: TGMD-2, FSST, PBS | Mean Δ T1-T0 in:
| / |
| Scholtes V A et al., 2010 [25] RCT  | 51 CP GMFCS I-II-III, mean age 10 y 5 mo | School PRT for lower limbs, 45–60 m × 3/w for 12 w | Conventional PT × 1–3/w | Pre- (T0), post-training (T1), 6 w Fu (T2). | Query 1: Mobility: GMFM-66, STS, LSU. 6-repetition maximum muscle strength on a leg-press. Isometric strength KE, KF, PF using a hand-held dynamometer. MobQues-28. | Mean T0, T1 and T3:
| / |
| Schranz C et al., 2018 [17] RCT  | 22 CP GMFCS I-II mean age IG 13.4 ± 2.4, CG 12.2 ± 2.7 y | HICT (as many repetitions as possible within 30 s intervals) × 3/w for 8 w | Home-based PRT × 3/w for 8 w | Pre- (T0), post-treatment (T1), 2 mo Fu (T2) | Query 1: Muscle strength (KF, MPST, TST, 6-MWT, GPS, TUG Query 2: ASKp, PODCI | Mean Δ T1-T0 in:
| Mean Δ T1-T0 in:
|
| Shen X et al., 2024 [29] RCT  | 36 IDD, mean age 16.44 y ± 0.73 | 6-month school-based adapted PA 3 days a week + remote collaboration-based family PA | 6-month school-based adapted PA 3 days a week | Pre- (T0), post-treatment (T1), 2 mo Fu (T2) | Query 1: Time spent at MVPA > 2800 CPM by means of actigraphs. Sedentary time at <100 CPM (LPA 100–2799 CPM). Query 2: WHOQOL-DIS-ID; PACES. |
|
|
| Toovey RAM et al., 2021 [21] RCT  | 62 CP GMFCS I-II, mean age IG 9.11 ± 2.8, CG 9.1 ± 2.4 (6–15) y | Task-specific bicycleskills training program 2 h/d × 3 consecutive days at an outdoor park + 30 m/d home practice × 4 d, for 1 w | Parent-led bicycle skills home program 30–45 m/d, for 1 w | Pre-, 1 w post- (T1) and 3 mo post-intervention (T2) | Query 1: GAS at T1 and T1; PAQC; active time by means of Activ8 triaxial accelerometer Query 2: SPP-YC, SPP-C or SPP-A; CHU9D; PEDI-CAT | Mean Δ between IG and CG at T1 and T2 in:
| Mean Δ between IG and CG at T1 and T2 in:
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faccioli, S.; Marianna, A.; Agata, M.G.R.; Silvia, S.; Silvia, S. Gross Motor Performance, Participation and Quality of Life After Adapted Physical Activity Interventions in Pediatric Populations with Neuromotor Disability: A Systematic Review. Children 2025, 12, 815. https://doi.org/10.3390/children12070815
Faccioli S, Marianna A, Agata MGR, Silvia S, Silvia S. Gross Motor Performance, Participation and Quality of Life After Adapted Physical Activity Interventions in Pediatric Populations with Neuromotor Disability: A Systematic Review. Children. 2025; 12(7):815. https://doi.org/10.3390/children12070815
Chicago/Turabian StyleFaccioli, Silvia, Avola Marianna, Mangano Giulia Rita Agata, Sghedoni Silvia, and Sassi Silvia. 2025. "Gross Motor Performance, Participation and Quality of Life After Adapted Physical Activity Interventions in Pediatric Populations with Neuromotor Disability: A Systematic Review" Children 12, no. 7: 815. https://doi.org/10.3390/children12070815
APA StyleFaccioli, S., Marianna, A., Agata, M. G. R., Silvia, S., & Silvia, S. (2025). Gross Motor Performance, Participation and Quality of Life After Adapted Physical Activity Interventions in Pediatric Populations with Neuromotor Disability: A Systematic Review. Children, 12(7), 815. https://doi.org/10.3390/children12070815





