Cranial Ultrasonography—Standards in Diagnosis of Intraventricular Hemorrhage and Ventricular Dilatation in Premature Neonates
Abstract
1. Introduction
1.1. Intraventricular Hemorrhage—Still a Common Complication of Extreme Prematurity
1.2. Posthemorrhagic Ventriculomegaly (PHVM)—Different Pathogenic Mechanisms
1.3. Challenges in Management of IVH and PHVM in NEONATAL Intensive Care Units (NICUs)
1.4. Neurologic Outcomes of Babies with IVH and PHVM—Prediction and Prevention
1.5. Role of CUS in Management of Neurologic Complications of Prematurity
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Limbrick, D.D.; de Vries, L.S. New insights into the management of post-hemorrhagic hydrocephalus. Semin. Perinatol. 2022, 46, 151597. [Google Scholar] [CrossRef] [PubMed]
- Papile, L.-A.; Burstein, J.; Burstein, R.; Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infants with birth weights less than 1,500 gm. J. Pediatr. 1978, 92, 529–534. [Google Scholar] [CrossRef]
- Bowerman, R.; Donn, S.; Silver, T.; Jaffe, M. Natural history of neonatal periventricular/intraventricular hemorrhage and its complications: Sonographic observations. Am. J. Roentgenol. 1984, 143, 1041–1052. [Google Scholar] [CrossRef]
- Cheng, B.; Ballabh, P. Recovery of the brain after intraventricular hemorrhage. Semin. Fetal Neonatal Med. 2022, 27, 101224. [Google Scholar] [CrossRef] [PubMed]
- Starr, R.; De Jesus, O.; Shah, S.D.; Borger, J. Periventricular and Intraventricular Hemorrhage. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK538310/ (accessed on 27 April 2023).
- El-Dib, M.; Limbrick, D.D.; Inder, T.; Whitelaw, A.; Kulkarni, A.V.; Warf, B.; Volpe, J.J.; de Vries, L.S. Management of Post-hemorrhagic Ventricular Dilatation in the Infant Born Preterm. J. Pediatr. 2020, 226, 16–27.e3. [Google Scholar] [CrossRef]
- Murphy, B.P. Posthaemorrhagic ventricular dilatation in the premature infant: Natural history and predictors of outcome. Arch. Dis. Child. Fetal Neonatal Ed. 2002, 87, F37–F41. [Google Scholar] [CrossRef] [PubMed]
- Law, J.B.; Wood, T.R.; Gogcu, S.; Comstock, B.A.; Dighe, M.; Perez, K.; Puia-Dumitrescu, M.; Mayock, D.E.; Heagerty, P.J.; Juul, S.E. Intracranial Hemorrhage and 2-Year Neurodevelopmental Outcomes in Infants Born Extremely Preterm. J. Pediatr. 2021, 238, 124–134.e10. [Google Scholar] [CrossRef]
- Hill, A.; Shackelford, G.D.; Volpe, J.J. A potential mechanism of pathogenesis for early posthemorrhagic hydrocephalus in the premature newborn. Pediatrics 1984, 73, 19–21. [Google Scholar] [CrossRef]
- Lolansen, S.D.; Rostgaard, N.; Barbuskaite, D.; Capion, T.; Olsen, M.H.; Norager, N.H.; Vilhardt, F.; Andreassen, S.N.; Toft-Bertelsen, T.L.; Ye, F.; et al. Posthemorrhagic hydrocephalus associates with elevated inflammation and CSF hypersecretion via activation of choroidal transporters. Fluids Barriers CNS 2022, 19, 62. [Google Scholar] [CrossRef]
- Louveau, A.; Smirnov, I.; Keyes, T.J.; Eccles, J.D.; Rouhani, S.J.; Peske, J.D.; Derecki, N.C.; Castle, D.; Mandell, J.W.; Lee, K.S.; et al. Structural and functional features of central nervous system lymphatic vessels. Nature 2015, 523, 337–341. [Google Scholar] [CrossRef]
- Karimy, J.K.; Zhang, J.; Kurland, D.B.; Theriault, B.C.; Duran, D.; A Stokum, J.; Furey, C.G.; Zhou, X.; Mansuri, M.S.; Montejo, J.; et al. Inflammation-dependent cerebrospinal fluid hypersecretion by the choroid plexus epithelium in posthemorrhagic hydrocephalus. Nat. Med. 2017, 23, 997–1003. [Google Scholar] [CrossRef]
- Steffensen, A.B.; Oernbo, E.K.; Stoica, A.; Gerkau, N.J.; Barbuskaite, D.; Tritsaris, K.; Rose, C.R.; MacAulay, N. Cotransporter-mediated water transport underlying cerebrospinal fluid formation. Nat. Commun. 2018, 9, 2167. [Google Scholar] [CrossRef]
- Toft-Bertelsen, T.L.; Barbuskaite, D.; Heerfordt, E.K.; Lolansen, S.D.; Andreassen, S.N.; Rostgaard, N.; Olsen, M.H.; Norager, N.H.; Capion, T.; Rath, M.F.; et al. Lysophosphatidic acid as a CSF lipid in posthemorrhagic hydrocephalus that drives CSF accumulation via TRPV4-induced hyperactivation of NKCC1. Fluids Barriers CNS 2022, 19, 69. [Google Scholar] [CrossRef]
- Piazza, M.; Damore, G.; Costa, B.; Gioannini, T.L.; Weiss, J.P.; Peri, F. Hemin and a metabolic derivative coprohemin modulate the TLR4 pathway differently through different molecular targets. Innate Immun. 2011, 17, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Rothaug, M.; Becker-Pauly, C.; Rose-John, S. The role of interleukin-6 signaling in nervous tissue. Biochim. Biophys. Acta Mol. Cell Res. 2016, 1863, 1218–1227. [Google Scholar] [CrossRef] [PubMed]
- Lolansen, S.D.; Rostgaard, N.; Oernbo, E.K.; Juhler, M.; Simonsen, A.H.; Macaulay, N. Inflammatory Markers in Cerebrospinal Fluid from Patients with Hydrocephalus: A Systematic Literature Review. Dis. Markers 2021, 2021, 8834822. [Google Scholar] [CrossRef] [PubMed]
- Wostrack, M.; Reeb, T.; Martin, J.; Kehl, V.; Shiban, E.; Preuss, A.; Ringel, F.; Meyer, B.; Ryang, Y.-M. Shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage: The role of intrathecal interleukin-6. Neurocrit Care 2014, 21, 78–84. [Google Scholar] [CrossRef]
- Groulx-Boivin, E.; Paquette, M.; Khairy, M.; Beltempo, M.; Dudley, R.; Ferrand, A.; Guillot, M.; Bizgu, V.; Garfinkle, J. Spontaneous resolution of post-hemorrhagic ventricular dilatation in preterm newborns and neurodevelopment. Pediatr. Res. 2023, 94, 1428–1435. [Google Scholar] [CrossRef]
- Cizmeci, M.N.; Groenendaal, F.; de Vries, L.S. Timing of Intervention for Posthemorrhagic Ventricular Dilatation: An Ongoing Debate. J. Pediatr. 2021, 234, 14–16. [Google Scholar] [CrossRef]
- Pindrik, J.; Schulz, L.; Drapeau, A. Diagnosis and Surgical Management of Neonatal Hydrocephalus. Semin. Pediatr. Neurol. 2022, 42, 100969. [Google Scholar] [CrossRef]
- Kolnik, S.E.; Upadhyay, K.; Wood, T.R.; Juul, S.E.; Valentine, G.C. Reducing Severe Intraventricular Hemorrhage in Preterm Infants with Improved Care Bundle Adherence. Pediatrics 2023, 152, e2021056104. [Google Scholar] [CrossRef] [PubMed]
- Whitelaw, A.; Lee-Kelland, R. Repeated lumbar or ventricular punctures in newborns with intraventricular haemorrhage. Cochrane Database Syst. Rev. 2017, 2017, CD000216. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, M.J.; de Vries, L.S.; Groenendaal, F.; Koopman, C.; Pistorius, L.R.; Mulder, E.J.H.; Benders, M.J.N.L. New reference values for the neonatal cerebral ventricles. Radiology 2012, 262, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Payne, A.H.; Hintz, S.R.; Hibbs, A.M.; Walsh, M.C.; Vohr, B.R.; Bann, C.M.; Wilson-Costello, D.E. Neurodevelopmental outcomes of extremely low-gestational-age neonates with low-grade periventricular-intraventricular hemorrhage. JAMA Pediatr. 2013, 167, 451–459. [Google Scholar] [CrossRef]
- Shah, V.; Musrap, N.; Maharaj, K.; Afifi, J.; El-Naggar, W.; Kelly, E.; Mukerji, A.; Shah, P.; Vincer, M. Grading of Intraventricular Hemorrhage and Neurodevelopment in Preterm <29 Weeks’ GA in Canada. Children 2022, 9, 1948. [Google Scholar] [CrossRef]
- Wang, Y.; Song, J.; Zhang, X.; Kang, W.; Li, W.; Yue, Y.; Zhang, S.; Xu, F.; Wang, X.; Zhu, C. The impact of different degrees of intraventricular hemorrhage on mortality and neurological outcomes in very preterm infants: A prospective cohort study. Front. Neurol. 2022, 13, 853417. [Google Scholar] [CrossRef]
- Lai, G.Y.; Aouad, P.; DeRegnier, R.A.O.; Dizon, M.L.V.; Palasis, S.; Lam, S.K. Ventriculomegaly thresholds for prediction of symptomatic post-hemorrhagic ventricular dilatation in preterm infants. Pediatr. Res. 2022, 92, 1621–1629. [Google Scholar] [CrossRef]
- Isaacs, A.M.; Shannon, C.N.; Browd, S.R.; Hauptman, J.S.; Holubkov, R.; Jensen, H.; Kulkarni, A.V.; McDonald, P.J.; McDowell, M.M.; Naftel, R.P.; et al. Neurodevelopmental outcomes of permanent and temporary CSF diversion in posthemorrhagic hydrocephalus: A Hydrocephalus Clinical Research Network study. J. Neurosurg. Pediatr. 2025, 35, 315–326. [Google Scholar] [CrossRef]
- Massey-Naranjo, A.Y. Normal values of the fronto-occipital relationship in fetuses between 18 and 40 weeks at two maternal fetal medicine units: Bogotá, Colombia. J. Clin. Ultrasound 2023, 52, 152–162. [Google Scholar] [CrossRef]
- Dudink, J.; Steggerda, S.J.; Horsch, S.; eurUS.brain Group. State-of-the-art neonatal cerebral ultrasound: Technique and reporting. Pediatr. Res. 2020, 87 (Suppl. S1), 3–12. [Google Scholar] [CrossRef]
- De Vries, L.S.; Benders, M.J.; Groenendaal, F. Imaging the premature brain: Ultrasound or MRI? Neuroradiology 2013, 55, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Al-Abdi, S.Y.; Al-Aamri, M.A. A systematic review and meta-analysis of the timing of early intraventricular hemorrhage in preterm neonates: Clinical and research implications. J. Clin. Neonatol. 2014, 3, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Pierrat, V.; Duquennoy, C.; Van Haastert, I.C.; Ernst, M.; Guilley, N.; De Vries, L.S. Ultrasound diagnosis and neurodevelopmental outcome of localised and extensive cystic periventricular leucomalacia. Arch. Dis. Child. Fetal Neonatal Ed. 2001, 84, F151–F156. [Google Scholar] [CrossRef]
- Pisapia, J.M.; Rozycki, M.; Akbari, H.; Bakas, S.; Thawani, J.P.; Moldenhauer, J.S.; Storm, P.B.; Zarnow, D.M.; Davatzikos, C.; Heuer, G.G. Correlations of atrial diameter and frontooccipital horn ratio with ventricle size in fetal ventriculomegaly. J. Neurosurg. Pediatr. 2017, 19, 300–306. [Google Scholar] [CrossRef]
- De Vries, L.S.; Groenendaal, F.; Liem, K.D.; Heep, A.; Brouwer, A.J.; van’t Verlaat, E.; Benavente-Fernández, I.; van Straaten, H.L.; van Wezel-Meijler, G.; Smit, B.J.; et al. Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: A randomised controlled trial. Arch. Dis. Child. Fetal Neonatal Ed. 2019, 104, F70–F75. [Google Scholar] [CrossRef]
- Benavente-Fernández, I.; Steggerda, S.J.; Liem, K.D.; Lubián-López, S.; de Vries, L.S. Ultrasonographic Estimation of Ventricular Volume in Infants Born Preterm with Posthemorrhagic Ventricular Dilatation: A Nested Substudy of the Randomized Controlled Early Versus Late Ventricular Intervention Study (ELVIS) Trial. J. Pediatr. 2023, 261, 113578. [Google Scholar] [CrossRef]
- Cizmeci, M.N.; Khalili, N.; Claessens, N.H.P.; Groenendaal, F.; Liem, K.D.; Heep, A.; Benavente-Fernandez, I.; van Straaten, H.L.M.; van Wezel-Meijler, G.; Steggerda, S.J.; et al. Assessment of Brain Injury and Brain Volumes after Posthemorrhagic Ventricular Dilatation: A Nested Substudy of the Randomized Controlled ELVIS Trial. J. Pediatr. 2019, 208, 191–197.e2. [Google Scholar] [CrossRef] [PubMed]
- Luyt, K.; Jary, S.L.; Lea, C.L.; Young, G.J.; E Odd, D.; E Miller, H.; Kmita, G.; Williams, C.; Blair, P.S.; Hollingworth, W.; et al. Drainage, irrigation and fibrinolytic therapy (DRIFT) for posthaemorrhagic ventricular dilatation: 10-year follow-up of a randomised controlled trial. Arch. Dis. Child. Fetal Neonatal Ed. 2020, 105, 466–473. [Google Scholar] [CrossRef]
- Cizmeci, M.N.; Groenendaal, F.; Liem, K.D.; van Haastert, I.C.; Benavente-Fernández, I.; van Straaten, H.L.; Steggerda, S.; Smit, B.J.; Whitelaw, A.; Woerdeman, P.; et al. Randomized Controlled Early versus Late Ventricular Intervention Study in Posthemorrhagic Ventricular Dilatation: Outcome at 2 Years. J. Pediatr. 2020, 226, 28–35.e2. [Google Scholar] [CrossRef]
- Leijser, L.M.; Miller, S.P.; van Wezel-Meijler, G.; Brouwer, A.J.; Traubici, J.; van Haastert, I.C.; Whyte, H.E.; Groenendaal, F.; Kulkarni, A.V.; Han, K.S.; et al. Posthemorrhagic ventricular dilatation in preterm infants When best to intervene. Neurology 2018, 90, E698–E706. [Google Scholar] [CrossRef]
- Leijser, L.M.; Scott, J.N.; Roychoudhury, S.; Zein, H.; Murthy, P.; Thomas, S.P.; Mohammad, K.; on behalf of the Calgary Neonatal Neuro-Critical Care Program. Post-hemorrhagic ventricular dilatation: Inter-observer reliability of ventricular size measurements in extremely preterm infants. Pediatr. Res. 2021, 90, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Obeid, R.; Jacobs, M.; Chang, T.; Massaro, A.N.; Bluth, E.; Murnick, J.G.; Bulas, D.; Bandarkar, A.; Oluigbo, C.; Penn, A.A. The utility of the fronto-temporal horn ratio on cranial ultrasound in premature newborns: A ventriculomegaly marker. Pediatr. Res. 2021, 89, 1715–1723. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, R.; Brown, B.P.; Kralik, S.F.; Bain, D.; Persohn, S.; Territo, P.R.; Jea, A.; Karmazyn, B. Frontal occipital and frontal temporal horn ratios: Comparison and validation of head ultrasound-derived indexes with MRI and ventricular volumes in infantile ventriculomegaly. Am. J. Roentgenol. 2019, 213, 925–931. [Google Scholar] [CrossRef]
- Lai, G.Y.; Abdelmageed, S.; DeRegnier, R.A.O.; Gaebler-Spira, D.; Dizon, M.L.V.; Lam, S.K. Degree of ventriculomegaly predicts school-aged functional outcomes in preterm infants with intraventricular hemorrhage. Pediatr. Res. 2022, 91, 1238–1247. [Google Scholar] [CrossRef]
- Cizmeci, M.N.; de Vries, L.S.; Ly, L.G.; van Haastert, I.C.; Groenendaal, F.; Kelly, E.N.; Traubici, J.; Whyte, H.E.; Leijser, L.M. Periventricular Hemorrhagic Infarction in Very Preterm Infants: Characteristic Sonographic Findings and Association with Neurodevelopmental Outcome at Age 2 Years. J. Pediatr. 2020, 217, 79–85.e1. [Google Scholar] [CrossRef]
- You, S.K. Neuroimaging of Germinal Matrix and Intraventricular Hemorrhage in Premature Infants. J. Korean Neurosurg. Soc. 2023, 66, 239–246. [Google Scholar] [CrossRef]
- Davies, M.W.; Swaminathan, M.; Chuang, S.L.; Betheras, F.R. Reference ranges for the linear dimensions of the intracranial ventricles in preterm neonates. Arch. Dis. Child. Fetal Neonatal Ed. 2000, 82, F218–F223. [Google Scholar] [CrossRef] [PubMed]
- Cizmeci, M.N.; de Vries, L.S. Fronto-temporal horn ratio: Yet another marker of ventriculomegaly. Pediatr. Res. 2021, 89, 1602–1603. [Google Scholar] [CrossRef]
- Whittemore, B.A.; Swift, D.M.; Thomas, J.M.; Chalak, L.F. A neonatal neuroNICU collaborative approach to neuromonitoring of posthemorrhagic ventricular dilation in preterm infants. Pediatr. Res. 2022, 91, 27–34. [Google Scholar] [CrossRef]
- Han, R.H.; Berger, D.; Gabir, M.; Baksh, B.S.; Morales, D.M.; Mathur, A.M.; Smyser, C.D.; Strahle, J.M.; Limbrick, D.D. Time-to-event analysis of surgically treated posthemorrhagic hydrocephalus in preterm infants: A single-institution retrospective study. Child’s Nerv. Syst. 2017, 33, 1917–1926. [Google Scholar] [CrossRef]
- Wellons, J.C.; Shannon, C.N.; Holubkov, R.; Riva-Cambrin, J.; Kulkarni, A.V.; Limbrick, D.D., Jr.; Whitehead, W.; Browd, S.; Rozzelle, C.; Simon, T.D.; et al. Shunting outcomes in posthemorrhagic hydrocephalus: Results of a Hydrocephalus Clinical Research Network prospective cohort study. J. Neurosurg. Pediatr. 2017, 20, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Bassan, H.; Benson, C.B.; Limperopoulos, C.; Feldman, H.A.; Ringer, S.A.; Veracruz, E.; Stewart, J.E.; Soul, J.S.; DiSalvo, D.N.; Volpe, J.J.; et al. Ultrasonographic features and severity scoring of periventricular hemorrhagic infarction in relation to risk factors and outcome. Pediatrics 2006, 117, 2111–2118. [Google Scholar] [CrossRef] [PubMed]
- Boyle, M.; Shim, R.; Gnanasekaran, R.; Tarrant, A.; Ryan, S.; Foran, A.; McCallion, N. Inclusion of extremes of prematurity in ventricular index centile charts. J. Perinatol. 2015, 35, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Flanders, T.M.; Lang, S.-S.; Ko, T.S.; Andersen, K.N.; Jahnavi, J.; Flibotte, J.J.; Licht, D.J.; Tasian, G.E.; Sotardi, S.T.; Yodh, A.G.; et al. Optical Detection of Intracranial Pressure and Perfusion Changes in Neonates with Hydrocephalus. J. Pediatr. 2021, 236, 54–61.e1. [Google Scholar] [CrossRef]
- Riva-Cambrin, J.; Shannon, C.N.; Holubkov, R.; Whitehead, W.E.; Kulkarni, A.V.; Drake, J.; Simon, T.D.; Browd, S.R.; Kestle, J.R.W.; Wellons, J.C. Center effect and other factors influencing temporization and shunting of cerebrospinal fluid in preterm infants with intraventricular hemorrhage. J. Neurosurg. Pediatr. 2012, 9, 473. [Google Scholar] [CrossRef]
- Toma, A.I.; Dima, V.; Rusu, L.; Nemeș, A.F.; Gonț, B.F.; Arghirescu, A.; Necula, A.; Fieraru, A.; Stoiciu, R.; Andrășoaie, L.; et al. Cerebral Ultrasound at Term-Equivalent Age: Correlations with Neuro-Motor Outcomes at 12–24 Months Corrected Age. Children 2024, 12, 30. [Google Scholar] [CrossRef]
- Edwards, A.D.; Redshaw, M.E.; Kennea, N.; Rivero-Arias, O.; Gonzales-Cinca, N.; Nongena, P.; Ederies, M.; Falconer, S.; Chew, A.; Omar, O.; et al. Effect of MRI on preterm infants and their families: A randomised trial with nested diagnostic and economic evaluation. Arch. Dis. Child. Fetal Neonatal Ed. 2018, 103, F15–F21. [Google Scholar] [CrossRef]
- Toma, A.I.; Dima, V.; Alexe, A.; Rusu, L.; Nemeș, A.F.; Gonț, B.F.; Arghirescu, A.; Necula, A.; Fieraru, A.; Stoiciu, R. Correlations between Head Ultrasounds Performed at Term-Equivalent Age in Premature Neonates and General Movements Neurologic Examination Patterns. Life 2023, 14, 46. [Google Scholar] [CrossRef]
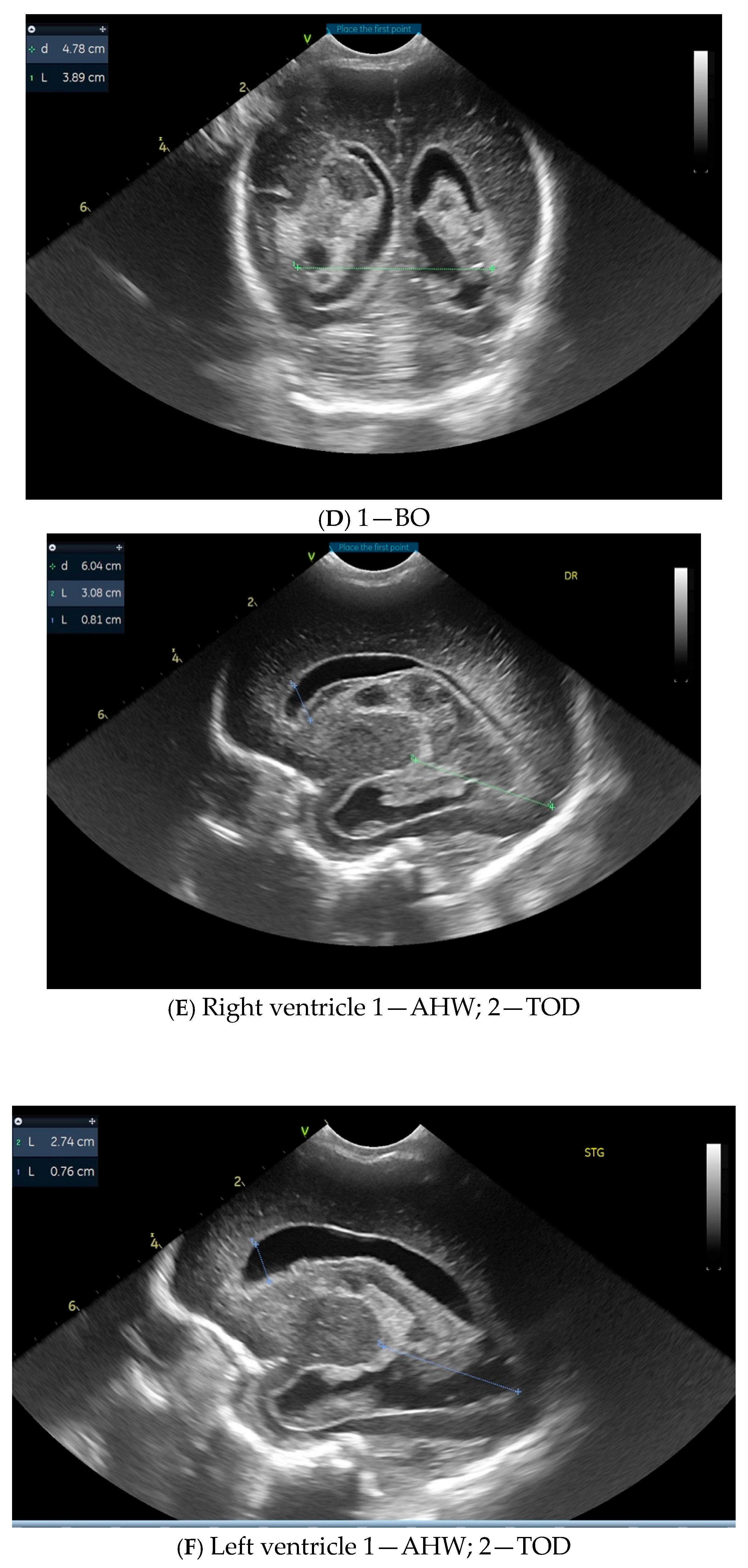
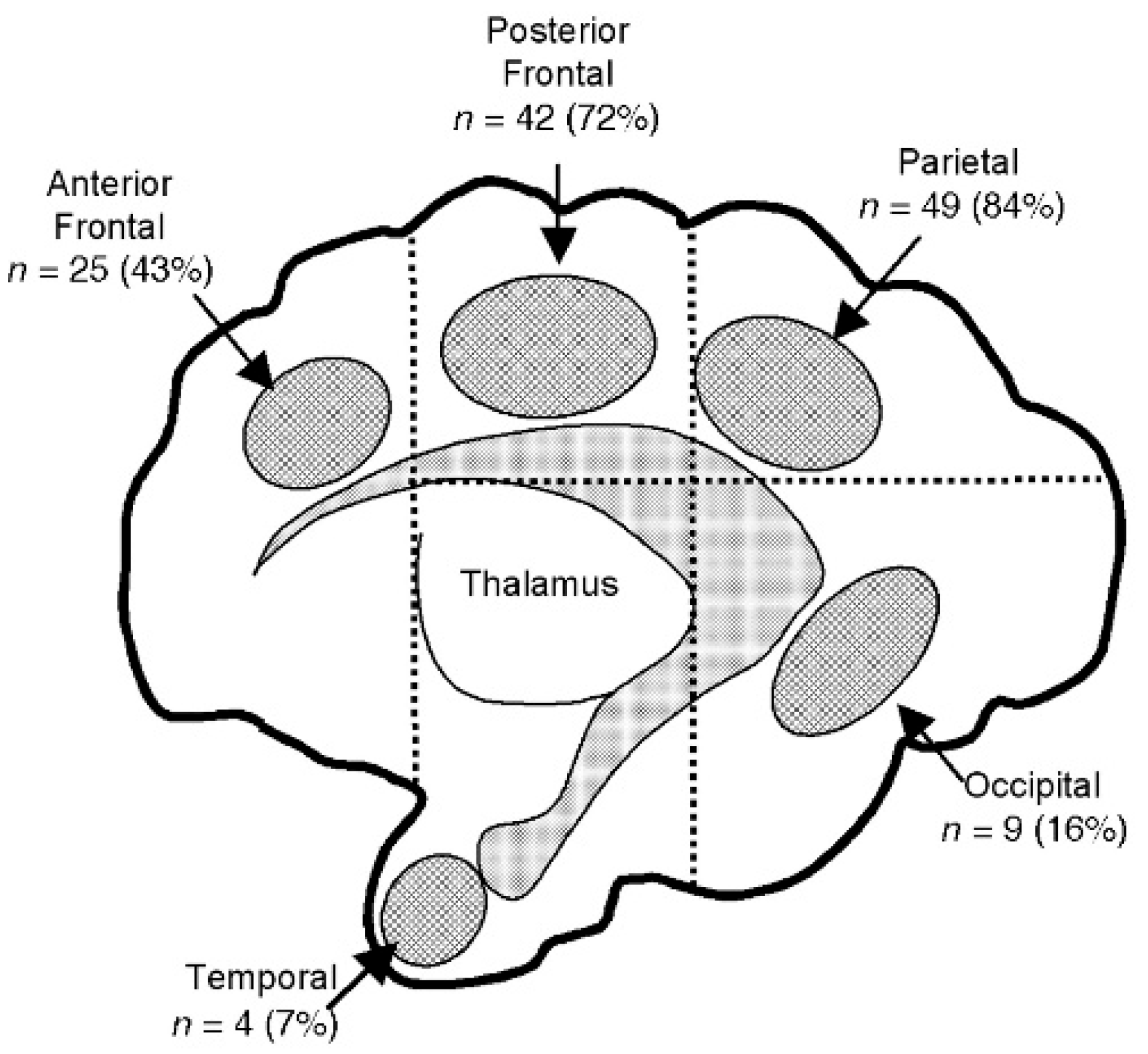
| Index/Ratios with Threshold Values | Study—Name/Type | Population | Outcomes | Conclusions |
| Low threshold (LT) VI > p97, AHW > 6 mm, FOHR—430.43 High threshold (HT) VI = p97 + 4 mm, AHW > 10 mm, FOHR—0.49 | ELVIS (European Early vs. Late Ventricular Intervention Study, 2002–2007); multicenter retrospective study (five NICUs) “Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: a randomised controlled trial” [36] | 95 patients with PHVM; 31 treated at LT; 42 infants treated at HT 22 patients without intervention | Correlation between time of onset of treatment of PHVD and difference in the requirement of a ventriculoperitoneal (VP) shunt and/or neurodevelopmental outcome | Late intervention required shunt insertion significantly more often than those treated early. |
| Low threshold VI > p97, AHW > 6 mm, FOHR—0.43 High threshold VI = p97 + 4 mm, AHW > 10 mm Ventr. volume | “Ultrasonographic Estimation of Ventricular Volume in Infants Born Preterm with Posthemorrhagic Ventricular Dilatation: A Nested Substudy of the Randomized Controlled Early Versus Late Ventricular Intervention Study (ELVIS) Trial” [37] | 59 patients from ELVIS from four participating centers | Correlation between ventricular volume (VV) in PHVM and prediction for ventriculoperitoneal (VP)-shunt insertion and 2-year or NDI | Maximum VI and AHW before reservoir insertion were independently associated with the need for VP shunt. The proposed thresholds in the ELVIS trial were associated with significant different long-term outcomes. |
| Low threshold VI > p97, AHW > 6 mm, FOHR 0.42 Hgh Threshold VI = p97 + 4 mm, AHW > 10 mm, FOHR 0.48 | “Assessment of Brain Injury and Brain Volumes after Posthemorrhagic Ventricular Dilatation: A Nested Substudy of the Randomized Controlled ELVIS Trial” [38] | 126 preterm infants ≤ 34 weeks and PHVM | Kidokoro Global Brain Abnormality Score and the frontal and occipital horn ratio were measured | FOHR was lower in the low-threshold group (p = 0.001). Infants in the low-threshold group had a normal or mildly increased score vs. infants in the high-threshold group (p = 0.002). |
| VI minimum p97 + 4 mm, VI max—no upper limit | “Drainage, irrigation and fibrinolytic therapy (DRIFT) for posthaemorrhagic ventricular dilatation): 10-year follow-up of a randomised controlled trial” (four centers) [39] | 77 preterm infants with IVH and progressive PHVM | Death Risk of VP shunt NDI | No significant difference in terms of death or need for VP shunt, but significantly lower NDI in the treatment arm. |
| Low threshold VI > p97 AHW > 6 mm TOD > 25 mm High threshold p97 + 4 mm AHW > 10 mm | “Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: a randomised controlled trial” [36] | 126 preterm < 34 weeks (14 NICUs) | Death Risk of VP shunt NDI | There was no significant difference in the primary composite outcome of VP shunt placement or death or lower VP shunt rate. Infants treated at the lower threshold received more invasive procedures. |
| FOHR 0.66 FTHR 0.62 AHW 15.5 mm VI 8.4 mm > p97 | “Ventriculomegaly thresholds for prediction of symptomatic posthemorrhagic venticular dilatation in preterm infants” [28] | 132 patients Retrospective, 2007–2020 | Threshold values of ventricular indices predicting surgical intervention | Indices were predictive from the first scans for progressive persistent ventriculomegaly with different sensitivity and specificity. |
| VI > p97, AHW > 6 mm (low threshold) VI > p97 + 4 mm and AHW > 10 mm (high threshold) | “Randomized Controlled Early versus Late Ventricular Intervention Study in Posthemorrhagic Ventricular Dilatation: Outcome at 2 years” [40] | 126 infants | Death or cerebral palsy or Bayley composite cognitive/motor scores < −2SD at 24 months corrected age | Earlier intervention was associated with lower odds of death or severe NDI. |
| FOHR > 0.55 | “Neurodevelopmental outcomes of permanent and temporary CSF diversion in posthemorrhagic hydrocephalus: a Hydrocephalus Clinical Research Network study” [29] | 106 patients 2012–2021 | Neurodevelopmental outcomes in preterm infants diagnosed with PHVM after temporary vs. permanent CSF diversion strategies | NDI is correlated with high values of FOHR at conversion to permanent diversion. |
| Early approach (EA) VI < +2SD AHW < 6 mm Late approach (LA) | “Posthemorrhagic ventricular dilatation in preterm infants: When best to intervene?” [41] | 127 preterm infants, gestation < 30 weeks, with early vs. late approach | Death Risk of VP shunt NDI | Significant lower rate of shunt placement in EA group. In the LA group, survivors had lower cognitive and motor scores (p = 0.002); VI comparable in EA/LA groups; AHW larger in infants undergoing intervention (p = 0.04). |
| VI AHW FHOR | “Post-hemorrhagic ventricular dilatation: inter-observer reliability of ventricular size measurements in extremely preterm infants” [42] | 139 preterm infants with IVH | Inter-observer reliability of these indices for prediction of severe PHVD | AHW and VI are highly reproducible in experienced hands compared to FTHR, with AHW from the second week onwards being the strongest predictor for receiving surgical intervention. |
| VI > p97 AHW > 6 mm compared to VI and FOHR | “Spontaneous resolution of post-hemorrhagic ventricular dilatation in preterm newborns and neurodevelopment” [19] | 88 preterms with PHVM MCT retrospective study, 2007–2020 | Role of ventricular indices in prediction of spontaneous resolution of PHVM and NDI | Spontaneous resolution of PHVM was better predicted by smaller AHW. Subjects with spontaneous resolution of PHVM had significant lower NDI. |
| FTHR 0.51 | “The utility of the fronto-temporal horn ratio on cranial ultrasound in premature newborns: a ventriculomegaly marker” [43] | 100 neonates with IVH; retrospective study—2011–2014 | Identifying the normal value of FTHR on CUS in relation to WMI and cerebral palsy (CP) | The FTHR cut-off point of 0.51 had the highest sensitivity and specificity for moderate-to-severe WMI. In the IVH grade 3–4 group, the elevated FTHR correlated with a lower FA and higher GMFCS. |
| FTHR FOHR | “Frontal occipital and frontal temporal horn ratios: Comparison and validation of head ultrasound-derived indexes with MRI and ventricular volumes in infantile ventriculomegaly” [44] | 90 infants < 6 months of age with PHVM 3-year retrospective study | Assessment of FOHR and FTHR obtained from cranial ultrasound as reliable measures of ventriculomegaly in infants | FOHR and FTHR obtained from CUS have excellent inter-observer concordance, are concordant with MRI-derived linear ratios, and correlate with MRI-derived ventricular volumes. US-derived FOHR and FTHR are reliable indexes for clinical follow-up of PHVM. |
| FOHR 0.62 ± 0.12 at surgical consult and 0.75 ± 0.13 at intervention (p < 0.001) | “Degree of ventriculomegaly predicts school-aged functional outcomes in preterm infants with intraventricular hemorrhage” [45] | 134 infants with Grade III/IV IVH (Papile) | NDI for patients with PHVM | Ventriculomegaly measured by FOHR and PVL are independent correlates of school-age functional outcomes in preterm infants with IVH regardless of need for neurosurgical intervention. |
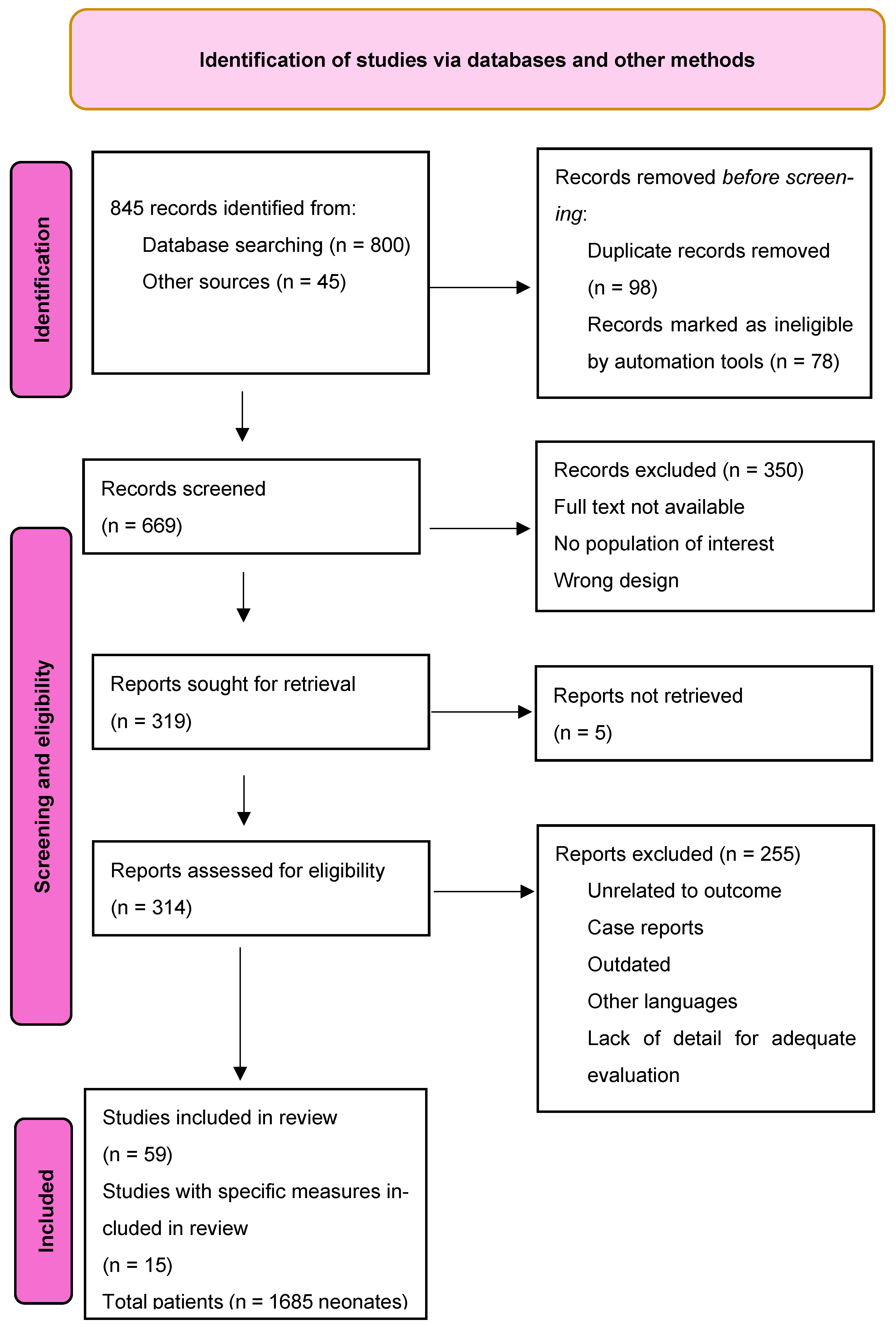
| Longest diagonal diameter of the PHVI Localization, shape, and midline shifting were noted (0–3) | “Periventricular Hemorrhagic Infarction in Very Preterm Infants: Characteristic Sonographic Findings and Association with Neurodevelopmental Outcome at Age 2 Years” [46] | 160 infants with median age 26.6 weeks and IVH grade III associated with PVHI | Mortality Cognitive and gross motor development | Increasing PHVI size and severity score for PHVI according to Bassan criteria are predictive for less optimal gross motor outcome and death. Ventricular dilatation is an independent risk factor for poorer cognitive and motor function. |
| Index/ Ratios | Refference Studies | Advantages | Disadvantages |
|---|---|---|---|
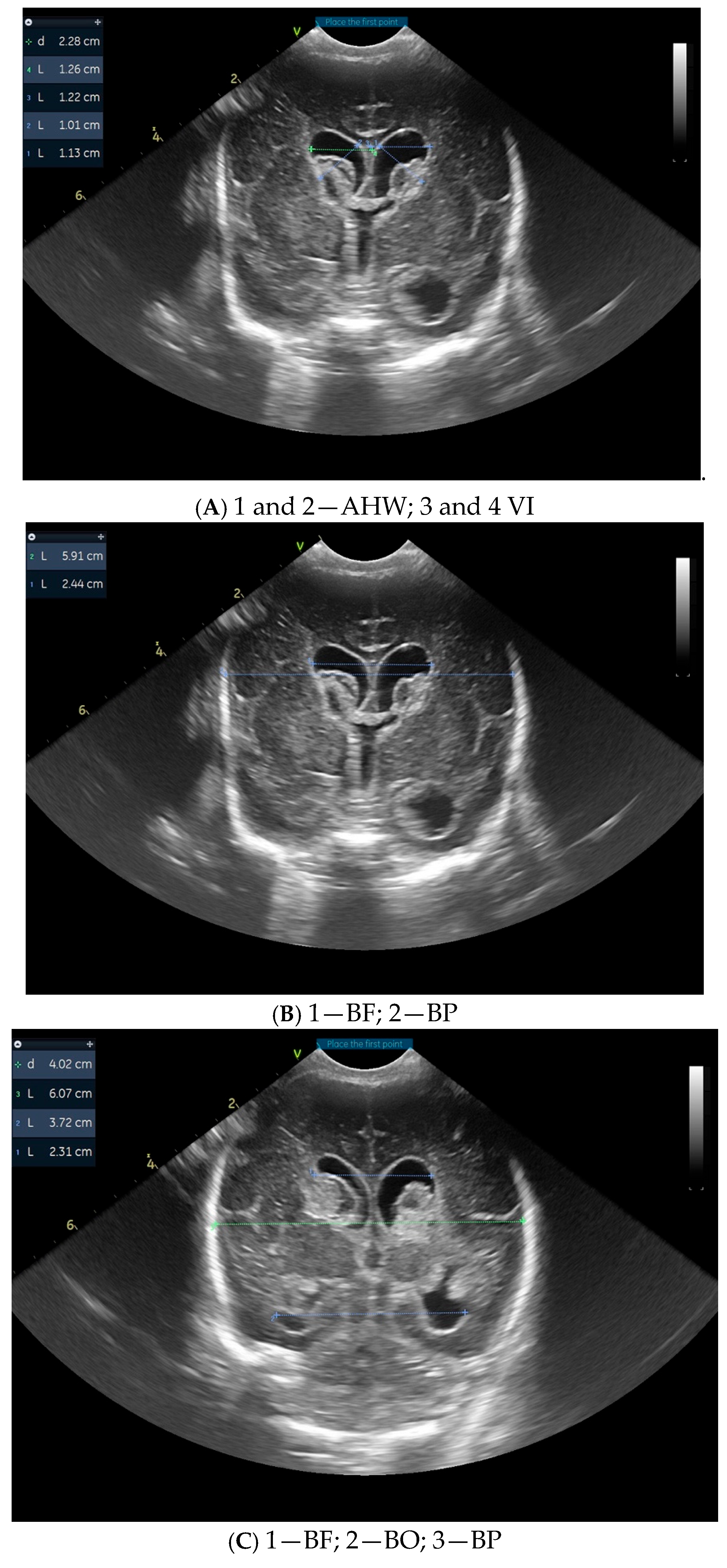
| VI | “Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: A randomised controlled trial” [36] “Ventriculomegaly thresholds for prediction of symptomatic post-hemorrhagic ventricular dilatation in preterm infants” [28] | Most used in all studies [36] Best specificity [28] | Dependent on gestational age [24,54] Restricted to 24–42 weeks post-conceptionally [28] Single-institution data reference [28] Inter-rater variability (use average of both sides) [24] Intraventricular clot or periventricular infarction can make ventricular border less defined [28] |
| AHW | “New reference values for the neonatal cerebral ventricles” [24] “Inclusion of extremes of prematurity in ventricular index centile charts” [54] “Post-hemorrhagic ventricular dilatation: inter-observer reliability of ventricular size measurements in extremely preterm infants” [42] “Timing of Intervention for Posthemorrhagic Ventricular Dilatation: An Ongoing Debate” [20] | Independent of gestational age [24,54] Best inter-rater reliability > than VI, FOHR, and FTHR [42] Better predictor for severe PHVM compared to other indices [55] | In cases of porencephalic cysts contiguous with the ventricle, it may be difficult to measure accurately [28] Intraventricular clot or periventricular infarction can make ventricular border less defined [49] |
| FTHR/FOHR | “Optical Detection of Intracranial Pressure and Perfusion Changes in Neonates with Hydrocephalus” [55] “Fronto-temporal horn ratio: yet another marker of ventriculomegaly?” [49] “Frontal occipital and frontal temporal horn ratios: Comparison and validation of head ultrasound-derived indexes with MRI and ventricular volumes in infantile ventriculomegaly” [44] | Independent of gestational age [24,54] Higher sensitivity compared to VI and AHW [28] Good correlation with ventricular volume measured from MRI [44] Reflects better ventricular size and injury of white matter (subsequently with NDI) [44] | The lateral boundaries of the parietal skull can be obscured, making measurement difficult Not correlated with high intracranial pressure [20,49] Lower inter-rater reliability compared to VI and AHW (requires three measurements) [28] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dan, A.M.; Vasilescu, D.I.; Dragomir, I.; Vasilescu, S.L.; Voicu, D.; Cîrstoiu, M.M. Cranial Ultrasonography—Standards in Diagnosis of Intraventricular Hemorrhage and Ventricular Dilatation in Premature Neonates. Children 2025, 12, 768. https://doi.org/10.3390/children12060768
Dan AM, Vasilescu DI, Dragomir I, Vasilescu SL, Voicu D, Cîrstoiu MM. Cranial Ultrasonography—Standards in Diagnosis of Intraventricular Hemorrhage and Ventricular Dilatation in Premature Neonates. Children. 2025; 12(6):768. https://doi.org/10.3390/children12060768
Chicago/Turabian StyleDan, Adriana Mihaela, Diana Iulia Vasilescu, Ion Dragomir, Sorin Liviu Vasilescu, Diana Voicu, and Monica Mihaela Cîrstoiu. 2025. "Cranial Ultrasonography—Standards in Diagnosis of Intraventricular Hemorrhage and Ventricular Dilatation in Premature Neonates" Children 12, no. 6: 768. https://doi.org/10.3390/children12060768
APA StyleDan, A. M., Vasilescu, D. I., Dragomir, I., Vasilescu, S. L., Voicu, D., & Cîrstoiu, M. M. (2025). Cranial Ultrasonography—Standards in Diagnosis of Intraventricular Hemorrhage and Ventricular Dilatation in Premature Neonates. Children, 12(6), 768. https://doi.org/10.3390/children12060768





