Complications of Reamer–Irrigator–Aspirator System in Pediatric Orthopedic Surgery–Case Series and Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Scoping Review
2.1.1. Search Strategy and Data Management
2.1.2. Study/Source of Evidence Selection
2.1.3. Inclusion and Exclusion Criteria
2.1.4. Types of Sources
2.1.5. Data Charting
2.2. Case Series Search Criteria
2.2.1. Search Criteria
2.2.2. Inclusion and Exclusion Criteria
3. Results
3.1. Case Series Overview
3.2. Case Descriptions
4. Scoping Review and Discussion
4.1. Scoping Review
4.1.1. Clinical Complications
4.1.2. Mechanical Failures
4.2. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| RIA | Reamer–Irrigator–Aspirator |
| JBI | Joanna Briggs Institute |
| MRSA | Methicillin-resistant Staphylococcus aureus |
| AP | Anteroposterior |
| FES | Fat embolism syndrome |
Appendix A
Appendix A.1. MEDLINE (PubMed) Search Strategy
Appendix A.2. COCHRANE Central Search Strategy
Appendix A.3. Embase Search Strategy
References
- Jacobson, E.; Schieve, B.C.; Klahs, K.J.; Macias, R.A.; Abdelgawad, A.; Thabet, A.M. Reamer Irrigator Aspirator (RIA) Reduces Risk of Fat Embolism in Bilateral Pediatric Femur Shaft Fractures: A Case Report. J. Surg. Case Rep. 2024, 2024, rjae042. [Google Scholar] [CrossRef] [PubMed]
- Belthur, M.V.; Conway, J.D.; Jindal, G.; Ranade, A.; Herzenberg, J.E. Bone Graft Harvest Using a New Intramedullary System. Clin. Orthop. Relat. Res. 2008, 466, 2973–2980. [Google Scholar] [CrossRef] [PubMed]
- Sagi, H.C.; Young, M.L.; Gerstenfeld, L.; Einhorn, T.A.; Tornetta, P. Qualitative and Quantitative Differences between Bone Graft Obtained from the intramedullary Canal (with a Reamer/Irrigator/Aspirator) and the Iliac Crest of the Same Patient. J. Bone Jt. Surg. 2012, 94, 2128–2135. [Google Scholar] [CrossRef]
- Dehghan, N.; Schemitsch, E.H. Extended Applications of the Reamer-Irrigator-Aspirator (RIA) System. Injury 2017, 48, S47–S51. [Google Scholar] [CrossRef] [PubMed]
- Billow, D.; Khlopas, A.; Chughtai, M.; Saleh, A.; Siqueira, M.B.; Marinello, P.; Mont, M.A. The Reamer-Irrigator-Aspirator System: A Review. Surg. Technol. Int. 2016, 29, 287–294. [Google Scholar]
- Chloros, G.D.; Giannoudis, V.P.; Kanakaris, N.K.; Giannoudis, P.V. A Technical Note: How to Extract Broken Reamer-Irrigator-Aspirator (RIA) Metal Intramedullary Debris. Injury 2022, 53, 1568–1571. [Google Scholar] [CrossRef]
- Jakma, T.S.C.; Röling, M.A.; Punt, B.; Reynders-Frederix, P. More Adverse Events than Expected in the Outcome after Use of the Reamer-Irrigator-Aspirator. Eur. J. Trauma Emerg. Surg. 2014, 40, 337–341. [Google Scholar] [CrossRef]
- Cox, G.; Jones, E.; McGonagle, D.; Giannoudis, P.V. Reamer-Irrigator-Aspirator Indications and Clinical Results: A Systematic Review. Int. Orthop. (SICOT) 2011, 35, 951–956. [Google Scholar] [CrossRef]
- Higgins, T.F.; Casey, V.; Bachus, K. Cortical Heat Generation Using An Irrigating/Aspirating Single-Pass Reaming vs. Conventional Stepwise Reaming. J. Orthop. Trauma 2007, 21, 192–197. [Google Scholar] [CrossRef]
- Volgas, D.; Burch, T.; Stannard, J.; Ellis, T.; Bilotta, J.; Alonso, J. Fat Embolus in Femur Fractures: A Comparison of Two Reaming Systems. Injury 2010, 41, S90–S93. [Google Scholar] [CrossRef]
- Laubach, M.; Weimer, L.P.; Bläsius, F.M.; Hildebrand, F.; Kobbe, P.; Hutmacher, D.W. Complications Associated Using the Reamer-Irrigator -Aspirator (RIA) System: A Systematic Review and Meta-Analysis. Arch. Orthop. Trauma Surg. 2023, 143, 3823–3843. [Google Scholar] [CrossRef] [PubMed]
- McCann, P.A.; Sarangi, P.P.; Baker, R.P.; Blom, A.W.; Amirfeyz, R. Thermal Damage during Humeral Reaming in Total Shoulder Resurfacing. Int. J. Shoulder Surg. 2013, 7, 100–104. [Google Scholar] [CrossRef]
- Lowe, J.A.; Della Rocca, G.J.; Murtha, Y.; Liporace, F.A.; Stover, M.D.; Nork, S.E.; Crist, B.D. Complications Associated With Negative Pressure Reaming for Harvesting Autologous Bone Graft: A Case Series. J. Orthop. Trauma 2010, 24, 46–52. [Google Scholar] [CrossRef]
- Streubel, P.N.; Desai, P.; Suk, M. Comparison of RIA and Conventional Reamed Nailing for Treatment of Femur Shaft Fractures. Injury 2010, 41 (Suppl. S2), S51–S56. [Google Scholar] [CrossRef] [PubMed]
- Haubruck, P.; Ober, J.; Heller, R.; Miska, M.; Schmidmaier, G.; Tanner, M.C. Complications and Risk Management in the Use of the Reaming-Irrigator-Aspirator (RIA) System: RIA Is a Safe and Reliable Method in Harvesting Autologous Bone Graft. PLoS ONE 2018, 13, e0196051. [Google Scholar] [CrossRef] [PubMed]
- Öhman, C.; Baleani, M.; Pani, C.; Taddei, F.; Alberghini, M.; Viceconti, M.; Manfrini, M. Compressive Behaviour of Child and Adult Cortical Bone. Bone 2011, 49, 769–776. [Google Scholar] [CrossRef]
- Depalle, B.; Duarte, A.G.; Fiedler, I.A.K.; Pujo-Menjouet, L.; Buehler, M.J.; Berteau, J.-P. The Different Distribution of Enzymatic Collagen Cross-Links Found in Adult and Children Bone Result in Different Mechanical Behavior of Collagen. Bone 2018, 110, 107–114. [Google Scholar] [CrossRef]
- Lucak, T.; Raju, S.; Andrews, A.; Igbokwe, L.; Heffernan, M.J. Dimensions of the Paediatric Femur: Anatomical Limitations of Flexible Intramedullary Nailing. J. Child. Orthop. 2019, 13, 220–225. [Google Scholar] [CrossRef]
- Davids, J.R. Rotational Deformity and Remodeling after Fracture of the Femur in Children. Clin. Orthop. Relat. Res. 1994, 302, 27–35. [Google Scholar] [CrossRef]
- Peters, M.D.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Scoping Reviews. In JBI Manual for Evidence Synthesis; Aromataris, E., Lockwood, C., Porritt, K., Pilla, B., Jordan, Z., Eds.; JBI: Adelaide, Australia, 2024; ISBN 978-0-648-84882-0. [Google Scholar]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Dodwell, E.R.; Pathy, R.; Widmann, R.F.; Green, D.W.; Scher, D.M.; Blanco, J.S.; Doyle, S.M.; Daluiski, A.; Sink, E.L. Reliability of the Modified Clavien-Dindo-Sink Complication Classification System in Pediatric Orthopaedic Surgery. JBJS OA 2018, 3, e0020. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.; McKee, M.; Vicente, M.; Morison, Z.; Dehghan, N.; Schemitsch, C.; Kreder, H.; Petrisor, B.; Schemitsch, E. Prospective Randomized Clinical Trial Investigating the Effect of the Reamer-Irrigator-Aspirator on the Volume of Embolic Load and Respiratory Function During Intramedullary Nailing of Femoral Shaft Fractures. J. Orthop. Trauma 2017, 31, 200–204. [Google Scholar] [CrossRef]
- He, Z.; Shi, Z.; Li, C.; Ni, L.; Sun, Y.; Arioli, F.; Wang, Y.; Ammirati, E.; Wang, D.W. Single-Case Metanalysis of Fat Embolism Syndrome. Int. J. Cardiol. 2021, 345, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Desai, P.P.; Bell, A.J.; Suk, M. Treatment of Recalcitrant, Multiply Operated Tibial Nonunions with the RIA Graft and Rh-BMP2 Using Intramedullary Nails. Injury 2010, 41, S69–S71. [Google Scholar] [CrossRef]
- Giori, N.J.; Beaupre, G.S. Femoral Fracture After Harvesting of Autologous Bone Graft Using a Reamer/Irrigator/Aspirator. J. Orthop. Trauma 2011, 25, e12–e14. [Google Scholar] [CrossRef]
- Dawson, J.; Kiner, D.; Gardner, W.; Swafford, R.; Nowotarski, P. The Reamer-Irrigator-Aspirator as a Device for Harvesting Bone Graft Compared with Iliac Crest Bone Graft: Union Rates and Complications. J. Orthop. Trauma 2014, 28, 584–590. [Google Scholar] [CrossRef]
- Marchand, L.S.; Rothberg, D.L.; Kubiak, E.N.; Higgins, T.F. Is This Autograft Worth It?: The Blood Loss and Transfusion Rates Associated With Reamer Irrigator Aspirator Bone Graft Harvest. J. Orthop. Trauma 2017, 31, 205–209. [Google Scholar] [CrossRef]
- Waterman, B.; Davey, S.; Kanlic, E.; Abdelgawad, A. Intramedullary Bone Graft Harvest Using Reamer-Irrigator-Aspirator System: A Case Series. J. Surg. Orthop. Adv. 2017, 26, 233–238. [Google Scholar]
- Davis, R.; Taylor, B.; Johnson, N.; Ferrel, J.; Castaneda, J. Retrograde Versus Antegrade Femoral Bone Graft Harvesting Using the Reamer-Irrigator-Aspirator. J. Orthop. Trauma 2015, 29, 370–372. [Google Scholar] [CrossRef]
- Pediatric Musculoskeletal Infections: Principles & Practice; Belthur, M.V., Ranade, A.S., Herman, M.J., Fernandes, J.A., Eds.; Springer International Publishing: Cham, Switzerland, 2022; ISBN 978-3-030-95793-3. [Google Scholar]
- Cipriano, C.A.; Arvanitis, L.D.; Virkus, W.W. Use of the Reamer–Irrigator–Aspirator May Reduce Tumor Dissemination During Intramedullary Fixation of Malignancies. Orthopedics 2012, 35, e48–e52. [Google Scholar] [CrossRef] [PubMed]
- Eisenstein, E.D.; Waterman, B.R.; Kanlic, E.M.; Abdelgawad, A.A. A New Technique for Obtaining Bone Graft in Cases of Distal Femur Nonunion: Passing a Reamer/Irrigator/Aspirator Retrograde Through the Nonunion Site. Am. J. Orthop. 2016, 45, E493–E496. [Google Scholar] [PubMed]
- Tupis, T.M.; Altman, G.T.; Altman, D.T.; Cook, H.A.; Miller, M.C. Femoral Bone Strains during Antegrade Nailing: A Comparison of Two Entry Points with Identical Nails Using Finite Element Analysis. Clin. Biomech. 2012, 27, 354–359. [Google Scholar] [CrossRef] [PubMed]
- MacNeil, J.A.M.; Francis, A.; El-Hawary, R. A Systematic Review of Rigid, Locked, Intramedullary Nail Insertion Sites and Avascular Necrosis of the Femoral Head in the Skeletally Immature. J. Pediatr. Orthop. 2011, 31, 377–380. [Google Scholar] [CrossRef]
- Park, P.J.; Weinberg, D.S.; Petro, K.F.; Liu, R.W. An Anatomic Study of the Greater Trochanter Starting Point for Intramedullary Nailing in the Skeletally Immature. J. Pediatr. Orthop. 2017, 37, 67–73. [Google Scholar] [CrossRef]


| Patient Characteristics | |||||||
|---|---|---|---|---|---|---|---|
| Case | Age | Sex | BMI | Prior Orthopedic Conditions | Medical PMH | Prior Orthopedic Surgeries | Surgical Indication |
| 1 | 12 | M | 15.63 | Congenital left femoral limb length discrepancy, contralateral genu valgum, left femoral cortex nonunion | Asthma | 5 cm left femoral lengthening with IM magnetic nail, distal medial femur physeal tethering | Nonunion |
| 2 | 13 | F | 21.47 | Chronic MRSA osteomyelitis of the left proximal tibial metaphysis, subperiosteal abscess | None | None | Osteomyelitis |
| 3 | 14 | M | 14.95 | Chronic multifocal (autoimmune) osteomyelitis, subperiosteal abscess, Brodie’s abscess | Disease-modifying rheumatologics | Brodie’s abscess, right femur I&D, subperiosteal abscess biopsy, right femoral IM antibiotic nail | Retained hardware |
| 4 | 8 | M | 28.14 | Traumatic fracture of the left femoral diaphysis | None | ORIF with flexible nails 8 months prior with I&D, tenodesis of the semitendinosus | Nonunion |
| Surgical Parameters | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Bone | Side | RIA Procedure | Ipselateral Deformity | Entry Point | Guide Pin | Medulla Width | Pre-Ream Size | RIA Size | Aspiration | Irrigation | Aspirate Volume |
| 1 | Femur | R | Bone harvest for nonunion | None | Greater trochanter | Yes | 10 mm | 8.5 mm | 10.5 mm | Continuous | Continuous | 20 cc |
| 2 | Tibia | L | Irrigation and debridement | None | Lateral tibial spine | Yes | 10 mm | 10.5 mm | 10.5 mm | Continuous | Continuous | N/A |
| 3 | Femur | R | Irrigation and debridement | None | Greater trochanter | No | 14 mm | 12 mm | 10.5 mm | Continuous | Continuous | N/A |
| 4 | Femur | L | Bone harvest for nonunion | Nonunion | Greater trochanter | Yes | 14.1 mm | 10 mm | 10.5 mm | Continuous | Continuous | 15 cc |
| Complication Description and Outcomes | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Case | Complication | Time | Diagnostic Modality | Severity | Management | Outcome | Follow-Up | Complication Resolution | Corrective Procedure |
| 1 | Retained hardware, 5 flanges | Intraop | Fluoroscopy | Grade I | Removal of 3 pieces with a curette | No long-term sequelae | 535 days | No | None |
| 2 | Retained hardware, 4 flanges | Intraop | Fluoroscopy | Grade I | Removal of 1 piece with pituitary rongeur | No long-term sequelae | 248 days | No | None |
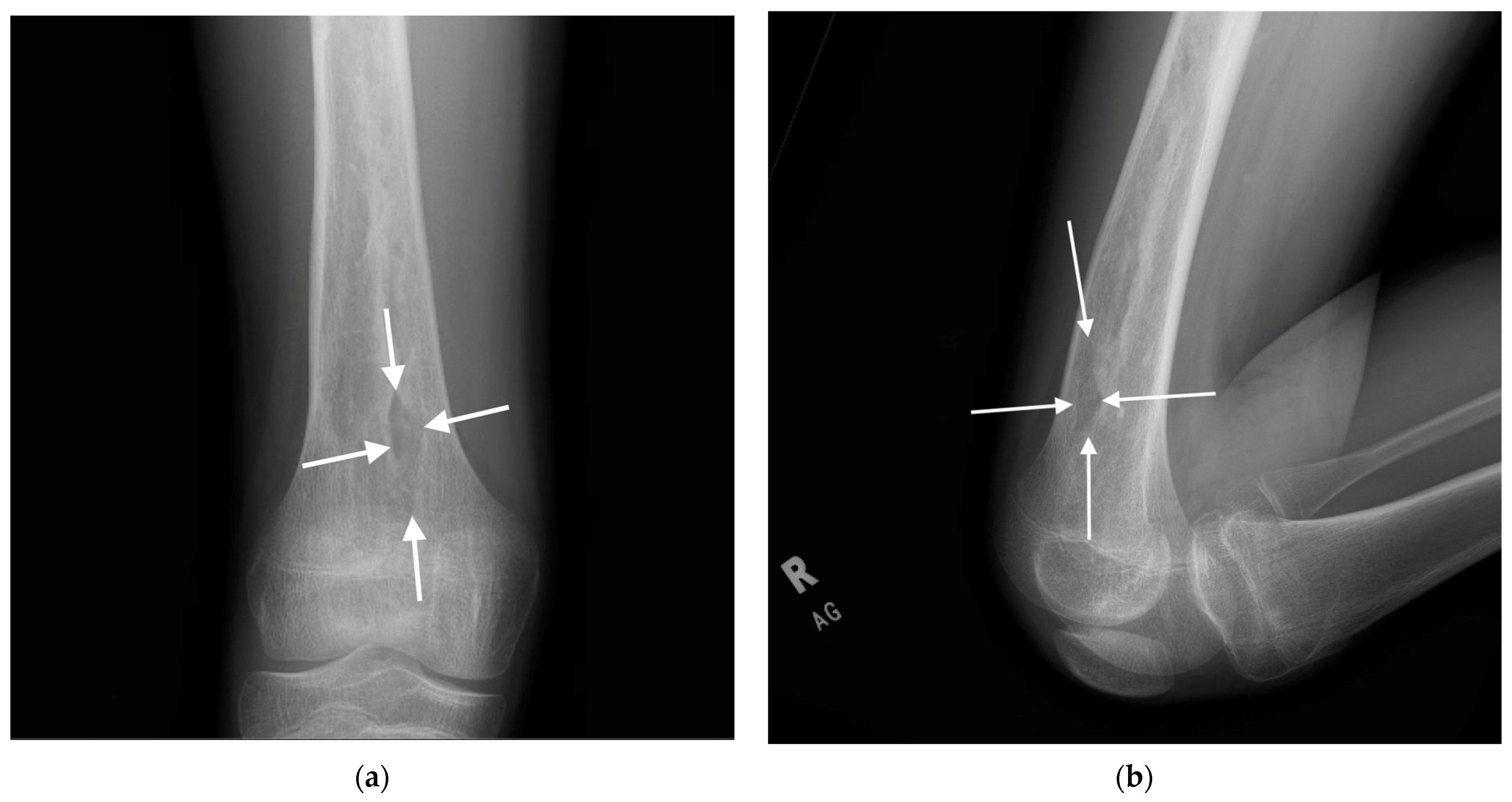
| 3 | Anterior cortical breach | Intraop | Fluoroscopy | Grade I | Nothing | No long-term sequelae | 670 days | No | None |
| 4 | Retained hardware, metal debris | Intraop | Fluoroscopy | Grade I | Nothing | No long-term sequelae | 123 days | No | None |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stickels, M.W.; Roh, K.M.; Belthur, M.; Belthur, M.V. Complications of Reamer–Irrigator–Aspirator System in Pediatric Orthopedic Surgery–Case Series and Scoping Review. Children 2025, 12, 700. https://doi.org/10.3390/children12060700
Stickels MW, Roh KM, Belthur M, Belthur MV. Complications of Reamer–Irrigator–Aspirator System in Pediatric Orthopedic Surgery–Case Series and Scoping Review. Children. 2025; 12(6):700. https://doi.org/10.3390/children12060700
Chicago/Turabian StyleStickels, Michael William, Kyung Min Roh, Meghana Belthur, and Mohan V. Belthur. 2025. "Complications of Reamer–Irrigator–Aspirator System in Pediatric Orthopedic Surgery–Case Series and Scoping Review" Children 12, no. 6: 700. https://doi.org/10.3390/children12060700
APA StyleStickels, M. W., Roh, K. M., Belthur, M., & Belthur, M. V. (2025). Complications of Reamer–Irrigator–Aspirator System in Pediatric Orthopedic Surgery–Case Series and Scoping Review. Children, 12(6), 700. https://doi.org/10.3390/children12060700






