Sagittal Spinal Alignment in Children and Adolescents: Associations with Age, Weight Status, and Sports Participation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population
2.3. Measurements
- A.
- Nutritional Assessment
- Underweight: Below the 5th percentile;
- Normal weight: 5th–84.9th percentile;
- Overweight: 85th–94.9th percentile;
- Obese: Above the 95th percentile.
- B.
- Spine Evaluation
- The physician identified the C7 spinous process by palpating the cervical spine in a neutral position.
- Localization of C7 was confirmed using the flexion–extension test.
- The S2 spinous process was identified as the midpoint between the left and right posterior superior iliac spines (PSISs).
- The plumb line technique was used:
- o
- A plumb line was stabilized against the patient’s parietal bone, ensuring alignment with the PSIS midpoint.
- o
- The distance between the plumb line and the reference points was measured using a rigid ruler.
- o
- The final SI was obtained by subtracting the S2 plumb line distance (PD) from the C7 PD.
- A positive SI value indicated a posterior displacement of C7 relative to S2, while a negative value indicated an anterior displacement.
- Children aged ≥ 9 years: SI > 95 mm (risk of hyperkyphosis);
- Children aged < 9 years: SI > 65 mm (risk of hyperkyphosis).
- C.
- Sports Participation
- 0
- No sport (sedentary);
- 1
- Skill-based sports (e.g., gymnastics, dance);
- 2
- Power sports (e.g., weightlifting, wrestling);
- 3
- Mixed sports (e.g., soccer, basketball);
- 4
- Endurance sports (e.g., long-distance running, swimming).
2.4. Statistical Analysis
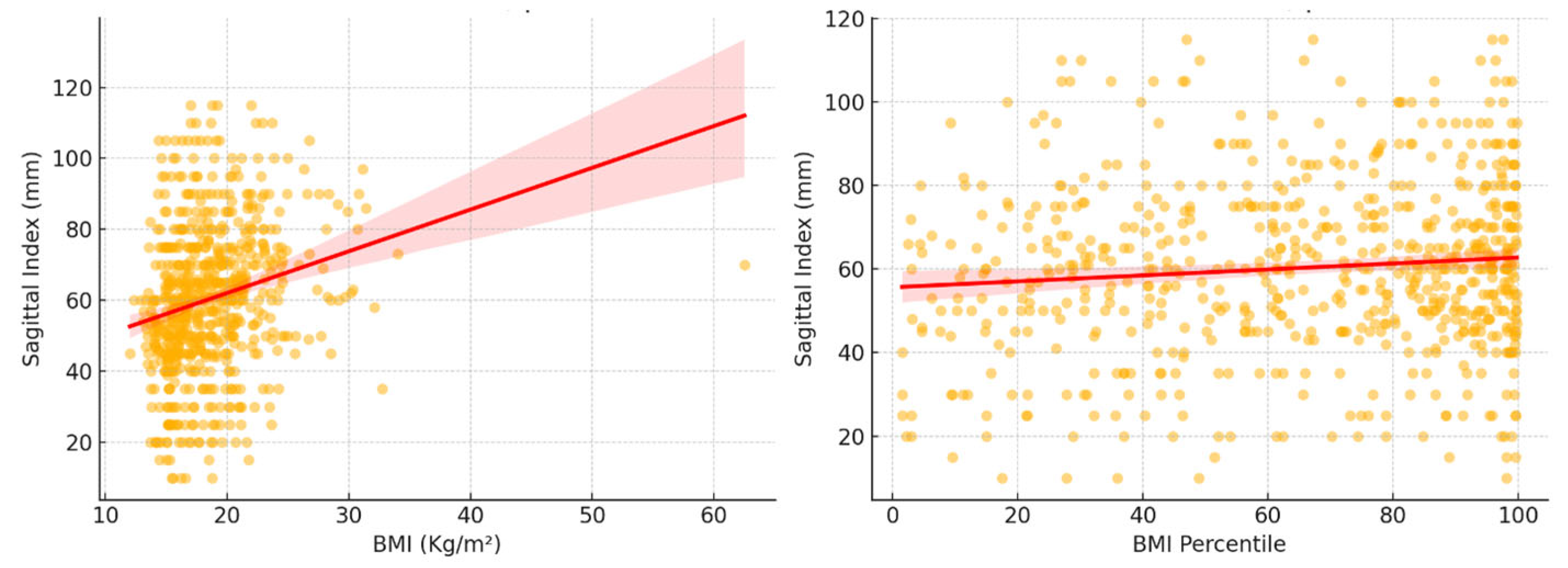
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SI | Sagittal Index |
| BMI | Body mass index |
References
- Yang, L.; Lu, X.; Yan, B.; Huang, Y. Prevalence of Incorrect Posture among Children and Adolescents: Finding from a Large Population-Based Study in China. iScience 2020, 23, 101043. [Google Scholar] [CrossRef] [PubMed]
- Lubkowska, W.; Mroczek, B. Assessment of body posture of boys aged 7–15 in relation to the body mass index—BMI. J. Educ. Health Sport 2017, 7, 371–380. [Google Scholar]
- Saunders, T.J.; Chaput, J.-P.; Tremblay, M.S. Sedentary Behaviour as an Emerging Risk Factor for Cardiometabolic Diseases in Children and Youth. Can. J. Diabetes 2014, 38, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Maciałczyk-Paprocka, K.; Stawińska-Witoszyńska, B.; Kotwicki, T.; Sowińska, A.; Krzyżaniak, A.; Walkowiak, J.; Krzywińska-Wiewiorowska, M. Prevalence of incorrect body posture in children and adolescents with overweight and obesity. Eur. J. Pediatr. 2017, 176, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Annarumma, G.; Spinelli, A.; Serio, A.; Di Fraia, T.; Gallinoro, C.M.; Caoduro, L.; Sirico, F. Forward head posture and neck disability: What is the effect on lung function? Explor. Med. 2023, 4, 207–214. [Google Scholar] [CrossRef]
- Grabara, M.; Witkowska, A. Sagittal spinal curvatures of young adults in the context of their self-reported physical activity and somatic parameters. Sci. Rep. 2024, 14, 12221. [Google Scholar] [CrossRef]
- Jankowicz-Szymańska, A.; Bibro, M.; Wódka, K.; Smola, E. Does excessive body weight change the shape of the spine in children? Child. Obes. 2019, 15, 346–352. [Google Scholar] [CrossRef]
- Palermi, S.; Vecchiato, M.; Pennella, S.; Marasca, A.; Spinelli, A.; De Luca, M.; De Martino, L.; Fernando, F.; Sirico, F.; Biffi, A. The Impact of the COVID-19 Pandemic on Childhood Obesity and Lifestyle—A Report from Italy. Pediatr. Rep. 2022, 14, 410–418. [Google Scholar] [CrossRef]
- Vandoni, M.; Marin, L.; Cavallo, C.; Gatti, A.; Grazi, R.; Albanese, I.; Taranto, S.; Silvestri, D.; Di Carlo, E.; Patanè, P.; et al. Poor Motor Competence Affects Functional Capacities and Healthcare in Children and Adolescents with Obesity. Sports 2024, 12, 44. [Google Scholar] [CrossRef]
- Vecchiato, M.; Quinto, G.; Palermi, S.; Foccardi, G.; Mazzucato, B.; Battista, F.; Duregon, F.; Michieletto, F.; Neunhaeuserer, D.; Ermolao, A. Are Gyms a Feasible Setting for Exercise Training Interventions in Patients with Cardiovascular Risk Factors? An Italian 10-Years Cross-Sectional Survey Comparison. Int. J. Environ. Res. Public Health 2022, 19, 2407. [Google Scholar] [CrossRef]
- Bhati, P.; Cheung, T.C.; Sithamparanathan, G.; Schmuckler, M.A. Striking a balance in sports: The interrelation between children’s sports experience, body size, and posture. AIMS Neurosci. 2022, 9, 288. [Google Scholar] [CrossRef] [PubMed]
- Zeppilli, P.; Biffi, A.; Cammarano, M.; Castelletti, S.; Cavarretta, E.; Cecchi, F.; Colivicchi, F.; Contursi, M.; Corrado, D.; D’andrea, A.; et al. Italian Cardiological Guidelines (COCIS) for Competitive Sport Eligibility in athletes with heart disease: Update 2024. Minerva Medica 2024, 115, 533–564. [Google Scholar] [CrossRef] [PubMed]
- Palermi, S.; Annarumma, G.; Spinelli, A.; Massa, B.; Serio, A.; Vecchiato, M.; Demeco, A.; Brugin, E.; Sirico, F.; Giada, F.; et al. Acceptability and Practicality of a Quick Musculoskeletal Examination into Sports Medicine Pre-Participation Evaluation. Pediatr. Rep. 2022, 14, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Iwaniec, U.T.; Turner, R.T. Influence of body weight on bone mass, architecture and turnover. J. Endocrinol. 2016, 230, R115–R130. [Google Scholar] [CrossRef]
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut Off Points; StatPearls: St. Petersburg, FL, USA, 2025. [Google Scholar]
- Negrini, A.; Vanossi, M.; Donzelli, S.; Zaina, F.; Romano, M.; Negrini, S. Spinal Coronal and Sagittal Balance in 584 Healthy Individuals During Growth: Normal Plumb Line Values and Their Correlation with Radiographic Measurements. Phys. Ther. 2019, 99, 1712–1718. [Google Scholar] [CrossRef]
- Palermi, S.; Sirico, F.; Fernando, F.; Gregori, G.; Belviso, I.; Ricci, F.; D’ascenzi, F.; Cavarretta, E.; De Luca, M.; Negro, F.; et al. Limited diagnostic value of questionnaire-based pre-participation screening algorithms: A “risk-exposed” approach to sports activity. J. Basic Clin. Physiol. Pharmacol. 2022, 33, 655–663. [Google Scholar] [CrossRef]
- Ambrosio, L.; Mazzuca, G.; Maguolo, A.; Russo, F.; Cannata, F.; Vadalà, G.; Maffeis, C.; Papalia, R.; Denaro, V. The burden of low back pain in children and adolescents with overweight and obesity: From pathophysiology to prevention and treatment strategies. Ther. Adv. Musculoskelet. Dis. 2023, 15, 1759720X231188831. [Google Scholar] [CrossRef]
- Calcaterra, V.; Marin, L.; Vandoni, M.; Rossi, V.; Pirazzi, A.; Grazi, R.; Patané, P.; Silvestro, G.S.; Pellino, V.C.; Albanese, I.; et al. Childhood Obesity and Incorrect Body Posture: Impact on Physical Activity and the Therapeutic Role of Exercise. Int. J. Environ. Res. Public Health 2022, 19, 16728. [Google Scholar] [CrossRef]
- Molina-Garcia, P.; Plaza-Florido, A.; Mora-Gonzalez, J.; Torres-Lopez, L.V.; Vanrenterghem, J.; Ortega, F.B. Role of physical fitness and functional movement in the body posture of children with overweight/obesity. Gait Posture 2020, 80, 331–338. [Google Scholar] [CrossRef]
- Mac-Thiong, J.-M.; Labelle, H.; Berthonnaud, E.; Betz, R.R.; Roussouly, P. Sagittal spinopelvic balance in normal children and adolescents. Eur. Spine J. 2005, 16, 227–234. [Google Scholar] [CrossRef]
- Poussa, M.S.; Heliövaara, M.M.; Seitsamo, J.T.; Könönen, M.H.; Hurmerinta, K.A.; Nissinen, M.J. Development of spinal posture in a cohort of children from the age of 11 to 22 years. Eur. Spine J. 2005, 14, 738–742. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, J.; Stuart, E.; Rodenberg, R. Musculoskeletal Low Back Pain in School-aged Children. JAMA Pediatr. 2017, 171, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J. Cervical spine anomalies in children and adolescents. Curr. Opin. Pediatr. 2013, 25, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Aghi, A.; Salvagnini, D.; Berton, G.; Cecconi, M.; Della Valle, E.; Spera, R.; Mambelli, M.; Palermi, S.; Neunhaeuserer, D.; Vecchiato, M. Selective Functional Movement Assessment (SFMA) Reliability and Proposal of Its Use in Sports. Int. J. Environ. Res. Public Health 2023, 20, 2032. [Google Scholar] [CrossRef]
- Barrio, E.D.; Ramirez-Campillo, R.; Serrano, A.G.d.A.; RaquelHernandez-García, R. Effects of core training on dynamic balance stability: A systematic review and meta-analysis. J. Sports Sci. 2022, 40, 1815–1823. [Google Scholar] [CrossRef]
- Hsu, S.-L.; Oda, H.; Shirahata, S.; Watanabe, M.; Sasaki, M. Effects of core strength training on core stability. J. Phys. Ther. Sci. 2018, 30, 1014–1018. [Google Scholar] [CrossRef]
- Katzman, W.B.; Vittinghoff, E.; Lin, F.; Schafer, A.; Long, R.K.; Wong, S.; Lane, N.E. Targeted spine strengthening exercise and posture training program to reduce hy-perkyphosis in older adults: Results from the study of hyperkyphosis, exercise, and function (SHEAF) randomized controlled trial. Osteoporos. Int. 2017, 28, 2831. [Google Scholar] [CrossRef]
- González-Gálvez, N.; Gea-García, G.M.; Marcos-Pardo, P.J. Effects of exercise programs on kyphosis and lordosis angle: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0216180. [Google Scholar] [CrossRef]

| Age (years) | 9.42 ± 2.84 |
| Gender (females) | 349 (50.0%) |
| Weight (Kg) | 36.91 ± 15.45 |
| Height (cm) | 138.01 ± 17.28 |
| BMI (Kg/cm2) | 18.55 ± 3.93 |
| BMI percentile | 66.17 ± 28.80 |
| Category | Group | SI | p-Value | Effect Size |
|---|---|---|---|---|
| Sex | Male | 61.0 ± 21.0 | 0.398 | Cohen’s d = 0.06 |
| Female | 59.7 ± 20.2 | |||
| BMI | Normal weight | 59.9 ± 21.0 | 0.407 | Cohen’s d = 0.06 |
| Overweight + obese | 61.2 ± 19.8 | |||
| Sport | Active | 60.3 ± 20.8 | 0.794 | Cohen’s d = 0.02 |
| Non-active | 60.8 ± 19.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Annarumma, G.; Mazza, F.; Ambrosi, A.; Keeling, E.; Fernando, F.; Sirico, F.; Gnasso, R.; Demeco, A.; Vecchiato, M.; Motti, M.L.; et al. Sagittal Spinal Alignment in Children and Adolescents: Associations with Age, Weight Status, and Sports Participation. Children 2025, 12, 659. https://doi.org/10.3390/children12050659
Annarumma G, Mazza F, Ambrosi A, Keeling E, Fernando F, Sirico F, Gnasso R, Demeco A, Vecchiato M, Motti ML, et al. Sagittal Spinal Alignment in Children and Adolescents: Associations with Age, Weight Status, and Sports Participation. Children. 2025; 12(5):659. https://doi.org/10.3390/children12050659
Chicago/Turabian StyleAnnarumma, Giada, Fiore Mazza, Alessandro Ambrosi, Erica Keeling, Fredrick Fernando, Felice Sirico, Rossana Gnasso, Andrea Demeco, Marco Vecchiato, Maria Letizia Motti, and et al. 2025. "Sagittal Spinal Alignment in Children and Adolescents: Associations with Age, Weight Status, and Sports Participation" Children 12, no. 5: 659. https://doi.org/10.3390/children12050659
APA StyleAnnarumma, G., Mazza, F., Ambrosi, A., Keeling, E., Fernando, F., Sirico, F., Gnasso, R., Demeco, A., Vecchiato, M., Motti, M. L., Biffi, A., & Palermi, S. (2025). Sagittal Spinal Alignment in Children and Adolescents: Associations with Age, Weight Status, and Sports Participation. Children, 12(5), 659. https://doi.org/10.3390/children12050659










