Tibial Eminence Avulsion Fracture in Pediatric Patients Reinserted with Arthroscopy and Pull-Out Suture Technique: Clinical and Functional Outcomes in a Long-Term Follow Up with Return to Sport
Abstract
1. Introduction
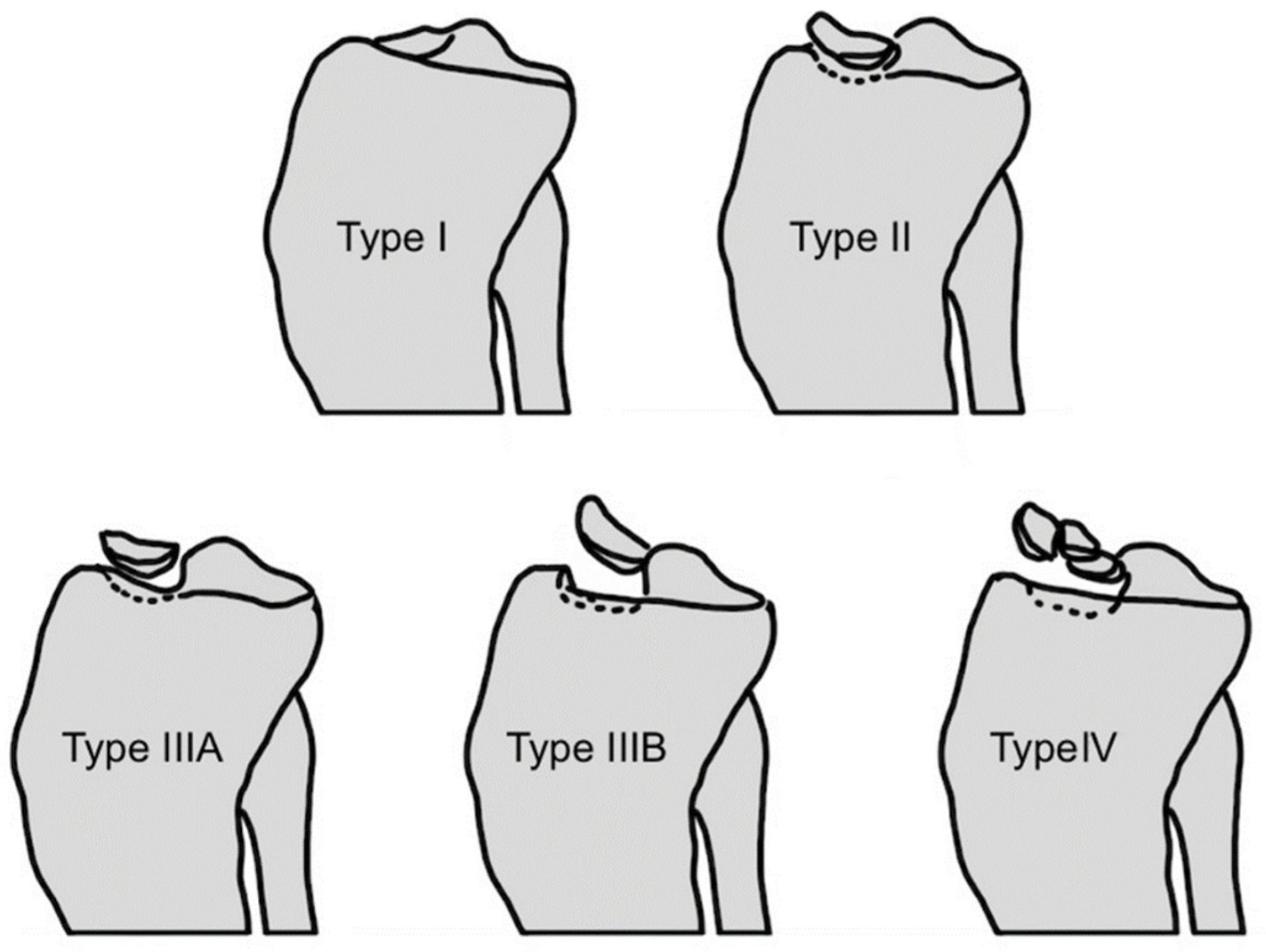
1.1. Background and Rationale
1.2. Aims
2. Materials and Methods
2.1. Study Design
2.2. Participants and Setting
2.3. Source Data and Quantitative Variables
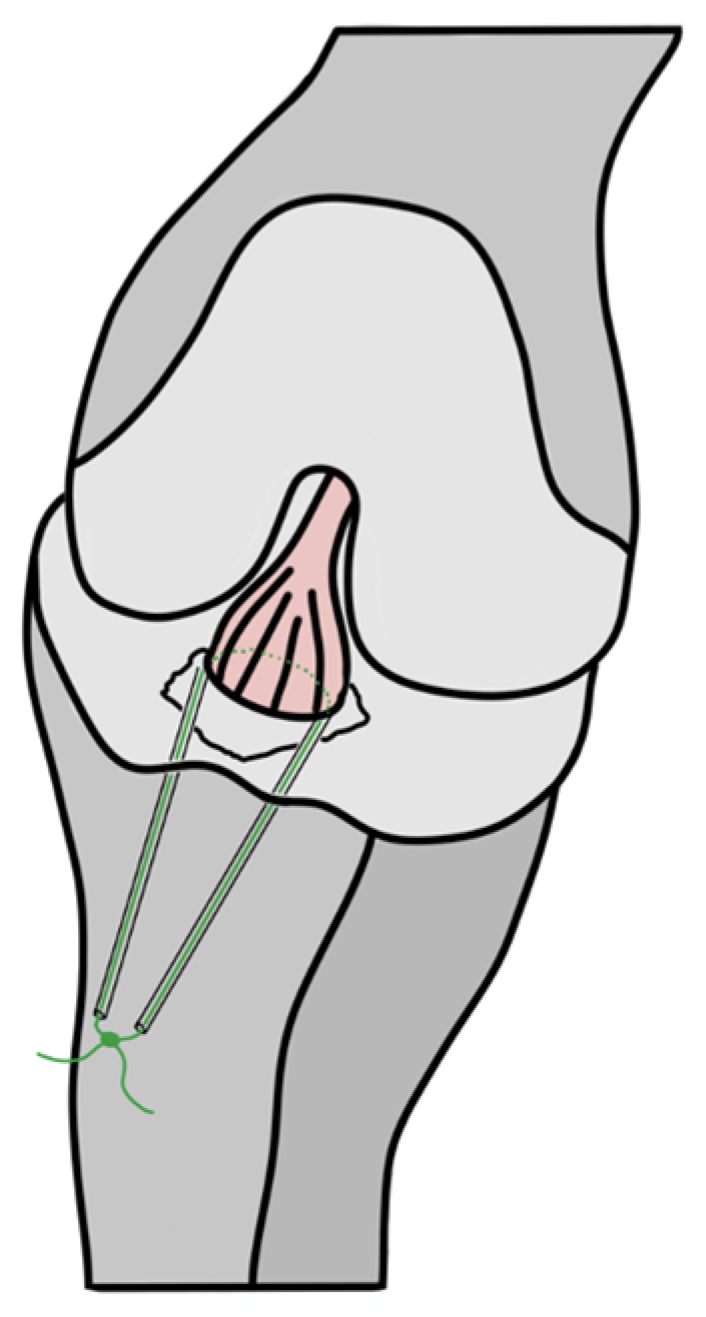
2.4. Description of Used Surgical Pull-Out Suture Technique
2.5. Statistical Method
3. Results
3.1. Participants
3.2. Descriptive Data
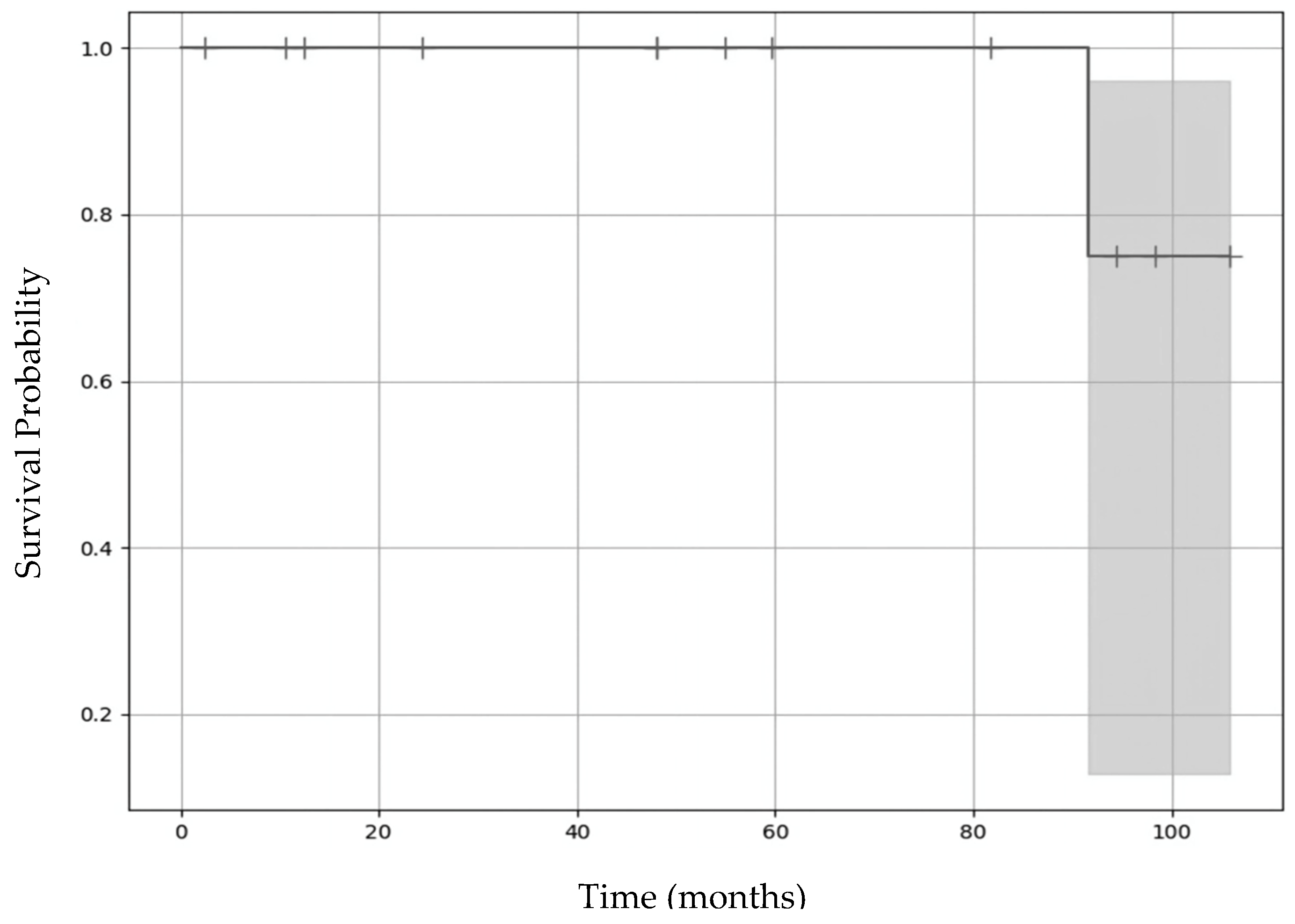
3.3. Primary Outcomes
3.4. Secondary Outcomes
4. Discussion
4.1. Long-Term Function and Objective Anterior Stability of the Knee Joint
4.2. Long-Term Functional Subjective Outcomes of Surgically Treated Patients with Displaced TEAF in Terms of Patient-Reported Outcomes (PROMs) and Return to Sport
4.3. Reoperation
4.4. Perspectives and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tercier, S.; Zambelli, P.-Y. Lésions Du Ligament Croisé Antérieur de l’enfant. Rev. Med. Suisse 2013, 9, 1408–1413. [Google Scholar] [CrossRef] [PubMed]
- DeFrancesco, C.J.; Tananbaum, A.; LeBrun, D.G.; Fabricant, P.D. The Incidence of Pediatric Tibial Spine Fractures Is Greater and Peaks Later in Male Patients. Arthrosc. Sports Med. Rehabil. 2022, 4, e639–e643. [Google Scholar] [CrossRef] [PubMed]
- Hunter, R.E.; Willis, J.A. Arthroscopic Fixation of Avulsion Fractures of the Tibial Eminence: Technique and Outcome. Arthrosc. J. Arthrosc. Relat. Surg. 2004, 20, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Meyers, M.H.; McKeever, F.M. Fracture of the Intercondylar Eminence of the Tibia. J. Bone Jt. Surg. 1959, 41, 209–222. [Google Scholar] [CrossRef]
- Zaricznyj, B. Avulsion Fracture of the Tibial Eminence: Treatment by Open Reduction and Pinning. J. Bone Jt. Surg. 1977, 59, 1111–1114. [Google Scholar] [CrossRef]
- Bogunovic, L.; Tarabichi, M.; Harris, D.; Wright, R. Treatment of Tibial Eminence Fractures: A Systematic Review. J. Knee Surg. 2014, 28, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.; Talathi, N.; Gandhi, J.; Patel, N.; Ganley, T. Tibial Spine Fractures in Children: Evaluation, Management, and Future Directions. J. Knee Surg. 2018, 31, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Stallone, S.; Selleri, F.; Trisolino, G.; Grassi, A.; Macchiarola, L.; Magnani, M.; Olivotto, E.; Zaffagnini, S.; Stilli, S.; Catani, F. Good Subjective Outcomes, Stable Knee and High Return to Sport after Tibial Eminence Avulsion Fracture in Children. Children 2020, 7, 173. [Google Scholar] [CrossRef] [PubMed]
- Ganko, A.; Engebretsen, L.; Ozer, H. The Rolimeter: A New Arthrometer Compared with the KT-1000. Knee Surg. Sports Traumatol. Arthrosc. 2000, 8, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Marcheggiani Muccioli, G.M.; Signorelli, C.; Grassi, A.; Sarsina, T.R.D.; Raggi, F.; Carbone, G.; Macchiarola, L.; Vaccari, V.; Zaffagnini, S. In-Vivo Pivot-Shift Test Measured with Inertial Sensors Correlates with the IKDC Grade. J. ISAKOS Jt. Disord. Orthop. Sports Med. 2018, 3, 89–93. [Google Scholar] [CrossRef]
- Fabricant, P.D.; Tepolt, F.A.; Kocher, M.S. Range of Motion Improvement Following Surgical Management of Knee Arthrofibrosis in Children and Adolescents. J. Pediatr. Orthop. 2018, 38, e495–e500. [Google Scholar] [CrossRef] [PubMed]
- Anderson, A.F.; Irrgang, J.J.; Kocher, M.S.; Mann, B.J.; Harrast, J.J. Members of the International Knee Documentation Committee The International Knee Documentation Committee Subjective Knee Evaluation Form: Normative Data. Am. J. Sports Med. 2006, 34, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Kocher, M.S.; Smith, J.T.; Iversen, M.D.; Brustowicz, K.; Ogunwole, O.; Andersen, J.; Yoo, W.J.; McFeely, E.D.; Anderson, A.F.; Zurakowski, D. Reliability, Validity, and Responsiveness of a Modified International Knee Documentation Committee Subjective Knee Form (Pedi-IKDC) in Children With Knee Disorders. Am. J. Sports Med. 2011, 39, 933–939. [Google Scholar] [CrossRef] [PubMed]
- Shirazi, C.P.; Israel, H.A.; Kaar, S.G. Is the Marx Activity Scale Reliable in Patients Younger Than 18 Years? Sports Health Multidiscip. Approach 2016, 8, 145–148. [Google Scholar] [CrossRef] [PubMed]
- Kocher, M.S.; Micheli, L.J.; Gerbino, P.; Hresko, M.T. Tibial Eminence Fractures in Children: Prevalence of Meniscal Entrapment. Am. J. Sports Med. 2003, 31, 404–407. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-M.; Kim, S.-J.; Yang, J.-Y.; Kim, K.-C. Pullout Reattachment of Tibial Avulsion Fractures of the Anterior Cruciate Ligament: A Firm, Effective Suture-Tying Method Using a Tensioner. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 847–850. [Google Scholar] [CrossRef] [PubMed]
- Gans, I.; Baldwin, K.D.; Ganley, T.J. Treatment and Management Outcomes of Tibial Eminence Fractures in Pediatric Patients: A Systematic Review. Am. J. Sports Med. 2014, 42, 1743–1750. [Google Scholar] [CrossRef] [PubMed]
- Coyle, C.; Jagernauth, S.; Ramachandran, M. Tibial Eminence Fractures in the Paediatric Population: A Systematic Review. J. Child. Orthop. 2014, 8, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Casalonga, A.; Bourelle, S.; Chalencon, F.; De Oliviera, L.; Gautheron, V.; Cottalorda, J. Tibial Intercondylar Eminence Fractures in Children: The Long-Term Perspective. Orthop. Traumatol. Surg. Res. 2010, 96, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Aderinto, J.; Walmsley, P.; Keating, J.F. Fractures of the Tibial Spine: Epidemiology and Outcome. Knee 2008, 15, 164–167. [Google Scholar] [CrossRef] [PubMed]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
| <16 years of age at the time of the accident | Not signed ICF or unwilling to participate |
| Open growth line with displaced TEAF | Multiple ligament or cartilage damages |
| TEAF type II to IV requiring surgical treatment | TEAF type I or II with conservative treatment |
| Pre- and post-radiological images | Fracture of the tibial plateau with osteosynthesis |
| Identical surgical technique: reduction with arthroscopy and fixation with pull-out suture | Other surgical technique or fixation method: arthrotomy or fixation with pins or screws |
| Neuromuscular disease | |
| Intra-substantial tear of the ACL |
| Parameter | Value |
|---|---|
| Sex | |
| Male | 60 |
| Female | 40 |
| Side | |
| Right | 40 |
| Left | 60 |
| Fracture type according to Meyer–McKeever | |
| II | 6.67 |
| III | 93.33 |
| Pre-operative additional imaging to radiographs | |
| MRI | 46.67 |
| CT scan | 33.33 |
| No | 20 |
| Injury mechanisme | |
| Ski | 53.33 |
| Running | 20 |
| Football | 6.67 |
| Bike | 6.67 |
| Gym | 6.67 |
| Motorbike | 6.67 |
| Parameter | Operated Knee | Non-Operated Knee | p-Value |
|---|---|---|---|
| Thigh circumference (cm) | 43.6 ± 2.1 | 43.8 ± 2 | 0.57 |
| Calf circumference (cm) | 33 ± 2.1 | 33.5 ± 2.1 | 0.19 |
| Knee flexion (degrees) | 137.7 ± 3 | 139.1 ± 3 | 0.34 |
| Knee extension (degrees) | 4.6 ± 1.3 | 4.8 ± 1.2 | 0.90 |
| Lachman (cm) | 0 ± 0 | 0.2 ± 0.2 | 0.34 |
| Rolimeter (mm) | 5.4 ± 0.5 | 5.4 ± 0.7 | 1 |
| Sport Activity | Last Follow-Up | Pre-Operative | p-Value |
|---|---|---|---|
| Hours/week | 2.92 ± 0.08 | 3.0 ± 0.08 | 0.76 |
| No. of sessions/week | 3.08 ± 0.15 | 3.25 ± 0.12 | 0.62 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kocher, F.M.; Galofaro, L.; Schwab, J.M.; Raabe, I.; Tannast, M.; Petek, D. Tibial Eminence Avulsion Fracture in Pediatric Patients Reinserted with Arthroscopy and Pull-Out Suture Technique: Clinical and Functional Outcomes in a Long-Term Follow Up with Return to Sport. Children 2025, 12, 499. https://doi.org/10.3390/children12040499
Kocher FM, Galofaro L, Schwab JM, Raabe I, Tannast M, Petek D. Tibial Eminence Avulsion Fracture in Pediatric Patients Reinserted with Arthroscopy and Pull-Out Suture Technique: Clinical and Functional Outcomes in a Long-Term Follow Up with Return to Sport. Children. 2025; 12(4):499. https://doi.org/10.3390/children12040499
Chicago/Turabian StyleKocher, Franziska M., Ludovic Galofaro, Joseph M. Schwab, Ines Raabe, Moritz Tannast, and Daniel Petek. 2025. "Tibial Eminence Avulsion Fracture in Pediatric Patients Reinserted with Arthroscopy and Pull-Out Suture Technique: Clinical and Functional Outcomes in a Long-Term Follow Up with Return to Sport" Children 12, no. 4: 499. https://doi.org/10.3390/children12040499
APA StyleKocher, F. M., Galofaro, L., Schwab, J. M., Raabe, I., Tannast, M., & Petek, D. (2025). Tibial Eminence Avulsion Fracture in Pediatric Patients Reinserted with Arthroscopy and Pull-Out Suture Technique: Clinical and Functional Outcomes in a Long-Term Follow Up with Return to Sport. Children, 12(4), 499. https://doi.org/10.3390/children12040499






