Impact of Kinesio Taping on Oral Feeding and Swallowing Functions: Acoustic Analysis of Swallowing Sounds in Late Preterm Infants—A Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
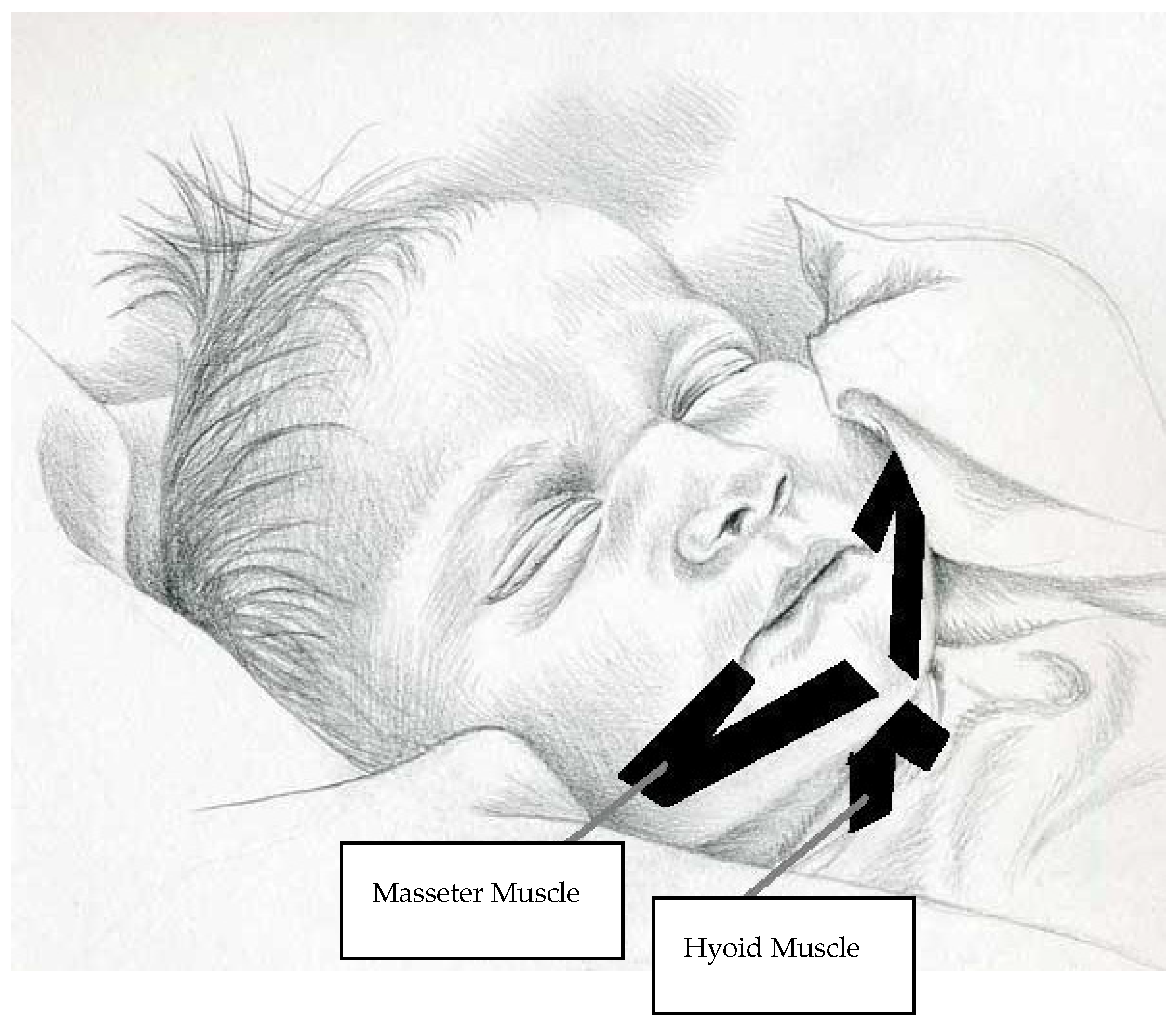
2.2. Procedure
2.3. Sample Size Calculation
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DOAJ | Directory of open access journals |
| TLA | Three letter acronym |
| LD | Linear dichroism |
References
- Ohuma, E.O.; Moller, A.-B.; Bradley, E.; Chakwera, S.; Hussain-Alkhateeb, L.; Lewin, A.; Okwaraji, Y.B.; Mahanani, W.R.; Johansson, E.W.; Lavin, T.; et al. National, regional, and global estimates of preterm birth in 2020, with trends from 2010: A systematic analysis. Lancet 2023, 402, 1261–1271. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.A.; Prade, L.S.; Keske-Soares, M.; Haëffner, L.S.; Weinmann, A.R. The oral motor capacity and feeding performance of preterm newborns at the time of transition to oral feeding. Braz. J. Med. Biol. Res. 2008, 41, 904–907. [Google Scholar] [CrossRef] [PubMed]
- Medoff-Cooper, B.; Rankin, K.; Li, Z.; Liu, L.; White-Traut, R. Multisensory intervention for preterm infants improves sucking organization. Adv. Neonatal Care 2015, 15, 142–149. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gouyon, J.B.; Iacobelli, S.; Ferdynus, C.; Bonsante, F. Neonatal problems of late and moderate preterm infants. Semin. Fetal Neonatal Med. 2012, 17, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Lau, C.; Smith, E.O.; Schanler, R.J. Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatr. 2003, 92, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Gewolb, I.H.; Vice, F.L. Abnormalities in the coordination of respiration and swallow in preterm infants with bronchopulmonary dysplasia. Dev. Med. Child Neurol. 2006, 48, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Kase, K.; Wallis, J.; Kase, T. Clinical Therapeutic Application of the Kinesio Taping Method; Ken Ikai Co., Ltd.: Tokyo, Japan, 2003. [Google Scholar]
- Öhman, A.M. The immediate effect of kinesiology taping on muscular imbalance for infants with congenital muscular torticollis. PMR 2012, 4, 504–508. [Google Scholar] [CrossRef] [PubMed]
- Giray, E.; Karadag-Saygi, E.; Mansiz-Kaplan, B.; Tokgoz, D.; Bayindir, O.; Kayhan, O. A randomized, single-blinded pilot study evaluating the effects of kinesiology taping and the tape application techniques in addition to therapeutic exercises in the treatment of congenital muscular torticollis. Clin. Rehabil. 2017, 31, 1098–1106. [Google Scholar] [CrossRef] [PubMed]
- Saniasiaya, J.; van der Meer, G.; Toll, E.C. Outcome of kinesio taping in drooling children: A systematic review. Int. J. Pediatr. Otorhinolaryngol. 2024, 184, 112057. [Google Scholar] [CrossRef] [PubMed]
- Abbas, Z.U.; Ahmed, U.; Sharif, F.; Siddique, K.; Shan EFatima, S.; Ajmal, M. Effects of routine physical therapy with and without kinesio taping in improving gross motor function in sitting and standing in spastic diplegic cerebral palsy children. J. Bodyw. Mov. Ther. 2024, 39, 666–672. [Google Scholar] [CrossRef] [PubMed]
- Yam, T.T.T.; Or, P.P.L.; Ma, A.W.W.; Fong, S.S.M.; Wong, M.S. Effect of Kinesio taping on Y-balance test performance and the associated leg muscle activation patterns in children with developmental coordination disorder: A randomized controlled trial. Gait Posture 2019, 68, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.L.; Wu, W.T.; Chang, K.V.; Lin, H.Y.; Chou, L.W. Application of Kinesio Taping method for newborn swallowing difficultly: A case report and literature review. Medicine 2016, 95, e4458. [Google Scholar] [CrossRef] [PubMed]
- Dodrill, P.; Gosa, M.M. Pediatric Dysphagia: Physiology, Assessment, and Management. Ann. Nutr. Metab. 2015, 66 (Suppl. S5), 24–31. [Google Scholar] [CrossRef] [PubMed]
- Yano, J.; Yamamoto-Shimizu, S.; Yokoyama, T.; Kumakura, I.; Hanayama, K.; Tsubahara, A. Effects of Tongue-Strengthening Exercise on the Geniohyoid Muscle in Young Healthy Adults. Dysphagia 2020, 35, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Denizoglu Kulli, H.; Karabulut, D.; Arslan, Y.Z. The prolonged effect of Kinesio Taping on joint torque and muscle activity. Somatosens. Mot. Res. 2023, 40, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-S.; Jung, Y.-J.; Kim, H.-H.; Lee, G. A Novel Method Using Kinesiology Taping for the Activation of Suprahyoid Muscles in Healthy Adults: A Preliminary Research. Dysphagia 2020, 35, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez Gonzalez, P.; Perez-Cabezas, V.; Chamorro-Moriana, G.; Ruiz Molinero, C.; Vazquez-Casares, A.M.; Gonzalez-Medina, G. Effectiveness of Oral Sensory-Motor Stimulation in Premature Infants in the Neonatal Intensive Care Unit (NICU) Systematic Review. Children 2021, 8, 758. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Foster, J.P.; Psaila, K.; Patterson, T. Non-nutritive sucking for increasing physiologic stability and nutrition in preterm infants. Cochrane Database Syst. Rev. 2016, 10, CD001071. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ni, W.S.; Zhang, Y.H.; Li, T.; Zhao, D.Y.; Tan, J.T.; Zhu, T.W.; Xie, L.J. Early rehabilitation intervention reduces the incidence of extrauterine growth retardation in preterm infants. Chin. J. Contemp. Pediatr. 2018, 20, 97–101. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hwang, Y.S.; Vergara, E.; Lin, C.H.; Coster, W.J.; Bigsby, R.; Tsai, W.H. Effects of prefeeding oral stimulation on feeding performance of preterm infants. Indian J. Pediatr. 2010, 77, 869–873. [Google Scholar] [CrossRef]
- Arora, K.; Goel, S.; Manerkar, S.; Konde, N.; Panchal, H.; Hegde, D.; Mondkar, J. Prefeeding Oromotor Stimulation Program for Improving Oromotor Function in Preterm Infants—A Randomized Controlled Trial. Indian Pediatr. 2018, 55, 675–678. [Google Scholar] [CrossRef] [PubMed]
- Ince, D.A.; Ecevit, A.; Acar, B.O.; Saracoglu, A.; Kurt, A.; Tekindal, M.A.; Tarcan, A. Noninvasive evaluation of swallowing sound is an effective way of diagnosing feeding maturation in newborn infants. Acta Paediatr. 2014, 103, e340–e348. [Google Scholar] [CrossRef] [PubMed]
- Kase, K.; Martin, P.; Yasukawa, A. Kinesio Taping in Pediatrics-Fundamentals and Whole Body Taping; Ken Ikai Co., Ltd.: Tokyo, Japan, 2006. [Google Scholar]
- Barton, B.; Peat, J. Medical Statistics: A Guide to SPSS, Data Analysis and Critical Appraisal; John Wiley & Sons: Hoboken, NJ, USA, 2014. [Google Scholar]
- Greene, Z.; O’Donnell, C.P.; Walshe, M. Oral stimulation for promoting oral feeding in preterm infants. Cochrane Database Syst. Rev. 2023, 6, CD009720. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gaebler, C.P.; Hanzlik, J.R. The effects of a prefeeding stimulation program on preterm infants. Am. J. Occup. Ther. 1996, 50, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Ostadi, M.; Jokar, F.; Armanian, A.M.; Namnabati, M.; Kazemi, Y.; Poorjavad, M. The effects of swallowing exercise and non-nutritive sucking exercise on oral feeding readiness in preterm infants: A randomized controlled trial. Int. J. Pediatr. Otorhinolaryngol. 2021, 142, 110602. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.J.; Kim, H.J.; Choi, J.B.; Park, J.S.; Hwang, N.K. Effect of Dysphagia Rehabilitation Using Kinesiology Taping on Oropharyngeal Muscle Hypertrophy in Post-Stroke Patients: A Double Blind Randomized Placebo-Controlled Trial. Healthcare 2020, 8, 411. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pervez, R.; Naz, S.; Babur, N.; Mumtaz, N. Effects of kinesio taping compared with manipulation therapy on drooling and speech intelligibility in children with oral dysphagia: A pilot study. Altern. Ther. Health Med. 2022, 28, 48–51. [Google Scholar] [PubMed]
- Amaizu, N.; Shulman, R.; Schanler, R.; Lau, C. Maturation of oral feeding skills in preterm infants. Acta Paediatr. 2008, 97, 61–67. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lagos, H.N.; Santos, R.S.; Abdulmassih, E.M.; Gallinea, L.F.; Langone, M. Characterization of swallowing sounds with the use of sonar Doppler in full-term and preterm newborns. Int. Arch. Otorhinolaryngol. 2013, 17, 383–386. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Geddes, D.T.; Chadwick, L.M.; Kent, J.C.; Garbin, C.P.; Hartmann, P.E. Ultrasound imaging of infant swallowing during breast-feeding. Dysphagia 2010, 25, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Ecevit, A.; Erdogan, B.; Anuk Ince, D.; Aksu, M.; Unal, S.; Turan, Ö.; Saracoglu, A.; Tarcan, A. Determination of oral feeding skills in late preterm, early term, and full-term infants using the neonatal oral feeding monitor (NeoSAFE). Ital. J. Pediatr. 2025, 51, 38. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Güleç, A.; Albayrak, I.; Erdur, Ö.; Öztürk, K.; Levendoglu, F. Effect of swallowing rehabilitation using traditional therapy, kinesiology taping and neuromuscular electrical stimulation on dysphagia in post-stroke patients: A randomized clinical trial. Clin. Neurol. Neurosurg. 2021, 211, 107020. [Google Scholar] [CrossRef] [PubMed]
- Naderifar, E.; Tarameshlu, M.; Salehi, R.; Ghelichi, L.; Bordbar, A.; Moradi, N.; Lessen Knoll, B. A Single-Subject Study to Consider the Premature Infant Oral Motor Intervention Combined with Kinesio-Tape in Premature Infants with Feeding Problems. Med. J. Islam. Repub. Iran 2024, 38, 38. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| KT Group X ± SD n = 37 | Control Group X ± SD n = 37 | p Value | |
|---|---|---|---|
| Gestational age (weeks) | 35.31 ± 0.82 | 35.29 ± 0.81 | 0.838 |
| Birth weight (grams) | 2330.56 ± 389.64 | 2426.21 ± 421.36 | 0.295 |
| Gender | |||
| Girls n (%) | 25 (56.8) | 17 (45.9) | 0.329 |
| Boys n (%) | 19 (43.2) | 20 (54.1) | |
| Apgar score | |||
| 1st min | 8.18 ± 0.81 | 7.64 ± 0.91 | 0.002 * |
| 5th min | 9.34 ± 0.52 | 8.91 ± 0.64 | 0.003 * |
| Maternal age (years) | 32.34 ± 4.19 | 32.75 ± 5.36 | 0.939 |
| Twin pregnancy n (%) | 24 (54.5) | 26 (70.3) | 0.707 |
| Feeding type (%) | |||
| Breastmilk | 11 (25.0) | 22 (59.5) | 0.001 * |
| Formula | 3 (6.8) | 5 (13.5) | |
| Mixed | 30 (68.2) | 10 (27.0) |
| KT Group X ± SD (n = 37) | Control X ± SD (n = 37) | p Value | |
|---|---|---|---|
| Amount of milk intake (mL) | |||
| before KT | 16.81 ± 6.38 | 16.35 ± 7.0 | 0.837 |
| after KT | 17.71 ± 6.22 | 18.27 ± 7.58 | 0.606 |
| after 24 h of KT | 21.47 ±7.45 | 23.33 ± 10.64 | 0.381 |
| Time for milk intake (s) | |||
| before KT | 121.70 ± 76.67 | 119.72 ± 1.64 | 0.045 * |
| after KT | 112.38 ± 51.33 | 117.03 ± 16.52 | 0.114 |
| after 24 h of KT | 123.92 ± 36.77 | 120.00 ± 15.57 | 0.816 |
| Maximum number of rhythmic swallows during milk intake (n) | |||
| before KT | 16.04 ± 10.32 | 14.80 ± 10.99 | 0.637 |
| after KT | 29.47 ± 20.16 | 14.53 ± 7.37 | 0.000 * |
| after 24 h of KT | 37.14 ± 21.16 | 19.20 ± 8.87 | 0.000 * |
| Heart rate during milk intake (/min.) | |||
| before KT | 136.02 ± 10.32 | 141.37 ± 2.65 | 0.152 |
| after KT | 138.43 ± 8.54 | 141.67 ± 2.64 | 0.033 * |
| after 24 h of KT | 135.85 ± 8.27 | 139.53 ± 3.21 | 0.021 * |
| Oxygen saturation during milk intake (%) | |||
| before KT | 96.84 ± 2.03 | 96.00 ± 1.22 | 0.015 |
| after KT | 96.40 ± 1.78 | 96.18 ± 1.22 | 0.677 |
| after 24 h of KT | 96.86 ± 2.10 | 96.43 ± 1.30 | 0.225 |
| Number of days for transition to full oral feeding | 2.64 ± 1.32 | 3.02 ± 2.36 | 0.924 |
| Number of days in the hospital | 5.50 ± 2.90 | 5.50 ± 4.60 | 0.373 |
| Number of days taking oxygen | 6.27 ± 17.01 | 2.14 ± 3.46 | 0.657 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Comuk Balci, N.; Anuk Ince, D.; Ecevit, A.; Erdoğan, B.; Doğan, I.E.; Turan, O.; Tarcan, A. Impact of Kinesio Taping on Oral Feeding and Swallowing Functions: Acoustic Analysis of Swallowing Sounds in Late Preterm Infants—A Randomized Clinical Trial. Children 2025, 12, 369. https://doi.org/10.3390/children12030369
Comuk Balci N, Anuk Ince D, Ecevit A, Erdoğan B, Doğan IE, Turan O, Tarcan A. Impact of Kinesio Taping on Oral Feeding and Swallowing Functions: Acoustic Analysis of Swallowing Sounds in Late Preterm Infants—A Randomized Clinical Trial. Children. 2025; 12(3):369. https://doi.org/10.3390/children12030369
Chicago/Turabian StyleComuk Balci, Nilay, Deniz Anuk Ince, Ayşe Ecevit, Balkar Erdoğan, Ilknur Ezgi Doğan, Ozden Turan, and Aylin Tarcan. 2025. "Impact of Kinesio Taping on Oral Feeding and Swallowing Functions: Acoustic Analysis of Swallowing Sounds in Late Preterm Infants—A Randomized Clinical Trial" Children 12, no. 3: 369. https://doi.org/10.3390/children12030369
APA StyleComuk Balci, N., Anuk Ince, D., Ecevit, A., Erdoğan, B., Doğan, I. E., Turan, O., & Tarcan, A. (2025). Impact of Kinesio Taping on Oral Feeding and Swallowing Functions: Acoustic Analysis of Swallowing Sounds in Late Preterm Infants—A Randomized Clinical Trial. Children, 12(3), 369. https://doi.org/10.3390/children12030369








