Usefulness of Non-High-Density Lipoprotein Cholesterol for Screening Dyslipidemia in Children and Adolescents with Overweight or Obesity: A Single-Center Retrospective Study
Highlights
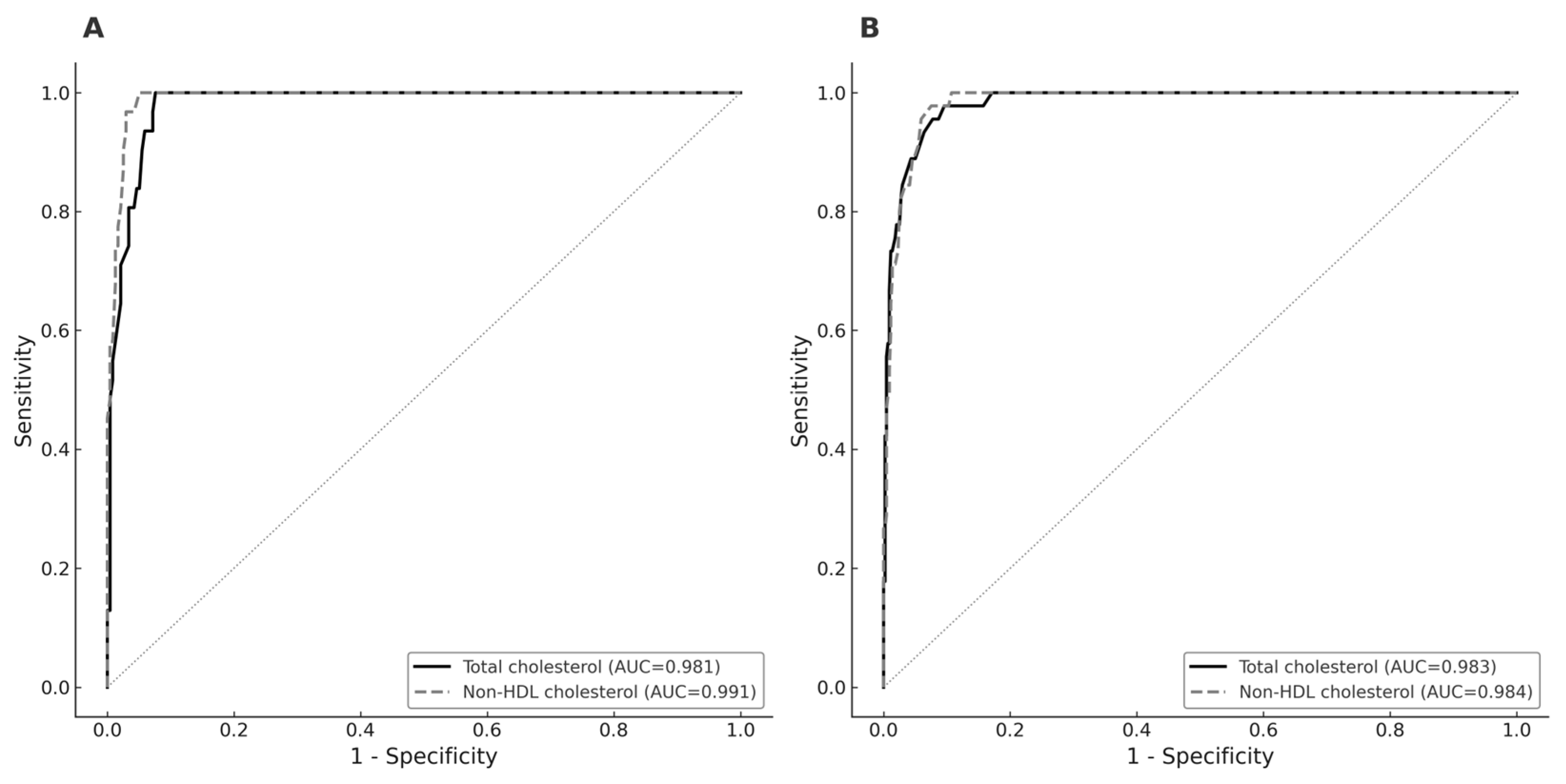
- Non–high-density-lipoprotein cholesterol (non-HDL cholesterol) showed high diagnostic performance for detecting elevated LDL-cholesterol, with a sensitivity of 100% in boys and 97.8% in girls.
- Random non-HDL cholesterol was non-inferior to fasting values and demonstrated significantly higher sensitivity in boys.
- Non-fasting non-HDL cholesterol is a practical first-line screening tool for dyslipidemia in overweight or obese children.
- More convenient screening may help identify more children at risk, allowing earlier lifestyle interventions to reduce future cardiovascular risk.
Abstract
1. Introduction
2. Subjects and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, J.; Kang, S.-C.; Kwon, O.; Hwang, S.-s.; Moon, J.S.; Chae, H.W.; Kim, J. Temporal Trends of the Prevalence of Abdominal Obesity and Metabolic Syndrome in Korean Children and Adolescents between 2007 and 2020. JOMES 2023, 32, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.-M.; Jung, J.-H.; Yang, Y.S.; Kim, W.; Cho, I.Y.; Lee, Y.-B.; Park, K.-Y.; Nam, G.E.; Han, K.; Taskforce Team of the Obesity Fact Sheet of the Korean Society for the Study of Obesity. 2023 Obesity Fact Sheet: Prevalence of Obesity and Abdominal Obesity in Adults, Adolescents, and Children in Korea from 2012 to 2021. JOMES 2024, 33, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, T.R.H.; Lausten-Thomsen, U.; Fonvig, C.E.; Bojsoe, C.; Pedersen, L.; Bratholm, P.S.; Hansen, T.; Pedersen, O.; Holm, J.C. Dyslipidemia and reference values for fasting plasma lipid concentrations in Danish/North-European White children and adolescents. BMC Pediatr. 2017, 17, 116. [Google Scholar] [CrossRef] [PubMed]
- Kuryan, R.E.; Jacobson, M.S.; Frank, G.R. Non-HDL-cholesterol in an adolescent diabetes population. J. Clin. Lipidol. 2014, 8, 194–198. [Google Scholar] [CrossRef]
- Korean Center for Disease Control and Prevension; The Korean Pediatric Society; Committee for Korean Children and Adolescents Growth Standard. 2017 Korean Children and Adolescents Growth Standard. Korean J. Pediatr. 2018, 61, 135–149. [Google Scholar] [CrossRef]
- Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics 2011, 128 (Suppl. 5), S213–S256. [Google Scholar] [CrossRef]
- Lim, J.S.; Kim, E.Y.; Kim, J.H.; Yoo, J.H.; Yi, K.H.; Chae, H.W.; Choi, J.H.; Kim, J.Y.; Hwang, I.T.; Committee of Dyslipidemia of Korean, C.; et al. 2017 Clinical practice guidelines for dyslipidemia of Korean children and adolescents. Ann. Pediatr. Endocrinol. Metab. 2020, 25, 199–207. [Google Scholar] [CrossRef]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Yoon, J.S.; Hwang, I.T. Screening and Management for Dyslipidemia in Korean Children and Adolescents. Ewha Med. J. 2022, 45, e4. [Google Scholar] [CrossRef]
- Kim, M.Y.; An, S.; Shim, Y.S.; Lee, H.S.; Hwang, J.S. Waist-height ratio and body mass index as indicators of obesity and cardiometabolic risk in Korean children and adolescents. Ann. Pediatr. Endocrinol. Metab. 2024, 29, 182–190. [Google Scholar] [CrossRef]
- Song, K.; Jeon, S.; Lee, H.S.; Choi, H.S.; Suh, J.; Kwon, A.; Kim, H.S.; Chae, H.W. Trends of Dyslipidemia in Korean Youth According to Sex and Body Mass Index: Based on the Korea National Health and Nutrition Examination Survey (2007–2018). J. Pediatr. 2021, 237, 71–78.e75. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Hwang, J.S.; Park, H.K.; Lee, H.S.; Kim, H.S.; Kim, E.Y.; Lim, J.S. Serum lipid concentrations, prevalence of dyslipidemia, and percentage eligible for pharmacological treatment of Korean children and adolescents; data from the Korea National Health and Nutrition Examination Survey IV (2007–2009). PLoS ONE 2012, 7, e49253. [Google Scholar] [CrossRef] [PubMed]
- Eichberger, L.; Kern, L.; Wang, H.; Crow, J.; Rhee, K.E. Universal Lipid Screening Among 9- to 11-Year-Old Children: Screening Results and Physician Management. Clin. Pediatr. 2022, 61, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.M. Dyslipidemia in children and adolescents: When and how to diagnose and treat? Pediatr. Gastroenterol. Hepatol. Nutr. 2014, 17, 85–92. [Google Scholar] [CrossRef]
- Jacobson, T.A.; Maki, K.C.; Orringer, C.E.; Jones, P.H.; Kris-Etherton, P.; Sikand, G.; La Forge, R.; Daniels, S.R.; Wilson, D.P.; Morris, P.B.; et al. National Lipid Association Recommendations for Patient-Centered Management of Dyslipidemia: Part 2. J. Clin. Lipidol. 2015, 9, S1–S122.e121. [Google Scholar] [CrossRef]
- Quispe, R.; Brownstein, A.J.; Sathiyakumar, V.; Park, J.; Chang, B.; Sajja, A.; Guallar, E.; Lazo, M.; Jones, S.R.; Martin, S.S. Utility of non-HDL-C and apoB targets in the context of new more aggressive lipid guidelines. Am. J. Prev. Cardiol. 2021, 7, 100203. [Google Scholar] [CrossRef]
- Juonala, M.; Wu, F.; Sinaiko, A.; Woo, J.G.; Urbina, E.M.; Jacobs, D.; Steinberger, J.; Prineas, R.; Koskinen, J.; Sabin, M.A.; et al. Non-HDL Cholesterol Levels in Childhood and Carotid Intima-Media Thickness in Adulthood. Pediatrics 2020, 145, e20192114. [Google Scholar] [CrossRef]
- Saleh, C. Carotid intima-media thickness as surrogate marker: The clouding effect of submillimetric inaccuracies. Ann. Pediatr. Endocrinol. Metab. 2024, 29, 387–388. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Juonala, M.; Jacobs, D.R., Jr.; Daniels, S.R.; Kahonen, M.; Woo, J.G.; Sinaiko, A.R.; Viikari, J.S.A.; Bazzano, L.A.; Burns, T.L.; et al. Childhood Non-HDL Cholesterol and LDL Cholesterol and Adult Atherosclerotic Cardiovascular Events. Circulation 2024, 149, 217–226. [Google Scholar] [CrossRef]
- Srinivasan, S.R.; Myers, L.; Berenson, G.S. Distribution and correlates of non-high-density lipoprotein cholesterol in children: The Bogalusa Heart Study. Pediatrics 2002, 110, e29. [Google Scholar] [CrossRef]
- Daniels, S.R.; Greer, F.R.; Committee on Nutrition. Lipid screening and cardiovascular health in childhood. Pediatrics 2008, 122, 198–208. [Google Scholar] [CrossRef]
- Lim, J.S. The current state of dyslipidemia in Korean children and adolescents and its management in clinical practice. Ann. Pediatr. Endocrinol. Metab. 2013, 18, 1–8. [Google Scholar] [CrossRef]
- Force, U.S.P.S.T.; Grossman, D.C.; Bibbins-Domingo, K.; Curry, S.J.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W., Jr.; Kemper, A.R.; Krist, A.H.; et al. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 2017, 317, 2417–2426. [Google Scholar] [CrossRef]
- Guirguis-Blake, J.M.; Evans, C.V.; Coppola, E.L.; Redmond, N.; Perdue, L.A. Screening for Lipid Disorders in Children and Adolescents: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2023, 330, 261–274. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Jacobs, D.R., Jr.; Daniels, S.R.; Kahonen, M.; Woo, J.G.; Sinaiko, A.R.; Viikari, J.S.A.; Bazzano, L.A.; Steinberger, J.; Urbina, E.M.; et al. Non-High-Density Lipoprotein Cholesterol Levels From Childhood to Adulthood and Cardiovascular Disease Events. JAMA 2024, 331, 1834–1844. [Google Scholar] [CrossRef] [PubMed]
- Nuotio, J.; Oikonen, M.; Magnussen, C.G.; Viikari, J.S.; Hutri-Kahonen, N.; Jula, A.; Thomson, R.; Sabin, M.A.; Daniels, S.R.; Raitakari, O.T.; et al. Adult dyslipidemia prediction is improved by repeated measurements in childhood and young adulthood. The Cardiovascular Risk in Young Finns Study. Atherosclerosis 2015, 239, 350–357. [Google Scholar] [CrossRef] [PubMed]
| Boys | Girls | Total | |
|---|---|---|---|
| Number (%) | 268 (35.7%) | 483 (64.3%) | 751 (100%) |
| Age | |||
| Subgroup 2–9 years | 8.0 (6.0–9.0) | 8.0 (7.0–8.0) | 8.0 (7.0–9.0) |
| Subgroup 10–19 years | 12.0 (11.0–15.0) | 11.0 (10.0–14.0) | 12.0 (10.0–15.0) |
| Body mass index SDS | 1.6 (1.1–2.2) | 1.7 (1.2–2.1) | 1.7 (1.2–2.2) |
| Total cholesterol ≥ 200 mg/dL (%) | 43 (16.0%) | 62 (12.8%) | 105 (14.0%) |
| Non-HDL cholesterol ≥ 145 mg/dL (%) | 50 (18.7%) | 82 (17.0%) | 132 (17.6%) |
| Measured LDL cholesterol ≥ 130 mg/dL (%) | 31 (11.6%) | 45 (9.3%) | 76 (10.1%) |
| Triglycerides ≥ 100 or 130 mg/dL a (%) | 95 (35.4%) | 150 (31.1%) | 245 (32.6%) |
| HDL cholesterol < 40 mg/dL (%) | 56 (20.9%) | 74 (15.3%) | 130 (17.3%) |
| Criteria | Cholesterol Cutoff Values | Number (%) * | Sensitivity | Specificity |
|---|---|---|---|---|
| Boys | Total cholesterol ≥ 200 mg/dL | 43 (16.0%) | 86.0 (72.7–93.4) | 94.2 (90.4–96.6) |
| Triglycerides ≥ 100 or 130 mg/dL a | 108 (40.3%) | 23.1 (16.2–31.9) | 84.4 (78.0–89.2) | |
| Measured LDL cholesterol ≥ 130 mg/dL | 31 (11.6%) | 100.0 (89.0–100.0) | 92.0 (87.8–94.8) | |
| Girls | Total cholesterol ≥ 200 mg/dL | 62 (12.8%) | 79.0 (67.4–87.3) | 92.2 (89.2–94.4) |
| Triglycerides ≥ 100 or 130 mg/dL a | 220 (45.5%) | 15.9 (11.7–21.3) | 82.1 (77.0–86.3) | |
| Measured LDL cholesterol ≥ 130 mg/dL | 45 (9.3%) | 97.8 (88.4–99.6) | 91.3 (88.3–93.6) |
| Criteria | Cholesterol Cutoff Values | Sex | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| Age (2–9 years) | Total cholesterol ≥ 200 mg/dL | Boys | 100.0 (78.5–100.0) | 91.3 (84.2–95.3) |
| Girls | 83.9 (67.4–92.9) | 94.5 (91.6–96.4) | ||
| Non-HDL cholesterol ≥ 145 mg/dL | Boys | 100.0 (78.5–100.0) | 94.2 (87.9–97.3) | |
| Girls | 100.0 (89.0–100.0) | 91.2 (87.8–93.7) | ||
| Age (10–19 years) | Total cholesterol ≥ 200 mg/dL | Boys | 88.2 (65.7–96.7) | 96.3 (91.6–98.4) |
| Girls | 100.0 (78.5–100.0) | 97.3 (90.8–99.3) | ||
| Non-HDL cholesterol ≥ 145 mg/dL | Boys | 100.0 (81.6–100.0) | 90.3 (84.1–94.2) | |
| Girls | 92.9 (68.5–98.7) | 92.0 (83.6–96.3) |
| Criteria | Cholesterol Cutoff Values | Sensitivity (%) | Specificity (%) |
|---|---|---|---|
| Boys | Non-HDL cholesterol in non-fasting state | 100 | 90.3 |
| Non-HDL cholesterol in fasting state | 94.3 | 95.7 | |
| Girls | Non-HDL cholesterol in non-fasting state | 92.9 | 92.0 |
| Non-HDL cholesterol in fasting state | 92.3 | 96.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nam, H.-K.; Kang, E.; Lee, K.-H.; Rhie, Y.-J. Usefulness of Non-High-Density Lipoprotein Cholesterol for Screening Dyslipidemia in Children and Adolescents with Overweight or Obesity: A Single-Center Retrospective Study. Children 2025, 12, 1518. https://doi.org/10.3390/children12111518
Nam H-K, Kang E, Lee K-H, Rhie Y-J. Usefulness of Non-High-Density Lipoprotein Cholesterol for Screening Dyslipidemia in Children and Adolescents with Overweight or Obesity: A Single-Center Retrospective Study. Children. 2025; 12(11):1518. https://doi.org/10.3390/children12111518
Chicago/Turabian StyleNam, Hyo-Kyoung, Eungu Kang, Kee-Hyoung Lee, and Young-Jun Rhie. 2025. "Usefulness of Non-High-Density Lipoprotein Cholesterol for Screening Dyslipidemia in Children and Adolescents with Overweight or Obesity: A Single-Center Retrospective Study" Children 12, no. 11: 1518. https://doi.org/10.3390/children12111518
APA StyleNam, H.-K., Kang, E., Lee, K.-H., & Rhie, Y.-J. (2025). Usefulness of Non-High-Density Lipoprotein Cholesterol for Screening Dyslipidemia in Children and Adolescents with Overweight or Obesity: A Single-Center Retrospective Study. Children, 12(11), 1518. https://doi.org/10.3390/children12111518





