Implementation of the Finnish Good Practice “Smart Family” in Poland
Abstract
1. Introduction
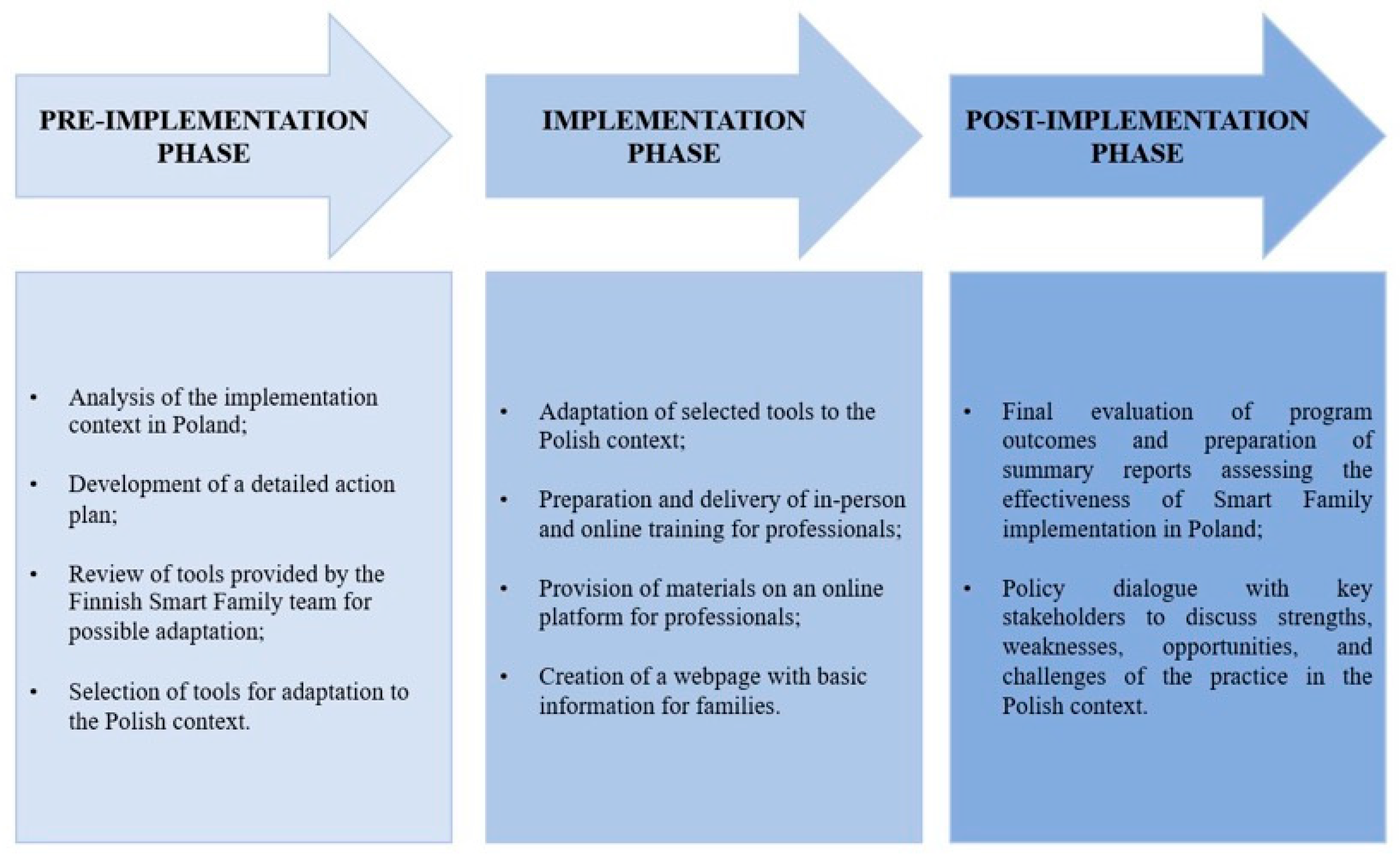
2. Materials and Methods
Implementation Process, Participant Description, Adaptation, and Evaluation
3. Results and Discussion
Implementation of the Smart Family Practice in Poland
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| WHO | World Health Organization |
| NGOs | Non-Governmental Organizations |
| JEŻ | Junior-Edu-Nutrition |
| DINO-PL | Diagnosis–Intervention–Hypertension–Obesity |
References
- GBD 2021 Adolescent BMI Collaborators. Global, regional, and national prevalence of child and adolescent overweight and obesity, 1990–2021, with forecasts to 2050: A forecasting study for the Global Burden of Disease Study 2021. Lancet 2025, 405, 785–812. [Google Scholar] [CrossRef]
- OECD. Health at a Glance 2021: OECD Indicators; OECD Publishing: Paris, France, 2021. [Google Scholar] [CrossRef]
- Bąk-Sosnowska, M.; Białkowska, M.; Bogdański, P.; Chomiuk, T.; Gałązka-Sobotka, M.; Holecki, M.; Jarosińska, A.; Jezierska, M.; Kamiński, P.; Kłoda, K.; et al. Clinical guidelines for the management of obesity 2022—Position of the Polish Society for the Treatment of Obesity. Med. Prakt. 2022, 1–87. Available online: https://ptlo.org.pl/resources/data/sections/114/ws_otylosc.pdf (accessed on 22 September 2025).
- World Health Organization. Population-Based Approaches to Childhood Obesity Prevention; WHO Library Cataloguing-in-Publication Data: Geneva, Switzerland, 2012. [Google Scholar]
- UNICEF. Prevention of Overweight and Obesity in Children and Adolescents; UNICEF: New York, NY, USA, 2025; Available online: https://www.unicef.org/documents/prevention-overweight-and-obesity-children-and-adolescents (accessed on 20 September 2025).
- Junior-Edu-Nutrition. About the Program. 2023. Available online: https://jez.edu.pl/o-programie (accessed on 20 September 2025).
- Institute of Mother and Child. DINO-PL Project. 2021. Available online: https://imid.med.pl/pl/top-menu/projekty-npz/projekt-dino-pl (accessed on 20 September 2025).
- Institute of Mother and Child. Obesity Treatment Program. 2021. Available online: https://www.czd.pl/strony/dzialalnosc-kliniczna/program-leczenia-otylosci (accessed on 21 September 2025).
- College of Family Physicians in Poland; Polish Society of Family Medicine; Polish Society for the Study of Obesity. Guidelines for the management of overweight and obesity in family medicine practice. Lekarz Rodz. 2017, 3, 1–56. [Google Scholar]
- National Health Fund. Regulation No. 124/2022/DSOZ of the President of the National Health Fund of 29 September 2022 on the Conditions for Concluding and Implementing Contracts for the Provision of Health Care Services in the Field of Primary Health Care. 2022. Available online: https://www.nfz.gov.pl (accessed on 25 September 2025).
- Health4EUKids. Project Website. 2025. Available online: https://www.dypede.gr/health4eukids/ (accessed on 20 September 2025).
- Neuvokas Perhe. Neuvokas Perhe. 2025. Available online: https://neuvokasperhe.fi/en/ (accessed on 22 September 2025).
- European Commission. EU4Health Programme 2021–2027—A Vision for a Healthier European Union; European Commission: Brussels, Belgium, 2021; Available online: https://health.ec.europa.eu/funding/eu4health-programme-2021-2027-vision-healthier-european-union_en (accessed on 22 September 2025).
- European Commission. Selection of Good Practices in NCD Prevention 2021; European Commission: Brussels, Belgium, 2021; Available online: https://webgate.ec.europa.eu/dyna/bp-portal/best-practice-file/379 (accessed on 22 September 2025).
- Fullaondo, A.; Txarramendieta, J.; de Manuel, E.; Barbolini, M. Guideline on Implementation Strategy. Module I: Pre-Implementation Phase; Final Version; Kronikgune: Bilbao, Spain, 2018. [Google Scholar]
- National Health Fund. Health4EUKids. “Healthy Family” Program; National Health Fund: Warsaw, Poland, 2023. Available online: https://akademia.nfz.gov.pl/health4eukids/ (accessed on 25 September 2025).
- National Health Fund. NFZ Academy—National Health Fund Service. National Health Fund: Warsaw, Poland. Available online: https://e-learning.nfz.gov.pl/course/view.php?id=20937 (accessed on 25 September 2025).
- National Health Fund. How to Talk About Childhood Obesity? A Guide for Professionals; National Health Fund: Warsaw, Poland, 2025. Available online: https://centrumwiedzy.nfz.gov.pl/media/data/202509/dla-profesjonalistow.pdf (accessed on 25 September 2025).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nowak, J.; Szymczak, A.; Kaczmarska, B.; Klonowska, K.A.; Morawska, M.; Kuusipalo, H.; Koivurinta, E.; Kuisma, K.; Mäki, P.; Sainio, T.; et al. Implementation of the Finnish Good Practice “Smart Family” in Poland. Children 2025, 12, 1437. https://doi.org/10.3390/children12111437
Nowak J, Szymczak A, Kaczmarska B, Klonowska KA, Morawska M, Kuusipalo H, Koivurinta E, Kuisma K, Mäki P, Sainio T, et al. Implementation of the Finnish Good Practice “Smart Family” in Poland. Children. 2025; 12(11):1437. https://doi.org/10.3390/children12111437
Chicago/Turabian StyleNowak, Justyna, Agata Szymczak, Barbara Kaczmarska, Katarzyna Anna Klonowska, Marta Morawska, Heli Kuusipalo, Emma Koivurinta, Kati Kuisma, Päivi Mäki, Taina Sainio, and et al. 2025. "Implementation of the Finnish Good Practice “Smart Family” in Poland" Children 12, no. 11: 1437. https://doi.org/10.3390/children12111437
APA StyleNowak, J., Szymczak, A., Kaczmarska, B., Klonowska, K. A., Morawska, M., Kuusipalo, H., Koivurinta, E., Kuisma, K., Mäki, P., Sainio, T., Savolainen, N., & Brukało, K. (2025). Implementation of the Finnish Good Practice “Smart Family” in Poland. Children, 12(11), 1437. https://doi.org/10.3390/children12111437





