Fundamental Movement/Motor Skills as an Important Component of Physical Literacy and Bridge to Physical Activity: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
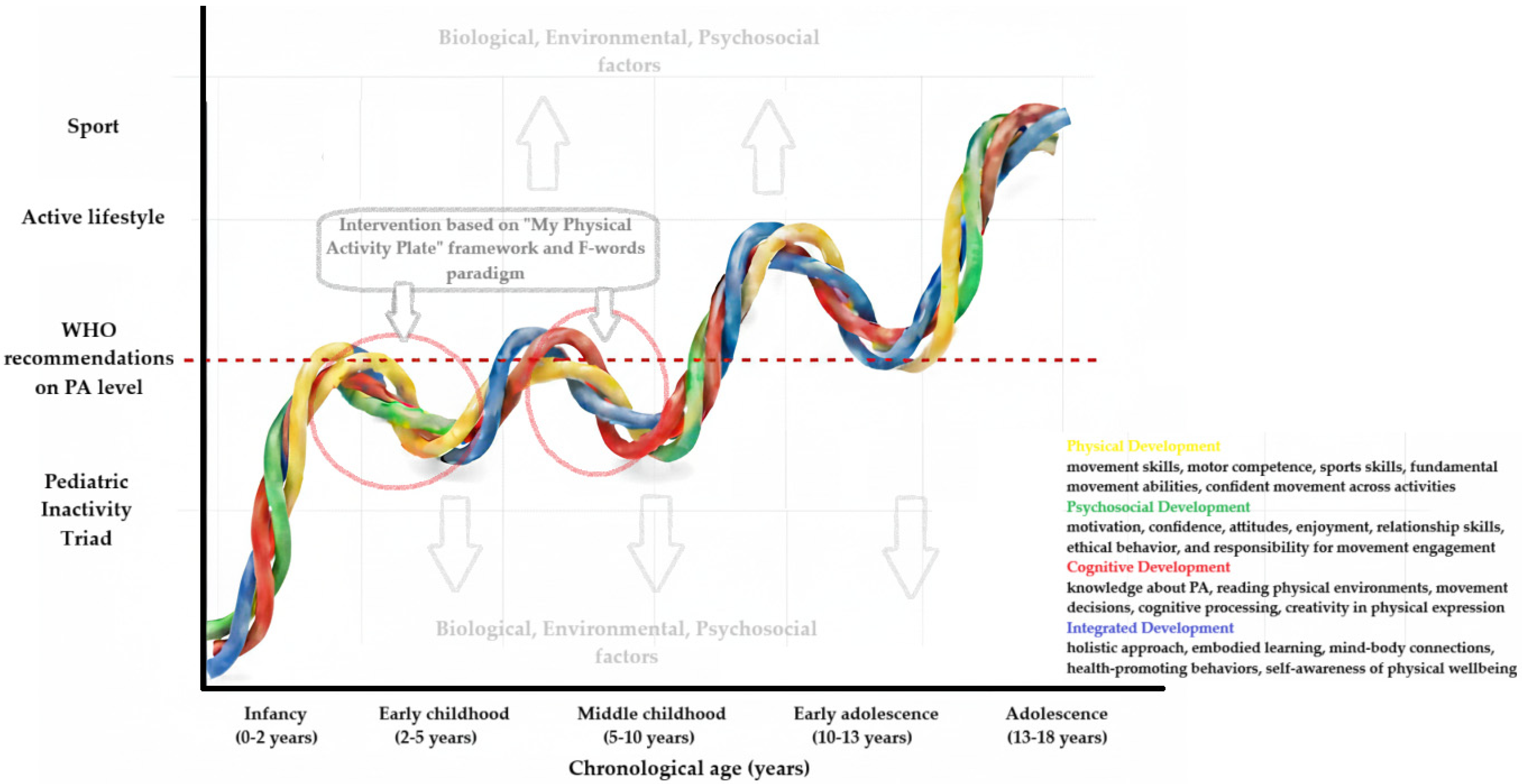
4. Discussion
- Concepts/Terms Used in the Context of FMSs: Motor Competence, Physical Literacy
- Associations of FMSs with other parameters/measures
- Tools for Assessing Fundamental Movement Skills (FMSs)
- Impact of Selected Interventions on Fundamental Movement Skills (FMSs)
- -
- In preschool
- -
- At school
- -
- The role of teachers, the role of parents
- Intervention Dosage
- The role of pediatric physicians, physiotherapists and occupational therapists
- Practical recommendations for clinicians:
- Routine screening for early identification of FMS deficiency:
- ○
- Collect information about PA patterns, play opportunities, and previous motor development milestones.
- ○
- Particularly between the ages of 3 and 6—ask about a child’s ability to run, jump, throw, catch, and keep static and dynamic balance.
- Prescribing intervention:
- ○
- In the presence of FMS deficits, children should be referred to pediatric physiotherapists who should conduct screening tests (e.g., TGMD).
- ○
- In patients with chronic diseases, individualized PA plans incorporating FMS elements are recommended.
- Parental education:
- ○
- Educate caregivers about the importance of movement quality—coordination, balance, and skill acquisition—over simple metrics such as step count or minutes of activity.
- ○
- Encourage home-based play and structured activities that develop motor skills.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| FMSs | fundamental movement skills |
| PA | physical activity |
| MC | motor competence |
| PF | physical fitness |
| PL | physical literacy |
| WHO | World Health Organization |
| TGMD | Test of Gross Motor Development |
| BOT | Bruininks–Oseretsky Test of Motor Proficiency |
| MABC | Movement Assessment Battery for Children |
| PE | physical education |
| ICF | International Classification of Functioning, Disability and Health |
References
- Malina, R. Motor Development during Infancy and Early Childhood: Overview and Suggested Directions for Research. Int. J. Sport Health Sci. 2004, 2, 50–66. [Google Scholar] [CrossRef]
- Thomason, M.E.; Hect, J.; Waller, R.; Manning, J.H.; Stacks, A.M.; Beeghly, M.; Boeve, J.L.; Wong, K.; Heuvel, M.I.v.D.; Hernandez-Andrade, E.; et al. Prenatal neural origins of infant motor development: Associations between fetal brain and infant motor development. Dev. Psychopathol. 2018, 30, 763–772. [Google Scholar] [CrossRef]
- Zi, Y.; VAN Beijsterveldt, C.E.M.; Bartels, M.; DE Geus, E.J.C. Genetic and Environmental Effects on the Early Motor Development as a Function of Parental Educational Attainment. Med. Sci. Sports Exerc. 2023, 55, 1845–1856. [Google Scholar] [CrossRef]
- Adolph, K.E.; Hoch, J.E. Motor Development: Embodied, Embedded, Enculturated, and Enabling. Annu. Rev. Psychol. 2019, 70, 141–164. [Google Scholar] [CrossRef]
- Wang, X.; Zhou, B. Motor development-focused exercise training enhances gross motor skills more effectively than ordinary physical activity in healthy preschool children: An updated meta-analysis. Front. Public Health 2024, 12, 1414152. [Google Scholar] [CrossRef] [PubMed]
- Wick, K.; Leeger-Aschmann, C.S.; Monn, N.D.; Radtke, T.; Ott, L.V.; Rebholz, C.E.; Cruz, S.; Gerber, N.; Schmutz, E.A.; Puder, J.J.; et al. Interventions to Promote Fundamental Movement Skills in Childcare and Kindergarten: A Systematic Review and Meta-Analysis. Sports Med. 2017, 47, 2045–2068. [Google Scholar] [CrossRef]
- Koolwijk, P.; Hoeboer, J.; Mombarg, R.; Savelsbergh, G.J.P.; de Vries, S. Fundamental movement skill interventions in young children: A systematic review. Int. J. Sport Exerc. Psychol. 2023, 22, 1661–1683. [Google Scholar] [CrossRef]
- Gallahue, D.L.; Ozmun, J.C.; Goodway, J. Understanding Motor Development Infants, Children, Adolescents, Adults; McGraw-Hill: New York, NY, USA, 2012. [Google Scholar]
- Logan, S.W.; Ross, S.M.; Chee, K.; Stodden, D.F.; Robinson, L.E. Fundamental motor skills: A systematic review of terminology. J. Sports Sci. 2017, 36, 781–796. [Google Scholar] [CrossRef]
- Rudd, J.R.; Barnett, L.M.; Butson, M.L.; Farrow, D.; Berry, J.; Polman, R.C.J. Fundamental Movement Skills Are More than Run, Throw and Catch: The Role of Stability Skills. PLoS ONE 2015, 10, e0140224. [Google Scholar] [CrossRef]
- Newell, K.M. What are Fundamental Motor Skills and What is Fundamental About Them? J. Mot. Learn. Dev. 2020, 8, 280–314. [Google Scholar] [CrossRef]
- Grillner, S.; El Manira, A. Current Principles of Motor Control, with Special Reference to Vertebrate Locomotion. Physiol. Rev. 2020, 100, 271–320. [Google Scholar] [CrossRef]
- Dominici, N.; Ivanenko, Y.P.; Cappellini, G.; D’avella, A.; Mondì, V.; Cicchese, M.; Fabiano, A.; Silei, T.; Di Paolo, A.; Giannini, C.; et al. Locomotor Primitives in Newborn Babies and Their Development. Science 2011, 334, 997–999. [Google Scholar] [CrossRef]
- Logan, S.W.; Robinson, L.E.; Wilson, A.E.; Lucas, W.A. Getting the fundamentals of movement: A meta-analysis of the effectiveness of motor skill interventions in children. Child Care Health Dev. 2011, 38, 305–315. [Google Scholar] [CrossRef]
- Hulteen, R.M.; Morgan, P.J.; Barnett, L.M.; Stodden, D.F.; Lubans, D.R. Development of Foundational Movement Skills: A Conceptual Model for Physical Activity Across the Lifespan. Sports Med. 2018, 48, 1533–1540. [Google Scholar] [CrossRef]
- Zheng, X.; Borhannudin, B.A.; Nasnoor, J.M.N.; Shamsulariffin, B.S.; Zeinab, Z. Relationship between Curriculum-Based Intervention and Fundamental Movement Skills among Preschoolers: A Systematic Literature Review. Int. J. Hum. Mov. Sports Sci. 2021, 9, 1174–1188. [Google Scholar]
- Bolger, L.E.; Bolger, L.A.; O’neill, C.; Coughlan, E.; O’brien, W.; Lacey, S.; Burns, C.; Bardid, F. Global levels of fundamental motor skills in children: A systematic review. J. Sports Sci. 2020, 39, 717–753. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Zhu, W.; Ulrich, D.A.; Qin, M. Have the Fundamental Movement Skills of U.S. Children Changed? Res. Q. Exerc. Sport 2023, 95, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Huotari, P.; Heikinaro-Johansson, P.; Watt, A.; Jaakkola, T. Fundamental movement skills in adolescents: Secular trends from 2003 to 2010 and associations with physical activity and BMI. Scand. J. Med. Sci. Sports 2017, 28, 1121–1129. [Google Scholar] [CrossRef]
- Webster, E.K.; Martin, C.K.; Staiano, A.E. Fundamental motor skills, screen-time, and physical activity in preschoolers. J. Sport Health Sci. 2019, 8, 114–121. [Google Scholar] [CrossRef]
- Loebach, J.; Sanches, M.; Jaffe, J.; Elton-Marshall, T. Paving the Way for Outdoor Play: Examining Socio-Environmental Barriers to Community-Based Outdoor Play. Int. J. Environ. Res. Public Health 2021, 18, 3617. [Google Scholar] [CrossRef]
- Barnett, L.M.; Stodden, D.; Cohen, K.E.; Smith, J.J.; Lubans, D.R.; Lenoir, M.; Iivonen, S.; Miller, A.D.; Laukkanen, A.; Dudley, D.; et al. Fundamental Movement Skills: An Important Focus. J. Teach. Phys. Educ. 2016, 35, 219–225. [Google Scholar] [CrossRef]
- Praxedes, P.; Maia, J.; Santos, C.; Garbeloto, F.; Hedeker, D.; Barreira, T.V.; Garganta, R.; Farias, C.; Tani, G.; Chaput, J.; et al. Associations of obesity, movement behaviors, and socioeconomic status with fundamental movement skills in children: Results from the REACT project. Am. J. Hum. Biol. 2024, 36, e24108. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef]
- Rico-González, M. The Effect of Primary School-Based Physical Education Programs: A Systematic Review of Randomized Controlled Trials. J. Phys. Act. Health 2023, 20, 317–347. [Google Scholar] [CrossRef]
- Bremer, E.; Cairney, J. Fundamental Movement Skills and Health-Related Outcomes: A Narrative Review of Longitudinal and Intervention Studies Targeting Typically Developing Children. Am. J. Lifestyle Med. 2016, 12, 148–159. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Cao, Y.; Zhang, Z.; Gao, R.; Qu, G. Correlation of fundamental movement skills with health-related fitness elements in children and adolescents: A systematic review. Front. Public Health 2023, 11, 1129258. [Google Scholar] [CrossRef]
- Wang, J.-W.; Qu, S.; Zhu, Z.-C.; Zhao, X.; Song, W.-J.; Li, X.; Chen, W.-D.; Luo, D.-M. Global hotspots and trends in research on preschool children’s motor development from 2012 to 2022: A bibliometric analysis. Front. Public Health 2023, 11, 1118674. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Grauduszus, M.; Wessely, S.; Klaudius, M.; Joisten, C. Definitions and assessments of physical literacy among children and youth: A scoping review. BMC Public Health 2023, 23, 1746. [Google Scholar] [CrossRef]
- Liu, Y.; Li, Z.; Yuan, L.; Zhou, Z. The Bidirectional Correlation between Fundamental Motor Skill and Moderate-to-Vigorous Physical Activities: A Systematic Review and Meta-Analysis. Children 2023, 10, 1504. [Google Scholar] [CrossRef] [PubMed]
- Nagy, Á.V.; Wilhelm, M.; Domokos, M.; Győri, F.; Berki, T. Assessment Tools Measuring Fundamental Movement Skills of Primary School Children: A Narrative Review in Methodological Perspective. Sports 2023, 11, 178. [Google Scholar] [CrossRef]
- Jerebine, A.; Heering, T.; Barnett, L.M. Educator-Perceived Barriers and Facilitators to Structured-Physical Activity in Early Childhood Centres: A Systematic Review. Res. Q. Exerc. Sport 2023, 95, 243–262. [Google Scholar] [CrossRef]
- Chaput, J.-P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Jago, R.; Ortega, F.B.; Katzmarzyk, P.T. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: Summary of the evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 141. [Google Scholar] [CrossRef]
- Tucker, P. The physical activity levels of preschool-aged children: A systematic review. Early Child. Res. Q. 2008, 23, 547–558. [Google Scholar] [CrossRef]
- Pereira, S.; Reyes, A.C.; Chaves, R.; Santos, C.; Vasconcelos, O.; Tani, G.; Katzmarzyk, P.T.; Baxter-Jones, A.; Maia, J. Correlates of the Physical Activity Decline during Childhood. Med. Sci. Sports Exerc. 2022, 54, 2129–2137. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J. Physical Inactivity in Childhood from Preschool to Adolescence. ACSMs Health Fit. J. 2019, 23, 21–25. [Google Scholar] [CrossRef]
- van Sluijs, E.M.F.; Ekelund, U.; Crochemore-Silva, I.; Guthold, R.; Ha, A.; Lubans, D.; Oyeyemi, A.L.; Ding, D.; Katzmarzyk, P.T. Physical activity behaviours in adolescence: Current evidence and opportunities for intervention. Lancet 2021, 398, 429–442. [Google Scholar] [CrossRef] [PubMed]
- Faigenbaum, A.D.; Rebullido, T.R.; MacDonald, J.P. Pediatric Inactivity Triad: A Risky PIT. Optom. Vis. Sci. 2018, 17, 45–47. [Google Scholar] [CrossRef]
- Myer, G.D.; Faigenbaum, A.D.; Edwards, N.M.; Clark, J.F.; Best, T.M.; Sallis, R.E. Sixty minutes of what? A developing brain perspective for activating children with an integrative exercise approach. Br. J. Sports Med. 2015, 49, 1510–1516. [Google Scholar] [CrossRef]
- Lopes, L.; Santos, R.; Coelho-E-Silva, M.; Draper, C.; Mota, J.; Jidovtseff, B.; Clark, C.; Schmidt, M.; Morgan, P.; Duncan, M.; et al. A Narrative Review of Motor Competence in Children and Adolescents: What We Know and What We Need to Find Out. Int. J. Environ. Res. Public Health 2020, 18, 18. [Google Scholar] [CrossRef]
- Robinson, L.E.; Stodden, D.F.; Barnett, L.M.; Lopes, V.P.; Logan, S.W.; Rodrigues, L.P.; D’Hondt, E. Motor Competence and its Effect on Positive Developmental Trajectories of Health. Sports Med. 2015, 45, 1273–1284. [Google Scholar] [CrossRef]
- Barnett, L.M.; Lai, S.K.; Veldman, S.L.C.; Hardy, L.L.; Cliff, D.P.; Morgan, P.J.; Zask, A.; Lubans, D.R.; Shultz, S.P.; Ridgers, N.D.; et al. Correlates of Gross Motor Competence in Children and Adolescents: A Systematic Review and Meta-Analysis. Sports Med. 2016, 46, 1663–1688. [Google Scholar] [CrossRef]
- Cattuzzo, M.T.; Henrique, R.D.S.; Ré, A.; de Oliveira, I.S.; Melo, B.M.; Moura, M.D.S.; de Araújo, R.C.; Stodden, D. Motor competence and health related physical fitness in youth: A systematic review. J. Sci. Med. Sport 2016, 19, 123–129. [Google Scholar] [CrossRef]
- Utesch, T.; Bardid, F.; Büsch, D.; Strauss, B. The Relationship Between Motor Competence and Physical Fitness from Early Childhood to Early Adulthood: A Meta-Analysis. Sports Med. 2019, 49, 541–551. [Google Scholar] [CrossRef]
- Burton, A.M.; Cowburn, I.; Thompson, F.; Eisenmann, J.C.; Nicholson, B.; Till, K. Associations Between Motor Competence and Physical Activity, Physical Fitness and Psychosocial Characteristics in Adolescents: A Systematic Review and Meta-analysis. Sports Med. 2023, 53, 2191–2256. [Google Scholar] [CrossRef]
- Santos, G.D.; Guerra, P.H.; Milani, S.A.; Santos, A.B.D.; Cattuzzo, M.T.; Ré, A.H.N. Sedentary behavior and motor competence in children and adolescents: A review. Rev. Saude Publica 2021, 55, 57. [Google Scholar] [CrossRef]
- Bardid, F.; Vannozzi, G.; Logan, S.W.; Hardy, L.L.; Barnett, L.M. A hitchhiker’s guide to assessing young people’s motor competence: Deciding what method to use. J. Sci. Med. Sport 2019, 22, 311–318. [Google Scholar] [CrossRef]
- De Meester, A.; Barnett, L.M.; Brian, A.; Bowe, S.J.; Jiménez-Díaz, J.; Van Duyse, F.; Irwin, J.M.; Stodden, D.F.; D’hOndt, E.; Lenoir, M.; et al. The Relationship Between Actual and Perceived Motor Competence in Children, Adolescents and Young Adults: A Systematic Review and Meta-analysis. Sports Med. 2020, 50, 2001–2049. [Google Scholar] [CrossRef]
- Jiménez-Díaz, J.; Chaves-Castro, K.; Salazar, W. Effects of Different Movement Programs on Motor Competence: A Systematic Review With Meta-Analysis. J. Phys. Act. Health 2019, 16, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Khodaverdi, Z.; O’bRien, W.; Duncan, M.; Clark, C.C.T. Motor competence interventions in children and adolescents—Theoretical and atheoretical approaches: A systematic review. J. Sports Sci. 2022, 40, 2233–2266. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, M. Definition of physical literacy and clarification of related issues. ICSSPE Bull. J. Sport Sci. Phys. Educ. 2013, 65, 28–33. [Google Scholar]
- Keegan, R.J.; Barnett, L.M.; Dudley, D.A.; Telford, R.D.; Lubans, D.R.; Bryant, A.S.; Roberts, W.M.; Morgan, P.J.; Schranz, N.K.; Weissensteiner, J.R.; et al. Defining Physical Literacy for Application in Australia: A Modified Delphi Method. J. Teach. Phys. Educ. 2019, 38, 105–118. [Google Scholar] [CrossRef]
- Edwards, L.C.; Bryant, A.S.; Keegan, R.J.; Morgan, K.; Jones, A.M. Definitions, Foundations and Associations of Physical Literacy: A Systematic Review. Sports Med. 2016, 47, 113–126. [Google Scholar] [CrossRef]
- Cornish, K.; Fox, G.; Fyfe, T.; Koopmans, E.; Pousette, A.; Pelletier, C.A. Understanding physical literacy in the context of health: A rapid scoping review. BMC Public Health 2020, 20, 1569. [Google Scholar] [CrossRef]
- Shearer, C.; Goss, H.R.; Boddy, L.M.; Knowles, Z.R.; Durden-Myers, E.J.; Foweather, L. Assessments Related to the Physical, Affective and Cognitive Domains of Physical Literacy Amongst Children Aged 7–11.9 Years: A Systematic Review. Sports Med.-Open 2021, 7, 37. [Google Scholar] [CrossRef]
- de Dieu, H.J.; Zhou, K. Physical Literacy Assessment Tools: A Systematic Literature Review for Why, What, Who, and How. Int. J. Environ. Res. Public Health 2021, 18, 7954. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.; Glibo, I.; Koenen, K.; Samsudin, N. What Is Physical Literacy? An International Review and Analysis of Definitions. Kinesiol. Rev. 2023, 12, 247–260. [Google Scholar] [CrossRef]
- Whitehead, I.M. The concept of physical literacy. Eur. J. Phys. Educ. 2001, 6, 127–138. [Google Scholar] [CrossRef]
- Urbano-Mairena, J.; Castillo-Paredes, A.; Muñoz-Bermejo, L.; Denche-Zamorano, Á.; Rojo-Ramos, J.; Pastor-Cisneros, R.; Mendoza-Muñoz, M. A Bibliometric Analysis of Physical Literacy Studies in Relation to Health of Children and Adolescents. Children 2023, 10, 660. [Google Scholar] [CrossRef] [PubMed]
- Essiet, I.A.; Lander, N.J.; Salmon, J.; Duncan, M.J.; Eyre, E.L.J.; Ma, J.; Barnett, L.M. A systematic review of tools designed for teacher proxy-report of children’s physical literacy or constituting elements. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 131. [Google Scholar] [CrossRef]
- Anico, S.; Wilson, L.; Eyre, E.; Smith, E. The effectiveness of school-based run/walk programmes to develop physical literacy and physical activity components in primary school children: A systematic review. J. Sports Sci. 2022, 40, 2552–2569. [Google Scholar] [CrossRef]
- Carl, J.; Schmittwilken, L.; Pöppel, K. Development and evaluation of a school-based physical literacy intervention for children in Germany: Protocol of the PLACE study. Front. Sports Act. Living 2023, 5, 1155363. [Google Scholar] [CrossRef]
- Barnett, L.M.; Jerebine, A.; Keegan, R.; Watson-Mackie, K.; Arundell, L.; Ridgers, N.D.; Salmon, J.; Dudley, D. Validity, Reliability, and Feasibility of Physical Literacy Assessments Designed for School Children: A Systematic Review. Sports Med. 2023, 53, 1905–1929. [Google Scholar] [CrossRef] [PubMed]
- Rudd, J.R.; Pesce, C.; Strafford, B.W.; Davids, K. Physical Literacy—A Journey of Individual Enrichment: An Ecological Dynamics Rationale for Enhancing Performance and Physical Activity in All. Front. Psychol. 2020, 11, 1904. [Google Scholar] [CrossRef]
- Dobell, A.; Pringle, A.; Faghy, M.A.; Roscoe, C.M.P. Fundamental Movement Skills and Accelerometer-Measured Physical Activity Levels during Early Childhood: A Systematic Review. Children 2020, 7, 224. [Google Scholar] [CrossRef]
- Malambo, C.; Nová, A.; Clark, C.; Musálek, M. Associations between Fundamental Movement Skills, Physical Fitness, Motor Competency, Physical Activity, and Executive Functions in Pre-School Age Children: A Systematic Review. Children 2022, 9, 1059. [Google Scholar] [CrossRef]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M.; Okely, A.D. Fundamental movement skills in children and adolescents: Review of associated health benefits. Sports Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef] [PubMed]
- Xin, F.; Chen, S.-T.; Clark, C.; Hong, J.-T.; Liu, Y.; Cai, Y.-J. Relationship between Fundamental Movement Skills and Physical Activity in Preschool-aged Children: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 3566. [Google Scholar] [CrossRef]
- Jones, D.; Innerd, A.; Giles, E.L.; Azevedo, L.B. Association between fundamental motor skills and physical activity in the early years: A systematic review and meta-analysis. J. Sport Health Sci. 2020, 9, 542–552. [Google Scholar] [CrossRef]
- Xu, Z.; Shen, S.-J.; Wen, Y.-H. The relationship between fundamental movement skills and physical activity in preschoolers: A systematic review. Early Child Dev. Care 2024, 194, 323–334. [Google Scholar] [CrossRef]
- Barnett, L.M.; Verswijveren, S.J.J.M.; Colvin, B.; Lubans, D.R.; Telford, R.M.; Lander, N.J.; Schott, N.; Tietjens, M.; Hesketh, K.D.; Morgan, P.J.; et al. Motor skill competence and moderate- and vigorous-intensity physical activity: A linear and non-linear cross-sectional analysis of eight pooled trials. Int. J. Behav. Nutr. Phys. Act. 2024, 21, 14. [Google Scholar] [CrossRef]
- Zi, Y.; de Geus, E.J.C. Reviewing the association between motor competence and physical activity from a behavioral genetic perspective. Front. Psychol. 2025, 16, 1480631. [Google Scholar] [CrossRef]
- Cook, G.; Burton, L.; Hoogenboom, B. Pre-participation screening: The use of fundamental movements as an assessment of function—Part 1. N. Am. J. Sports Phys. Ther. 2006, 1, 62–72. [Google Scholar]
- Cook, G.; Burton, L.; Hoogenboom, B. Pre-participation screening: The use of fundamental movements as an assessment of function—Part 2. N. Am. J. Sports Phys. Ther. 2006, 1, 132–139. [Google Scholar]
- Vehrs, P.R.; Uvacsek, M.; Johnson, A.W. Assessment of Dysfunctional Movements and Asymmetries in Children and Adolescents Using the Functional Movement Screen—A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 12501. [Google Scholar] [CrossRef]
- O’bRien, W.; Khodaverdi, Z.; Bolger, L.; Tarantino, G.; Philpott, C.; Neville, R.D. The Assessment of Functional Movement in Children and Adolescents: A Systematic Review and Meta-Analysis. Sports Med. 2021, 52, 37–53. [Google Scholar] [CrossRef]
- Davies, K.F.; Sacko, R.S.; Lyons, M.A.; Duncan, M.J. Association between Functional Movement Screen Scores and Athletic Performance in Adolescents: A Systematic Review. Sports 2022, 10, 28. [Google Scholar] [CrossRef]
- Scheuer, C.; Herrmann, C.; Bund, A. Motor tests for primary school aged children: A systematic review. J. Sports Sci. 2018, 37, 1097–1112. [Google Scholar] [CrossRef] [PubMed]
- Cools, W.; De Martelaer, K.; Samaey, C.; Andries, C. Movement skill assessment of typically developing preschool children: A review of seven movement skill assessment tools. J. Sports Sci. Med. 2009, 8, 154–168. [Google Scholar] [PubMed]
- Zheng, Y.; Ye, W.; Korivi, M.; Liu, Y.; Hong, F. Gender Differences in Fundamental Motor Skills Proficiency in Children Aged 3–6 Years: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 8318. [Google Scholar] [CrossRef] [PubMed]
- Klingberg, B.; Schranz, N.; Barnett, L.M.; Booth, V.; Ferrar, K. The feasibility of fundamental movement skill assessments for pre-school aged children. J. Sports Sci. 2018, 37, 378–386. [Google Scholar] [CrossRef]
- Eddy, L.H.; Bingham, D.D.; Crossley, K.L.; Shahid, N.F.; Ellingham-Khan, M.; Otteslev, A.; Figueredo, N.S.; Mon-Williams, M.; Hill, L.J.B. The validity and reliability of observational assessment tools available to measure fundamental movement skills in school-age children: A systematic review. PLoS ONE 2020, 15, e0237919. [Google Scholar] [CrossRef]
- Hulteen, R.M.; Barnett, L.M.; True, L.; Lander, N.J.; Cruz, B.d.P.; Lonsdale, C. Validity and reliability evidence for motor competence assessments in children and adolescents: A systematic review. J. Sports Sci. 2020, 38, 1717–1798. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.C.T.; Bisi, M.C.; Duncan, M.J.; Stagni, R. Technology-based methods for the assessment of fine and gross motor skill in children: A systematic overview of available solutions and future steps for effective in-field use. J. Sports Sci. 2021, 39, 1236–1276. [Google Scholar] [CrossRef]
- Coe, D.P. Means of Optimizing Physical Activity in the Preschool Environment. Am. J. Lifestyle Med. 2018, 14, 16–23. [Google Scholar] [CrossRef]
- Johnstone, A.; Hughes, A.R.; Martin, A.; Reilly, J.J. Utilising active play interventions to promote physical activity and improve fundamental movement skills in children: A systematic review and meta-analysis. BMC Public Health 2018, 18, 789. [Google Scholar] [CrossRef]
- Engel, A.C.; Broderick, C.R.; van Doorn, N.; Hardy, L.L.; Parmenter, B.J. Exploring the Relationship Between Fundamental Motor Skill Interventions and Physical Activity Levels in Children: A Systematic Review and Meta-analysis. Sports Med. 2018, 48, 1845–1857. [Google Scholar] [CrossRef]
- Graham, M.; Azevedo, L.; Wright, M.; Innerd, A.L. The Effectiveness of Fundamental Movement Skill Interventions on Moderate to Vigorous Physical Activity Levels in 5- to 11-Year-Old Children: A Systematic Review and Meta-Analysis. Sports Med. 2021, 52, 1067–1090. [Google Scholar] [CrossRef]
- Jylänki, P.; Mbay, T.; Hakkarainen, A.; Sääkslahti, A.; Aunio, P. The effects of motor skill and physical activity interventions on preschoolers’ cognitive and academic skills: A systematic review. Prev. Med. 2022, 155, 106948. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.K.; Costigan, S.A.; Morgan, P.J.; Lubans, D.R.; Stodden, D.F.; Salmon, J.; Barnett, L.M. Do School-Based Interventions Focusing on Physical Activity, Fitness, or Fundamental Movement Skill Competency Produce a Sustained Impact in These Outcomes in Children and Adolescents? A Systematic Review of Follow-Up Studies. Sports Med. 2013, 44, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Van Capelle, A.; Broderick, C.R.; van Doorn, N.; Ward, R.E.; Parmenter, B.J. Interventions to improve fundamental motor skills in pre-school aged children: A systematic review and meta-analysis. J. Sci. Med. Sport 2017, 20, 658–666. [Google Scholar] [CrossRef]
- Morgan, P.J.; Barnett, L.M.; Cliff, D.P.; Okely, A.D.; Scott, H.A.; Cohen, K.E.; Lubans, D.R. Fundamental Movement Skill Interventions in Youth: A Systematic Review and Meta-analysis. Pediatrics 2013, 132, e1361–e1383. [Google Scholar] [CrossRef]
- Altunsöz, I.H.; Goodway, J.D. Skiping to Motor Competence: The Influence of Project Successful Kinesthetic Instruction for Preschoolers on Motor Competence of Disadvantaged Preschoolers. Phys. Educ. Sport Pedagog. 2016, 21, 366–385. [Google Scholar] [CrossRef]
- Brian, A.; Taunton, S. Effectiveness of motor skill intervention varies based on implementation strategy. Phys. Educ. Sport Pedagog. 2017, 23, 222–233. [Google Scholar] [CrossRef]
- Brian, A.; Goodway, J.D.; Logan, J.A.; Sutherland, S. SKIPing With Head Start Teachers: Influence of T-SKIP on Object-Control Skills. Res. Q. Exerc. Sport 2017, 88, 479–491. [Google Scholar] [CrossRef]
- Brian, A.; Goodway, J.D.; Logan, J.A.; Sutherland, S. SKIPing with teachers: An early years motor skill intervention. Phys. Educ. Sport Pedagog. 2016, 22, 270–282. [Google Scholar] [CrossRef]
- Iivonen, S.; Sääkslahti, A.; Nissinen, K. The Development of Fundamental Motor Skills of Four-to Five-Year-Old Preschool Children and the Effects of a Preschool Physical Education Curriculum. Early Child Dev. Care 2011, 181, 335–343. [Google Scholar] [CrossRef]
- Palmer, K.K.; Chinn, K.M.; Robinson, L.E. The Effect of the CHAMP Intervention on Fundamental Motor Skills and Outdoor Physical Activity in Preschoolers. J. Sport Health Sci. 2019, 8, 98–105. [Google Scholar] [CrossRef]
- Foulkes, J.D.; Knowles, Z.; Fairclough, S.J.; Stratton, G.; O’dwyer, M.; Ridgers, N.D.; Foweather, L. Effect of a 6-Week Active Play Intervention on Fundamental Movement Skill Competence of Preschool Children. Percept. Mot. Ski. 2017, 124, 393–412. [Google Scholar] [CrossRef] [PubMed]
- Flynn, R.J.; Pringle, A.; Roscoe, C.M.P. Direct Parent Engagement to Improve Fundamental Movement Skills in Children: A Systematic Review. Children 2023, 10, 1247. [Google Scholar] [CrossRef]
- Ramires, V.V.; dos Santos, P.C.; Filho, V.C.B.; Bandeira, A.d.S.; Tenório, M.C.M.; de Camargo, E.M.; Ravagnani, F.C.d.P.; Sandreschi, P.; de Oliveira, V.J.M.; Hallal, P.C.; et al. Physical Education for Health Among School-Aged Children and Adolescents: A Scoping Review of Reviews. J. Phys. Act. Health 2023, 20, 586–599. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Alonso-Martínez, A.M.; Ramírez-Vélez, R.; Pérez-Sousa, M.Á.; Ramírez-Campillo, R.; Izquierdo, M. Association of Physical Education With Improvement of Health-Related Physical Fitness Outcomes and Fundamental Motor Skills Among Youths. JAMA Pediatr. 2020, 174, e200223. [Google Scholar] [CrossRef]
- Liu, W.; Zeng, N.; McDonough, D.J.; Gao, Z. Effect of Active Video Games on Healthy Children’s Fundamental Motor Skills and Physical Fitness: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8264. [Google Scholar] [CrossRef]
- Hassan, M.A.; Liu, W.; McDonough, D.J.; Su, X.; Gao, Z. Comparative Effectiveness of Physical Activity Intervention Programs on Motor Skills in Children and Adolescents: A Systematic Review and Network Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 11914. [Google Scholar] [CrossRef]
- Oppici, L.; Stell, F.M.; Utesch, T.; Woods, C.T.; Foweather, L.; Rudd, J.R. A Skill Acquisition Perspective on the Impact of Exergaming Technology on Foundational Movement Skill Development in Children 3–12 Years: A Systematic Review and Meta-analysis. Sports Med.-Open 2022, 8, 148. [Google Scholar] [CrossRef]
- Comeras-Chueca, C.; Marin-Puyalto, J.; Matute-Llorente, A.; Vicente-Rodriguez, G.; Casajus, J.A.; Gonzalez-Aguero, A. The Effects of Active Video Games on Health-Related Physical Fitness and Motor Competence in Children and Adolescents with Healthy Weight: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6965. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Valkanover, S.; Roebers, C.; Conzelmann, A. Promoting a functional physical self-concept in physical education: Evaluation of a 10-week intervention. Eur. Phys. Educ. Rev. 2013, 19, 232–255. [Google Scholar] [CrossRef]
- Collins, H.; Booth, J.N.; Duncan, A.; Fawkner, S. The effect of resistance training interventions on fundamental movement skills in youth: A meta-analysis. Sports Med.-Open 2019, 5, 17. [Google Scholar] [CrossRef]
- Lin, J.; Zhang, R.; Shen, J.; Zhou, A. Effects of school-based neuromuscular training on fundamental movement skills and physical fitness in children: A systematic review. PeerJ 2022, 10, e13726. [Google Scholar] [CrossRef] [PubMed]
- Strieter, L.; Arena, R.; Huizar, M. Moving more and sitting less in schools: What’s the next step? Prog. Cardiovasc. Dis. 2021, 64, 22–26. [Google Scholar] [CrossRef]
- Cowley, J.G.; McIntosh, I.; Kiely, J.; Collins, D.J. The post 16 gap: How do young people conceptualise PE? An exploration of the barriers to participation in physical education, physical activity and sport in senior school pupils. Int. J. Adolesc. Med. Health 2020, 33, 313–321. [Google Scholar] [CrossRef] [PubMed]
- van Abswoude, F.; Mombarg, R.; de Groot, W.; Spruijtenburg, G.E.; Steenbergen, B. Implicit motor learning in primary school children: A systematic review. J. Sports Sci. 2021, 39, 2577–2595. [Google Scholar] [CrossRef]
- Filho, V.C.B.; Pereira, W.M.G.; Farias, B.d.O.; Moreira, T.M.M.; Guerra, P.H.; Queiroz, A.C.M.; de Castro, V.H.S.; Silva, K.S. Scoping Review on Interventions for Physical Activity and Physical Literacy Components in Brazilian School-Aged Children and Adolescents. Int. J. Environ. Res. Public Health 2021, 18, 8349. [Google Scholar] [CrossRef]
- Petrigna, L.; Thomas, E.; Brusa, J.; Rizzo, F.; Scardina, A.; Galassi, C.; Verde, D.L.; Caramazza, G.; Bellafiore, M. Does Learning Through Movement Improve Academic Performance in Primary Schoolchildren? A Systematic Review. Front. Pediatr. 2022, 10, 841582. [Google Scholar] [CrossRef]
- Jerebine, A.; Fitton-Davies, K.; Lander, N.; Eyre, E.L.J.; Duncan, M.J.; Barnett, L.M. “All the fun stuff, the teachers say, ‘that’s dangerous!’” Hearing from children on safety and risk in active play in schools: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 72. [Google Scholar] [CrossRef]
- Li, B.; Liu, J.; Ying, B. Physical education interventions improve the fundamental movement skills in kindergarten: A systematic review and meta-analysis. Food Sci. Technol. 2022, 42, e46721. [Google Scholar] [CrossRef]
- Reilly, T.; Williams, A.M.; Nevill, A.; Franks, A. A multidisciplinary approach to talent identification in soccer. J. Sports Sci. 2000, 18, 695–702. [Google Scholar] [CrossRef]
- Mao, X.; Zhang, J.; Li, Y.; Cao, Y.; Ding, M.; Li, W.; Fan, L. The effects of football practice on children’s fundamental movement skills: A systematic review and meta-analysis. Front. Pediatr. 2022, 10, 1019150. [Google Scholar] [CrossRef]
- Al Attar, W.S.A.; Bizzini, M.; Alzahrani, H.; Alarifi, S.; Ghulam, H.; Alyami, M.; Alzhrani, M.; Sanders, R.H. The FIFA 11+ Kids Injury Prevention Program Reduces Injury Rates Among Male Children Soccer Players: A Clustered Randomized Controlled Trial. Sports Health A Multidiscip. Approach 2022, 15, 397–409. [Google Scholar] [CrossRef] [PubMed]
- Jimenez-Garcia, J.A.; Miller, M.B.; DeMont, R.G. Effects of Multicomponent Injury Prevention Programs on Children and Adolescents’ Fundamental Movement Skills: A Systematic Review With Meta-Analyses. Am. J. Health Promot. 2022, 37, 705–719. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, L.; Roscoe, C.M.P. The Impact of Swimming on Fundamental Movement Skill Development in Children (3–11 Years): A Systematic Literature Review. Children 2023, 10, 1411. [Google Scholar] [CrossRef]
- Lorås, H. The Effects of Physical Education on Motor Competence in Children and Adolescents: A Systematic Review and Meta-Analysis. Sports 2020, 8, 88. [Google Scholar] [CrossRef] [PubMed]
- Lander, N.; Eather, N.; Morgan, P.J.; Salmon, J.; Barnett, L.M. Characteristics of Teacher Training in School-Based Physical Education Interventions to Improve Fundamental Movement Skills and/or Physical Activity: A Systematic Review. Sports Med. 2016, 47, 135–161. [Google Scholar] [CrossRef]
- Buckler, E.J.; Faulkner, G.E.; Beauchamp, M.R.; Rizzardo, B.; DeSouza, L.; Puterman, E. A Systematic Review of Educator-Led Physical Literacy and Activity Interventions. Am. J. Prev. Med. 2023, 64, 742–760. [Google Scholar] [CrossRef]
- van Beurden, E.; Zask, A.; Barnett, L.; Dietrich, U. Fundamental movement skills—How do primary school children perform? The ‘Move it Groove it’ program in rural Australia. J. Sci. Med. Sport 2002, 5, 244–252. [Google Scholar] [CrossRef]
- Tompsett, C.; Sanders, R.; Taylor, C.; Cobley, S. Pedagogical Approaches to and Effects of Fundamental Movement Skill Interventions on Health Outcomes: A Systematic Review. Sports Med. 2017, 47, 1795–1819. [Google Scholar] [CrossRef]
- Ma, J.; Lander, N.; Eyre, E.L.J.; Barnett, L.M.; Essiet, I.A.; Duncan, M.J. It’s Not Just What You Do but the Way You Do It: A Systematic Review of Process Evaluation of Interventions to Improve Gross Motor Competence. Sports Med. 2021, 51, 2547–2569. [Google Scholar] [CrossRef]
- O’brien, W.; Khodaverdi, Z.; Bolger, L.; Murphy, O.; Philpott, C.; Kearney, P.E. Exploring Recommendations for Child and Adolescent Fundamental Movement Skills Development: A Narrative Review. Int. J. Environ. Res. Public Health 2023, 20, 3278. [Google Scholar] [CrossRef]
- Eguia, K.F.; Ng, S.S.M.; Wong, T.W.L. Attentional Focus Strategies for Promoting Children’s Motor Learning: A Scoping Review With a Learner-Task-Environment Framework. Percept. Mot. Ski. 2023, 130, 2700–2722. [Google Scholar] [CrossRef]
- Flôres, F.S.; Rodrigues, L.P.; Copetti, F.; Lopes, F.; Cordovil, R. Affordances for Motor Skill Development in Home, School, and Sport Environments: A Narrative Review. Percept. Mot. Ski. 2019, 126, 366–388. [Google Scholar] [CrossRef] [PubMed]
- Fasting, M.L.; Høyem, J. Freedom, joy and wonder as existential categories of childhood—Reflections on experiences and memories of outdoor play. J. Adventure Educ. Outdoor Learn. 2022, 24, 145–158. [Google Scholar] [CrossRef]
- Richard, V.; Holder, D.; Cairney, J. Creativity in Motion: Examining the Creative Potential System and Enriched Movement Activities as a Way to Ignite It. Front. Psychol. 2021, 12, 690710. [Google Scholar] [CrossRef]
- Feleszko, W.; Makrinioti, H.; Nalej, M.; Ooka, T.; Zhu, Z.; Sullivan, A.F.; Jartti, T.; Hasegawa, K.; Camargo, C.A. Early-life exposure to residential greenness and risk of asthma in a U.S. bronchiolitis cohort. Allergy 2024, 79, 3036–3046. [Google Scholar] [CrossRef]
- Houser, N.E.; Roach, L.; Stone, M.R.; Turner, J.; Kirk, S.F. Let the Children Play: Scoping Review on the Implementation and Use of Loose Parts for Promoting Physical Activity Participation. AIMS Public Health 2016, 3, 781–799. [Google Scholar] [CrossRef]
- Johnstone, A.; McCrorie, P.; Cordovil, R.; Fjørtoft, I.; Iivonen, S.; Jidovtseff, B.; Lopes, F.; Reilly, J.J.; Thomson, H.; Wells, V.; et al. Nature-Based Early Childhood Education and Children’s Physical Activity, Sedentary Behavior, Motor Competence, and Other Physical Health Outcomes: A Mixed-Methods Systematic Review. J. Phys. Act. Health 2022, 19, 456–472. [Google Scholar] [CrossRef] [PubMed]
- Hansford, H.J.; A Wewege, M.; Cashin, A.G.; Hagstrom, A.D.; Clifford, B.K.; McAuley, J.H.; Jones, M.D. If exercise is medicine, why don’t we know the dose? An overview of systematic reviews assessing reporting quality of exercise interventions in health and disease. Br. J. Sports Med. 2022, 56, 692–700. [Google Scholar] [CrossRef]
- Lubans, D.R.; Lonsdale, C.; Cohen, K.; Eather, N.; Beauchamp, M.R.; Morgan, P.J.; Sylvester, B.D.; Smith, J.J. Framework for the design and delivery of organized physical activity sessions for children and adolescents: Rationale and description of the ‘SAAFE’ teaching principles. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 24. [Google Scholar] [CrossRef]
- Robinson, L.E. Effect of a Mastery Climate Motor Program on Object Control Skills and Perceived Physical Competence in Preschoolers. Res. Q. Exerc. Sport 2011, 82, 355–359. [Google Scholar] [CrossRef] [PubMed]
- Grace, B.; Lucas, C.T.; Shetgiri, R.; Cardenas, K.; de la Garza, G.P.; Pak, Y.; Yee, J.K. Physical Activity Counseling and Documentation by Pediatric Residents in Primary Care: Before and After Introduction of the FITT Principle. Clin. Pediatr. 2022, 62, 449–455. [Google Scholar] [CrossRef]
- Lubans, D.R.; Smith, J.J.; Plotnikoff, R.C.; Dally, K.A.; Okely, A.D.; Salmon, J.; Morgan, P.J. Assessing the sustained impact of a school-based obesity prevention program for adolescent boys: The ATLAS cluster randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 92. [Google Scholar] [CrossRef] [PubMed]
- Kirk, M.A.; Rhodes, R.E. Motor skill interventions to improve fundamental movement skills of preschoolers with developmental delay. Adapt. Phys. Act. Q. 2011, 28, 210–232. [Google Scholar] [CrossRef]
- Kavanagh, H.; Manninen, M.; Issartel, J. Comparing the fundamental movement skill proficiency of children with intellectual disabilities and typically developing children: A systematic review and meta-analysis. J. Intellect. Disabil. Res. 2023, 67, 1336–1353. [Google Scholar] [CrossRef]
- Foulder-Hughes, L.A.; Cooke, R.W. Motor, cognitive, and behavioural disorders in children born very preterm. Dev. Med. Child Neurol. 2003, 45, 97–103. [Google Scholar] [CrossRef]
- Kahlon, S.; Brubacher-Cressman, K.; Caron, E.; Ramonov, K.; Taubman, R.; Berg, K.; Wright, F.V.; Hilderley, A.J. Opening the Door to Physical Activity for Children With Cerebral Palsy: Experiences of Participants in the BeFAST or BeSTRONG Program. Adapt. Phys. Act. Q. 2019, 36, 202–222. [Google Scholar] [CrossRef]
- Joschtel, B.; Gomersall, S.R.; Tweedy, S.; Petsky, H.; Chang, A.B.; Trost, S.G. Fundamental movement skill proficiency and objectively measured physical activity in children with bronchiectasis: A cross-sectional study. BMC Pulm. Med. 2021, 21, 269. [Google Scholar] [CrossRef] [PubMed]
- Joschtel, B.; Gomersall, S.R.; Tweedy, S.; Petsky, H.; Chang, A.B.; Trost, S.G. Effects of a therapeutic exercise program in children with non-cystic fibrosis bronchiectasis: A pilot randomized controlled trial. Front. Pediatr. 2022, 10, 953429. [Google Scholar] [CrossRef]
- Holm, I.; Fredriksen, P.M.; Fosdahl, M.A.; Olstad, M.; Vøllestad, N. Impaired Motor Competence in School-aged Children With Complex Congenital Heart Disease. Arch. Pediatr. Adolesc. Med. 2007, 161, 945–950. [Google Scholar] [CrossRef]
- Almaas, R.; Jensen, U.; Loennecken, M.C.; Tveter, A.T.; Sanengen, T.; Scholz, T.; Holm, I. Impaired Motor Competence in Children With Transplanted Liver. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 723–728. [Google Scholar] [CrossRef] [PubMed]
- Naumann, F.L.; Hunt, M.; Ali, D.; Wakefield, C.E.; Moultrie, K.; Cohn, R.J. Assessment of Fundamental Movement Skills in Childhood Cancer Patients. Pediatr. Blood Cancer 2015, 62, 2211–2215. [Google Scholar] [CrossRef]
- Riet, D.C.M.D.; Engelbert, R.H.H.; VAN Genderen, F.R.; Ronde, M.T.M.T.H.; DE Goede-Bolder, A.; Hartman, A. Physical fitness in children with haemophilia and the effect of overweight. Haemophilia 2009, 15, 519–527. [Google Scholar] [CrossRef]
- O Olusanya, B.; Halpern, R.; Cheung, V.G.; Nair, M.K.C.; Boo, N.Y.; Hadders-Algra, M. Disability in children: A global problem needing a well-coordinated global action. BMJ Paediatr. Open 2022, 6, e001397. [Google Scholar] [CrossRef]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. New York: United Nations; 2015. Available online: https://sdgs.un.org/2030agenda (accessed on 10 January 2024).
- Lobelo, F.; Muth, N.D.; Hanson, S.; Nemeth, B.A.; Council on Sports Medicine and Fitness, Section on Obesity. Physical Activity Assessment and Counseling in Pediatric Clinical Settings. Pediatrics 2020, 145, e20193992. [Google Scholar] [CrossRef]
- Rosenbaum, P.; Gorter, J.W. The ‘F-words’ in childhood disability: I swear this is how we should think! Child Care Health Dev. 2012, 38, 457–463. [Google Scholar] [CrossRef]
- Eddy, L.H.; Wood, M.L.; Shire, K.A.; Bingham, D.D.; Bonnick, E.; Creaser, A.; Mon-Williams, M.; Hill, L.J. A systematic review of randomized and case-controlled trials investigating the effectiveness of school-based motor skill interventions in 3- to 12-year-old children. Child Care Health Dev. 2019, 45, 773–790. [Google Scholar] [CrossRef] [PubMed]
- Faigenbaum, A.D.; Rebullido, T.R.; Chulvi-Medrano, I. Youth Physical Activity Is All About the “F-Words”. Strength Cond. J. 2020, 42, 2–6. [Google Scholar] [CrossRef]
- Faigenbaum, A.D.; MacDonald, J.P.; Stracciolini, A.; Rebullido, T.R. From Hierarchy to Harmony: Transforming the Activity Pyramid into My Physical Activity Plate. Curr. Sports Med. Rep. 2025, 24, 137–139. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, L.S.; dos Santos, J.C.C. The era of pediatric physical illiteracy: A global call to address the Pediatric Inactivity Triad. Pediatr. Res. 2025. [Google Scholar] [CrossRef]

| Category (Number of Accepted Articles for Detailed Analysis) | Most Recent Paper Included for Detailed Analysis |
|---|---|
| Discussing FMSs and motor development (N = 11) | Wang JW, et al. Global hotspots and trends in research on preschool children’s motor development from 2012 to 2022: a bibliometric analysis [28]. |
| Concepts/terms used in the FMS context: motor competence, physical literacy (N = 8) | Grauduszus M, et al. Definitions and assessments of physical literacy among children and youth: a scoping review [30]. |
| Relationship between FMSs and other parameters (N = 15) | Liu Y, et al. The Bidirectional Correlation between Fundamental Motor Skill and Moderate-to-Vigorous Physical Activities: A Systematic Review and Meta-Analysis [31]. |
| Tools for FMS assessment (N = 14) | Nagy ÁV, et al. Assessment Tools Measuring Fundamental Movement Skills of Primary School Children: A Narrative Review in Methodological Perspective [32]. |
| Intervention effects on FMSs (N = 47) | Jerebine A, et al. Educator-Perceived Barriers and Facilitators to Structured-Physical Activity in Early Childhood Centres: A Systematic Review [33]. |
| First Author and Reference | Article Offers Complementary Perspectives on: |
|---|---|
| Scheuer et al. [79] | Motor testing instruments used in primary school settings by reviewing and synthesizing their theoretical frameworks, psychometric properties, and areas of application, while highlighting the distinctions between tests based on motor abilities, motor skills, and motor competencies constructs |
| Cools et al. [80] | Movement skill assessment tools by comparing seven standardized instruments used for evaluating FMSs in typically developing preschool children, examining their content validity, reliability, administrative feasibility, and normative data quality across European and international contexts |
| Klingberg et al. [82] | The feasibility of 13 FMS assessment tools available for use with pre-school aged children (3–6 years), providing a systematic comparison of considerations such as administration time, equipment requirements, space needs, training demands, and qualification requirements |
| Eddy et al. [83] | The validity and reliability of 24 observational FMS assessment tools for school-aged children by examining their psychometric properties through the COSMIN framework to evaluate their suitability for universal screening in educational settings |
| Hulteen et al. [84] | The validity and reliability of 57 motor competence assessments in children and adolescents providing complementary perspectives on (1) measurement properties across diverse populations—examining both child (3–12 years) and adolescent (13–17 years) populations; (2) multiple assessment approaches—including process-oriented, product-oriented, and hybrid assessments, as well as single-skill and battery assessments; (3) comprehensive measurement properties—examining content validity, construct validity, criterion validity, internal consistency, test-retest reliability, intra-rater reliability, and inter-rater reliability; and (4) assessment content and prevalence |
| Nagy et al. [32] | FMS assessment tools by analyzing them from a methodological perspective, examining their test items, tools, time requirements, and the specific types of FMSs they measure, rather than focusing solely on psychometric properties like validity and reliability |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piotrowski, T.; Makaruk, H.; Tekień, E.; Feleszko, W.; Kołodziej, M.; Albrecht, K.; Grela, K.; Makuch, R.; Werner, B.; Gąsior, J.S. Fundamental Movement/Motor Skills as an Important Component of Physical Literacy and Bridge to Physical Activity: A Scoping Review. Children 2025, 12, 1406. https://doi.org/10.3390/children12101406
Piotrowski T, Makaruk H, Tekień E, Feleszko W, Kołodziej M, Albrecht K, Grela K, Makuch R, Werner B, Gąsior JS. Fundamental Movement/Motor Skills as an Important Component of Physical Literacy and Bridge to Physical Activity: A Scoping Review. Children. 2025; 12(10):1406. https://doi.org/10.3390/children12101406
Chicago/Turabian StylePiotrowski, Tomasz, Hubert Makaruk, Edyta Tekień, Wojciech Feleszko, Maciej Kołodziej, Katarzyna Albrecht, Krystyna Grela, Robert Makuch, Bożena Werner, and Jakub S. Gąsior. 2025. "Fundamental Movement/Motor Skills as an Important Component of Physical Literacy and Bridge to Physical Activity: A Scoping Review" Children 12, no. 10: 1406. https://doi.org/10.3390/children12101406
APA StylePiotrowski, T., Makaruk, H., Tekień, E., Feleszko, W., Kołodziej, M., Albrecht, K., Grela, K., Makuch, R., Werner, B., & Gąsior, J. S. (2025). Fundamental Movement/Motor Skills as an Important Component of Physical Literacy and Bridge to Physical Activity: A Scoping Review. Children, 12(10), 1406. https://doi.org/10.3390/children12101406









