Sex-Based Anatomical Variations and Complication Risks in Pediatric Both-Bone Forearm Fractures: A Level of Evidence IV Retrospective Analysis
Abstract
Highlights
- The study demonstrated that boys with both-bone forearm fractures had greater initial radius angulation and longer forearm bones compared to girls. Surgical intervention was required only in boys, whereas overall complication rates did not differ significantly between sexes.
- These results indicate that male-specific anatomical characteristics predispose boys to unstable fracture patterns and a higher likelihood of surgical treatment. Considering sex-based anatomical differences in treatment planning may improve early risk stratification and guide timely surgical decisions.
Abstract
1. Introduction
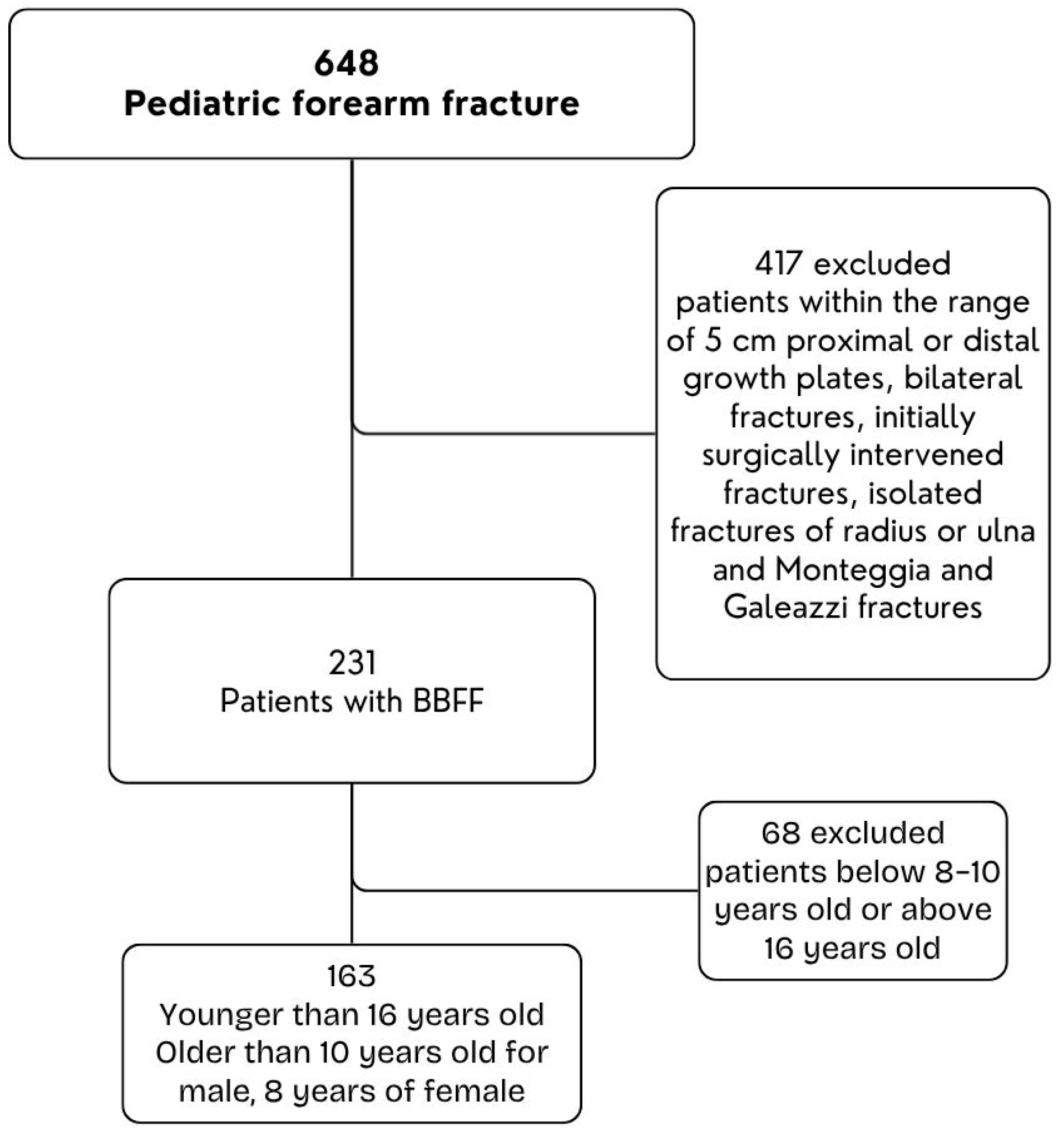
2. Materials and Methods
3. Fracture Management
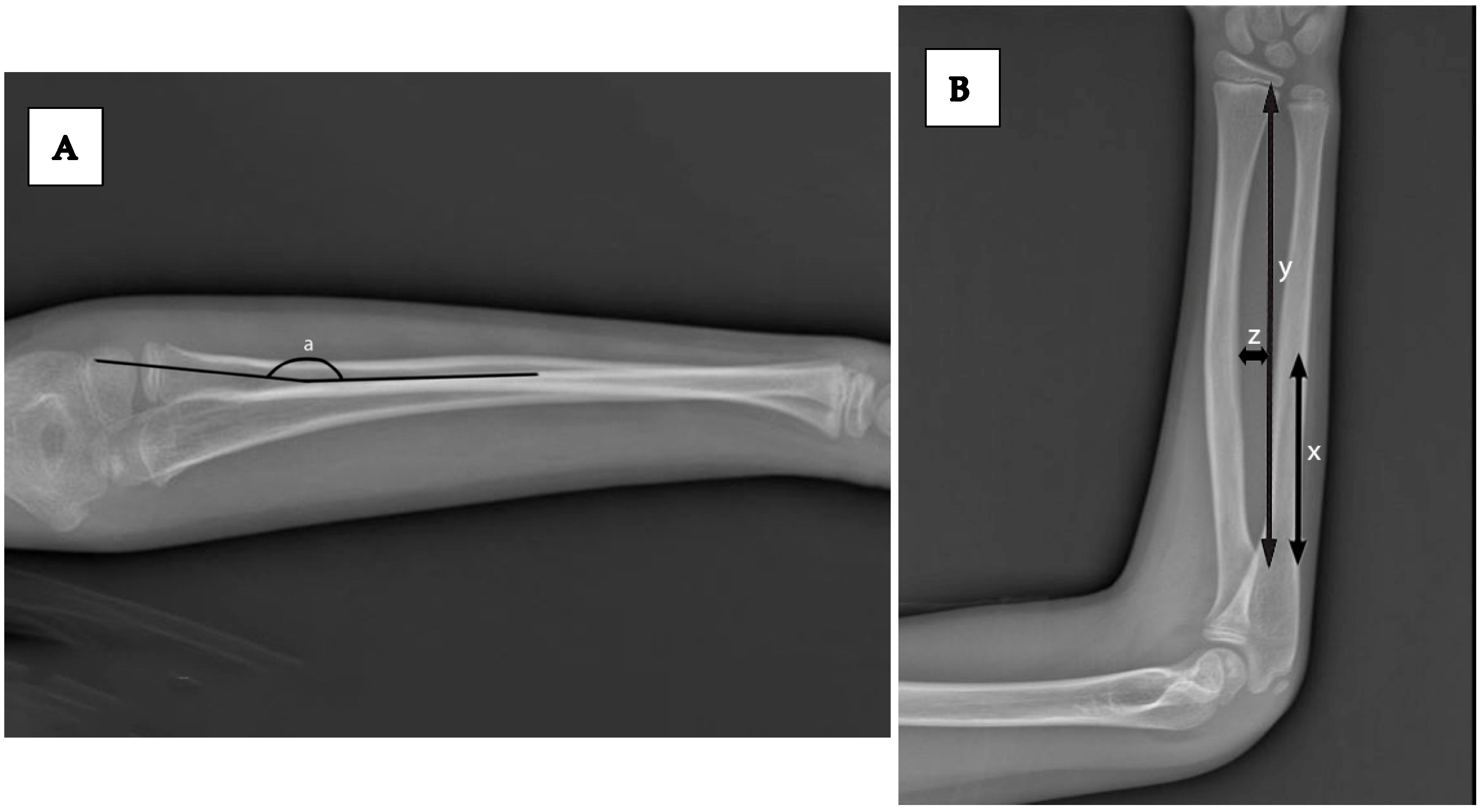
4. Radiographic Measurements
- Angulation of radius and ulna in AP and lateral views
- Bone length (radius and ulna) on the unaffected side
5. Outcome Measures
- Anatomical differences between sexes (angulation, bone length, bow characteristics)
- Complication rates (major: re-reduction failure, loss of reduction, need for surgery, pre-compartment syndrome; minor: swelling, mild post-reduction pain, tenderness)
- Surgical intervention rates
- Time to radiographic healing (defined as callus bridging the fracture gap in at least three cortices)
Statistical Analysis
6. Results
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Landin, L.A. Epidemiology of children’s fractures. J. Pediatr. Orthop. 1997, 6, 79–83. [Google Scholar] [CrossRef]
- Worlock, P.; Stower, M. Fracture patterns in Nottingham children. J. Pediatr. Orthop. 1986, 6, 656–660. [Google Scholar] [CrossRef]
- Cooper, C.; Dennison, E.M.; Leufkens, H.G.; Bishop, N.; van Staa, T.P. Epidemiology of childhood fractures in Britain: A study using the general practice research database. J. Bone Miner. Res. 2004, 19, 1976–1981. [Google Scholar] [CrossRef]
- Mäyränpää, M.K.; Mäkitie, O.; Kallio, P.E. Decreasing incidence and changing pattern of childhood fractures: A population-based study. J. Bone Miner. Res. 2010, 25, 2752–2759. [Google Scholar] [CrossRef]
- Chia, B.; Kozin, S.H.; Herman, M.J.; Safier, S.; Abzug, J.M. 44 Complications of pediatric distal radius and forearm fractures. Instr. Course Lect. 2015, 64, 499–508. [Google Scholar]
- Mehlman, C.T.; Wall, E.J. Injuries to the shafts of the radius and ulna. In Rockwood and Wilkins’ Fractures in Children, 6th ed.; Beaty, J.H., Kasser, J.R., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006; pp. 399–840. [Google Scholar]
- Bould, M.; Bannister, G. Refractures of the radius and ulna in children. Injury 1999, 30, 583–586. [Google Scholar] [CrossRef] [PubMed]
- Kailis, V.; Hariga, H.; Docquier, P.-L. Prevention of re-fractures of both bones of the forearm in children. Acta Orthop. Belg. 2016, 82, 872–875. [Google Scholar] [PubMed]
- Kay, S.; Smith, C.; Oppenheim, W.L. Both-bone midshaft forearm fractures in children. J. Pediatr. Orthop. 1986, 6, 306–310. [Google Scholar] [CrossRef] [PubMed]
- Caruso, G.; Caldari, E.; Sturla, F.D.; Caldaria, A.; Re, D.L.; Pagetti, P.; Palummieri, F.; Massari, L. Management of pediatric forearm fractures: What is the best therapeutic choice? A narrative review of the literature. Musculoskelet. Surg. 2021, 105, 225–234. [Google Scholar] [CrossRef]
- Teoh, K.H.; Chee, Y.-H.; Shortt, N.; Wilkinson, G.; Porter, D.E. An age-and sex-matched comparative study on both-bone diaphyseal paediatric forearm fracture. J. Child. Orthop. 2009, 3, 367–373. [Google Scholar] [CrossRef]
- Ryan, L.M.; Teach, S.J.; Searcy, K.; Singer, S.A.; Wood, R.; Wright, J.L.; Chamberlain, J.M. Epidemiology of Pediatric Forearm Fractures in Washington, DC. J. Trauma Acute Care Surg. 2010, 69, S200–S205. [Google Scholar]
- Bowman, E.N.; Mehlman, C.T.; Lindsell, C.J.; Tamai, J. Nonoperative treatment of both-bone forearm shaft fractures in children: Predictors of early radiographic failure. J. Pediatr. Orthop. 2011, 31, 23–32. [Google Scholar] [CrossRef]
- Schemitsch, E.H.; Richards, R.R. The effect of malunion on functional outcome after plate fixation of fractures of both bones of the forearm in adults. JBJS 1992, 74, 1068–1078. [Google Scholar] [CrossRef]
- Firl, M.; Wünsch, L. Measurement of bowing of the radius. J. Bone Jt. Surg. Br. Vol. 2004, 86, 1047–1049. [Google Scholar] [CrossRef]
- Flynn, J.M.; Waters, P.M. Single-bone fixation of both-bone forearm fractures. J. Pediatr. Orthop. 1996, 16, 655–659. [Google Scholar] [CrossRef]
- Lascombes, P.; Prevot, J.; Ligier, J.; Metaizeau, J.; Poncelet, T. Elastic stable intramedullary nailing in forearm shaft fractures in children: 85 cases. J. Pediatr. Orthop. 1990, 10, 167–171. [Google Scholar] [CrossRef]
- Shoemaker, S.D.; Comstock, C.P.; Mubarak, S.J.; Wenger, D.R.; Chambers, H.G. Intramedullary Kirschner wire fixation of open or unstable forearm fractures in children. J. Pediatr. Orthop. 1999, 19, 329–337. [Google Scholar] [CrossRef]
- Van der Reis, W.L.; Otsuka, N.Y.; Moroz, P.; Mah, J. Intramedullary nailing versus plate fixation for unstable forearm fractures in children. J. Pediatr. Orthop. 1998, 18, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.C.; Ng, B.; Ying, S.; Lam, P. A 10-year study of the changes in the pattern and treatment of 6493 fractures. J. Pediatr. Orthop. 1999, 19, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Sinikumpu, J.-J.; Lautamo, A.; Pokka, T.; Serlo, W. Complications and radiographic outcome of children’s both-bone diaphyseal forearm fractures after invasive and non-invasive treatment. Injury 2013, 44, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Bochang, C.; Katz, K.; Weigl, D.; Yang, J.; Wang, Z.; Bar-On, E. Are frequent radiographs necessary in the management of closed forearm fractures in children? J. Child. Orthop. 2008, 2, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Soumekh, L.; Sylvanus, T.; Karlen, A.; Wahl, C.; Huser, A.J.; Truong, W.H. Refracture rate of both bone forearm fractures: A retrospective comparison of casting alone versus casting and extended functional bracing. J. Pediatr. Orthop. 2021, 41, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Monga, P.; Raghupathy, A.; Courtman, N.H. Factors affecting remanipulation in paediatric forearm fractures. J. Pediatr. Orthop. B 2010, 19, 181–187. [Google Scholar] [CrossRef]
- Price, C.T.; Scott, D.S.; Kurzner, M.E.; Flynn, J.C. Malunited forearm fractures in children. J. Pediatr. Orthop. 1990, 10, 705–712. [Google Scholar] [CrossRef]
- Högström, H.; Nllsson, B.E.; Wlllner, S. Correction with growth following diaphyseal forearm fracture. Acta Orthop. Scand. 1976, 47, 299–303. [Google Scholar] [PubMed]
- Fuller, D.; McCullough, C. Malunited fractures of the forearm in children. J. Bone Jt. Surg. Br. Vol. 1982, 64, 364–367. [Google Scholar] [CrossRef]
- Daruwalla, J.S. A study of radioulnar movements following fractures of the forearm in children. Clin. Orthop. Relat. Res. (1976–2007) 1979, 139, 114–120. [Google Scholar] [CrossRef]
- Matthews, L.S.; Kaufer, H.; Garver, D.; Sonstegard, D. The effect on supination-pronation of angular malalignment of fractures of both bones of the forearm. JBJS 1982, 64, 14–17. [Google Scholar]
- Zionts, L.E.; Zalavras, C.G.; Gerhardt, M.B. Closed treatment of displaced diaphyseal both-bone forearm fractures in older children and adolescents. J. Pediatr. Orthop. 2005, 25, 507–512. [Google Scholar] [CrossRef]
- Husum, H.C.; Rahbek, O.; Søjbjerg, J.O.; Nissen, K.A.; Rahbek, C. The risk of refracture and malunion in children treated for diaphyseal forearm fractures: A retrospective cohort study. Acta Orthop. 2025, 96, 189–194. [Google Scholar] [CrossRef]
- Wang, B.; Guo, J.; Li, Z.; Ji, Z.; Liu, F.; Sun, K.; Feng, W. Pediatric distal both-bone forearm fractures treated with percutaneous pinning with or without ulna fixation: A retrospective cohort study from two centres. BMC Musculoskelet. Disord. 2024, 25, 683. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.M.; Said, E.; Addosooki, A.; Attya, H.A.; Awad, A.K.; Ahmed, E.H.; Tammam, H. Intramedullary versus plate fixation of both bone forearm fractures in skeletally immature patients: A systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 2263–2278. [Google Scholar] [CrossRef] [PubMed]
| N (%) | 95% CI | ||
|---|---|---|---|
| Sex | Male | 129 (79.1%) | 72.2–84.5% |
| Female | 34 (20.9%) | 15.5–27.8% | |
| Age (Mean, ±SD) | 11.5 (±1.6) | 11.0–12.0% | |
| Side | Left | 101 (62.0%) | 54.4–69.0% |
| Right | 62 (39.0%) | 31.0–45.6% |
| Sex | ||||||
|---|---|---|---|---|---|---|
| Male | Female | |||||
| Median (IQR (25; 75) ***) [95% CI] | Median (IQR (25; 75)) [95% CI] | p * Raw Value | Adjusted p † (BH-FDR) | D ** Cohen | ||
| Radius Angulation on AP View | Initial | 9.8 (4.2; 17.1) [8.6–11.7] | 8.4 (1.7; 13.1) [5.4–12.3] | 0.314 | 0.48 | 0.177 |
| Post-reduction | 2.0 (1.1; 4.3) [1.8–2.8] | 2.2 (0.9; 4.1) [1.5–2.4] | 0.962 | 0.96 | 0.008 | |
| Change | 7.4 (0.4; 13.2) [7.0–8.1] | 3.3 (0.3; 12.8) [2.8–3.5] | 0.637 | 0.79 | 0.083 | |
| Radius Angulation on Lateral View | Initial | 26.3 (18.4; 31.5) [23.6–27.6] | 18.5 (13; 24.8) [13.8–21.9] | 0.010 | 0.03 | 0.459 |
| Post-reduction | 4.3 (1.7; 8.0) [3.5–5.4] | 5.4 (2.9; 8.7) [2.5–6.7] | 0.569 | 0.79 | 0.100 | |
| Change | 21 (11.0; 27.2) [18.1–26.2] | 11.8 (8.7; 16.4) [9.9–13.5] | 0.017 | 0.04 | 0.426 | |
| Ulna Angulation on Ap View | Initial | 10.1 (5.5; 19.1) [9.1–13.1] | 8.7 (1.6; 26.4) [7.9–13.7] | 0.735 | 0.88 | 0.059 |
| Post-reduction | 3.1 (1.5; 5.4) [1.9–3.4] | 3.0 (1.7; 5.5) [1.3–4.7] | 0.960 | 0.96 | 0.009 | |
| Change | 6.5 (1.3; 15.7) [4.9–8.2] | 6.8 (−0.2; 21.8) [5.1–8.8] | 0.931 | 0.96 | 0.015 | |
| Ulna Angulation on Lateral View | Initial | 25.0 (13.3; 35.4) [19.2–26.7] | 18.7 (9.5; 26.0) [11.0–23.6] | 0.100 | 0.20 | 0.291 |
| Post-reduction | 3.6 (1.6; 6.8) [2.7–4.1] | 1.6 (0.7; 6.7) [1.2–2.0] | 0.142 | 0.24 | 0.259 | |
| Change | 20 (9.6; 31.6) [14.9–23.2] | 17.8 (8.2; 22.7) [15.0–21.2] | 0.244 | 0.39 | 0.204 | |
| Lenght of Radius (mm) | Unaffected side | 206.8 (197; 222) [203.5–216.7] | 187.1 (184; 203) [184.0–202.8] | <0.001 | <0.001 | 0.798 |
| Fractured side (Final X-Ray) | 210.3 (198; 223) [205.8–219.4] | 190.9 (186; 210) [187.8–209.8] | 0.001 | 0.003 | 0.672 | |
| Lenght of Ulna (mm) | Unaffected side | 214.6 (204; 234) [211.5–229.0] | 194.6 (190; 214) [192.2–213.8] | 0.001 | 0.003 | 0.725 |
| Fractured side (Final X-Ray) | 217.5 (206; 236) [211.6–230.0] | 205.0 (195; 221) [198.3–221.2] | 0.008 | 0.02 | 0.551 | |
| Location of Maximum Radial Bowing (mm) | Unaffected side | 62.0 (60; 65) [61.0–64.0] | 65.0 (62; 69) [63.0–68.0] | 0.010 | 0.03 | 0.504 |
| Fractured side (Final X-Ray) | 64.0 (59; 67) [62.0–65.0] | 63.0 (59; 65) [62.0–63.5] | 0.671 | 0.79 | 0.081 | |
| Maximum Radial Bow (%) | Unaffected side | 7.5 (6.8; 8.1) [7.1–7.8] | 6.9 (6.7; 7.8) [6.7–7.0] | 0.062 | 0.12 | 0.364 |
| Fractured side (Final X-Ray) | 7.1 (7.0; 7.7) [6.9–7.6] | 7.0 (6.9; 7.8) [6.7–7.7] | 0.597 | 0.79 | 0.101 | |
| Sex | |||||||
|---|---|---|---|---|---|---|---|
| Male | Female | ||||||
| N | N % | N | N % | p * Value | φ ** (Eff. Size) | ||
| Major Complications | Yes | 63 | 48.8 | 10 | 29.4 | 0.074 | 0.15 |
| No | 66 | 51.2 | 24 | 70.6 | |||
| Closed Reduction | Unacceptable | 34 | 26.4% | 4 | 11.8% | 0.118 ‡ | 0.12 |
| Acceptable | 95 | 73.6% | 30 | 88.2% | |||
| Re-displacement | Yes | 22 | 17.0% | 5 | 14.7% | 0.783 ‡ | 0.0170 |
| No | 107 | 83.0% | 29 | 85.3% | |||
| Operation | Yes | 20 | 19.2% | 0 | 0.0% | 0.007 ‡ | 0.2 |
| No | 84 | 80.8% | 30 | 100.0% | |||
| Outcome | Independent Predictor | β (Coefficient) | 95% CI | p Value |
|---|---|---|---|---|
| Radius Angulation on AP View | Male Sex (Ref = Female) | +6.2 | 2.1–10.3 | 0.003 |
| Age | 0.8 | −0.2–1.8 | 0.115 | |
| Height | 0.05 | −0.03–0.13 | 0.21 | |
| Weight | 0.3 | −0.5–1.1 | 0.445 | |
| Lenght of Radius | Male Sex (Ref = Female) | +17.4 | 10.8–23.9 | <0.001 |
| Age | +1.2 | 0.2–2.3 | 0.018 | |
| Height | +0.11 | 0.05–0.17 | <0.001 | |
| Weight | +0.6 | –0.3–1.5 | 0.180 | |
| Lenght of Ulna | Male Sex (Ref = Female) | +15.9 | 9.2–22.6 | <0.001 |
| Age | +1.0 | –0.1–2.0 | 0.071 | |
| Height | +0.09 | 0.02–0.16 | 0.009 | |
| Weight | +0.4 | –0.5–1.3 | 0.374 |
| Any Complication (Yes) | Independent Predictor | Adjusted OR | 95% CI | p Value |
|---|---|---|---|---|
| Surgical Intervention (Yes) | Male Sex (Ref = Female) | 3.1 | 1.2–8.4 | 0.022 |
| Age | 1.1 | 0.8–1.5 | 0.490 | |
| Height | 1.01 | 0.98–1.03 | 0.390 | |
| Weight | 0.9 | 0.6–1.4 | 0.670 | |
| Complication (Yes) | Male Sex (Ref = Female) | 1.5 | 0.7–3.3 | 0.284 |
| Age | 1.0 | 0.8–1.2 | 0.880 | |
| Height | 1.0 | 0.98–1.02 | 0.765 | |
| Weight | 1.1 | 0.9–1.4 | 0.320 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cetin, O.; Koluman, A.C.; Demirkoparan, M.; Yucesan, A.; Karahan, G.; Coskunol, E. Sex-Based Anatomical Variations and Complication Risks in Pediatric Both-Bone Forearm Fractures: A Level of Evidence IV Retrospective Analysis. Children 2025, 12, 1404. https://doi.org/10.3390/children12101404
Cetin O, Koluman AC, Demirkoparan M, Yucesan A, Karahan G, Coskunol E. Sex-Based Anatomical Variations and Complication Risks in Pediatric Both-Bone Forearm Fractures: A Level of Evidence IV Retrospective Analysis. Children. 2025; 12(10):1404. https://doi.org/10.3390/children12101404
Chicago/Turabian StyleCetin, Onur, Ali Can Koluman, Mesut Demirkoparan, Ali Yucesan, Gokhan Karahan, and Erhan Coskunol. 2025. "Sex-Based Anatomical Variations and Complication Risks in Pediatric Both-Bone Forearm Fractures: A Level of Evidence IV Retrospective Analysis" Children 12, no. 10: 1404. https://doi.org/10.3390/children12101404
APA StyleCetin, O., Koluman, A. C., Demirkoparan, M., Yucesan, A., Karahan, G., & Coskunol, E. (2025). Sex-Based Anatomical Variations and Complication Risks in Pediatric Both-Bone Forearm Fractures: A Level of Evidence IV Retrospective Analysis. Children, 12(10), 1404. https://doi.org/10.3390/children12101404








