Medical–Legal Liability and Indoor Air Pollution in Non-Industrial Environments and Perspectives for Maternal and Child Health
Abstract
1. Introduction
1.1. Sources and Types of Indoor Air Pollutants
1.2. Health Effects and Vulnerable Populations
1.3. Legal and Regulatory Frameworks
1.4. Case Studies of Medical–Legal Liability Related to Indoor Air Quality
2. Literature Review
2.1. Search Strategy
2.1.1. Datasets
2.1.2. Inclusion and Exclusion Criteria
2.1.3. Study Selection
2.1.4. Data Extraction
3. Results
4. Discussion
5. Limitation
6. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Settimo, G.; Manigrasso, M.; Avino, P. Avino, Indoor Air Quality: A Focus on the European Legislation and State-of-the-Art Research in Italy. Atmosphere 2020, 11, 370. [Google Scholar] [CrossRef]
- Van Tran, V.; Park, D.; Lee, Y.-C. Indoor Air Pollution, Related Human Diseases, and Recent Trends in the Control and Improvement of Indoor Air Quality. Int. J. Environ. Res. Public Health 2020, 17, 2927. [Google Scholar] [CrossRef]
- Vardoulakis, S.; Giagloglou, E.; Steinle, S.; Davis, A.; Sleeuwenhoek, A.; Galea, K.S.; Dixon, K.; Crawford, J.O. Indoor Exposure to Selected Air Pollutants in the Home Environment: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8972. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, J.A.; Alexis, N.; Bacchus, H.; Bernstein, I.L.; Fritz, P.; Horner, E.; Li, N.; Mason, S.; Nel, A.; Oullette, J.; et al. The health effects of nonindustrial indoor air pollution. J. Allergy Clin. Immunol. 2007, 121, 585. [Google Scholar] [CrossRef] [PubMed]
- Baeza_Romero, M.T.; Dudzinska, M.R.; Torkmahalleh, M.A.; Barros, N.; Coggins, A.M.; Ruzgar, D.G.; Kildsgaard, I.; Naseri, M.; Rong, L.; Saffell, J.; et al. A review of critical residential buildings parameters and activities when investigating indoor air quality and pollutants. Indoor Air 2022, 32, e13144. [Google Scholar] [CrossRef] [PubMed]
- Aswin Sidhaarth, K.R.; Shabarish, S.; Vinod Kumar, M.; Tamilarasan, K. Diagnosis of Ailment in Gaseous Matrix (Air) at Operation Suite—A Detailed Insight. Türk Bilgi. Mat. Eğitimi Derg. 2021, 12, 1752. [Google Scholar] [CrossRef]
- Kumar, P.; Skouloudis, A.N.; Bell, M.; Viana, M.; Carotta, M.C.; Biskos, G.; Morawska, L. Real-time sensors for indoor air monitoring and challenges ahead in deploying them to urban buildings. Sci. Total Environ. 2016, 560–561, 150–159. [Google Scholar] [CrossRef]
- Kumar, P.; Singh, A.; Arora, T.; Singh, S.; Singh, R. Critical review on emerging health effects associated with the indoor air quality and its sustainable management. Sci. Total Environ. 2023, 872, 162163. [Google Scholar] [CrossRef]
- Senitkova, I.J.; Kraus, M. Indoor Air Pollution in Housing Units. IOP Conf. Ser. Mater. Sci. Eng. 2021, 1203, 22071. [Google Scholar] [CrossRef]
- Maung, T.Z.; Bishop, J.E.; Holt, E.; Turner, A.M.; Pfrang, C. Indoor Air Pollution and the Health of Vulnerable Groups: A Systematic Review Focused on Particulate Matter (PM), Volatile Organic Compounds (VOCs) and Their Effects on Children and People with Pre-Existing Lung Disease. Int. J. Environ. Res. Public Health 2022, 19, 8752. [Google Scholar] [CrossRef]
- Lachowicz, J.I.; Milia, S.; Jaremko, M.; Oddone, E.; Cannizzaro, E.; Cirrincione, L.; Malta, G.; Campagna, M.; Lecca, L.I. Cooking Particulate Matter: A Systematic Review on Nanoparticle Exposure in the Indoor Cooking Environment. Atmosphere 2022, 14, 12. [Google Scholar] [CrossRef]
- Kuncoro, C.B.D.; Asyikin, M.B.Z.; Amaris, A. Smart-Autonomous Wireless Volatile Organic Compounds Sensor Node for Indoor Air Quality Monitoring Application. Int. J. Environ. Res. Public Health 2022, 19, 2439. [Google Scholar] [CrossRef] [PubMed]
- Chawla, H.; Anand, P.; Garg, K.; Bhagat, N.; Varmani, S.G.; Bansal, T.; McBain, A.J.; Marwah, R.G. A comprehensive review of microbial contamination in the indoor environment: Sources, sampling, health risks, and mitigation strategies. Front. Public Health 2023, 11, 1285393. [Google Scholar] [CrossRef]
- Oar, Oria, and Ied. Indoor Air Pollution: An Introduction for Health Professionals. 2014. Available online: https://swap.stanford.edu/20151013060837/http:/www2.epa.gov/indoor-air-quality-iaq/indoor-air-pollution-introduction-health-professionals (accessed on 1 September 2025).
- Kumar, P.; Kausar, M.A.; Singh, A.B.; Singh, R. Biological contaminants in the indoor air environment and their impacts on human health. Air Qual. Atmos. Health 2021, 14, 1723. [Google Scholar] [CrossRef]
- Ko Fanny, W.S.M.D.; Hui David, S.C.M.D. Effects of Air Pollution on Lung Health. Clin. Pulm. Med. 2010, 17, 300. [Google Scholar] [CrossRef]
- Kurt, O.K.; Zhang, J.; Pinkerton, K.E. Pinkerton. Pulmonary health effects of air pollution. Curr. Opin. Pulm. Med. 2016, 22, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Amini, R.; Ghaffarianhoseini, A.; Ghaffarianhoseini, A.; Berardi, U. Numerical investigation of indoor thermal comfort and air quality for a multi-purpose hall with various shading and glazing ratios. Therm. Sci. Eng. Prog. 2020, 22, 100812. [Google Scholar] [CrossRef]
- Kubba, S. Indoor Environmental Quality (IEQ). In Elsevier eBooks; Elsevier BV: Amsterdam, The Netherlands, 2015; p. 303. [Google Scholar] [CrossRef]
- Banerjee, A.; Melkania, N.; Nain, A. Indoor Air Quality (IAQ) in Green Buildings, a Pre-Requisite to Human Health and Well-Being. In Digital Cities Roadmap: IoT-Based Architecture and Sustainable Buildings; Wiley: Hoboken, NJ, USA, 2021; p. 293. [Google Scholar] [CrossRef]
- Levasseur, M.-E.; Poulin, P.; Campagna, C.; Leclerc, J.-M. Integrated Management of Residential Indoor Air Quality: A Call for Stakeholders in a Changing Climate. Int. J. Environ. Res. Public Health 2017, 14, 1455. [Google Scholar] [CrossRef]
- Xu, X.-M.; Ou, S.-J. The Discussion on the relationship among indoor air quality, environmental cognition and user’s behaviour. IOP Conf. Ser. Earth Environ. Sci. 2019, 291, 12005. [Google Scholar] [CrossRef]
- Ha, Q.P.; Metia, S.; Phung, M.D. Phung. Sensing Data Fusion for Enhanced Indoor Air Quality Monitoring. IEEE Sens. J. 2020, 20, 4430. [Google Scholar] [CrossRef]
- Kuramochi, H.; Tsurumi, R.; Ishibashi, Y. Meta-Analysis of the Effect of Ventilation on Intellectual Productivity. Int. J. Environ. Res. Public Health 2023, 20, 5576. [Google Scholar] [CrossRef]
- Kajander, J.-K.; Sivunen, M.; Junnila, S. Valuing Indoor Air Quality Benefits in a Healthcare Construction Project with Real Option Analysis. Buildings 2014, 4, 785. [Google Scholar] [CrossRef]
- Wargocki, P. Measurements of the Effects of Air Quality on Sensory Perception. Chem. Senses. 2001, 26, 345. [Google Scholar] [CrossRef][Green Version]
- Lovrić, M.; Gajski, G.; Fernández-Agüera, J.; Pöhlker, M.; Gursch, H.; Consortium, E.D.A.I.; Borg, A.; Switters, J.; Mureddu, F. Evidence driven indoor air quality improvement: An innovative and interdisciplinary approach to improving indoor air quality. BioFactors 2025, 51, e2126. [Google Scholar] [CrossRef]
- Wiehn, J.; Tietjen, S.; Beese, F.; Birmili, W.; Bunge, C.; Daniels, A.; Lahore, A.F.; Hahn, D.; Kolossa-Gehring, M.; Kuhnert, R.; et al. Indoor air pollution inequalities among children and adolescents in Germany: An analysis of repeated cross-sectional data from GerES and KiGGS. Sci. Rep. 2025, 15, 14521. [Google Scholar] [CrossRef]
- Allen, J.G.; MacNaughton, P.; Satish, U.; Santanam, S.; Vallarino, J.; Spengler, J.D. Associations of Cognitive Function Scores with Carbon Dioxide, Ventilation, and Volatile Organic Compound Exposures in Office Workers: A Controlled Exposure Study of Green and Conventional Office Environments. Environ. Health Perspect. 2015, 124, 805. [Google Scholar] [CrossRef]
- Karimi, H.; Adibhesami, M.A.; Bazazzadeh, H.; Movafagh, S. Green Buildings: Human-Centered and Energy Efficiency Optimization Strategies. Energies 2023, 16, 3681. [Google Scholar] [CrossRef]
- Rajput, T.S.; Thomas, A.; Ooka, R. Analyzing the effects of passive design strategies on building ventilation performance and thermal comfort using simulation-based approach. E3S Web Conf. 2023, 396, 02023. [Google Scholar] [CrossRef]
- Sun, Z.; Wang, S. A CFD-based test method for control of environment and space ventilation. Build. Environ. 2009, 45, 1441. [Google Scholar] [CrossRef]
- Dai, H.; Imani, S.; Choi, J.-H. Correlating Indoor Environmental Quality Parameters with Human Physiological Responses for Adaptive Comfort Control in Commercial Buildings. Energies 2025, 18, 2280. [Google Scholar] [CrossRef]
- Persily, A.K.; Emmerich, S.J. Emmerich. Indoor air quality in sustainable, energy efficient buildings. HVACR Res. 2012, 18, 4. [Google Scholar] [CrossRef]
- Khalvati, F.; Omidvar, A. The Performance Evaluation of Ventilated Windows in the Simultaneous Improvement of Energy Efficiency and Indoor Air Quality in Office Buildings: A Case Study. New Energy Exploit. Appl. 2021, 1, 8–16. [Google Scholar] [CrossRef]
- Khalil, E.E. Thermal Management in Hospitals: Comfort, Air Quality, and Energy Utilization. In Proceedings of the 6th International Energy Conversion Engineering Conference (IECEC), Cleveland, OH, USA, 28–30 June 2008. [Google Scholar] [CrossRef]
- Su, W.; Ai, Z.; Liu, J.; Yang, B.; Wang, F. Maintaining an acceptable indoor air quality of spaces by intentional natural ventilation or intermittent mechanical ventilation with minimum energy use. Appl. Energy 2023, 348, 121504. [Google Scholar] [CrossRef]
- Sarhan, A.; El Gelil, R.A.; Awad, H. The assessment of natural ventilation performance for thermal comfort in educational space: A case study of design studio in the AAST-Alexandria. Proc. IOP Conf. Ser. Mater. Sci. Eng. 2019, 609, 32059. [Google Scholar] [CrossRef]
- Reda, I.; AbdelMessih, R.N.; Steit, M.; Mina, E.M. Quantifying Fenestration Effect on Thermal Comfort in Naturally Ventilated Classrooms. Sustainability 2021, 13, 7385. [Google Scholar] [CrossRef]
- Marques, G.; Pitarma, R. Indoor Air Quality Monitoring for Enhanced Healthy Buildings. In Indoor Environmental Quality; IntechOpen eBooks; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef]
- Asim, N.; Badiei, M.; Mohammad, M.; Razali, H.; Rajabi, A.; Haw, L.C.; Ghazali, M.J. Sustainability of Heating, Ventilation and Air-Conditioning (HVAC) Systems in Buildings—An Overview. Int. J. Environ. Res. Public Health 2022, 19, 1016. [Google Scholar] [CrossRef]
- Zender-Świercz, E. Review of IAQ in Premises Equipped with Façade–Ventilation Systems. Atmosphere 2021, 12, 220. [Google Scholar] [CrossRef]
- Stanley, H.O.; Onwuna, B.; Ugboma, C.J. Microbial Assessment of Indoor Air Quality of Ventilation Systems. Asian J. Adv. Res. Rep. 2019, 3, 1–7. [Google Scholar] [CrossRef]
- Hussin, N.B.; Ibrahim, D.B.; Ahmad, F.N.B.; Yahya, N.H.B.M.; Hashim, S.M.B. IMPROVING INDOOR AIR QUALITY USING LOCAL EXHAUST VENTILATION (LEV). J. Teknol. 2015, 76, 7–11. [Google Scholar] [CrossRef][Green Version]
- Nag, P.K. Ventilation in Office Buildings. In Design Science and Innovation; Springer Nature: New York, NY, USA, 2018; p. 341. [Google Scholar] [CrossRef]
- Gwak, J.; Shino, M.; Ueda, K.; Kamata, M. An Investigation of the Effects of Changes in the Indoor Ambient Temperature on Arousal Level, Thermal Comfort, and Physiological Indices. Appl. Sci. 2019, 9, 899. [Google Scholar] [CrossRef]
- Alfano, F.R.D.; Olesen, B.W.; Palella, B.I.; Riccio, G. Thermal comfort: Design and assessment for energy saving. Energy Build. 2014, 81, 326. [Google Scholar] [CrossRef]
- Ikechukwu, O.; Lin, L.; Moses, I.O.; Moses, O. Towards Enhancing the Effectiveness of Classroom Designs for Natural Ventilation Comfort in Yola, Nigeria. Open J. Energy Effic. 2019, 8, 129. [Google Scholar] [CrossRef]
- Puad, M.H.M.; Zuhairi, A.J.A. Regulating Indoor Environmental Quality (IEQ) Factors in Influencing Learning Satisfaction among Technical and Vocational Education and Training (TVET) Students. Int. J. Acad. Res. Progress. Educ. Dev. 2019, 8, 688–704. [Google Scholar] [CrossRef]
- Bluyssen, P.M. The role of flooring materials in health, comfort and performance of children in classrooms. Cogent Psychol. 2016, 3, 1268774. [Google Scholar] [CrossRef]
- Khean, C.C.; Yih, T.Y. A Review of the Effectiveness Study of Botanical Components That Improves Air Filtration. Proc. IOP Conf. Ser. Earth Environ. Sci. 2018, 167, 12033. [Google Scholar] [CrossRef]
- Mujan, I.; Anđelković, A.S.; Munćan, V.; Kljajić, M.; Ružić, D. Influence of indoor environmental quality on human health and productivity—A review. J. Clean. Prod. 2019, 217, 646. [Google Scholar] [CrossRef]
- Jones, A.P. Indoor air quality and health. Atmos. Environ. 1999, 33, 4535. [Google Scholar] [CrossRef]
- Assali, I. Enhance Indoor Environment in Buildings and Its Effect on Improving Occupant’s Health. J. Tek. Lingkung. Electron. J. Civ. Environ. Eng. 2016, 10, 104. Available online: https://publications.waset.org/10003570/enhance-indoor-environment-in-buildings-and-its-effect-on-improving-occupants-health (accessed on 1 September 2025).
- Miao, D.; Cao, X.; Zuo, W. Associations of Indoor Environmental Quality Parameters with Students’ Perceptions in Undergraduate Dormitories: A Field Study in Beijing during a Transition Season. Int. J. Environ. Res. Public Health 2022, 19, 16997. [Google Scholar] [CrossRef]
- Huang, L.; Zhu, Y.; Ouyang, Q.; Cao, B. A study on the effects of thermal, luminous, and acoustic environments on indoor environmental comfort in offices. Build. Environ. 2011, 49, 304. [Google Scholar] [CrossRef]
- Arata, S.; Sugiuchi, M.; Ikaga, T.; Shiraishi, Y.; Hayashi, T.; Ando, S.; Kawakubo, S. Economic benefits of the effects of office environment on perceived work efficiency and presenteeism. Build. Environ. 2023, 243, 110712. [Google Scholar] [CrossRef]
- Dimitroulopoulou, S.; Dudzińska, M.R.; Gunnarsen, L.; Hägerhed, L.; Maula, H.; Singh, R.; Toyinbo, O.; Haverinen-Shaughnessy, U. Indoor air quality guidelines from across the world: An appraisal considering energy saving, health, productivity, and comfort. Environ. Int. 2023, 178, 108127. [Google Scholar] [CrossRef]
- Erlandson, G.; Magzamen, S.; Carter, E.; Sharp, J.L.; Reynolds, S.J.; Schaeffer, J.W. Characterization of Indoor Air Quality on a College Campus: A Pilot Study. Int. J. Environ. Res. Public Health 2019, 16, 2721. [Google Scholar] [CrossRef]
- Emmerich, S.J.; Teichman, K.Y.; Persily, A.K. Literature review on field study of ventilation and indoor air quality performance verification in high-performance commercial buildings in North America. Sci. Technol. Built Environ. 2017, 23, 1159. [Google Scholar] [CrossRef]
- Omidvarborna, H.; Kumar, P.; Hayward, J.; Gupta, M.; Nascimento, E.G.S. Low-Cost Air Quality Sensing towards Smart Homes. Atmosphere 2021, 12, 453. [Google Scholar] [CrossRef]
- Mannan, M.; Al-Ghamdi, S.G. Indoor Air Quality in Buildings: A Comprehensive Review on the Factors Influencing Air Pollution in Residential and Commercial Structure. Int. J. Environ. Res. Public Health 2021, 18, 3276. [Google Scholar] [CrossRef]
- Kapoor, N.R.; Kumar, A.; Alam, T.; Kumar, A.; Kulkarni, K.S.; Blecich, P. A Review on Indoor Environment Quality of Indian School Classrooms. Sustainability 2021, 13, 11855. [Google Scholar] [CrossRef]
- Orecchio, S. Polycyclic aromatic hydrocarbons (PAHs) in indoor emission from decorative candles. Atmos. Environ. 2010, 45, 1888. [Google Scholar] [CrossRef]
- He, L.; Guan, W.; Zeng, Y.; Zhao, D.Z.; Qiu, X.; Guo, J. Molybdenum Sulfide (MoS2)/Ordered Mesoporous Carbon (OMC) Tubular Mesochannel Photocatalyst for Enhanced Photocatalytic Oxidation for Removal of Volatile Organic Compounds (VOCs). Front. Chem. 2022, 9, 748622. [Google Scholar] [CrossRef] [PubMed]
- Laurent, J.G.C.; Allen, J.G.; McNeely, E.; Dominici, F.; Spengler, J.D. Influence of the residential environment on undergraduate students’ health. J. Expo. Sci. Environ. Epidemiol. 2019, 30, 320. [Google Scholar] [CrossRef]
- Mitchell, C.S.; Zhang, J.; Sigsgaard, T.; Jantunen, M.; Lioy, P.J.; Samson, R.; Karol, M.H. Current State of the Science: Health Effects and Indoor Environmental Quality. Environmental Health Perspectives. Natl. Inst. Environ. Health Sci. 2007, 115, 958. [Google Scholar] [CrossRef]
- Wierzbicka, A.; Pedersen, E.; Stroh, E.; Li, Y.; Dahlblom, M.; Lundgren-Kownacki, K.; Isaxon, C.; Gudmundsson, A.; Wargocki, P.; Persson, R.; et al. Healthy Indoor Environments: The Need for a Holistic Approach. Int. J. Environ. Res. Public Health 2018, 15, 1874. [Google Scholar] [CrossRef]
- Campos-Gil, J.A.; Ortega-Andeane, P.; Chanes, D.V. Children’s Microsystems and Their Relationship to Stress and Executive Functioning. Front. Psychol. 2020, 11, 996. [Google Scholar] [CrossRef]
- Saridi, M.; Toska, A.; Latsou, D.; Karakousi, S.; Albani, E.; Souliotis, K.; Sarafis, P. The effect of physical activity and indoor environment on preschool children’s health. Magna Sci. Adv. Res. Rev. 2021, 1, 45. [Google Scholar] [CrossRef]
- Kebede, M. Healthy buildings, healthy people. Bull. World Health Organ. 2018, 96, 151. [Google Scholar] [CrossRef]
- Fuentes-Leonarte, V.; Ballester, F.; Tenías, J.M. Sources of Indoor Air Pollution and Respiratory Health in Preschool Children. J. Environ. Public Health 2009, 2009, 727516. [Google Scholar] [CrossRef]
- Aubin, D.; Ouazia, B.; Poulin, P.; Levesque, B.; Tremblay, F.; Boulet, L.-P.; Duchaine, C.; Degois, J.; Maltais, F.; Brisson, M.; et al. Intervention field study in the Canadian arctic: Improving ventilation, indoor air quality, and the respiratory health in Nunavik dwellings and children. Proc. IOP Conf. Ser. Mater. Sci. Eng. 2019, 609, 42055. [Google Scholar] [CrossRef]
- Saad, S.M.; Shakaff, A.Y.M.; Saad, A.R.M.; Kamarudin, A.M.Y. Development of wireless sensor network for monitoring indoor air pollutant. AIP Conf. Proc. 2015, 1660, 70077. [Google Scholar] [CrossRef]
- Fernández, L.C.; Alvarez, R.F.; González-Barcala, F.J.; Portal, J.A.R. Contaminación del aire interior y su impacto en la patología respiratoria. Arch. Bronconeumol. 2012, 49, 22. [Google Scholar] [CrossRef] [PubMed]
- Hodas, N.; Loh, M.; Shin, H.; Li, D.; Bennett, D.; McKone, T.E.; Jolliet, O.; Weschler, C.J.; Jantunen, M.; Lioy, P.; et al. Indoor inhalation intake fractions of fine particulate matter: Review of influencing factors. Indoor Air. 2015, 26, 836. [Google Scholar] [CrossRef] [PubMed]
- Murniati, N. Sick Building Syndrome in Indonesia and Singapore: A Comparative Study. In Proceedings of the 3rd International Conference on Vocational Higher Education (ICVHE 2018), Batam, Indonesia, 2–4 August 2018. [Google Scholar] [CrossRef]
- Ciuzas, D.; Prasauskas, T.; Krugly, E.; Sidaraviciute, R.; Jurelionis, A.; Seduikyte, L.; Kauneliene, V.; Wierzbicka, A.; Martuzevicius, D. Characterization of indoor aerosol temporal variations for the real-time management of indoor air quality. Atmos. Environ. 2015, 118, 107. [Google Scholar] [CrossRef]
- Islam, N.; Saikia, B.K. Atmospheric particulate matter and potentially hazardous compounds around residential/road side soil in an urban area. Chemosphere 2020, 259, 127453. [Google Scholar] [CrossRef]
- Patel, S.; Sankhyan, S.; Boedicker, E.K.; DeCarlo, P.F.; Farmer, D.K.; Goldstein, A.H.; Katz, E.F.; Nazaroff, W.W.; Tian, Y.; Vanhanen, J.; et al. Indoor Particulate Matter during HOMEChem: Concentrations, Size Distributions, and Exposures. Environ. Sci. Technol. 2020, 54, 7107. [Google Scholar] [CrossRef] [PubMed]
- Goyal, R.; Khare, M. Indoor Air Quality: Current Status, Missing Links and Future Road Map for India. J. Civ. Environ. Eng. 2012, 2, 000118. [Google Scholar] [CrossRef]
- Kapoor, C.S. Efficient Control of Air Pollution through Plants a Cost Effective Alternatives. J. Climatol. Weather. Forecast. 2016, 4, 1000184. [Google Scholar] [CrossRef]
- Singh, A.; Thajudeen, T. A Hybrid Particle Swarm Optimization-Tuning Algorithm for the Prediction of Nanoparticle Morphology from Microscopic Images. Aerosol Air Qual. Res. 2023, 23, 220453. [Google Scholar] [CrossRef]
- Thurston, G.D.; Kipen, H.; Annesi-Maesano, I.; Balmes, J.; Brook, R.D.; Cromar, K.; De Matteis, S.; Forastiere, F.; Forsberg, B.; Frampton, M.W.; et al. A joint ERS/ATS policy statement: What constitutes an adverse health effect of air pollution? An analytical framework. Eur. Respir. J. 2016, 49, 1600419. [Google Scholar] [CrossRef]
- Luo, K.; Zeng, D.; Kang, Y.; Lin, X.; Sun, N.; Li, C.; Zhu, M.; Chen, Z.; Man, Y.B.; Li, H. Dermal bioaccessibility and absorption of polycyclic aromatic hydrocarbons (PAHs) in indoor dust and its implication in risk assessment. Environ. Pollut. 2020, 264, 114829. [Google Scholar] [CrossRef]
- Mannino, M.R.; Orecchio, S. Polycyclic aromatic hydrocarbons (PAHs) in indoor dust matter of Palermo (Italy) area: Extraction, GC–MS analysis, distribution and sources. Atmos. Environ. 2007, 42, 1801. [Google Scholar] [CrossRef]
- Han, B.; Bai, Z.; Liu, Y.; You, Y.; Xu, J.; Zhou, J.; Zhang, J.; Niu, C.; Zhang, N.; He, F.; et al. Characterizations, relationship, and potential sources of outdoor and indoor particulate matter bound polycyclic aromatic hydrocarbons (PAHs) in a community of Tianjin, Northern China. Indoor Air 2014, 25, 320. [Google Scholar] [CrossRef]
- Liaud, C.; Chouvenc, S.; Le Calvé, S. Calvé. Simultaneous Monitoring of Particle-Bound PAHs Inside a Low-Energy School Building and Outdoors over Two Weeks in France. Atmosphere 2021, 12, 108. [Google Scholar] [CrossRef]
- Låg, M.; Øvrevik, J.; Refsnes, M.; Holme, J.A. Holme. Potential role of polycyclic aromatic hydrocarbons in air pollution-induced non-malignant respiratory diseases. Respir. Res. BioMed. Cent. 2020, 21, 299. [Google Scholar] [CrossRef]
- Shi, S. Contributions of indoor and outdoor sources to airborne polycyclic aromatic hydrocarbons indoors. Build. Environ. 2018, 131, 154. [Google Scholar] [CrossRef]
- Cilluffo, G.; Ferrante, G.; Murgia, N.; Mancini, R.; Pichini, S.; Cuffari, G.; Giudice, V.; Tirone, N.; Malizia, V.; Montalbano, L.; et al. Effects of Polycyclic Aromatic Hydrocarbons on Lung Function in Children with Asthma: A Mediation Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1826. [Google Scholar] [CrossRef]
- Siudek, P. Compositional and seasonal differences of gas and particle phase polycyclic aromatic hydrocarbons (PAHs) over the southern Baltic Sea coast. Sci. Rep. 2022, 12, 21005. [Google Scholar] [CrossRef] [PubMed]
- Badyda, A.; Wierzba, W.; Gayer, A. Indoor air quality in schools: Seasonal variation and health implications for children. Eur. J. Public Health 2024, 34 (Suppl. S33), ckae144.797. [Google Scholar] [CrossRef]
- Jakovljević, I.; Dvoršćak, M.; Jagić, K.; Klinčić, D. Polycyclic Aromatic Hydrocarbons in Indoor Dust in Croatia: Levels, Sources, and Human Health Risks. Int. J. Environ. Res. Public Health 2022, 19, 11848. [Google Scholar] [CrossRef] [PubMed]
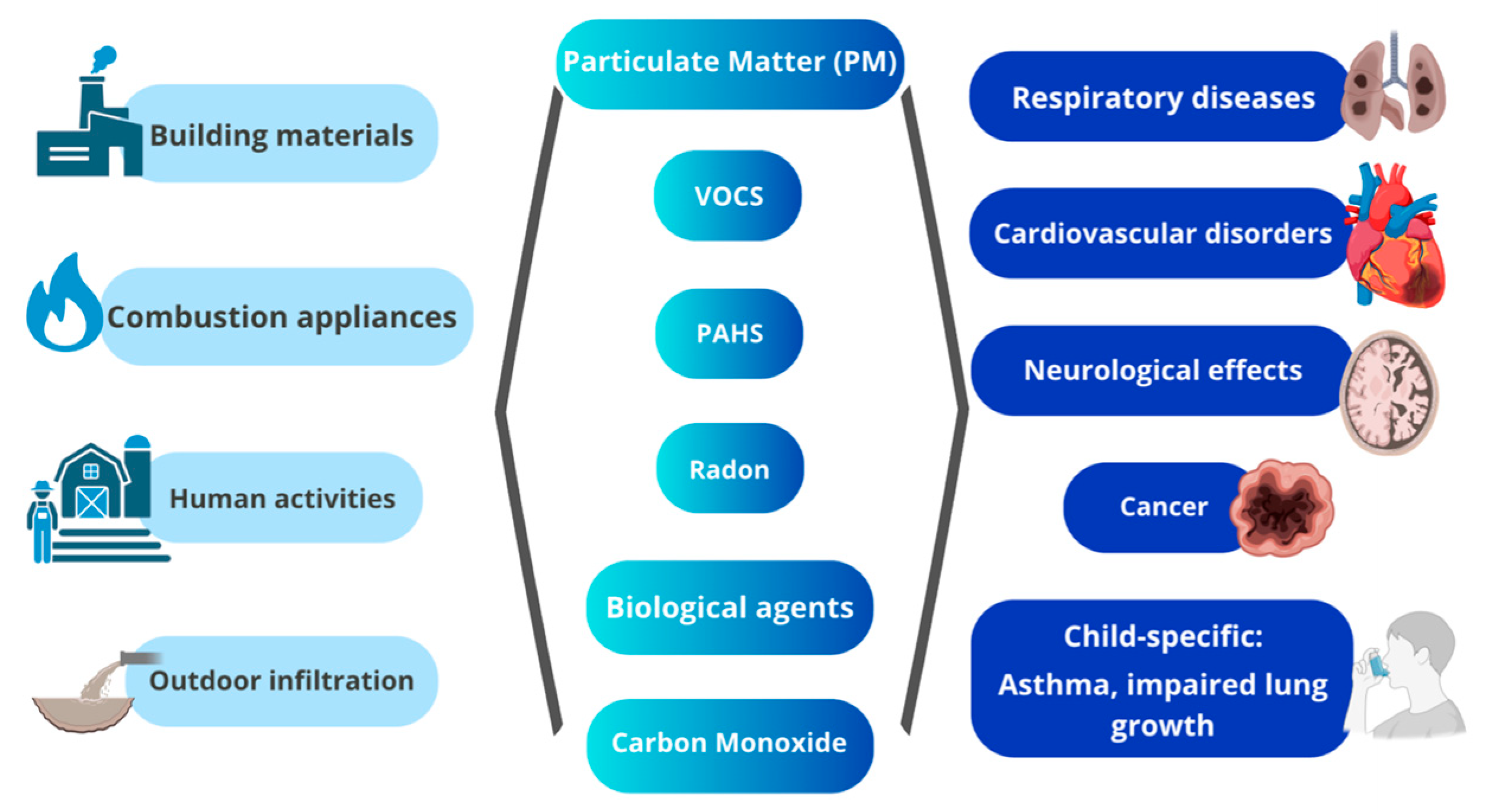
| Pollutant | Main Sources | Health Effects (Especially in Children) |
|---|---|---|
| Particulate Matter (PM2.5, PM10) | Cooking, heating, smoking, candles, outdoor infiltration | Asthma, bronchitis, impaired lung development, cardiovascular risk |
| Volatile Organic Compounds (VOCs: benzene, toluene, formaldehyde) | Paints, adhesives, cleaning agents, furniture | Irritation of eyes and respiratory tract, neurotoxicity, cancer |
| Polycyclic Aromatic Hydrocarbons (PAHs) | Combustion of fossil fuels, tobacco smoke, fireplaces, incense | Asthma, airway inflammation, lung cancer, cardiovascular diseases |
| Radon | Soil infiltration, building materials | Lung cancer |
| Biological contaminants (mold, bacteria, viruses, allergens) | Damp environments, poor ventilation, pets, pests | Allergies, asthma exacerbations, respiratory infections |
| Carbon Monoxide (CO) | Stoves, heaters, fireplaces, tobacco smoke | Headaches, neurological effects, death at high levels |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malta, G.; Montana, A.; Argo, A.; Zerbo, S.; Plescia, F.; Cannizzaro, E. Medical–Legal Liability and Indoor Air Pollution in Non-Industrial Environments and Perspectives for Maternal and Child Health. Children 2025, 12, 1287. https://doi.org/10.3390/children12101287
Malta G, Montana A, Argo A, Zerbo S, Plescia F, Cannizzaro E. Medical–Legal Liability and Indoor Air Pollution in Non-Industrial Environments and Perspectives for Maternal and Child Health. Children. 2025; 12(10):1287. https://doi.org/10.3390/children12101287
Chicago/Turabian StyleMalta, Ginevra, Angelo Montana, Antonina Argo, Stefania Zerbo, Fulvio Plescia, and Emanuele Cannizzaro. 2025. "Medical–Legal Liability and Indoor Air Pollution in Non-Industrial Environments and Perspectives for Maternal and Child Health" Children 12, no. 10: 1287. https://doi.org/10.3390/children12101287
APA StyleMalta, G., Montana, A., Argo, A., Zerbo, S., Plescia, F., & Cannizzaro, E. (2025). Medical–Legal Liability and Indoor Air Pollution in Non-Industrial Environments and Perspectives for Maternal and Child Health. Children, 12(10), 1287. https://doi.org/10.3390/children12101287










