Assessing Psychological Disorders in Turkish Adolescents with Transfusion-Dependent Thalassemia
(This article belongs to the Section Pediatric Mental Health)
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.3. Statistical Analysis
3. Results
Assessing the Utmost Vulnerable Subpopulation among TDT Patients
4. Discussion
5. Conclusions
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TDT | Transfusion-dependent thalassemia |
| RCADS | Revised Child Anxiety and Depression Scale |
| IQR | Interquartile range |
| LR | Linear regression test |
| GLM | Generalized linear model |
References
- Origa, R. β-Thalassemia. Genet. Med. 2017, 19, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Sevimli, C.; Yilmaz, Y.; Bayramoglu, Z.; Comert, R.G.; Gul, N.; Dursun, M.; Karakas, Z. Pancreatic MR imaging and endocrine complications in patients with beta-thalassemia: A single-center experience. Clin. Exp. Med. 2022, 22, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Afifi, T.; Elessi, K.; Samaan, M.; Elhatal, H.A.; Lamzi, A.A.; Elian, R.; Elblbessy, M.; Ataya, A.A.; Humeid, M.; Amro, H.A.; et al. Anxiety and Depression among Children with Cancer, Children Undergoing Hemodialysis and Children with Thalassemia: A Comparative Study. Int. J. Clin. Med. Edu. Res. 2022, 1, 89–93. [Google Scholar]
- Shonkoff, J.P.; Garner, A.S. Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, & Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012, 129, e232–e246. [Google Scholar] [CrossRef] [PubMed]
- El-said, S.G.; Darwish, A.; Wahba, N.M. Stress, anxiety and depression among adolescents suffering from thalassemia. Port Said Sci. J. Nurs. 2021, 8, 149–168. [Google Scholar]
- Eren, R.; Karışmaz, A.; Aslan, C.; Doğu, M.H.; Altındal, Ş.; Yokuş, O.; Suyanı, E. Beta thalassemia minor: Patients are not tired but depressed and anxious. Med. Princ. Pract. 2021, 30, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Graves, J.K.; Hodge, C.; Jacob, E. Depression, Anxiety, and Quality of Life in Children and Adolescents with Sickle Cell Disease. Pediatr. Nurs. 2016, 42, 113–119, 144. [Google Scholar]
- Koutelekos, J.; Haliasos, N. Depression and Thalassemia in children, adolescents and adults. Health Sci. J. 2013, 7, 239–247. [Google Scholar]
- Chorpita, B.F.; Yim, L.; Moffitt, C.; Umemoto, L.A.; Francis, S.E. Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behav. Res. Ther. 2000, 38, 835–855. [Google Scholar] [CrossRef]
- Piqueras, J.A.; Martín-Vivar, M.; Sandin, B.; San Luis, C.; Pineda, D. The Revised Child Anxiety and Depression Scale: A systematic review and reliability generalization meta-analysis. J. Affect. Disord. 2017, 218, 153–169. [Google Scholar] [CrossRef]
- Gormez, V.; Kilincaslan, A.; Ebesutani, C.; Orengul, A.C.; Kaya, I.; Ceri, V.; Nasiroglu, S.; Filiz, M.; Chorpita, B.F. Psychometric Properties of the Parent Version of the Revised Child Anxiety and Depression Scale in a Clinical Sample of Turkish Children and Adolescents. Child. Psychiatry Hum. Dev. 2017, 48, 922–933. [Google Scholar] [CrossRef]
- Bitsko, M.J.; Cohen, D.; Dillon, R.; Harvey, J.; Krull, K.; Klosky, J.L. Psychosocial Late Effects in Pediatric Cancer Survivors: A Report from the Children’s Oncology Group. Pediatr. Blood Cancer. 2016, 63, 337–343. [Google Scholar] [CrossRef]
- Kolaitis, G. Mood disorders in childhood and adolescence: Continuities and discontinuities to adulthood. Psychiatriki 2012, 23, 94–100. [Google Scholar] [PubMed]
- Canatan, D.; Ratip, S.; Kaptan, S.; Cosan, R. Psychosocial burden of beta-thalassaemia major in Antalya, south Turkey. Soc. Sci. Med. 2003, 56, 815–819. [Google Scholar] [CrossRef]
- Zolaly, M.A.; Zolaly, F.M.; Al Belowi, L.; Shuqdar, R.; Al Belowi MASr Alwasaidi, T.A.; Albadrani, M. Depression, Anxiety, and Stress Symptoms in Patients with Beta Thalassemia Major in Almadinah Almunawwarah, Saudi Arabia. Cureus 2020, 12, e11367. [Google Scholar] [CrossRef]
- Maheri, A.; Sadeghi, R.; Shojaeizadeh, D.; Tol, A.; Yaseri, M.; Rohban, A. Depression, Anxiety, and Perceived Social Support among Adults with Beta-Thalassemia Major: Cross-Sectional Study. Korean J. Fam. Med. 2018, 39, 101–107. [Google Scholar] [CrossRef]
- Jaafari, Z.; Sadidi, N.; Abdolahinia, Z.; Shahesmaeili, A. Prevalence of Depression among Iranian Patients with Beta-Thalassemia Major: A Systematic Review and Meta-analysis. Iran. J. Med. Sci. 2022, 47, 15–24. [Google Scholar] [CrossRef]
- Adib-Hajbaghery, M.; Ahmadi, M.; Poormansouri, S. Health Related Quality of Life, Depression, Anxiety and Stress in Patients with Beta-Thalassemia Major. Iran. J. Ped Hematol. Oncol. 2015, 5, 193–205. [Google Scholar]
- Töret, E.; Karadaş, N.Ö.; Gökçe, N.Ö.; Kaygusuz, A.; Karapınar, T.H.; Oymak, Y.; Gözmen, S. Quality of Life and Depression in Turkish Patients with β-Thalassemia Major: A Cross-Sectional Study. Hemoglobin 2018, 42, 326–329. [Google Scholar] [CrossRef]
- Messina, G.; Colombo, E.; Cassinerio, E.; Ferri, F.; Curti, R.; Altamura, C.; Cappellini, M.D. Psychosocial aspects and psychiatric disorders in young adult with thalassemia major. Intern. Emerg. Med. 2008, 3, 339–343. [Google Scholar] [CrossRef]
- Ghanizadeh, A.; Khajavian, S.; Ashkani, H. Prevalence of psychiatric disorders, depression, and suicidal behavior in child and adolescent with thalassemia major. J. Pediatr. Hematol. Oncol. 2006, 28, 781–784. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, O.; Zehra, B.; Torun, Y.A.; Karakukcu, M. Anxiety, Depression, Self-Esteem, and Attitude toward Illness among Children with Leukemia and Lymphoma in Remission. HemaSphere 2019, 3, 771–772. [Google Scholar] [CrossRef]
- Al-Makinah, S.; Al-Aithan, Z.; Al-Quryan, A. Prevalence of anxiety and its effect on academic performance among secondary school students in Al-Ahsa city, Eastern Saudi Arabia, 2020: Cross-sectional study. Adv. Clin. Exp. Med. 2023, 10, 239–251. [Google Scholar]
- Islam, M.I.; Khanam, R.; Kabir, E. Depression and anxiety have a larger impact on bullied girls than on boys to experience self-harm and suicidality: A mediation analysis. J. Affect. Disord. 2022, 297, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, R.; Chakraborty, K.; Sen, A.; Neogi, R.; Bhattacharyya, S. A comparative study of temperamental, behavioral, and cognitive changes in thalassemia major, thalassemia minor, and normal population. Indian. J. Psychiatry 2019, 61, 618–622. [Google Scholar] [CrossRef]
- Al-Hakeim, H.K.; Najm, A.H.; Al-Dujaili, A.H.; Maes, M. Major Depression in Children with Transfusion-Dependent Thalassemia Is Strongly Associated with the Combined Effects of Blood Transfusion Rate, Iron Overload, and Increased Pro-inflammatory Cytokines. Neurotox. Res. 2020, 38, 228–241. [Google Scholar] [CrossRef]


| TDT Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Girls | Boys | Full Sample | Girls | Boys | Full Sample | |
| Age | 15.4 ± 2.6 (11−18) | 15.1 ± 2.9 (11−18) | 15.2 ± 2.8 (11−18) | 14.6 ± 2.1 (10−18) | 14.8 ± 1.9 (11−18) | 14.7 ± 2.0 (10−18) |
| TDT Group | Control Group | |||
|---|---|---|---|---|
| Girls | Boys | Girls | Boys | |
| General Anxiety | 59.3 ± 11.7 (42−80) | 63.9 ± 13.2 (44−80) | 54.2 ± 4.4 (43−64) | 54.7 ± 4.7 (41−65) |
| Separation Anxiety | 61.2 ± 13.5 (42−80) | 67.7 ± 12.3 (46−80) | 47.5 ± 6.9 (41−66) | 47.9 ± 6.1 (38−65) |
| Panic Disorder | 63.2 ± 12.9 (41−80) | 71.2 ± 12.7 (46−80) | 54.1 ± 5.3 (48−78) | 52.7 ± 4.8 (40−65) |
| Social Phobia | 48.8 ± 11.9 (31−80) | 57.8 ± 13.6 (35−80) | 38.9 ± 10.5 (30−66) | 41.5 ± 10.1 (30−66) |
| Obsession | 61.7 ± 12.1 (43−80) | 67.7 ± 11.8 (47−80) | 47.2 ± 11.5 (38−77) | 48.9 ± 10.6 (38−70) |
| Depression | 60.6 ± 12.2 (41−80) | 65.0 ± 13.2 (42−0) | 48.6 ± 8.7 (41−73) | 50.2 ± 8.2 (41−65) |
| Total Anxiety | 59.4 ± 12.7 (40−80) | 67.4 ± 13 (42−80) | 47.9 ± 9.0 (40−71) | 49.6 ± 8.1 (40−61) |
| Total Depression | 60.1 ± 12.4 (42−80) | 67.6 ± 12.6 (45−80) | 48.8 ± 9.0 (41−73) | 50.5 ± 8.3 (41−62) |
| RCADS Subscale Scores Mean ± SD | RCADS Elevated Score Percentage (>70 Points) | |||||
|---|---|---|---|---|---|---|
| Patient (n = 40) | Control (n = 62) | p | Patient (n = 40) | Control (n = 62) | p | |
| General Anxiety | 62.0 ± 12.6 | 54.4 ± 4.5 | 0.003 M | 25.0% (n = 10) | 0% | <0.001 F |
| Separation Anxiety | 64.9 ± 13.1 | 47.7 ± 6.4 | <0.001 S | 40.0% (n = 16) | 0% | <0.001 C |
| Panic Disorder | 67.8 ± 13.2 | 53.4 ± 5.1 | <0.001 M | 55.0% (n = 22) | 1.6% (n = 1) | <0.001 F |
| Social Phobia | 54.0 ± 13.5 | 40.2 ± 10.3 | <0.001 M | 12.5% (n = 5) | 0% | 0.008 F |
| Obsession | 65.1 ± 12.1 | 48.0 ± 11.0 | <0.001 M | 42.5% (n = 17) | 1.6% (n = 1) | <0.001 F |
| Depression | 63.1 ± 12.8 | 49.4 ± 8.5 | <0.001 M | 32.5% (n = 13) | 1.6% (n = 1) | <0.001 F |
| Total Anxiety | 64.0 ± 13.3 | 48.7 ± 8.5 | <0.001 M | 32.5% (n = 13) | 1.6% (n = 1) | <0.001 C |
| Total Depression | 64.4 ± 12.9 | 49.6 ± 8.6 | <0.001 M | 35.0% (n = 14) | 1.6% (n = 1) | <0.001 C |
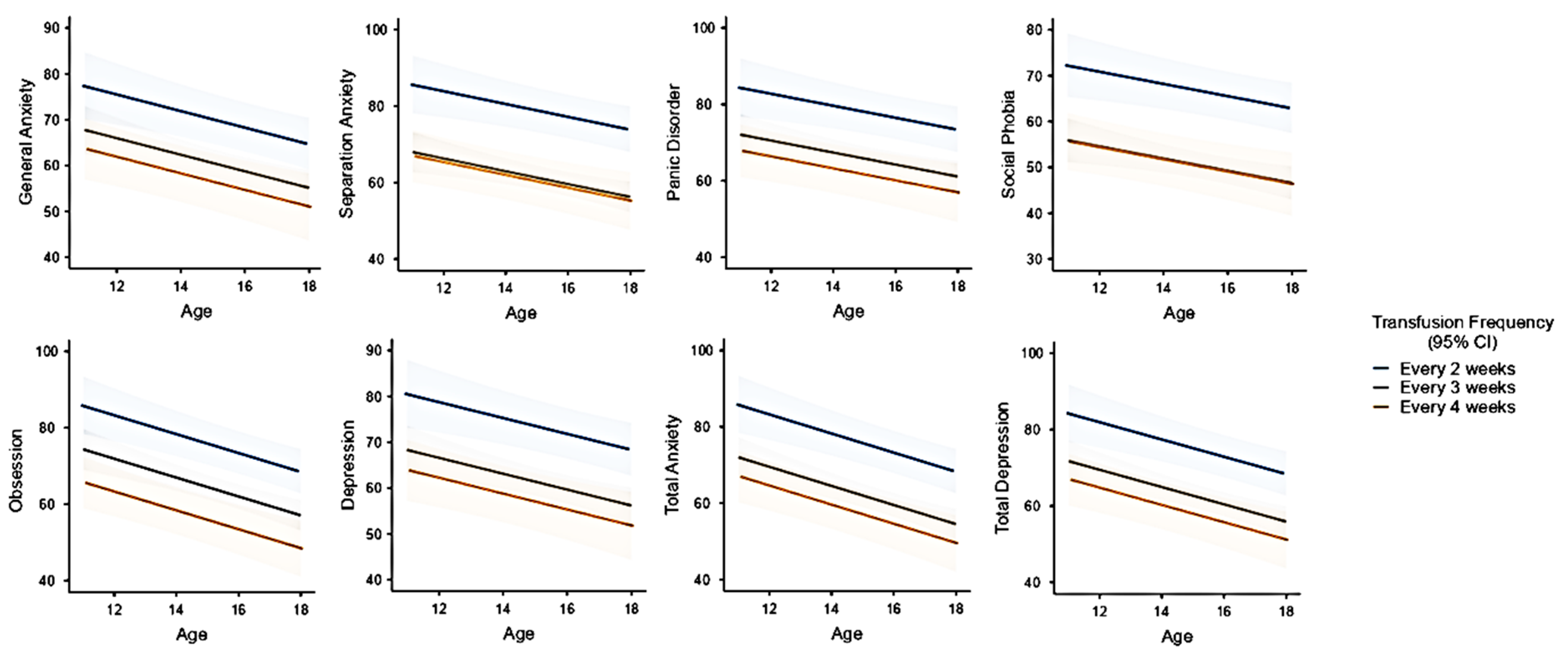
| Transfusion Frequency | Age | General Anxiety | Separation Anxiety | Panic Disorder | Social Phobia | Obsession | Depression | Total Anxiety | Total Depression |
|---|---|---|---|---|---|---|---|---|---|
| Every 2 weeks | 12 | 75 (65−84) | 83 (74−92) | 82 (72−95) | 70 (60−79) | 82 (75−90) | 78 (69−87) | 82 (73−91) | 81 (72−90) |
| 15 | 70 (62−78) | 79 (71−86) | 78 (69−86) | 66 (58−75) | 76 (69−82) | 73 (66−81) | 75 (68−83) | 75 (67−82) | |
| 18 | 65 (57−74) | 74 (66−82) | 74 (65−82) | 63 (55−72) | 69 (62−75) | 69 (60−77) | 69 (61−77) | 69 (61−77) | |
| Every 3 weeks | 12 | 65 (59−72) | 66 (60−72) | 70 (63−76) | 54 (47−60) | 71 (66−76) | 66 (60−72) | 68 (63−74) | 69 (63−74) |
| 15 | 61 (56−65) | 61 (57−66) | 66 (61−71) | 50 (46−55) | 64 (60−68) | 61 (57−66) | 62 (57−66) | 62 (58−67) | |
| 18 | 56 (50−62) | 57 (51−62) | 62 (55−68) | 47 (41−53) | 57 (52−62) | 56 (50−62) | 55 (50−61) | 56 (51−62) | |
| Every 4 weeks | 12 | 61 (51−71) | 65 (55−74) | 65 (55−76) | 54 (44−64) | 62 (54−70) | 61 (52−71) | 63 (54−72) | 63 (54−73) |
| 15 | 56 (46−66) | 60 (51−69) | 61 (51−72) | 50 (40−61) | 55 (47−63) | 56 (47−66) | 56 (47−66) | 57 (48−67) | |
| 18 | 51 (40−63) | 56 (45−66) | 57 (45−70) | 47 (35−59) | 48 (39−57) | 51 (40−63) | 50 (39−61) | 51 (40−62) |
| Scales | Bayesian Kendall’s Tau | BF10 | Evidence |
|---|---|---|---|
| General Anxiety | 0.263 | 3.294 | Moderate (H1) |
| Separation Anxiety | 0.292 | 6.291 | Moderate (H1) |
| Panic Disorder | 0.076 | 0.258 | Moderate (H0) |
| Social Phobia | 0.262 | 3.184 | Moderate (H1) |
| Obsession | 0.140 | 0.448 | Anecdotal (H0) |
| Depression | 0.158 | 0.554 | Anecdotal (H0) |
| Total Anxiety | 0.102 | 0.310 | Moderate (H0) |
| Total Depression | 0.205 | 1.1 | Anecdotal (H1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yetim Şahin, A.; Kandemir, I.; Dağ, H.; Türkkan, E.; Tuğrul Aksakal, M.; Sahin, M.; Baş, F.; Karakaş, Z. Assessing Psychological Disorders in Turkish Adolescents with Transfusion-Dependent Thalassemia. Children 2024, 11, 837. https://doi.org/10.3390/children11070837
Yetim Şahin A, Kandemir I, Dağ H, Türkkan E, Tuğrul Aksakal M, Sahin M, Baş F, Karakaş Z. Assessing Psychological Disorders in Turkish Adolescents with Transfusion-Dependent Thalassemia. Children. 2024; 11(7):837. https://doi.org/10.3390/children11070837
Chicago/Turabian StyleYetim Şahin, Aylin, Ibrahim Kandemir, Hüseyin Dağ, Emine Türkkan, Melike Tuğrul Aksakal, Memduh Sahin, Firdevs Baş, and Zeynep Karakaş. 2024. "Assessing Psychological Disorders in Turkish Adolescents with Transfusion-Dependent Thalassemia" Children 11, no. 7: 837. https://doi.org/10.3390/children11070837
APA StyleYetim Şahin, A., Kandemir, I., Dağ, H., Türkkan, E., Tuğrul Aksakal, M., Sahin, M., Baş, F., & Karakaş, Z. (2024). Assessing Psychological Disorders in Turkish Adolescents with Transfusion-Dependent Thalassemia. Children, 11(7), 837. https://doi.org/10.3390/children11070837







