Sex Differences in Children with Uncomplicated Attention Deficit/Hyperactivity Disorder and Sleep Problems
Abstract
1. Introduction
2. Materials and Methods
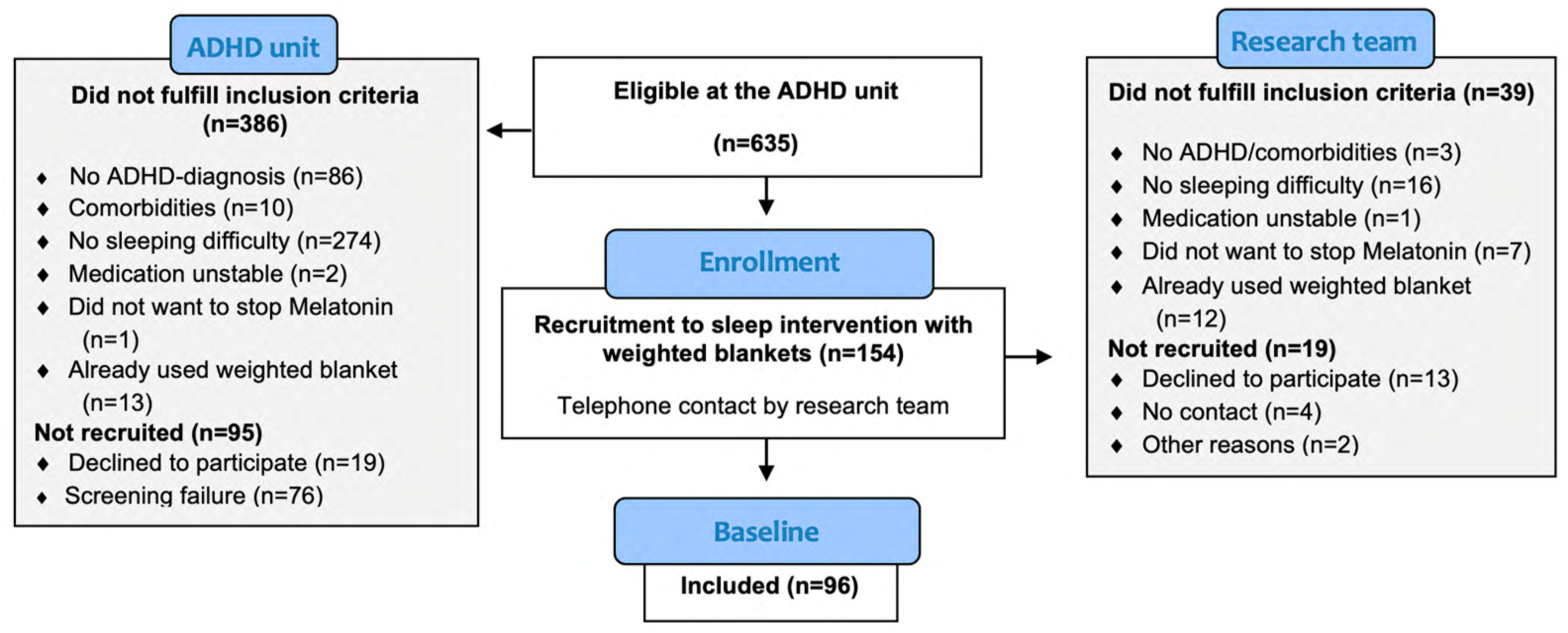
2.1. Study Participants and Design
2.2. Measurements
2.2.1. ActiGraph
2.2.2. Children’s Sleep Habits Questionnaire
2.2.3. Insomnia Severity Index
2.2.4. The Parent-Reported Swanson, Nolan and Pelham Rating Scale
2.2.5. EuroQol-5 Dimensions-Youth
2.2.6. Child Outcome Rating Scale
2.2.7. The Short Form of the State-Trait Anxiety Inventory
2.3. Statistics
3. Results
3.1. Demographic Characteristics
3.2. Objectively Measured Sleep
3.3. Subjectively Measured Sleep
3.4. ADHD and Anxiety Symptoms
3.5. Functioning in Daily Life
3.6. Differences between Children Who Reported No or Some Problems Such as Feeling Worried, Sad, or Unhappy in EQ-5D-Y
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variables | Not Worried, Sad, or Unhappy (n = 50) | Worried, Sad, or Unhappy (n = 46) | p |
|---|---|---|---|
| Age | |||
| Median | 10.00 | 9.00 ^ | 0.232 |
| Range | 6–14 | 6–13 | |
| Diagnosis | |||
| Attention deficit, n (%) | 13 (26) | 12 (26) ” | 0.992 |
| Hyperactivity, n (%) | 1 (2) | 2 (4) | |
| Combined hyperactivity and attention deficit, n (%) | 36 (72) | 32 (70) | |
| Medication | |||
| Melatonin, n (%) | 3 (6) | 6 (13) ” | 0.163 |
| Stimulants, n (%) | 25 (50) | 22 (47.8) * | 0.588 |
| Iso Body mass index | |||
| Underweight, n (%) | 4 (8) | 1 (2) ” | 0.136 |
| Normal weight, n (%) | 28 (56) | 27 (58.7) | |
| Overweight, n (%) | 14 (28) | 8 (17.3) | |
| Obesity, n (%) | 4 (8) | 10 (21.7) | |
| Parental education | |||
| University, n (%) | 26 (52.1) | 29 (63) ” | 0.244 |
| Upper secondary school, n (%) | 22 (44) | 13 (28.3) | |
| Elementary school, n (%) | 2 (4) | 4 (8.7) | |
| Parental age | |||
| 20–30, n (%) | 2 (4) | 1 (2.1) ” | 0.786 |
| 31–40, n (%) | 28 (56) | 29 (63) | |
| 41–50, n (%) | 15 (30) | 15 (32) | |
| >50, n (%) | 5 (10) | 1 (2.1) |
| ActiGraph | Not Worried, Sad, or Unhappy (n = 50) | Worried, Sad, or Unhappy (n = 46) | p |
|---|---|---|---|
| Number of days (n) | |||
| Mean, Sd, Median | 6.71 ± 0.61, 7.00 | 7.00 | 0.972 |
| 7 | 39 | 39 | |
| 6 | 6 | 5 | |
| 5 | 4 | 1 | |
| Missing (n) | 1 | 1 | |
| Total sleep time (mean, sd, median) | 481.37 ± 53.98, 470.29 | 497.18 ± 46.79, 500.29 | 0.134 |
| Sleep onset latency (mean, sd, median) | 38.30 ± 34.63, 27.20 | 30.66 ± 19.24, 27.29 | 0.384 |
| Sleep efficiency (mean, sd, median) | 86.29 ± 4.13, 86.63 | 87.16 ± 3.61, 87.67 | 0.771 |
| Wake after sleep onset (mean, sd, median) | 41.40 ± 16.86, 39.43 | 42.32 ± 16.46, 40.00 | 0.438 |
| Questionnaires | Not Worried, Sad, or Unhappy (n = 50) | Worried, Sad, or Unhappy (n = 46) | p |
|---|---|---|---|
| CSHQ | |||
| Total sum (mean, sd, median) | 50.64 ± 7.66, 50.50 | 53.91 ± 7.63, 55.00 | 0.027 |
| Missing (n) | 2 | 1 | |
| ISI | |||
| Total score (mean, sd, median) | 8.14 ± 4.78, 7.00 | 11.80 ± 4.44, 10.50 | <0.001 |
| Measure Instrument | Not Worried, Sad, or Unhappy (n = 50) | Worried, Sad, or Unhappy (n = 46) | p |
|---|---|---|---|
| SNAP IV-parent | |||
| Inattention score, (mean, sd) | 18.12 ± 4.91 | 17.15 ± 5.22 * | 0.351 |
| Hyperactivity/impulsivity score (mean, sd) | 14.78 ± 5.50 | 15.37 ± 6.20 * | 0.623 |
| Inattention | |||
| <13 | 8 | 9 | |
| 13–17 | 15 | 15 | |
| 18–22 | 15 | 25 | |
| 23–27 | 12 | 7 | |
| Missing (n) | 0 | 0 | |
| Hyperactivity/impulsivity | |||
| <13 | 16 | 12 | |
| 13–17 | 17 | 16 | |
| 18–22 | 11 | 11 | |
| 23–27 | 6 | 7 | |
| Missing (n) | 0 | 0 | |
| Short STAI | |||
| Total score | 9.78 ± 3.48, 9.00 | 12.28 ± 3.43, 12.00 ^ | <0.001 |
| Range | 6–19 | 6–19 |
| Questionnaire | Not Worried, Sad, or Unhappy | Worried, Sad, or Unhappy | p |
|---|---|---|---|
| (n = 50) | (n = 46) | ||
| CORS | |||
| total score (mean, sd, median) | 34.13 ± 5.12, 35.25 | 27.98 ± 6.07, 28.60 | <0.001 |
| ≥28 (n) | 45 | 25 | |
| <28 (n) | 5 | 21 | |
| Me (mean, sd, median) | 8.92 ± 1.43, 9.80 | 7.12 ± 2.23, 7.40 | 0.013 |
| Family (mean, sd, median) | 8.90 ± 21.60, 9.80 | 7.89 ± 2.03, 8.55 | 0.030 |
| School (mean, sd, median) | 7.32 ± 2.48, 7.75 | 6.17 ± 2.76, 6.00 | <0.001 |
| Life (mean, sd, median) | 8.99 ± 1.34, 9.85 | 6.79 ± 2.49, 7.25 | <0.001 |
| Total Sleep Time | <9 Years of Age | >9 Years of Age | p |
|---|---|---|---|
| (n = 37) | (n = 57) | ||
| Mean, sd | 521 ± 40.77 | 467.78 ± 45.79 | <0.001 |
| Missing (n) | 0 | 2 |
References
- Salari, N.; Ghasemi, H.; Abdoli, N.; Rahmani, A.; Shiri, M.H.; Hashemian, A.H.; Akbari, H.; Mohammadi, M. The global prevalence of ADHD in children and adolescents: A systematic review and meta-analysis. Ital. J. Pediatr. 2023, 49, 48. [Google Scholar] [CrossRef]
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [Internet]; American Psychiatric Association Publishing: Washington, DC, USA, 2013.
- Russell, G.; Ford, T.; Rosenberg, R.; Kelly, S. The association of attention deficit hyperactivity disorder with socioeconomic disadvantage: Alternative explanations and evidence. J. Child Psychol. Psychiatry 2014, 55, 436–445. [Google Scholar] [CrossRef]
- Biederman, J.; Faraone, S.V. Attention-deficit hyperactivity disorder. Lancet 2005, 366, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Faraone, S.V.; Banaschewski, T.; Coghill, D.; Zheng, Y.; Biederman, J.; Bellgrove, M.A.; Newcorn, J.H.; Gignac, M.; Al Saud, N.M.; Manor, I.; et al. The World Federation of ADHD International Consensus Statement: 208 Evidence-based conclusions about the disorder. Neurosci. Biobehav. Rev. 2021, 128, 789–818. [Google Scholar] [CrossRef] [PubMed]
- The Social Welfare Board. Diagnoses in Inpatient Care and Specialised Outpatient Care. Available online: https://www.socialstyrelsen.se/statistik-och-data/statistik/statistikdatabasen (accessed on 1 October 2023).
- Gershon, J. A meta-analytic review of gender differences in ADHD. J. Atten. Disord. 2002, 5, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Hinshaw, S.P.; Nguyen, P.T.; O’Grady, S.M.; Rosenthal, E.A. Annual Research Review: Attention-deficit/hyperactivity disorder in girls and women: Underrepresentation, longitudinal processes, and key directions. J. Child Psychol. Psychiatry 2022, 63, 484–496. [Google Scholar] [CrossRef] [PubMed]
- Young, S.; Adamo, N.; Asgeirsdottir, B.B.; Branney, P.; Beckett, M.; Colley, W.; Cubbin, S.; Deeley, Q.; Farrag, E.; Gudjonsson, G.; et al. Females with ADHD: An expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/hyperactivity disorder in girls and women. BMC Psychiatry 2020, 20, 404. [Google Scholar] [CrossRef]
- Carucci, S.; Narducci, C.; Bazzoni, M.; Balia, C.; Donno, F.; Gagliano, A.; Zuddas, A. Clinical characteristics, neuroimaging findings, and neuropsychological functioning in attention-deficit hyperactivity disorder: Sex differences. J. Neurosci. Res. 2023, 101, 704–717. [Google Scholar] [CrossRef] [PubMed]
- Quinn, P.O.; Madhoo, M. A review of attention-deficit/hyperactivity disorder in women and girls: Uncovering this hidden diagnosis. Prim. Care Companion CNS Disord. 2014, 16, 27250. [Google Scholar] [CrossRef]
- Rucklidge, J.J. Gender differences in attention-deficit/hyperactivity disorder. Psychiatr. Clin. N. Am. 2010, 33, 357–373. [Google Scholar] [CrossRef]
- Cortese, S.; Faraone, S.V.; Konofal, E.; Lecendreux, M. Sleep in children with attention-deficit/hyperactivity disorder: Meta-analysis of subjective and objective studies. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 894–908. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Zimmerman, A.W. Sleep in Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder. Semin. Pediatr. Neurol. 2015, 22, 113–125. [Google Scholar] [CrossRef]
- Van Dongen, H.P.; Maislin, G.; Mullington, J.M.; Dinges, D.F. The cumulative cost of additional wakefulness: Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep 2003, 26, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Gross, D.W.; Gotman, J. Correlation of high-frequency oscillations with the sleep-wake cycle and cognitive activity in humans. Neuroscience 1999, 94, 1005–1018. [Google Scholar] [CrossRef]
- Gosling, C.J.; Cortese, S.; Konofal, E.; Lecendreux, M.; Faraone, S.V. Association of Parent-Rated Sleep Disturbances With Attention-Deficit/Hyperactivity Disorder Symptoms: 9-Year Follow-up of a Population-Based Cohort Study. J. Am. Acad. Child Adolesc. Psychiatry 2023, 62, 244–252. [Google Scholar] [CrossRef]
- Bondopadhyay, U.; Diaz-Orueta, U.; Coogan, A.N. A Systematic Review of Sleep and Circadian Rhythms in Children with Attention Deficit Hyperactivity Disorder. J. Atten. Disord. 2022, 26, 149–224. [Google Scholar] [CrossRef] [PubMed]
- Lucas, I.; Mulraney, M.; Sciberras, E. Sleep problems and daytime sleepiness in children with ADHD: Associations with social, emotional, and behavioral functioning at school, a cross-sectional study. Behav. Sleep Med. 2019, 17, 411–422. [Google Scholar] [CrossRef] [PubMed]
- Sung, V.; Hiscock, H.; Sciberras, E.; Efron, D. Sleep problems in children with attention-deficit/hyperactivity disorder: Prevalence and the effect on the child and family. Arch. Pediatr. Adolesc. Med. 2008, 162, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.A.; Papadopoulos, N.; Chellew, T.; Rinehart, N.J.; Sciberras, E. Associations between parenting stress, parent mental health and child sleep problems for children with ADHD and ASD: Systematic review. Res. Dev. Disabil. 2019, 93, 103463. [Google Scholar] [CrossRef]
- Chaput, J.P.; Gray, C.E.; Poitras, V.J.; Carson, V.; Gruber, R.; Olds, T.; Weiss, S.K.; Gorber, S.C.; Kho, M.E.; Sampson, M.; et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. Physiol. Appl. Nutr. Metabolisme 2016, 41 (Suppl. S3), S266–S282. [Google Scholar] [CrossRef]
- Schlieber, M.; Han, J. The Role of Sleep in Young Children’s Development: A Review. J. Genet. Psychol. 2021, 182, 205–217. [Google Scholar] [CrossRef] [PubMed]
- Corkum, P.; Tannock, R.; Moldofsky, H.; Hogg-Johnson, S.; Humphries, T. Actigraphy and parental ratings of sleep in children with attention-deficit/hyperactivity disorder (ADHD). Sleep 2001, 24, 303–312. [Google Scholar] [CrossRef]
- Hodgkins, P.; Setyawan, J.; Mitra, D.; Davis, K.; Quintero, J.; Fridman, M.; Shaw, M.; Harpin, V. Management of ADHD in children across Europe: Patient demographics, physician characteristics and treatment patterns. Eur. J. Pediatr. 2013, 172, 895–906. [Google Scholar] [CrossRef]
- Owens, J.A. The ADHD and sleep conundrum: A review. J. Dev. Behav. Pediatr. JDBP 2005, 26, 312–322. [Google Scholar] [CrossRef] [PubMed]
- Yürümez, E.; Kılıç, B.G. Relationship Between Sleep Problems and Quality of Life in Children With ADHD. J. Atten. Disord. 2016, 20, 34–40. [Google Scholar] [CrossRef]
- Efron, D.; Lycett, K.; Sciberras, E. Use of sleep medication in children with ADHD. Sleep Med. 2014, 15, 472–475. [Google Scholar] [CrossRef]
- Quach, J.; Hiscock, H.; Wake, M. Sleep problems and mental health in primary school new entrants: Cross-sectional community-based study. J. Paediatr. Child Health 2012, 48, 1076–1081. [Google Scholar] [CrossRef]
- Becker, S.P.; Cusick, C.N.; Sidol, C.A.; Epstein, J.N.; Tamm, L. The impact of comorbid mental health symptoms and sex on sleep functioning in children with ADHD. Eur. Child Adolesc. Psychiatry 2018, 27, 353–365. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.Y.; Jain, U.; Shapiro, C. Sleep in attention-deficit/hyperactivity disorder in children and adults: Past, present, and future. Sleep Med. Rev. 2012, 16, 371–388. [Google Scholar] [CrossRef]
- Kirov, R.; Kinkelbur, J.; Heipke, S.; Kostanecka-Endress, T.; Westhoff, M.; Cohrs, S.; Ruther, E.; Hajak, G.; Banaschewski, T.; Rothenberger, A. Is there a specific polysomnographic sleep pattern in children with attention deficit/hyperactivity disorder? Sleep Res. 2004, 13, 87–93. [Google Scholar] [CrossRef]
- Miano, S.; Donfrancesco, R.; Bruni, O.; Ferri, R.; Galiffa, S.; Pagani, J.; Montemitro, E.; Kheirandish, L.; Gozal, D.; Villa, M.P. NREM sleep instability is reduced in children with attention-deficit/hyperactivity disorder. Sleep 2006, 29, 797–803. [Google Scholar] [PubMed]
- Ball, J.D.; Tiernan, M.; Janusz, J.; Furr, A. Sleep patterns among children with attention-deficit hyperactivity disorder: A reexamination of parent perceptions. J. Pediatr. Psychol. 1997, 22, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Stein, D.; Pat-Horenczyk, R.; Blank, S.; Dagan, Y.; Barak, Y.; Gumpel, T.P. Sleep disturbances in adolescents with symptoms of attention-deficit/hyperactivity disorder. J. Learn. Disabil. 2002, 35, 268–275. [Google Scholar] [CrossRef]
- Chervin, R.D.; Dillon, J.E.; Bassetti, C.; Ganoczy, D.A.; Pituch, K.J. Symptoms of sleep disorders, inattention, and hyperactivity in children. Sleep 1997, 20, 1185–1192. [Google Scholar] [CrossRef] [PubMed]
- Owens, J.A.; Maxim, R.; Nobile, C.; McGuinn, M.; Msall, M. Parental and self-report of sleep in children with attention-deficit/hyperactivity disorder. Arch. Pediatr. Adolesc. Med. 2000, 154, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Jin, X.; Yan, C.; Wu, S.; Jiang, F.; Shen, X. Sleep problems in chinese school-aged children with a parent-reported history of ADHD. J. Atten. Disord. 2009, 13, 18–26. [Google Scholar] [PubMed]
- Lim, C.G.; Ooi, Y.P.; Fung, D.S.; Mahendran, R.; Kaur, A. Sleep disturbances in Singaporean children with attention deficit hyperactivity disorder. Ann. Acad. Med. Singap. 2008, 37, 655–661. [Google Scholar] [CrossRef]
- Agostini, A.; Centofanti, S. Normal Sleep in Children and Adolescence. Child. Adolesc. Psychiatr. Clin. N. Am. 2021, 30, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Stražišar, B.G. Sleep Measurement in Children-Are We on the Right Track? Sleep Med. Clin. 2021, 16, 649–660. [Google Scholar] [CrossRef]
- Riley, A.W. Evidence that school-age children can self-report on their health. Ambul. Pediatr. 2004, 4 (Suppl. S4), 371–376. [Google Scholar] [CrossRef]
- Chorney, D.B.; Detweiler, M.F.; Morris, T.L.; Kuhn, B.R. The interplay of sleep disturbance, anxiety, and depression in children. J. Pediatr. Psychol. 2008, 33, 339–348. [Google Scholar] [CrossRef] [PubMed]
- Lönn, M.; Svedberg, P.; Nygren, J.; Jarbin, H.; Aili, K.; Larsson, I. The efficacy of weighted blankets for sleep in children with attention-deficit/hyperactivity disorder—A randomized controlled crossover trial. J. Sleep Res. 2024, 33, e13990. [Google Scholar] [CrossRef] [PubMed]
- Larsson, I.; Aili, K.; Nygren, J.M.; Johansson, P.; Jarbin, H.; Svedberg, P. SLEEP: Intervention with weighted blankets for children with attention deficit hyperactivity disorder (ADHD) and sleep problems: Study protocol for a randomised control trial. BMJ Open 2022, 12, e047509. [Google Scholar] [CrossRef] [PubMed]
- Wernersson, R.; Johansson, J.; Andersson, M.; Jarbin, H. Evaluation of a new model for assessment and treatment of uncomplicated ADHD—Effect, patient satisfaction and costs. Nord. J. Psychiatry 2020, 74, 96–104. [Google Scholar] [CrossRef]
- Sadeh, A. The role and validity of actigraphy in sleep medicine: An update. Sleep Med. Rev. 2011, 15, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Owens, J.A.; Spirito, A.; McGuinn, M. The Children’s Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep 2000, 23, 1043–1051. [Google Scholar] [CrossRef] [PubMed]
- Owens, J.; Maxim, R.; McGuinn, M.; Nobile, C.; Msall, M.; Alario, A. Television-viewing habits and sleep disturbance in school children. Pediatrics 1999, 104, e27. [Google Scholar] [CrossRef] [PubMed]
- Larsson, I.; Svedberg, P.; Nygren, J.M.; Malmborg, S.J. Validity and reliability of the Swedish version of the Children’s sleep Habits Questionnaire (CSHQ-SWE). BMC Pediatrics, 2024; resubmitted. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Chung, K.F.; Kan, K.K.; Yeung, W.F. Assessing insomnia in adolescents: Comparison of Insomnia Severity Index, Athens Insomnia Scale and Sleep Quality Index. Sleep Med. 2011, 12, 463–470. [Google Scholar] [CrossRef]
- Hall, C.L.; Guo, B.; Valentine, A.Z.; Groom, M.J.; Daley, D.; Sayal, K.; Hollis, C. The Validity of the SNAP-IV in Children Displaying ADHD Symptoms. Assessment 2020, 27, 1258–1271. [Google Scholar] [CrossRef]
- Swanson, J.M.; Kraemer, H.C.; Hinshaw, S.P.; Arnold, L.E.; Conners, C.K.; Abikoff, H.B.; Clevenger, W.; Davies, M.; Elliott, G.R.; Greenhill, L.L.; et al. Clinical relevance of the primary findings of the MTA: Success rates based on severity of ADHD and ODD symptoms at the end of treatment. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 168–179. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Wille, N.; Badia, X.; Bonsel, G.; Burström, K.; Cavrini, G.; Devlin, N.; Egmar, A.-C.; Gusi, N.; Herdman, M.; et al. Feasibility, reliability, and validity of the EQ-5D-Y: Results from a multinational study. Qual. Life Res. 2010, 19, 887–897. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.; Duncan, B.I.; Brown, J. The Outcome Rating Scale: A Preliminary Study of the Reliability, Validity and Feasibility of a Brief Visual Analog Measure. J. Brief Ther. 2003, 2, 91–100. [Google Scholar]
- Duncan, B.L.; Sparks Jacqueline, A.; Miller, S.D.; Bohanske, R.T.; Claud, D.A. Giving youth a voice: A preliminary study of the reliability and validity of a brief outcome measure for children, adolescents, and caretakers. J. Brief Ther. 2006, 5, 71–88. [Google Scholar]
- Marteau, T.M.; Bekker, H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI). Br. J. Clin. Psychol. 1992, 31, 301–306. [Google Scholar] [CrossRef]
- Nilsson, S.; Buchholz, M.; Thunberg, G. Assessing Children’s Anxiety Using the Modified Short State-Trait Anxiety Inventory and Talking Mats: A Pilot Study. Nurs. Res. Pract. 2012, 2012, 932570. [Google Scholar] [CrossRef]
- Gaub, M.; Carlson, C.L. Gender differences in ADHD: A meta-analysis and critical review. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 1036–1045. [Google Scholar] [CrossRef] [PubMed]
- Slobodin, O.; Davidovitch, M. Gender Differences in Objective and Subjective Measures of ADHD Among Clinic-Referred Children. Front. Hum. Neurosci. 2019, 13, 441. [Google Scholar] [CrossRef]
- Virring, A.; Lambek, R.; Thomsen, P.H.; Møller, L.R.; Jennum, P.J. Disturbed sleep in attention-deficit hyperactivity disorder (ADHD) is not a question of psychiatric comorbidity or ADHD presentation. J. Sleep Res. 2016, 25, 333–340. [Google Scholar] [CrossRef]
- Godino, J.G.; Wing, D.; de Zambotti, M.; Baker, F.C.; Bagot, K.; Inkelis, S.; Pautz, C.; Higgins, M.; Nichols, J.; Brumback, T.; et al. Performance of a commercial multi-sensor wearable (Fitbit Charge HR) in measuring physical activity and sleep in healthy children. PLoS ONE 2020, 15, e0237719. [Google Scholar] [CrossRef]
- Sadeh, A.; Pergamin, L.; Bar-Haim, Y. Sleep in children with attention-deficit hyperactivity disorder: A meta-analysis of polysomnographic studies. Sleep. Med. Rev. 2006, 10, 381–398. [Google Scholar] [CrossRef]
- Virring, A.; Lambek, R.; Jennum, P.J.; Møller, L.R.; Thomsen, P.H. Sleep Problems and Daily Functioning in Children With ADHD: An Investigation of the Role of Impairment, ADHD Presentations, and Psychiatric Comorbidity. J. Atten. Disord. 2017, 21, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Chiraphadhanakul, K.; Jaimchariyatam, N.; Pruksananonda, C.; Chonchaiya, W. Increased Sleep Disturbances in Thai Children With Attention-Deficit Hyperactivity Disorder Compared with Typically Developing Children. Behav. Sleep Med. 2016, 14, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Lycett, K.; Mensah, F.K.; Hiscock, H.; Sciberras, E. Comparing subjective measures of behavioral sleep problems in children with ADHD: A cross-sectional study. Sleep Med. 2015, 16, 1377–1380. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Shea, K.S.C.; Chiu, W.V.; Lau, F.L.F.; Wong, C.K.D.; Yu, W.M.M.; Li, A.M.; Wing, Y.K.; Lai, Y.C.K.; Li, S.X. The associations of insomnia symptoms with daytime behavior and cognitive functioning in children with attention-deficit/hyperactivity disorder. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2022, 18, 2029–2039. [Google Scholar] [CrossRef]
- Lunsford-Avery, J.R.; Krystal, A.D.; Kollins, S.H. Sleep disturbances in adolescents with ADHD: A systematic review and framework for future research. Clin. Psychol. Rev. 2016, 50, 159–174. [Google Scholar] [CrossRef]
- Goldman, S.E.; Richdale, A.L.; Clemons, T.; Malow, B.A. Parental sleep concerns in autism spectrum disorders: Variations from childhood to adolescence. J. Autism Dev. Disord. 2012, 42, 531–538. [Google Scholar] [CrossRef]
- Peasgood, T.; Bhardwaj, A.; Biggs, K.; Brazier, J.E.; Coghill, D.; Cooper, C.L.; Daley, D.; De Silva, C.; Harpin, V.; Hodgkins, P.; et al. The impact of ADHD on the health and well-being of ADHD children and their siblings. Eur. Child Adolesc. Psychiatry 2016, 25, 1217–1231. [Google Scholar] [CrossRef]
| Variables | Boys (n = 55) | Girls (n = 41) | p |
|---|---|---|---|
| Age | |||
| Median | 9.00 | 10.00 ^ | 0.011 |
| Range | 6–13 | 6–14 | |
| Diagnosis | |||
| Attention deficit, n (%) | 10 (18) | 15 (37) ” | 0.023 |
| Hyperactivity, n (%) | 3 (6) | 0 (0) | |
| Combined hyperactivity/attention deficit, n (%) | 42 (76) | 26 (63) | |
| Medication | |||
| Melatonin, n (%) | 6 (10.8) | 3 (7.8) ” | 0.449 |
| Stimulants, n (%) | 31 (55) | 16 (40) * | 0.103 |
| Iso Body mass index | |||
| Underweight, n (%) | 2 (3.6) | 3 (7.3) ” | 0.814 |
| Normal weight, n (%) | 32 (57.1) | 23 (58) | |
| Overweight, n (%) | 14 (25.5) | 8 (19.5) | |
| Obesity, n (%) | 8 (14.5) | 6 (14.6) | |
| Parental education | |||
| University, n (%) | 32 (58.2) | 23 (56) ” | 1.000 |
| Upper secondary school, n (%) | 20 (36.3) | 15 (36.5) | |
| Elementary school, n (%) | 3 (5.4) | 3 (7.3) | |
| Parental age | |||
| 20–30, n (%) | 2 (3.6) | 1 (2.4) ” | 0.694 |
| 31–40, n (%) | 36 (65.5) | 21 (51.2) | |
| 41–50, n (%) | 14 (25.5) | 16 (39) | |
| >50, n (%) | 3 (5.4) | 3 (7.3) |
| ActiGraph | Boys (n = 55) | Girls (n = 41) | p |
|---|---|---|---|
| Number of days (n) | |||
| Mean, Sd, Median | 6.85 ± 0.41, 7.00 | 6.68 ± 0.66, 7.00 | 0.188 |
| 7 | 47 | 31 | |
| 6 | 6 | 5 | |
| 5 | 1 | 4 | |
| Missing (n) | 1 | 1 | |
| Total sleep time (mean, sd, median) | 493.37 ± 43.57, 489.07 | 482.94 ± 59.70, 475.57 | 0.468 |
| Sleep onset latency (mean, sd, median) | 36.04 ± 25.04, 29.86 | 32.76 ± 32.71, 21.00 | 0.175 |
| Sleep efficiency (mean, sd, median) | 86.26 ± 4.16, 86.61 | 86.99 ± 5.41, 88.22 | 0.206 |
| Wake after sleep onset (mean, sd, median) | 43.02 ± 14.69, 39.36 | 40.26 ± 18.92, 38.71 | 0.206 |
| Questionnaires | Boys (n = 55) | Girls (n = 41) | p |
|---|---|---|---|
| CSHQ (parent-reported) | |||
| Bedtime resistance (mean, sd, median) | 9.64 ± 3.36, 9.00 | 8.85 ± 3.02, 8.00 | 0.324 |
| Missing (n) | 0 | 0 | |
| Sleep onset delay (mean, sd, median) | 2.27 ± 0.80, 2.00 | 2.32 ± 0.61, 2.00 | 0.965 |
| Missing (n) | 0 | 0 | |
| Sleep duration (mean, sd, median) | 5.27 ± 1.75, 5.00 | 5.63 ± 1.66, 6.00 | 0.322 |
| Missing (n) | 0 | 0 | |
| Sleep anxiety (mean, sd, median) | 6.73 ± 2.54, 7.00 | 5.63 ± 2.35, 5.00 | 0.022 |
| Missing (n) | 2 | 1 | |
| Night-time awakenings (mean, sd, median) | 5.04 ± 1.86, 5.00 | 4.15 ± 1.67, 4.00 | 0.032 |
| Missing (n) | 0 | 1 | |
| Parasomnias (mean, sd, median) | 9.13 ± 1.92, 9.00 | 8.44 ± 2.48, 8.00 | 0.073 |
| Missing (n) | 0 | 1 | |
| Sleep disorder breathing (mean, sd, median) | 3.20 ± 0.45, 3.00 | 3.10 ± 0.74, 3.00 | 0.794 |
| Missing (n) | 1 | 2 | |
| Daytime sleepiness (mean, sd, median) | 15.15 ± 3.79, 15:00 * | 16.10 ± 3.14, 16.00 | 0.097 |
| Missing (n) | 1 | 0 | |
| Total CSHQ score (mean, sd, median) | 52.87 ± 7.71, 53.00 | 51.32 ± 7.88, 51.00 | 0.458 |
| ISI (child-reported) | |||
| Total score (mean, sd, median) | 9.55 ± 5.01, 9.00 | 10.37 ± 4.90, 10.00 | 0.280 |
| Measure Instrument | Boys (n = 55) | Girls (n = 41) | p |
|---|---|---|---|
| SNAP IV (parent reported) | |||
| Inattention score, (mean, sd) | 16.87 ± 5.33 | 18.71 ± 4.51 * | 0.039 |
| Hyperactivity/impulsivity score (mean, sd) | 14.82 ± 5.67 | 15.39 ± 6.07 * | 0.318 |
| Inattention | |||
| (n without missing answers) | 53 | 40 | |
| (n with <3 missing answers) | 3 | 1 | |
| <13 | 13 | 4 | |
| 13–17 | 17 | 13 | |
| 18–22 | 17 | 13 | |
| 23–27 | 8 | 11 | |
| Missing (n) | 0 | 0 | |
| Hyperactivity/impulsivity | |||
| (n without missing answers) | 49 | 38 | |
| (n with <4 missing answers) | 7 | 3 | |
| <13 | 18 | 10 | |
| 13–17 | 18 | 15 | |
| 18–22 | 11 | 11 | |
| 23–27 | 8 | 5 | |
| Missing (n) | 0 | 0 | |
| Short STAI (child-reported) | |||
| Total score (mean, sd, median) | 10.64 ± 3.37, 11.00 | 11.44 ± 4.02, 10.00 ^ | 0.420 |
| Range | 6–19 | 6–19 |
| Self-Reported Questionnaires | Boys (n = 55) | Girls (n = 41) | p | |
|---|---|---|---|---|
| EQ-5D-Y (child-reported) | ||||
| Mobility | No problems with mobility | 56 (100%) | 39 (95%) ” | 0.180 |
| Some/a lot of problems with mobility | 0 (0%) | 2 (5%) | ||
| Looking after myself | No problems looking after myself | 35 (64%) | 30 (73%) * | 0.381 |
| Some/a lot of problems looking after myself | 20 (36%) | 11 (27%) | ||
| Doing usual activities | No problems doing usual activities | 37 (67%) | 31 (76%) * | 0.497 |
| Some/a lot of problems doing usual activities | 18 (33%) | 10 (24%) | ||
| Having pain or discomfort | No pain or discomfort | 44 (80%) | 26 (63%) * | 0.103 |
| Some/a lot of pain and discomfort | 11 (20%) | 15 (37%) | ||
| Feeling worried sad or unhappy | Not worried, sad, or unhappy | 30 (54%) | 20 (49%) * | 0.680 |
| A bit worried, sad, or unhappy | 25 (46%) | 21 (51%) | ||
| EQ-5D-Y, VAS (child-reported) (mean, sd, median) | 82.42 ± 19.18, 86.00 | 80.39 ± 16.61, 80.00 | 0.417 | |
| CORS (child-reported) | ||||
| Total score, (mean, sd, median) | 32.59 ± 6.36, 34.00 | 29.29 ± 5.94, 29.40 ^ | 0.006 | |
| ≥28 (n) | 46 | 24 | ||
| <28 (n) | 9 | 17 | ||
| Well-being (mean, sd median) | 8.54 ± 2.04, 9.90 | 7.41 ± 1.91, 7.80 ^ | 0.001 | |
| Family (mean, sd, median) | 8.32 ± 1.95, 9.00 | 8.54 ± 1.79, 9.10 ^ | 0.649 | |
| School (mean, sd, median) | 7.39 ± 2.63, 8.00 | 5.94 ± 2.52, 6.00 ^ | 0.004 | |
| Life overall (mean, sd, median) | 8.34 ± 2.09, 9.10 | 7.39 ± 2.37, 8.10 ^ | 0.017 | |
| Questionnaires | Not Worried, Sad, or Unhappy (n = 50) | Worried, Sad, or Unhappy (n = 46) | p |
|---|---|---|---|
| CSHQ | |||
| Total sum (mean, sd, median) | 50.64 ± 7.66, 50.50 | 53.91 ± 7.63, 55.00 | 0.027 |
| Missing (n) | 2 | 1 | |
| ISI | |||
| Total score (mean, sd, median) | 8.14 ± 4.78, 7.00 | 11.80± 4.44, 10.50 | <0.001 |
| Short STAI | |||
| Total score (mean, sd, median) | 9.78 ± 3.48, 9.00 | 12.28 ± 3.43, 12.00 | <0.001 |
| Range | 6–19 | 6–19 | |
| CORS | |||
| Total score, (mean, sd, median) | 34.13 ± 5.12, 35.25 | 27.98 ± 6.07, 28.60 | <0.001 |
| ≥28 (n) | 45 | 25 | |
| <28 (n) | 5 | 21 | |
| Well-being (mean, sd median) | 8.92 ± 1.43, 9.80 | 7.12 ± 2.23, 7.40 | 0.013 |
| Family (mean, sd, median) | 8.90 ± 21.60, 9.80 | 7.89 ± 2.03, 8.55 | 0.030 |
| School (mean, sd, median) | 7.32± 2.48, 7.75 | 6.17 ± 2.76, 6.00 | <0.001 |
| Life overall (mean, sd, median) | 8.99 ± 1.34, 9.85 | 6.79 ± 2.49, 7.25 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lindholm, A.; Jarbin, H.; Aili, K.; Nygren, J.M.; Svedberg, P.; Larsson, I. Sex Differences in Children with Uncomplicated Attention Deficit/Hyperactivity Disorder and Sleep Problems. Children 2024, 11, 636. https://doi.org/10.3390/children11060636
Lindholm A, Jarbin H, Aili K, Nygren JM, Svedberg P, Larsson I. Sex Differences in Children with Uncomplicated Attention Deficit/Hyperactivity Disorder and Sleep Problems. Children. 2024; 11(6):636. https://doi.org/10.3390/children11060636
Chicago/Turabian StyleLindholm, Annelie, Håkan Jarbin, Katarina Aili, Jens M. Nygren, Petra Svedberg, and Ingrid Larsson. 2024. "Sex Differences in Children with Uncomplicated Attention Deficit/Hyperactivity Disorder and Sleep Problems" Children 11, no. 6: 636. https://doi.org/10.3390/children11060636
APA StyleLindholm, A., Jarbin, H., Aili, K., Nygren, J. M., Svedberg, P., & Larsson, I. (2024). Sex Differences in Children with Uncomplicated Attention Deficit/Hyperactivity Disorder and Sleep Problems. Children, 11(6), 636. https://doi.org/10.3390/children11060636





