Trauma Outcomes in Pediatric Nonfatal Road Traffic Accidents
Abstract
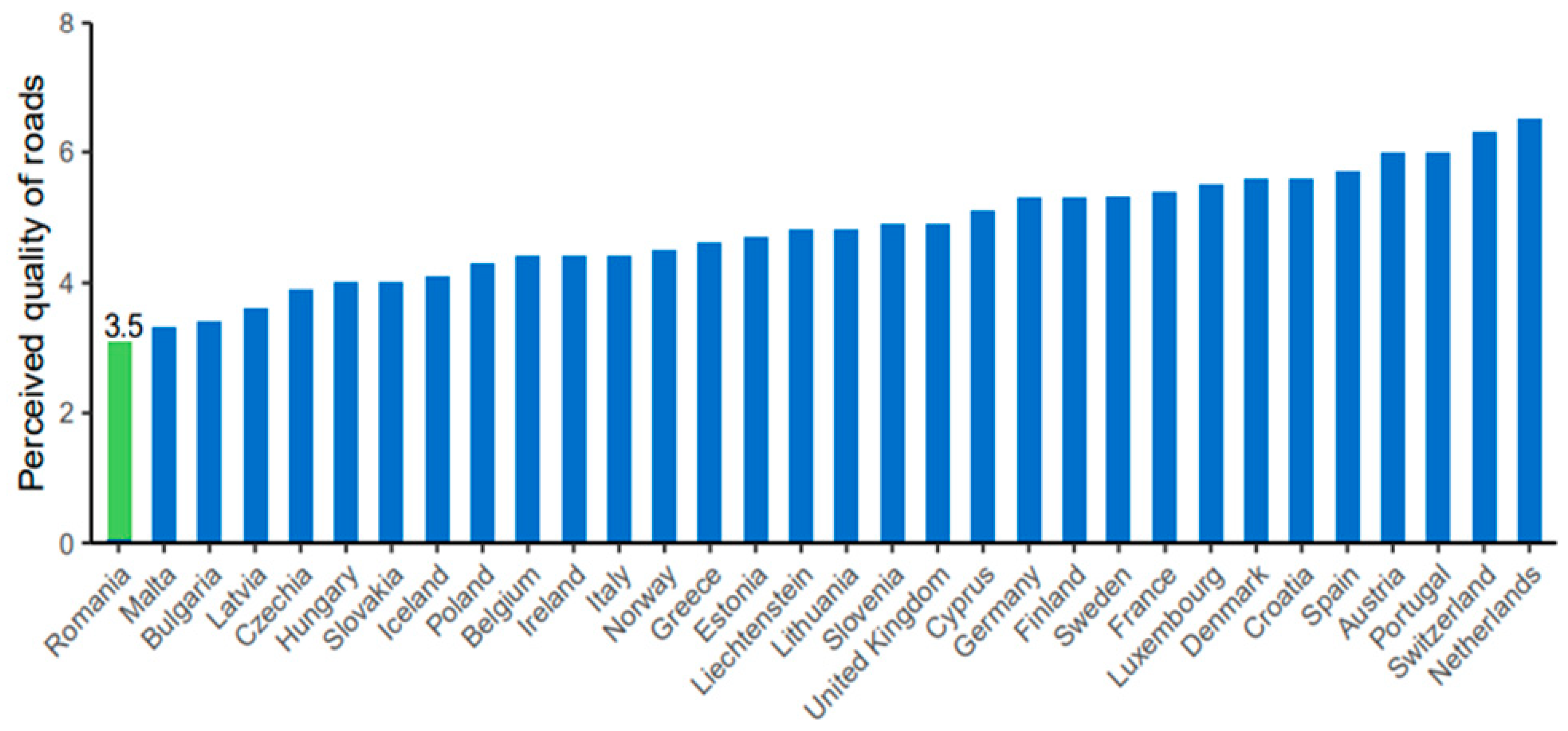
1. Introduction
2. Materials and Methods
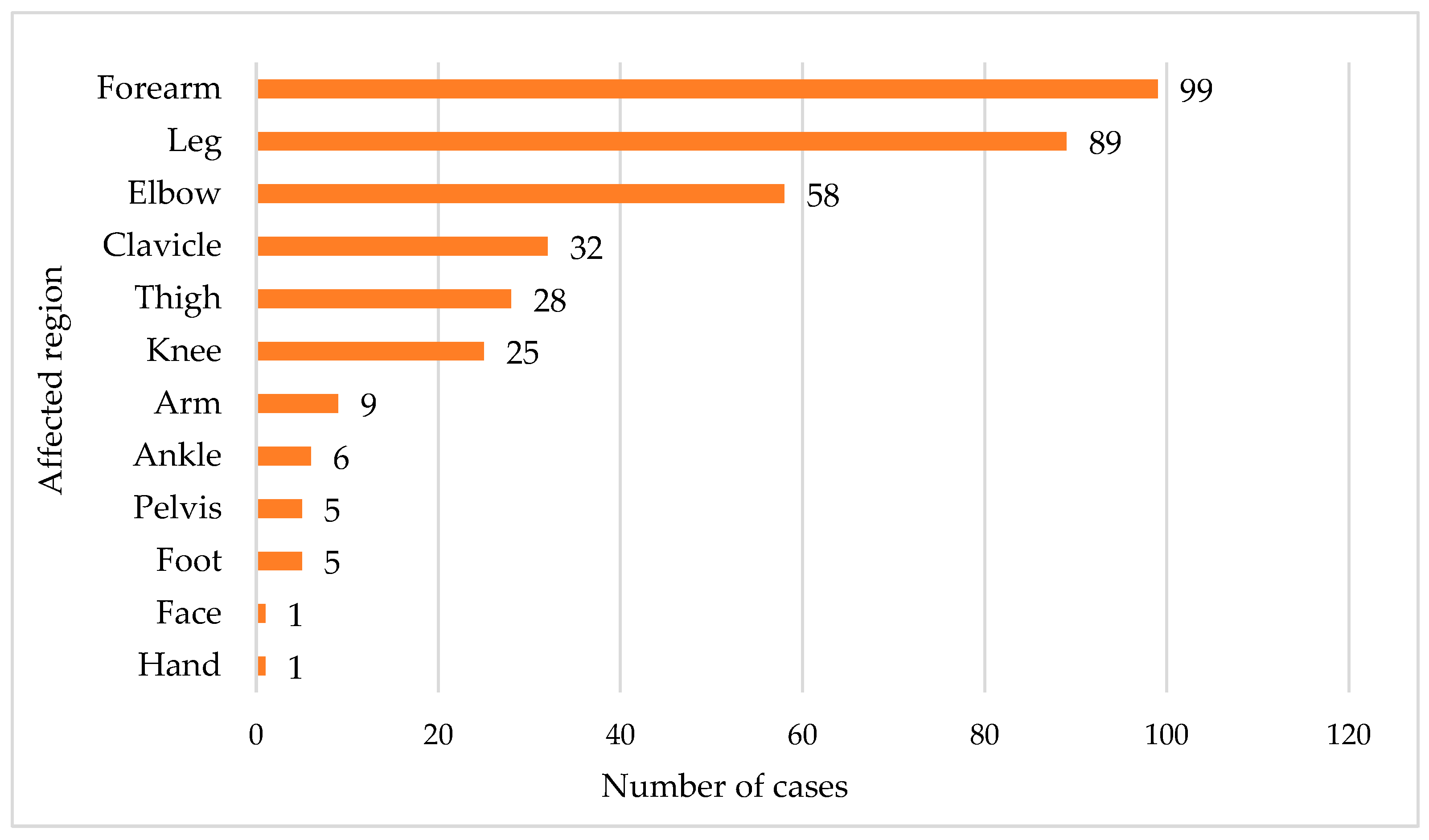
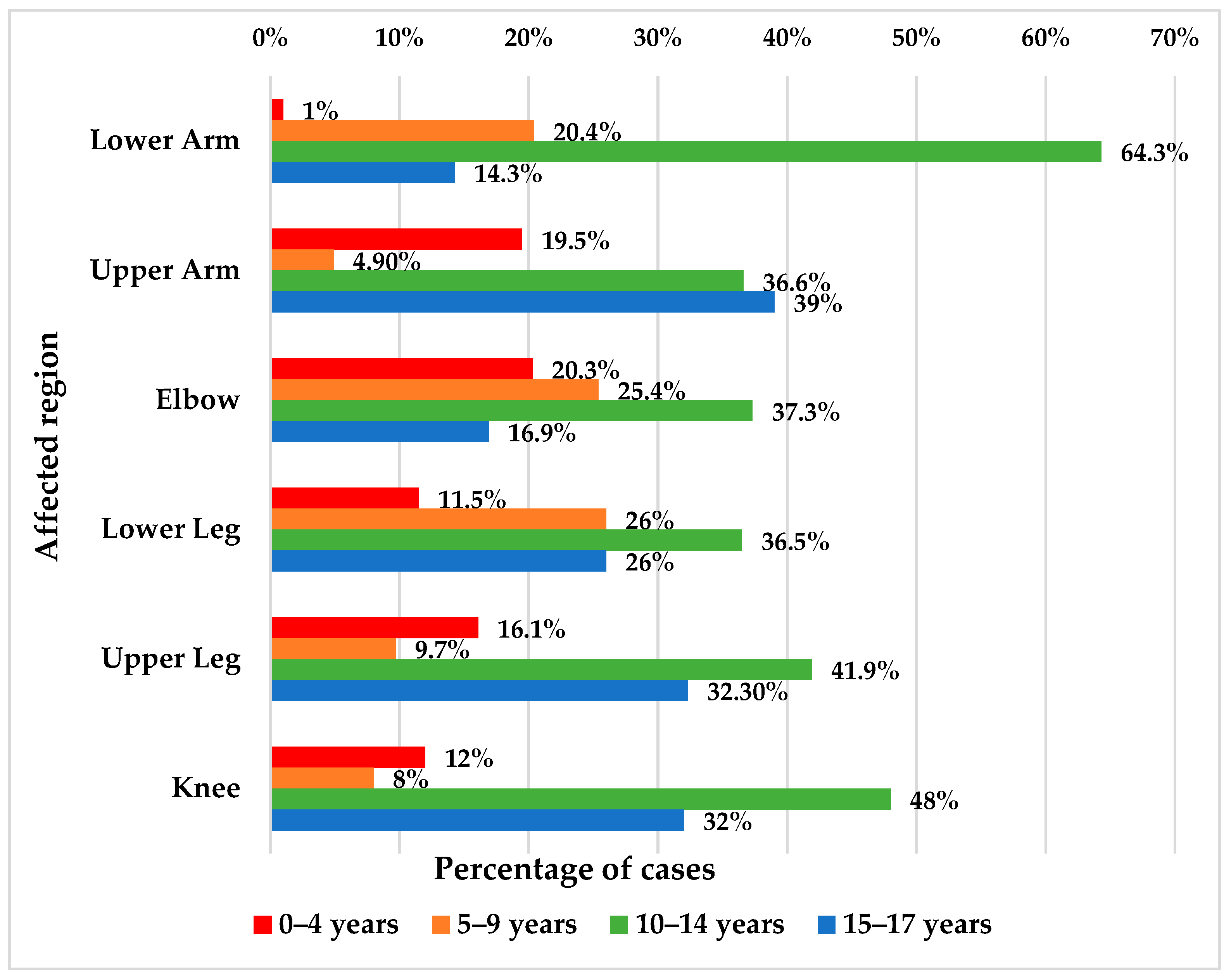
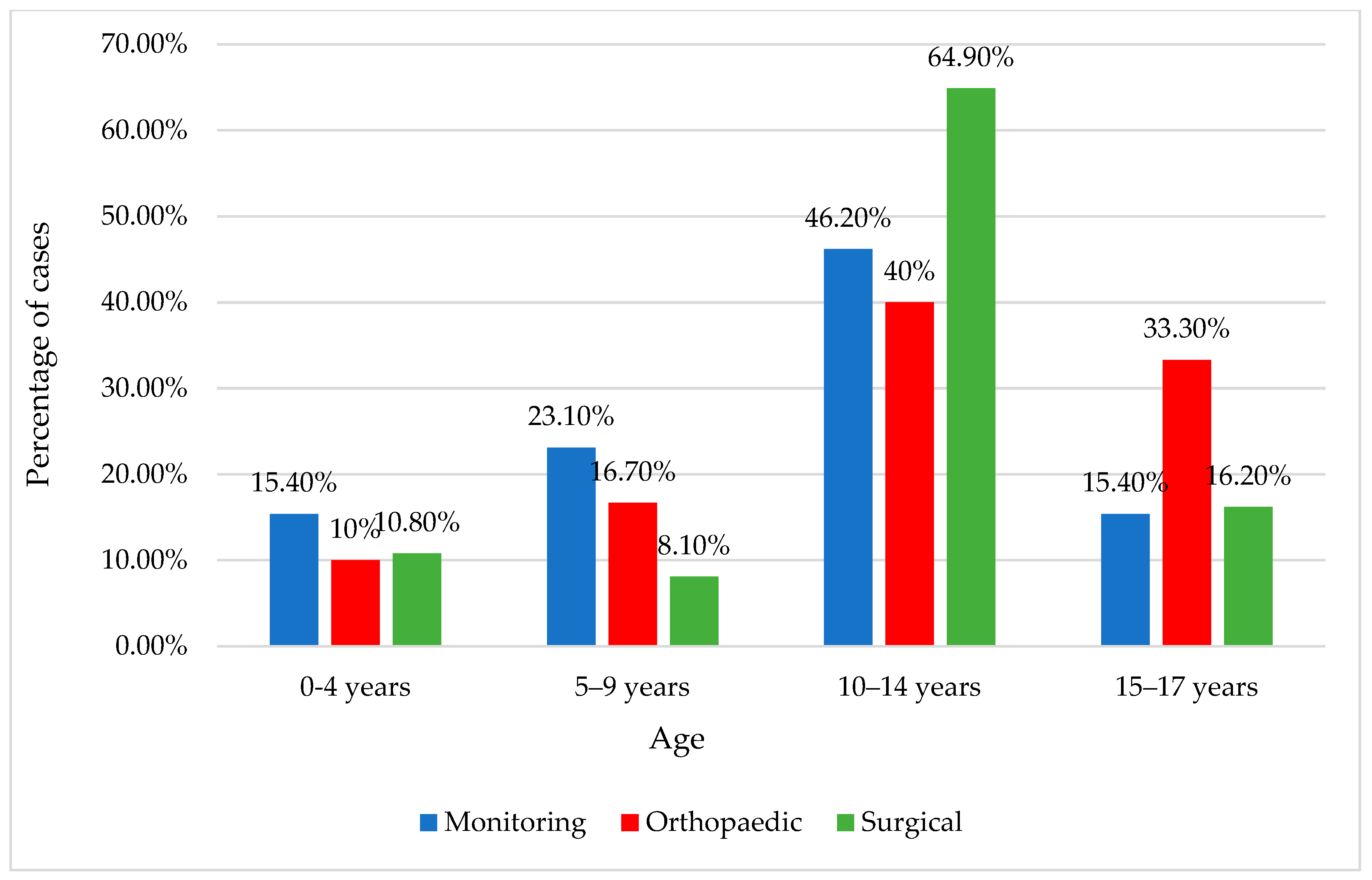
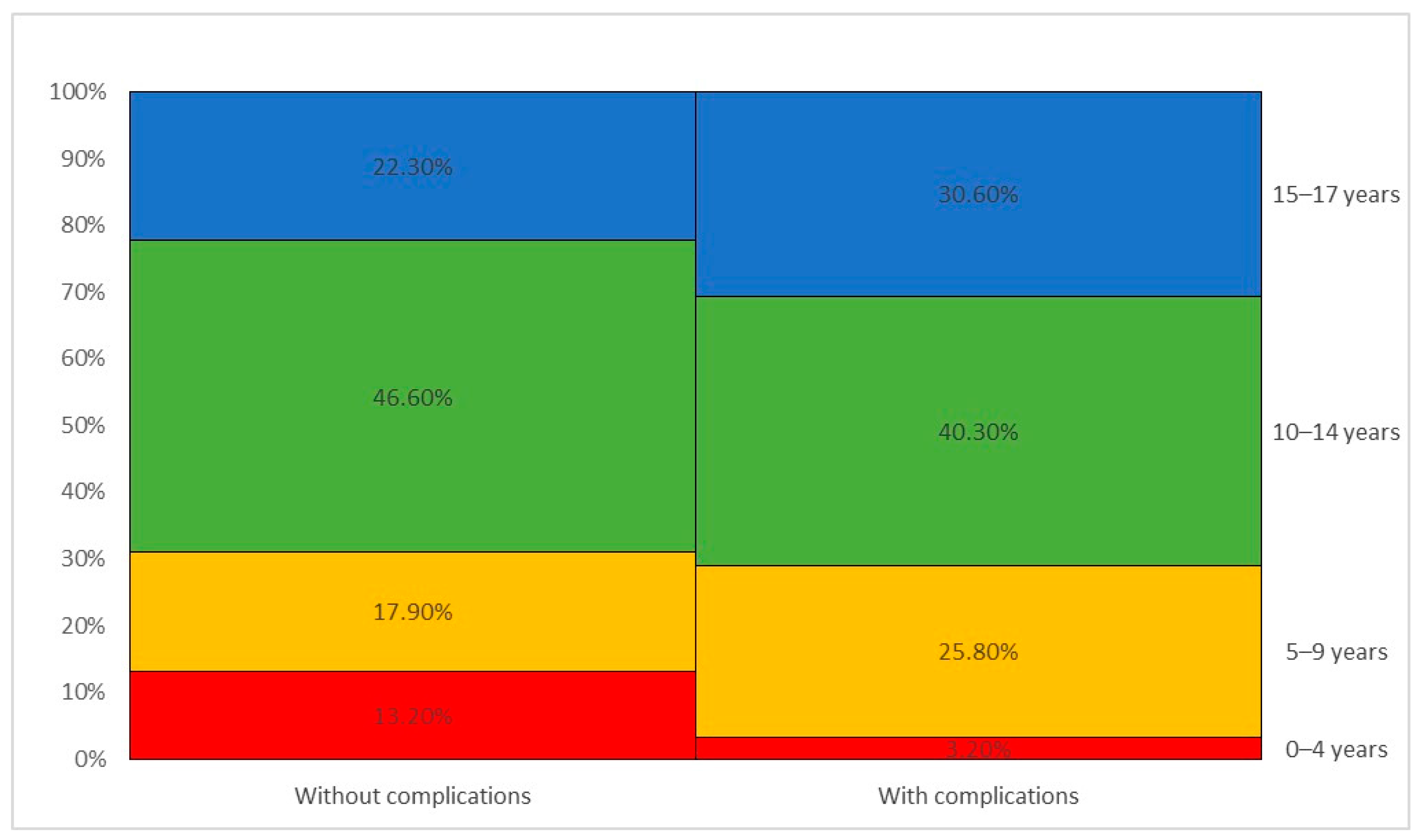
3. Results
4. Discussion
5. Limitations of This Study and Further Studies
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Söderlund, N.; Zwi, A.B. Traffic-related mortality in industrialized and less developed countries. Bull. World Health Organ. 1995, 73, 175–182. [Google Scholar] [PubMed]
- Bakhtiyari, M.; Delpisheh, A.; Monfared, A.B.; Kazemi-Galougahi, M.H.; Mehmandar, M.R.; Riahi, M.; Salehi, M.; Mansournia, M.A. The road traffic crashes as a neglected public health concern; an observational study from Iranian population. Traffic Inj. Prev. 2014, 16, 36–41. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Status Report on Road Safety 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- WHO. The Global Burden of Disease; Projected Change in the Ranking of the 15 Leading Causes of Death and Disease (DALYs) Worldwide, 1990–2020; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Version 2.0. Available online: https://road-safety.transport.ec.europa.eu/system/files/2023-02/erso-country-overview-2023-sweden_0.pdf (accessed on 21 February 2023).
- Kumar, N.; Kumar, M. Medicolegal study of fatal road traffic accidents in Varanasi region. Int. J. Sci. Res. IJSR 2015, 4, 1492–1496. [Google Scholar]
- Doud, A.N.; Schoell, S.L.; Weaver, A.A.; Talton, J.W.; Barnard, R.T.; Petty, J.K.; Stitzel, J.D. Disability risk in pediatric motor vehicle crash occupants. J. Trauma Acute Care Surg. 2017, 82, 933–938. [Google Scholar] [CrossRef]
- Gaffley, M.; Weaver, A.A.; Talton, J.W.; Barnard, R.T.; Stitzel, J.D.; Zonfrillo, M.R. Age-based differences in the disability of extremity injuries in pediatric and adult occupants. Traffic Inj. Prev. 2019, 20, S63–S68. [Google Scholar] [CrossRef]
- Schoell, S.L.; Weaver, A.A.; Talton, J.W.; Baker, G.; Doud, A.N.; Barnard, R.T.; Stitzel, J.D.; Zonfrillo, M.R. Functional outcomes of motor vehicle crash head injuries in pediatric and adult occupants. Traffic Inj. Prev. 2016, 17, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Zonfrillo, M.R.; Durbin, D.R.; Winston, F.K.; Zhao, H.; Stineman, M.G. Physical disability after injury-related inpatient rehabilitation in children. Pediatrics 2013, 131, e206–e213. [Google Scholar] [CrossRef]
- Janssens, L.; Gorter, J.W.; Ketelaar, M.; Kramer, W.L.; Holtslag, H.R. Long-term health condition in major pediatric trauma: A pilot study. J. Pediatr. Surg. 2009, 44, 1591–1600. [Google Scholar] [CrossRef]
- Twisk, D.A.M.; Bos, N.M.; Weijermars, W.A.M. Road injuries, health burden, but not fatalities make 12-to-17-year-olds a high-risk group in the Netherlands. Eur. J. Public Health 2017, 27, 981–984. [Google Scholar] [CrossRef]
- Romanian Police National Statistics Center 2019. Available online: https://www.politiaromana.ro/ro/structura-politiei-romane/unitati-centrale/directia-rutiera/statistici (accessed on 11 February 2024).
- Batailler, P.; Hours, M.; Maza, M.; Charnay, P.; Tardy, H.; Tournier, C.; Javouhey, E. Health status recovery at one year in children injured in a road accident: A cohort study. Accid. Anal. Prev. 2014, 71, 267–272. [Google Scholar] [CrossRef]
- Lystad, R.P.; Bierbaum, M.; Curtis, K.; Braithwaite, J.; Mitchell, R. Unwarranted clinical variation in the care of children and young people hospitalised for injury: A population-based cohort study. Injury 2018, 49, 1781–1786. [Google Scholar] [CrossRef]
- Olofsson, E.; Bunketorp, O.; Andersson, A.L. Children at risk of residual physical problems after public road traffic injuries—A 1-year follow-up study. Injury 2012, 43, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Doong, J.L.; Lai, C.H. Risk factors for child and adolescent occupants, bicyclists, and pedestrians in motorized vehicle collisions. Traffic Inj. Prev. 2012, 13, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Eilert-Petersson, E.; Schelp, L. An epidemiological study of non-fatal pedestrian injuries. Saf. Sci. 1998, 29, 125–141. [Google Scholar] [CrossRef]
- Mitchell, R.J.; Bambach, M.R.; Foster, K.; Curtis, K. Risk factors associated with the severity of injury outcome for pediatric road trauma. Injury. 2015, 46, 874–882. [Google Scholar] [CrossRef] [PubMed]
- Cunha-Diniz, F.; Taveira-Gomes, T.; Teixeira, J.M.; Magalhães, T. Trauma outcomes in nonfatal road traffic accidents: A Portuguese medico-legal approach. Forensic Sci. Res. 2022, 7, 528–539. [Google Scholar] [CrossRef] [PubMed]
- Borobia, C.; Alías, P.; Pascual, G. Avaliação do dano corporal em crianças e idosos [The assessment of bodily harm in children and elderly]. In Aspectos Práticos da Avaliação do Dano Corporal em Direito Civil [Practical Aspects of Personal Injury Assessment in Civil Law]; Vieira, D.N., Quintero, J.M.A., Eds.; Imprensa da Universidade de Coimbra: Coimbra, Portugal, 2008; pp. 131–146, (In Portuguese). [Google Scholar] [CrossRef]
- Grivna, M.; Eid, H.O.; Abu-Zidan, F.M. Pediatric and Youth Traffic-Collision Injuries in Al Ain, United Arab Emirates: A Prospective Study. PLoS ONE 2013, 8, e68636. [Google Scholar] [CrossRef]
- Tenenbaum, S.; Bariteau, J.T.; Chechik, O.; Givon, A.; Peleg, K.; Thein, R.; Israeli Trauma Group. Lower Extremity Fractures in Hospitalized Pediatric Patients Following Road Traffic Accidents. Pediatr. Emerg. Care 2018, 35, 862–867. [Google Scholar] [CrossRef]
- Weijermars, W.; Bos, N.; Filtness, A.; Brown, L.; Bauer, R.; Dupont, E.; Martin, J.L.; Perez, K.; Thomas, P. Burden of injury of serious road injuries in six EU countries. Accid. Anal. Prev. 2018, 111, 184–192. [Google Scholar] [CrossRef]
- Tournier, C.; Charnay, P.; Tardy, H.; Chossegros, L.; Carnis, L.; Hours, M. A few seconds to have an accident, a long time to recover: Consequences for road accident victims from the ESPARR cohort 2 years after the accident. Accid. Anal. Prev. 2014, 72, 422–432. [Google Scholar] [CrossRef]
- Magalhães, T.; Hamonet, C. Handicap assessment: Setting the grounds for an effective intervention in the community. Med. Law 2001, 20, 153–166. [Google Scholar] [PubMed]
- Elrud, R.; Friberg, E.; Alexanderson, K.; Stigson, H. Sickness absence, disability pension and permanent medical impairment among 64 000 injured car occupants of working ages: A two-year prospective cohort study. Accid. Anal. Prev. 2019, 127, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Monarrez-Espino, J.; Laflamme, L.; Berg, H.Y. Measuring and assessing risk of quality of life loss following a road traffic injury: A proposed methodology for use of a composite score. Accid. Anal. Prev. 2018, 115, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Polinder, S.; Haagsma, J.; Bos, N.; Panneman, M.; Wolt, K.K.; Brugmans, M.; Weijermars, W.; van Beeck, E. Burden of road traffic injuries: Disability-adjusted life years in relation to hospitalization and the maximum abbreviated injury scale. Accid. Anal. Prev. 2015, 80, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Carter, P.M.; Flannagan, C.A.C.; Reed, M.P.; Cunningham, R.M.; Rupp, J.D. Comparing the effects of age, BMI and gender on severe injury (AIS 3+) in motor-vehicle crashes. Accid. Anal. Prev. 2014, 72, 146–160. [Google Scholar] [CrossRef] [PubMed]
- Gray, S.E.; Hassani-Mahmooei, B.; Kendall, E.; Cameron, I.D.; Kenardy, J.; Collie, A. Factors associated with graduated return to work following injury in a road traffic crash. J. Transp. Health 2018, 10, 167–177. [Google Scholar] [CrossRef]
- Hours, M.; Chossegros, L.; Charnay, P.; Tardy, H.; Nhac-Vu, H.-T.; Boisson, D.; Luauté, J.; Laumon, B. Outcomes one year after a road accident: Results from the ESPARR cohort. Accid. Anal. Prev. 2013, 50, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, M.; Stigson, H.; Krafft, M.; Kullgren, A. Risk of permanent medical impairment (RPMI) in car crashes correlated to age and gender. Traffic Inj. Prev. 2015, 16, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Read, K.M.; Kufera, J.A.; Dischinger, P.C.; Kerns, T.J.; Ho, S.M.; Burgess, A.R.; Burch, C.A. Life-altering outcomes after lower extremity injury sustained in motor vehicle crashes. J. Trauma 2004, 57, 815–823. [Google Scholar] [CrossRef] [PubMed]
- Paffrath, T.; Lefering, R.; Flohé, S. How to define severely injured patients?—An Injury Severity Score (ISS) based approach alone is not sufficient. Injury 2014, 45, S64–S69. [Google Scholar] [CrossRef]
- Palmer, C.S.; Gabbe, B.J.; Cameron, P.A. Defining major trauma using the 2008 Abbreviated Injury Scale. Injury 2016, 47, 109–115. [Google Scholar] [CrossRef]
- Christoffersen, T.; Emaus, N.; Dennison, E.; Furberg, A.-S.; Gracia-Marco, L.; Grimnes, G.; Nilsen, O.A.; Vlachopoulos, D.; Winther, A.; Ahmed, L.A. The association between childhood fractures and adolescence bone outcomes: A population-based study, the Tromsø Study, Fit Futures. Osteoporos. Int. 2018, 29, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Holton, C.S.; Kelley, S.P. The response of children to trauma. Orthop. Trauma 2015, 29, 337–349. [Google Scholar] [CrossRef]
- Bohman, K.; Stigson, H.; Krafft, M. Long-term medical consequences for child occupants 0 to 12 years injured in car crashes. Traffic Inj. Prev. 2014, 15, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, C.; Coelho, J.; Pedrosa, D.; Caetano, C.; Corte-Real, F.; Vieira, D.N.; Corte-Real, A. Dental evaluation specificity in orofacial damage assessment: A serial case study. J. Forensic Leg. Med. 2019, 68, 101861. [Google Scholar] [CrossRef] [PubMed]
- Wright, T. Too scared to learn: Teaching young children who have experienced trauma. Young Child. 2014, 69, 88. [Google Scholar]
- de Haan, A.; Tutus, D.; Goldbeck, L.; Rosner, R.; Landolt, M.A. Do dysfunctional posttraumatic cognitions play a mediating role in trauma adjustment? Findings from interpersonal and accidental trauma samples of children and adolescents. Eur. J. Psychotraumatol. 2019, 10, 1596508. [Google Scholar] [CrossRef] [PubMed]
- Crandall, J.R.; Myers, B.S.; Meaney, D.F.; Zellers Schmidtke, S. Pediatric Injury Biomechanics; Crandall, J.R., Myers, B.S., Meaney, D.F., Zellers Schmidtke, S., Eds.; Springer: New York, NY, USA, 2013; ISBN 978-1-4614-4153-3. [Google Scholar]
- Wilhelm, J.; Ptak, M.; Fernandes, F.A.O.; Kubicki, K.; Kwiatkowski, A.; Ratajczak, M.; Sawicki, M.; Szarek, D. Injury Biomechanics of a Child’s Head: Problems, Challenges and Possibilities with a New aHEAD Finite Element Model. Appl. Sci. 2020, 10, 4467. [Google Scholar] [CrossRef]
- Traffic Code Emergency Ordinance no. 195/2002 Regarding Traffic on Public Roads. Available online: https://www.legislatierutiera.ro/legislatie-rutiera/codul-rutier/ (accessed on 11 February 2024).
- Ptak, M.; Wilhelm, J.; Sawicki, M.; Dymek, M.; Fernandes, F.A.O.; Kristen, H.; Garatea, E. Assessment of Child Safety on Bicycles in Baby Carriers: The Importance of Evaluating Both Head and Neck Injuries. J. Saf. Res. 2023, 85, 254–265. [Google Scholar] [CrossRef]
- Bachani, A.M.; Branchini, C.; Ear, C.; Roehler, D.R.; Parker, E.M.; Tum, S.; Ballesteros, M.F.; Hydera, A.A. Trends in prevalence, knowledge, attitudes, and practices of helmet use in Cambodia: Results from a two-year study. Injury 2013, 44 (Suppl. S4), S31–S37. [Google Scholar] [CrossRef]
- Bachani, A.M.; Hung, Y.W.; Mogere, S.; Akunga, D.; Nyamari, J.; Hyder, A.A. Helmet wearing in Kenya: Prevalence, knowledge, attitude, practice and implications. Public Health 2017, 144, S23–S31. [Google Scholar] [CrossRef] [PubMed]
- Du, R.Y.; LoPresti, M.A.; García, R.M.; Lam, S. Primary prevention of road traffic accident-related traumatic brain injuries in younger populations: A systematic review of helmet legislation. J. Neurosurg. Pediatr. 2020, 25, 361–374. [Google Scholar] [CrossRef] [PubMed]
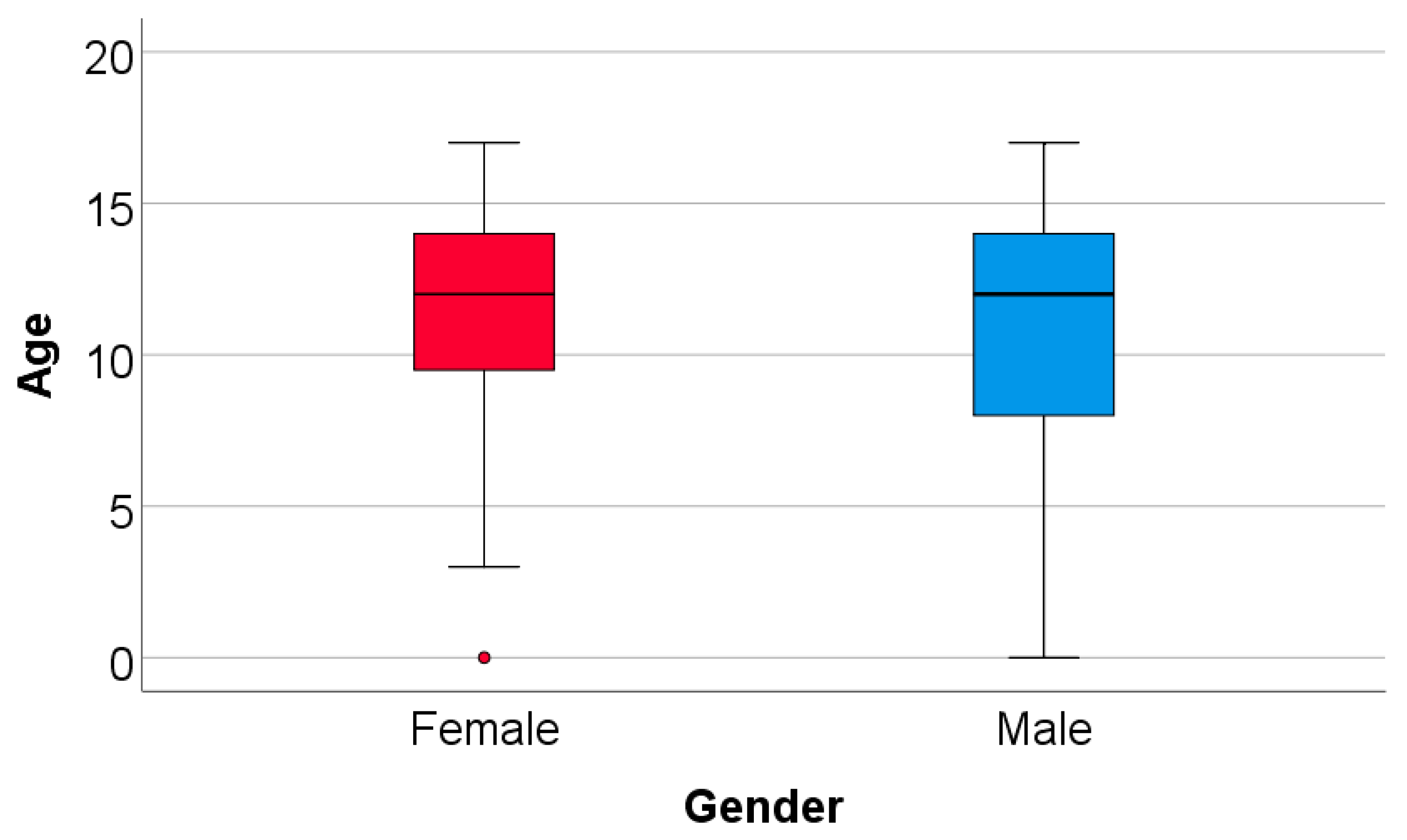



| Gender | Mean ± SD | Median (IQR) | Mean Rank | p * | |
|---|---|---|---|---|---|
| Female (p < 0.001 **) | 11.48 ± 4.08 | 12 (9.25–14) | 185.23 | 0.573 | |
| Male (p < 0.001 **) | 11.03 ± 4.45 | 12 (8–14) | 177.85 | ||
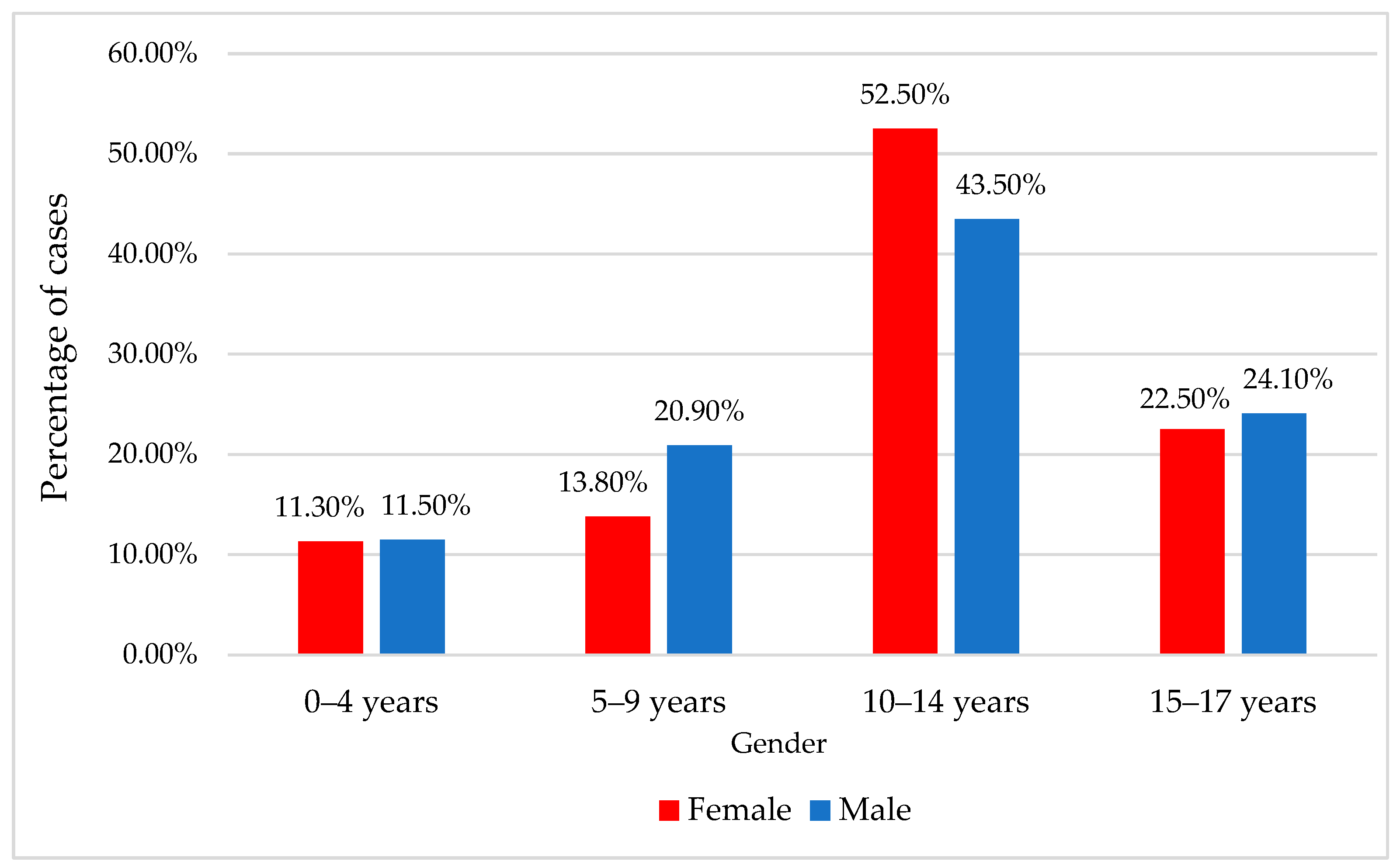
| Gender/Age | Female | Male | p *** | ||
| Nr. | % | Nr. | % | ||
| 0–4 years | 9 | 11.3% | 32 | 11.5% | 0.435 |
| 5–9 years | 11 | 13.8% | 58 | 20.9% | |
| 10–14 years | 42 | 52.5% | 121 | 43.5% | |
| 15–17 years | 18 | 22.5% | 67 | 24.1% | |
| Age/Personal Pathological History (Female) | Absent | Present | p * | ||||
|---|---|---|---|---|---|---|---|
| Nr. (%) | Nr. (%) | ||||||
| 0–4 years | 8 (12.3%) | 1 (6.7%) | 0.416 | ||||
| 5–9 years | 7 (10.8%) | 4 (26.7%) | |||||
| 10–14 years | 34 (52.3%) | 8 (53.3%) | |||||
| 15–17 years | 16 (24.6%) | 2 (13.3%) | |||||
| Age/Type of History (Female) | Orthopedic | Neurologic | Hematologic | Cardiologic | Allergology | Other | p * |
| Nr. (%) | Nr. (%) | Nr. (%) | Nr. (%) | Nr. (%) | Nr. (%) | ||
| 0–4 years | 0 (0%) | 1 (33.3%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0.353 |
| 5–9 years | 1 (20%) | 1 (33.3%) | 0 (0%) | 0 (0%) | 2 (50%) | 0 (0%) | |
| 10–14 years | 4 (80%) | 0 (0%) | 1 (100%) | 1 (50%) | 2 (50%) | 0 (0%) | |
| 15–17 years | 0 (0%) | 1 (33.3%) | 0 (0%) | 1 (50%) | 0 (0%) | 0 (0%) | |
| Age/Personal Pathological History (Male) | Absent | Present | p * | ||||
|---|---|---|---|---|---|---|---|
| Nr. (%) | Nr. (%) | ||||||
| 0–4 years | 29 (12%) | 3 (8.1%) | 0.791 | ||||
| 5–9 years | 50 (20.7%) | 8 (21.6%) | |||||
| 10–14 years | 106 (44%) | 15 (40.5%) | |||||
| 15–17 years | 56 (23.2%) | 11 (29.7%) | |||||
| Age/Type of history (Male) | Orthopedic | Neurologic | Hematologic | Cardiologic | Allergology | Other | p * |
| Nr. (%) | Nr. (%) | Nr. (%) | Nr. (%) | Nr. (%) | Nr. (%) | ||
| 0–4 years | 0 (0%) | 1 (8.3%) | 2 (28.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0.482 |
| 5–9 years | 2 (28.6%) | 1 (8.3%) | 2 (28.6%) | 0 (0%) | 1 (25%) | 2 (66.7%) | |
| 10–14 years | 4 (57.1%) | 4 (33.3%) | 2 (28.6%) | 3 (75%) | 1 (25%) | 1 (33.3%) | |
| 15–17 years | 1 (14.3%) | 6 (50%) | 1 (14.3%) | 1 (25%) | 2 (50%) | 0 (0%) | |
| Accident Type/Age Group | OR (95% C.I.) | p | |
|---|---|---|---|
| Other type | 0–4 years | 0.364 (0.093–1.425) | 0.147 |
| 5–9 years | 0.340 (0.127–0.907) | 0.031 | |
| 10–14 years | 0.316 (0.141–0.709) | 0.005 | |
| 15–17 years | - | - | |
| Car passenger | 0–4 years | 8.5 (2.829–25.542) | <0.001 |
| 5–9 years | 1.943 (0.655–5.765) | 0.231 | |
| 10–14 years | 2.752 (1.054–7.186) | 0.039 | |
| 15–17 years | - | - | |
| Bicyclist | 0–4 years | 0.291 (0.076–1.124) | 0.073 |
| 5–9 years | 0.583 (0.263–1.291) | 0.183 | |
| 10–14 years | 0.894 (0.473–1.689) | 0.729 | |
| 15–17 years | - | - | |
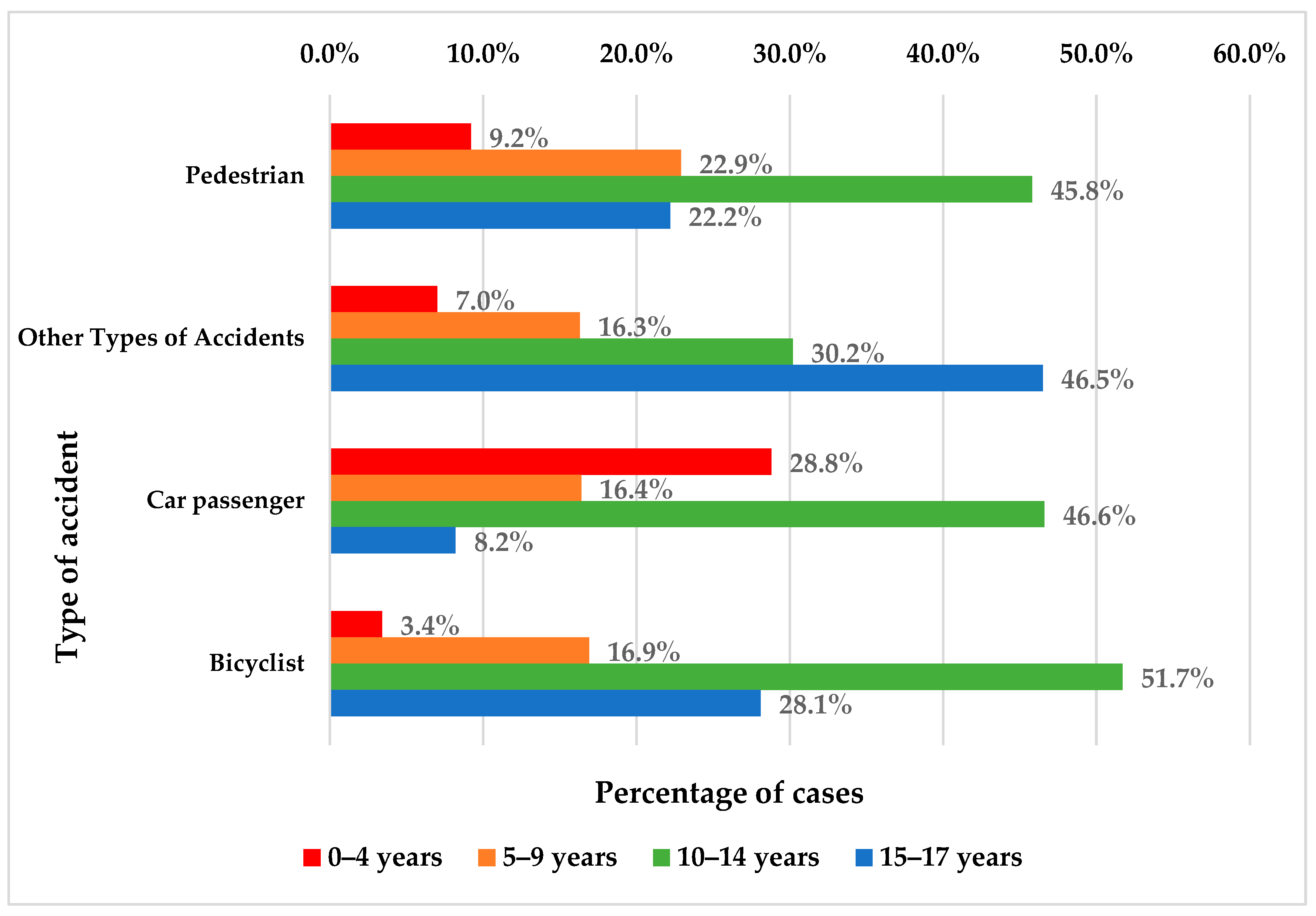
| Age/Type of Accident | Pedestrian | Other Types | Car Passenger | Bicyclist | p * | ||||
|---|---|---|---|---|---|---|---|---|---|
| Nr. | % | Nr. | % | Nr. | % | Nr. | % | ||
| 0–4 years | 14 | 9.2% | 3 | 7% | 21 | 28.8% | 3 | 3.4% | <0.001 |
| 5–9 years | 35 | 22.9% | 7 | 16.3% | 12 | 16.4% | 15 | 16.9% | |
| 10–14 years | 70 | 45.8% | 13 | 30.2% | 34 | 46.6% | 46 | 51.7% | |
| 15–17 years | 34 | 22.2% | 20 | 46.5% | 6 | 8.2% | 25 | 28.1% | |
| Gender/Type of Accident | Pedestrian | Other Types | Car Passenger | Bicyclist | p * | ||||
|---|---|---|---|---|---|---|---|---|---|
| Nr. | % | Nr. | % | Nr. | % | Nr. | % | ||
| Female | 44 | 28.8% | 6 | 14% | 13 | 17.8% | 17 | 19.1% | 0.090 |
| Male | 109 | 71.2% | 37 | 86% | 60 | 82.2% | 72 | 80.9% | |
| Complications | N | % |
|---|---|---|
| Without complications | 296 | 82.7 |
| Postoperative wound dehiscence | 10 | 2.8 |
| Wound infection | 10 | 2.8 |
| Genu valgum | 8 | 2.2 |
| Limping gait | 8 | 2.2 |
| Radial nerve palsy | 7 | 1.9 |
| Secondary sciatic nerve palsy | 4 | 1.1 |
| Acute posthemorrhagic anemia | 4 | 1.1 |
| Delayed union | 3 | 0.8 |
| Genu varum | 2 | 0.6 |
| Posttraumatic shortening 2.5 cm | 2 | 0.6 |
| Posttraumatic shortening 4.5 cm | 2 | 0.6 |
| Total | 358 | 100.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popa, Ș.; Bulgaru-Iliescu, D.; Ciongradi, C.I.; Surd, A.O.; Candussi, I.-L.; Popa, I.P.; Sârbu, I. Trauma Outcomes in Pediatric Nonfatal Road Traffic Accidents. Children 2024, 11, 425. https://doi.org/10.3390/children11040425
Popa Ș, Bulgaru-Iliescu D, Ciongradi CI, Surd AO, Candussi I-L, Popa IP, Sârbu I. Trauma Outcomes in Pediatric Nonfatal Road Traffic Accidents. Children. 2024; 11(4):425. https://doi.org/10.3390/children11040425
Chicago/Turabian StylePopa, Ștefan, Diana Bulgaru-Iliescu, Carmen Iulia Ciongradi, Adrian Onisim Surd, Iuliana-Laura Candussi, Irene Paula Popa, and Ioan Sârbu. 2024. "Trauma Outcomes in Pediatric Nonfatal Road Traffic Accidents" Children 11, no. 4: 425. https://doi.org/10.3390/children11040425
APA StylePopa, Ș., Bulgaru-Iliescu, D., Ciongradi, C. I., Surd, A. O., Candussi, I.-L., Popa, I. P., & Sârbu, I. (2024). Trauma Outcomes in Pediatric Nonfatal Road Traffic Accidents. Children, 11(4), 425. https://doi.org/10.3390/children11040425







