Parental Attitudes towards Child Oral Health and Their Structural Analysis
Abstract
1. Introduction
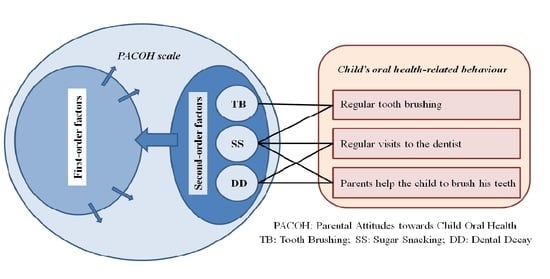
2. Materials and Methods
2.1. Setting
2.2. Study Design and Sample Size
2.3. Subjects
2.4. Questionnaire
2.5. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Analysis of the Original 38-Item Scale
3.3. Shortening the Scale
3.4. Multi-Group Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Likhar, A.; Baghel, P.; Patil, M. Early childhood development and social determinants. Cureus 2022, 14, e29500. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.M.; Shinn, C.; Fullilove, M.T.; Scrimshaw, S.C.; Fielding, J.E.; Normand, J.; Carande-Kulis, V.G.; Task Force on Community Preventive Services. The effectiveness of early childhood development programs. A systematic review. Am. J. Prev. Med. 2003, 24 (Suppl. S3), 32–46. [Google Scholar] [CrossRef] [PubMed]
- Petrauskienė, S.; Narbutaitė, J.; Petrauskienė, A.; Virtanen, J.I. Oral health behaviour, attitude towards, and knowledge of dental caries among mothers of 0- to 3-year-old children living in Kaunas, Lithuania. Clin. Exp. Dent. Res. 2020, 6, 215–224. [Google Scholar] [CrossRef]
- Dăguci, L.; Bătăiosu, M.; Andrei, O.C.; Scrieciu, M.; Margaritescu, C.; Dascălu, I.; Amarascu, M.; Daguci, C. Risk of dental caries for children aged 4 to 6 in Craiova. Curr. Health Sci. J. 2016, 42, 145–150. [Google Scholar] [CrossRef]
- Skrīvele, S.; Care, R.; Bērziņa, S.; Kneist, S.; de Moura-Sieber, V.; de Moura, R.; Borutta, A.; Maslak, E.; Tserekhava, T.; Shakovets, N.; et al. Caries and Its Risk Factors in Young Children in Five Different Countries. Stomatologija 2013, 15, 39–46. Available online: https://sbdmj.lsmuni.lt/132/132-01.pdf (accessed on 6 February 2024).
- Harris, R.V.; Nicoll, A.D.; Adair, P.M.; Pine, C.M. Risk factors for dental caries in young children: A systematic review of the literature. Community Dent. Health 2004, 21, 71–85. [Google Scholar] [PubMed]
- Butera, A.; Maiorani, C.; Morandini, A.; Simonini, M.; Morittu, S.; Trombini, J.; Scribante, A. Evaluation of children caries risk factors: A narrative review of nutritional aspects, oral hygiene habits, and bacterial alterations. Children 2022, 9, 262. [Google Scholar] [CrossRef]
- Lam, P.P.Y.; Chua, H.; Ekambaram, M.; Lo, E.C.M.; Yiu, C.K.Y. Risk predictors of early childhood caries increment—A systematic revirw and meta-analysis. J. Evid. Based Dent. Pract. 2022, 22, 101732. [Google Scholar] [CrossRef]
- Moynihan, P.J.; Kelly, S.A. Effect on caries of restricting sugars intake: Systematic review to inform WHO guidelines. J. Dent. Res. 2014, 93, 8–18. [Google Scholar] [CrossRef]
- Sheiham, A.; James, W.P. A reappraisal of the quantitative relationship between sugar intake and dental caries: The need for new criteria for developing goals for sugar intake. BMC Public Health 2014, 14, 863. [Google Scholar] [CrossRef]
- Chi, D.L.; Scott, J.M. Added sugar and dental caries in children: A scientific update and future steps. Dent. Clin. N. Am. 2019, 63, 17–33. [Google Scholar] [CrossRef]
- Skafida, V.; Chambers, S. Positive association between sugar consumption and dental decay prevalence independent of oral hygiene in pre-school children: A longitudinal prospective study. J. Public Health 2018, 40, e275–e283. [Google Scholar] [CrossRef]
- Action on Sugar/Sugar and Health/Sugars and Tooth Decay. Available online: https://www.actiononsugar.org/sugar-and-health/sugars-and-tooth-decay/ (accessed on 6 February 2024).
- Padung, N. First dental visit: Age reasons oral health status and dental treatment needs among children aged 1 month to 14 years. Int. J. Clin. Pediatr. Dent. 2022, 15, 394–397. [Google Scholar] [CrossRef]
- Breiner, H.; Ford, M.; Gadsden, V.L. (Eds.) Parenting Matters: Supporting Parents of Children Ages 0–8; Chapter 2. Parenting Knowledge, Attitudes, and Practices; National Academies Press: Washington, DC, USA, 2016. Available online: https://www.ncbi.nlm.nih.gov/books/NBK402020/ (accessed on 6 February 2024).
- Castilho, A.R.; Mialhe, F.L.; Barbosa, T.d.S.; Puppin-Rontani, R.M. Influence of family environment on children’s oral health: A systematic review. J. Pediatr. 2013, 89, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.R.; Brega, A.G.; Thomas, J.F.; Henderson, W.G.; Lind, K.E.; Braun, P.A.; Batliner, T.S.; Albino, J. Validity of measures assessing oral health beliefs of American Indian parents. J. Racial Ethn. Health Disparities 2018, 5, 1254–1263. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, J.I.; Vehkalahti, K.I.; Vehkalahti, M.M. Oral health behaviors and bacterial transmission from mother to child: An explorative study. BMC Oral Health 2015, 15, 75. [Google Scholar] [CrossRef] [PubMed]
- Hooley, M.; Skouteris, H.; Boganin, C.; Satur, J.; Kilpatrick, N. Parental influence and the development of dental caries in children aged 0–6 years: A systematic review of the literature. J. Dent. 2012, 40, 873–885. [Google Scholar] [CrossRef] [PubMed]
- Vanagas, G.; Milasauskiene, Z.; Grabauskas, V.; Mickeviciene, A. Associations between parental skills and their attitudes toward importance to develop good oral hygiene skills in their children. Medicina 2009, 45, 718–723. [Google Scholar] [CrossRef] [PubMed]
- Adair, P.M.; Pine, C.M.; Burnside, G.; Nicoll, A.D.; Gillett, A.; Anwar, S.; Broukal, Z.; Chestnutt, I.G.; Declerck, D.; Ping, F.X.; et al. Familial and cultural perceptions and beliefs of oral hygiene and dietary practices among ethnically and socio-economically diverse groups. Community Dent. Health 2004, 21 (Suppl. S1), 102–111. [Google Scholar] [PubMed]
- Ríos-León, R.D.P.; Salas-Huallparimache, J.M.; Díaz-Pizán, M.E.; Blanco-Victorio, D.J. Validity and reliability of questionnaires measuring attitudes to oral health: A review of the literature. J. Clin. Exp. Dent. 2022, 14, e776–e781. [Google Scholar] [CrossRef]
- Momeni, Z.; Sargeran, K.; Yazdani, R.; Shahbazi Sighaldeh, S. Psychometric properties of a new questionnaire assessing the mothers’ knowledge and perception about the oral health of their school children. Front. Dent. 2022, 19, 11. [Google Scholar] [CrossRef] [PubMed]
- Pine, C.M.; Adair, P.M.; Petersen, P.E.; Douglass, C.; Burnside, G.; Nicoll, A.D.; Gillett, A.; Anderson, R.; Beighton, D.; Jin-You, B.; et al. Developing explanatory models of health inequalities in childhood dental caries. Community Dent. Health 2004, 21 (Suppl. S1), 86–95. [Google Scholar] [PubMed]
- Aizen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the Health Belief Model. Health Educ. Q 1988, 15, 175–183. [Google Scholar] [CrossRef]
- Wallston, K.; Wallston, B.S.; DeVellis, R. Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health Educ. Monogr. 1978, 6, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.R.; Brega, A.G.; Campagna, E.J.; Braun, P.A.; Henderson, W.G.; Bryant, L.L.; Batliner, T.S.; Quissell, D.O.; Albino, J. Validation and impact of caregivers’ oral health knowledge and behavior on children’s oral health status. Pediatr. Dent. 2016, 38, 47–54. [Google Scholar]
- Clarke, R. Parental Attitudes, Beliefs and Behaviors about Caries Prevention among Black Preschool Children. Ph.D. Thesis, Florida International University, Miami, FL, USA, 2017. Available online: https://digitalcommons.fiu.edu/cgi/viewcontent.cgi?article=4158&context=etd (accessed on 6 February 2024).
- Skeie, M.S.; Klock, K.S.; Haugejorden, O.; Riordan, P.J.; Espelid, I. Tracking of parents’ attitudes to their children’s oral health-related behavior—Oslo, Norway, 2002–2004. Acta Odontol. Scand. 2010, 68, 49–56. [Google Scholar] [CrossRef]
- Mustafa, M.; Nasir, E.F.; Åstrøm, A.N. Attitudes toward brushing children’s teeth—A study among parents with immigrant status in Norway. Int. J. Paediatr. Dent. 2021, 31, 80–88. [Google Scholar] [CrossRef]
- Soltani, R.; Sharifirad, G.; Mahaki, B.; Eslami, A.A. Determinants of oral health behavior among preschool children: Application of the Theory of Planned Behavior. J. Dent. 2018, 19, 273–279. [Google Scholar]
- Razmienė, J. The State of Oral Hygiene of Children Aged 4–6 Years Attending Lithuanian Preschool Institutions, the Vulnerability of Teeth to Caries, Its Relationship with the Socioeconomic Status of the Family. Ph.D. Thesis, Lithuanian University of Health Sciences, Kaunas, Lithuania, 2013. Available online: https://portalcris.lsmuni.lt/server/api/core/bitstreams/2d097f6d-86fe-4e73-8613-b72886809db2/content (accessed on 6 February 2024). (In Lithuanian).
- Lithuanian Department of Statistics. Number of Permanent Residents. 2023. Available online: https://osp.stat.gov.lt/statistiniu-rodikliu-analize?indicator=S3R166#/ (accessed on 6 February 2024).
- Lithuanian Department of Statistics. Lithuania’s Children. 2023. Available online: https://osp.stat.gov.lt/statistiniu-rodikliu-analize?hash=ae6bf3b2-6d06-4221-bde0-5433232880d7#/ (accessed on 6 February 2024).
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed.; Harper & Row: New York, NY, USA, 2012; Volume 2, pp. 17–22. [Google Scholar]
- Morgado, F.F.R.; Meireles, J.F.F.; Neves, C.M.; Amaral, A.C.S.; Ferreira, M.E.C. Scale development: Ten main limitations and recommendations to improve future research practices. Psicol. Reflexão Crítica 2017, 30, 3. [Google Scholar] [CrossRef]
- Arbuckle, J.L. IBM SPSS AMOS 21 User’s Guide; AMOS Development Corporation: New York, NY, USA, 2012. [Google Scholar]
- Chen, F.F.; West, S.G.; Sousa, K.H. A comparison of bifactor and second-order models of quality of life. Multivar. Behav. Res. 2006, 41, 189–225. [Google Scholar] [CrossRef]
- Rudnev, M.; Lydkina, E.; Davidov, E.; Schmidt, P.; Zick, A. Testing measurement invariance for a second-order factor. A cross-national test of the alienation scale. Methods Data Anal. 2018, 12, 30. [Google Scholar] [CrossRef]
- Xia, Y.; Yang, Y. RMSEA, CFI, and TLI in structural equation modelling with ordered categorical data: The story they tell depends on the estimation methods. Behav. Res. Methods 2019, 51, 409–428. [Google Scholar] [CrossRef]
- Kyndt, E.; Onghena, P. The integration of work and learning: Tackling the complexity by means of structural equation modeling. In Discourses on Professional Learning: On the Boundary between Learning and Working, 2014th ed.; Harteis, C., Rausch, A., Seifried, J., Eds.; Springer: Berlin/Heidelberg, Germany, 2014; Available online: https://www.researchgate.net/publication/268279544 (accessed on 6 February 2024). [CrossRef]
- Hooper, D.; Caughlan, J.; Mullen, M.R. Structural equation modeling: Guidelines for determining model fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar] [CrossRef]
- Rajiv, J.; Hammond, T. Principles of Social Psychology, 1st International H5P ed.; BCcampus Open Education: Victoria, BC, Canada, 2023; Available online: https://opentextbc.ca/socialpsychology/chapter/exploring-attitudes/ (accessed on 6 February 2024).
- Malinowska, E.; Dzwonkowska-Godula, K.; Garncarek, E.; Czernecka, J.; Brzezińska, J. Gender, Age and Gendered Age in Relation to Attitudes to One’s Own Appearance and Health (Chosen Aspects); University of Lodz: Łódź, Poland, 2017; Available online: https://wydawnictwo.uni.lodz.pl/wp-content/uploads/2018/04/Malinowska-i-in._Gender-.pdf (accessed on 6 February 2024).
- Brennan, J.; Chanfreau, J.; Finnegan, J.; Griggs, J.; Kiss, Z.; Park, A. The Effect of Higher Education on Graduate’s Attitudes: Secondary Analysis of the British Social Attitudes Survey; BIS Research Paper No. 200; Department for Business, Innovation & Skills of the UK Government: London, UK, 2015. Available online: https://assets.publishing.service.gov.uk/media/5a74ea9fe5274a3cb2868385/BIS-15-89-the-effect-of-higher-education-on-attitudes.pdf (accessed on 6 February 2024).
- Chen, L.; Hong, J.; Xiong, D.; Zhang, L.; Li, Y.; Huang, S.; Hua, F. Are parents’ education levels associated with either their oral health knowledge or their children’s oral health behaviors? A survey of 8446 families in Wuhan. BMC Oral Health 2020, 20, 203. [Google Scholar] [CrossRef] [PubMed]
- Lambert, M.J.; Vanobbergen, J.S.N.; Martens, L.C.; De Visschere, L.M.J. Socioeconomic inequalities in caries experience, care level and dental attendance in primary school children in Belgium: A cross-sectional survey. BMJ Open 2017, 7, e015042. [Google Scholar] [CrossRef] [PubMed]
- Crouch, E.; Nelson, J.; Merrell, M.A.; Martin, A. The oral health status of America’s rural children: An opportunity for policy change. J. Public Health Dent. 2021, 81, 251–260. [Google Scholar] [CrossRef]
- Verplanken, B.; Orbell, S. Attitudes, habits, and behavior change. Annu. Rev. Psychol. 2022, 73, 327–352. [Google Scholar] [CrossRef]
- Clarke, R.; Shaw-Ridley, M. Parental attitudes and beliefs about preschooler preventive oral health behaviors: Implications for health promotion. J. Immigr. Minor. Health 2019, 21, 731–736. [Google Scholar] [CrossRef]
- Duijster, D.; de Jong-Lenters, M.; Verrips, E.; van Loveren, C. Establishing oral health promoting behaviours in children—Parents’ views on barriers, facilitators and professional support: A qualitative study. BMC Oral Health 2015, 15, 157. [Google Scholar] [CrossRef]


| Characteristic | n | % |
|---|---|---|
| Gender of respondents: | ||
| males (fathers) | 40 | 13.2 |
| females (mothers) | 262 | 86.8 |
| Age of respondents: | ||
| <35 years | 165 | 54.6 |
| ≥35 years | 137 | 45.4 |
| Gender of children: | ||
| boys | 164 | 54.3 |
| girls | 138 | 45.7 |
| Age of children: | ||
| <5 years | 151 | 50.0 |
| ≥5 years | 151 | 50.0 |
| Kindergartens location: | ||
| urban area | 202 | 66.9 |
| rural area | 100 | 33.1 |
| Education level of respondents: | ||
| less than college or university | 76 | 25.2 |
| college or university | 226 | 74.8 |
| The respondent brushes his/her teeth: | ||
| 2 times a day | 228 | 75.5 |
| less than 2 times a day | 74 | 24.5 |
| The child brushes his/her teeth: | ||
| 2 times a day | 167 | 55.3 |
| less than 2 times a day | 135 | 44.7 |
| How does the child brush his/her teeth: | ||
| the child brushes his teeth by himself | 142 | 47.0 |
| parents help the child brush his/her teeth | 160 | 53.0 |
| The respondent visits the dentist with the child: | ||
| once a year or more frequently | 187 | 61.9 |
| irregularly | 115 | 38.1 |
| Respondent’s dental health status: | ||
| good | 244 | 80.8 |
| poor | 58 | 19.2 |
| Child’s dental health status: | ||
| good | 240 | 79.5 |
| poor | 62 | 20.5 |
| Item No. | Dimensions, Factors, and Items | Attitude 1 | Percentage of Definite Answers 2 | Item Mean 3 | Skewness |
|---|---|---|---|---|---|
| Dimension TB: Parental attitudes towards children’s tooth brushing behaviour (Cronbach’s alpha = 0.633) | |||||
| Factor TB1: Importance and intention to brush the child’s teeth (Cronbach’s alpha = 0.618) | |||||
| b1 | As a family, we intend on brushing our child’s teeth for him/her | positive | 99.3 | 1.12 | 4.07 |
| b2 | We intend brushing our child’s teeth for him/her twice a day | positive | 99.0 | 1.21 | 2.48 |
| b3 | The people in my family would feel it was important to help brush our child’s teeth twice a day | positive | 99.3 | 1.35 | 1.48 |
| b4 | The people we know well would feel it was important to brush our child’s teeth twice a day | positive | 86.1 | 1.65 | 0.90 |
| b5 | We feel able to brush our child’s teeth for him/her | positive | 99.3 | 2.70 | 0.17 |
| Factor TB2: Parental efficacy in relation to child tooth brushing (Cronbach’s alpha = 0.697) | |||||
| b6 | If our child does not want to brush his/her teeth every day, we don’t feel we should make them | negative | 97.4 | 3.40 | −1.21 |
| b7 | I don’t know how to brush my child’s teeth properly | negative | 96.4 | 3.28 | −0.83 |
| b8 | It would not make any difference to our child getting tooth decay if we helped him/her brush every day | negative | 93.4 | 3.29 | −1.03 |
| b9 | We don’t have time to help brush our child’s teeth twice a day | negative | 98.0 | 3.60 | −1.73 |
| b10 | We cannot make our child brush his/her teeth twice a day | negative | 94.4 | 3.39 | −1.17 |
| b11 | It is not worth it to battle with our child to brush his/her teeth twice a day | negative | 96.4 | 3.50 | −1.61 |
| Factor TB3: Attitudes towards prevention (Cronbach’s alpha = 0.588) | |||||
| b12 | It is important to clean my child’s teeth every day so my child has a nice smile | positive | 96.4 | 1.38 | 1.72 |
| b13 | If we brush our child’s teeth twice a day, we can prevent our child getting tooth decay in the future | positive | 97.4 | 1.33 | 1.78 |
| b14 | If our child uses fluoride toothpaste, it will prevent tooth decay | positive | 80.8 | 1.86 | 0.47 |
| Dimension SS: Parental attitudes towards child sugar snacking (Cronbach’s alpha = 0.689) | |||||
| Factor SS1: Importance and intention to control child sugar snacking (Cronbach’s alpha = 0.767) | |||||
| s1 | We can prevent tooth decay in our children by reducing sugary foods and drinks between meals | positive | 98.7 | 1.52 | 1.21 |
| s2 | As a family, we intend controlling how often our child has sugary foods or drinks between meals | positive | 99.0 | 1.71 | 0.80 |
| s3 | The people in my family would feel it was important to control how often our child has sugary foods and drinks between meals | positive | 98.0 | 1.61 | 1.04 |
| s4 | Our child eating sugary foods and drinks in between meals would cause tooth decay | positive | 96.4 | 1.69 | 0.93 |
| s5 | The people we know well would feel it was important to control how often our child has sugary foods and drinks | positive | 83.4 | 1.95 | 0.44 |
| Factor SS2: Parental efficacy in relation to controlling child sugar snacking (Cronbach’s alpha = 0.677) | |||||
| s6 | As a family, we feel it is difficult for us to stop our child having sugary foods | negative | 97.0 | 2.86 | −0.20 |
| s7 | It is worthwhile to give our child sweets/biscuits to behave well | negative | 95.4 | 3.27 | −0.85 |
| s8 | In our family, it would be unfair not to give sweets to our child every day | negative | 95.4 | 2.63 | 0.07 |
| s9 | It is often too stressful to say no to my child when he/she wants sweets | negative | 93.0 | 3.03 | −0.51 |
| Dimension DD: Parental attitudes towards child dental decay (Cronbach’s alpha = 0.690) | |||||
| Factor DD1: Perceived seriousness of tooth decay in children (Cronbach’s alpha = 0.718) | |||||
| d1 | As a family, we are confident we can reduce the chances of our child from getting tooth decay | positive | 93.7 | 1.78 | 0.56 |
| d2 | Tooth decay will not get better by itself | positive | 90.4 | 1.44 | 1.81 |
| d3 | Tooth decay would have major consequences on our child’s general health | positive | 92.1 | 1.39 | 1.75 |
| d4 | Tooth decay is a serious problem in baby teeth | positive | 91.7 | 1.40 | 1.05 |
| d5 | As parents, it is our responsibility to prevent our child getting tooth decay | positive | 98.0 | 1.23 | 1.85 |
| d6 | Our child losing a baby tooth due to tooth decay would be upsetting | positive | 93.0 | 1.44 | 1.25 |
| d7 | We feel it is important that we check our child’s teeth for decay | positive | 98.4 | 1.19 | 2.54 |
| Factor DD2: Chance control—decay occurs by chance (Cronbach’s alpha = 0.731) | |||||
| d8 | No matter what we do, our child is likely to get tooth decay | negative | 77.2 | 2.77 | −0.07 |
| d9 | It is just bad luck if our child gets tooth decay | negative | 84.8 | 3.38 | −0.89 |
| d10 | If our child gets tooth decay, it is by chance | negative | 85.8 | 3.48 | −1.13 |
| d11 | Tooth decay runs in families | negative | 83.8 | 2.48 | 0.53 |
| d12 | Some people just naturally have soft teeth | negative | 88.7 | 2.14 | 0.66 |
| Factor DD3 External control—preventing decay is the dentist’s responsibility (Cronbach’s alpha = 0.628) | |||||
| d13 | It is the responsibility of the dentist to prevent our child getting tooth decay | negative | 92.7 | 2.55 | 0.18 |
| d14 | Bringing our child to the dentist on a regular basis is the best way to prevent tooth decay | negative | 96.7 | 1.79 | 0.92 |
| d15 | The dentist is the best person to prevent tooth decay in our child | negative | 93.7 | 2.81 | −0.19 |
| Dimensions and Items | Factors and Loadings | ||
|---|---|---|---|
| Dimension TB | TB1 | TB2 | TB3 |
| b1 | 0.527 | ||
| b2 | 0.775 | ||
| b3 | 0.345 | ||
| b4 | 0.544 | ||
| b5 | −0.170 | 0.155 | |
| b6 | 0.764 | ||
| b7 | 0.432 | ||
| b8 | 0.406 | 0.427 | |
| b9 | 0.517 | ||
| b10 | 0.785 | ||
| b11 | 0.748 | ||
| b12 | 0.653 | ||
| b13 | 0.759 | ||
| b14 | 0.678 | ||
| Dimension SS | SS1 | SS2 | |
| s1 | 0.688 | ||
| s2 | 0.698 | ||
| s3 | 0.768 | ||
| s4 | 0.795 | ||
| s5 | 0.628 | ||
| s6 | 0.624 | ||
| s7 | 0.741 | ||
| s8 | 0.660 | ||
| s9 | 0.793 | ||
| Dimension DD | DD1 | DD2 | DD3 |
| d1 | 0.438 | ||
| d2 | 0.466 | ||
| d3 | 0.756 | ||
| d4 | 0.744 | ||
| d5 | 0.696 | ||
| d6 | 0.618 | ||
| d7 | 0.517 | ||
| d8 | 0.649 | ||
| d9 | 0.634 | ||
| d10 | 0.655 | ||
| d11 | 0.762 | ||
| d12 | 0.665 | ||
| d13 | 0.662 | ||
| d14 | 0.698 | ||
| d15 | 0.838 | ||
| Groups of Respondents or Children to Be Compared | Multiple-Group Factor Analysis 1 | Sum Score Analysis | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Conditional Factor Means (Δχ2 (df); p) 2 | Correlations between Factors (Δχ2; p) 3 | Means of Sum Scores | Correlations between Sum Scores | |||||||||
| TB | SS | DD | TB–SS | SS–DD | TB–DD | TB | SS | DD | TB–SS | SS–DD | TB–DD | |
| Gender of respondents: | (Δχ2 = 0.687 (3); p = 0.876) | (Δχ2 = 23.416 (6); p = 0.001) | ||||||||||
| males | 0 | 0 | 0 | 0.218 | 0.277 | 0.820 * | 27.89 | 22.19 | 21.24 | 0.261 | 0.158 | 0.557 *** |
| females | 0.016 | −0.001 | 0.060 | 0.683 * | 0.781 *** | 0.627 * | 27.85 | 22.42 | 21.43 | 0.330 *** | 0.337 *** | 0.370 *** |
| Age of respondents: | (Δχ2 = 2.532 (3); p = 0.469) | (Δχ2 = 8.744 (6); p = 0.188) | ||||||||||
| <35 years | 0.027 | 0.023 | −0.039 | 0.639 ** | 0.642 *** | 0.715 ** | 28.06 | 22.52 | 21.38 | 0.331 *** | 0.363 *** | 0.363 *** |
| ≥35 years | 0 | 0 | 0 | 0.647 ** | 0.724 *** | 0.854 ** | 27.60 | 22.23 | 21.43 | 0.300 *** | 0.233 ** | 0.444 *** |
| Gender of children: | (Δχ2 = 2.954 (3); p = 0.399) | (Δχ2 = 10.757 (6); p = 0.096) | ||||||||||
| boys | 0 | 0 | 0 | 0.421 * | 0.846 *** | 0.838 *** | 27.70 | 22.57 | 21.11 | 0.212 ** | 0.351 *** | 0.444 *** |
| girls | −0.023 | 0.027 | −0.058 | 0.622 ** | 0.729 *** | 0.846 *** | 27.98 | 22.24 | 21.65 | 0.449 *** | 0.278 *** | 0.339 *** |
| Age of children: | (Δχ2 = 1.942; p = 0.585) | (Δχ2 = 9.129; p = 0.166) | ||||||||||
| <5 years | 0.024 | 0.058 | 0.052 | 0.538 * | 0.966 *** | 0.682 ** | 27.94 | 22.72 | 21.55 | 0.348 *** | 0.422 *** | 0.411 *** |
| ≥5 years | 0 | 0 | 0 | 0.740 * | 0.504 ** | 0.955 ** | 27.76 | 22.06 | 21.25 | 0.291 *** | 0.198 ** | 0.378 *** |
| Children from kindergartens located in: | (Δχ2 = 6.553; p = 0.088) | (Δχ2 = 15.131; p = 0.019) | ||||||||||
| urban area | 0.060 | 0.135 * | 0.092 | 0.361 * | 0.590 *** | 0.699 ** | 28.19 ** | 22.77 ** | 21.67 * | 0.242 *** | 0.254 *** | 0.327 *** |
| rural area | 0 | 0 | 0 | 0.508 ** | 0.632 *** | 0.793 ** | 27.18 | 21.62 | 20.87 | 0.414 *** | 0.368 *** | 0.464 *** |
| Education level of respondents: | (Δχ2 = 13.856 (3); p = 0.003) | (Δχ2 = 13.072 (6); p = 0.042) | ||||||||||
| less than college or university | 0 | 0 | 0 | 0.494 ** | 0.588 *** | 0.733 *** | 27.82 | 22.30 | 20.47 | 0.339 ** | 0.363 *** | 0.510 *** |
| college or university | −0.055 | 0.010 | 0.137 ** | 0.380 * | 0.522 *** | 0.656 ** | 27.87 | 22.42 | 21.72 *** | 0.314 *** | 0.299 *** | 0.359 *** |
| The respondent brushes his/her teeth: | (Δχ2 = 5.708 (3); p = 0.127) | (Δχ2 = 4.458 (6); p = 0.615) | ||||||||||
| 2 times a day | 0.071 | 0.070 | 0.132 * | 0.658 ** | 0.756 *** | 0.846 *** | 28.32 *** | 22.51 | 21.62 * | 0.330 *** | 0.327 *** | 0.373 *** |
| less than 2 times a day | 0 | 0 | 0 | 0.868 ** | 0.912 ** | 0.898 ** | 26.43 | 22.01 | 20.72 | 0.269* | 0.251 * | 0.377 *** |
| The child brushes his/her teeth: | (Δχ2 = 34.184 (3); p < 0.001) | (Δχ2 = 3.372 (6); p = 0.761) | ||||||||||
| 2 times a day | 0.357 *** | 0.127 * | 0.023 | 0.526 ** | 0.767 *** | 0.786 *** | 28.81 *** | 22.74* | 21.49 | 0.299 *** | 0.357 *** | 0.373 *** |
| less than 2 times a day | 0 | 0 | 0 | 0.899 ** | 0.727 *** | 0.828 *** | 26.67 | 21.96 | 21.29 | 0.304 | 0.246 ** | 0.448 *** |
| How does the child brush his/her teeth: | (Δχ2 = 18.115 (3); p < 0.001) | (Δχ2 = 9.340 (6); p = 0.135) | ||||||||||
| the child brushes his teeth by himself/ | 0 | 0 | 0 | 0.713 * | 0.862 *** | 0.624 * | 27.45 | 21.98 | 20.72 | 0.284 ** | 0.363 *** | 0.307 *** |
| parents help the child brush his teeth | 0.011 | 0.119* | 0.171 *** | 0.574 * | 0.670 *** | 0.930 ** | 28.21 * | 22.75 * | 22.01 *** | 0.337 *** | 0.219 ** | 0.462 *** |
| The child visits the dentist: | (Δχ2 = 9.216 (3); p = 0.027) | (Δχ2 = 2.030 (6); p = 0.917) | ||||||||||
| once a year or more frequently | 0.049 | 0.103 * | 0.134 ** | 0.693 ** | 0.653 *** | 0.824 ** | 28.19 * | 22.68 * | 21.79 *** | 0.349 *** | 0.311 *** | 0.367 *** |
| irregularly | 0 | 0 | 0 | 0.604 * | 0.888 *** | 0.858 * | 27.31 | 21.82 | 20.78 | 0.241 ** | 0.279 ** | 0.400 *** |
| Respondent’s dental health status: | (Δχ2 = 9.200 (3); p = 0.027) | (Δχ2 = 5.318; p = 0.504) | ||||||||||
| good | 0.060 | 0.005 | 0.185 ** | 0.638 ** | 0.708 *** | 0.795 ** | 28.10 ** | 22.43 | 21.65 *** | 0.338 *** | 0.331 *** | 0.372 *** |
| poor | 0 | 0 | 0 | 0.658 ** | 0.738 *** | 0.824 ** | 26.82 | 22.22 | 20.36 | 0.233 | 0.239 | 0.391 ** |
| Child’s dental health status: | (Δχ2 = 2.994; p = 0.393) | (Δχ2 = 6.443; p = 0.375) | ||||||||||
| good | 0.028 | 0.040 | 0.116 | 0.622 * | 0.716 *** | 0.839 * | 28.08 * | 22.48 | 21.61 ** | 0.326 *** | 0.333 *** | 0.349 *** |
| poor | 0 | 0 | 0 | 0.685 | 0.883 * | 0.625 | 26.98 | 22.06 | 20.59 | 0.287 * | 0.222 | 0.476 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaborskis, A.; Razmienė, J.; Razmaitė, A.; Andruškevičienė, V.; Narbutaitė, J.; Bendoraitienė, E.A.; Kavaliauskienė, A. Parental Attitudes towards Child Oral Health and Their Structural Analysis. Children 2024, 11, 333. https://doi.org/10.3390/children11030333
Zaborskis A, Razmienė J, Razmaitė A, Andruškevičienė V, Narbutaitė J, Bendoraitienė EA, Kavaliauskienė A. Parental Attitudes towards Child Oral Health and Their Structural Analysis. Children. 2024; 11(3):333. https://doi.org/10.3390/children11030333
Chicago/Turabian StyleZaborskis, Apolinaras, Jaunė Razmienė, Augustė Razmaitė, Vilija Andruškevičienė, Julija Narbutaitė, Eglė Aida Bendoraitienė, and Aistė Kavaliauskienė. 2024. "Parental Attitudes towards Child Oral Health and Their Structural Analysis" Children 11, no. 3: 333. https://doi.org/10.3390/children11030333
APA StyleZaborskis, A., Razmienė, J., Razmaitė, A., Andruškevičienė, V., Narbutaitė, J., Bendoraitienė, E. A., & Kavaliauskienė, A. (2024). Parental Attitudes towards Child Oral Health and Their Structural Analysis. Children, 11(3), 333. https://doi.org/10.3390/children11030333