Pediatric Patients with Osteomyelitis and/or Septic Joint Undergoing Surgical Debridement Have Equivalent Short-Term Outcomes with or without Preoperative MRI
Abstract
1. Introduction
2. Materials and Methods
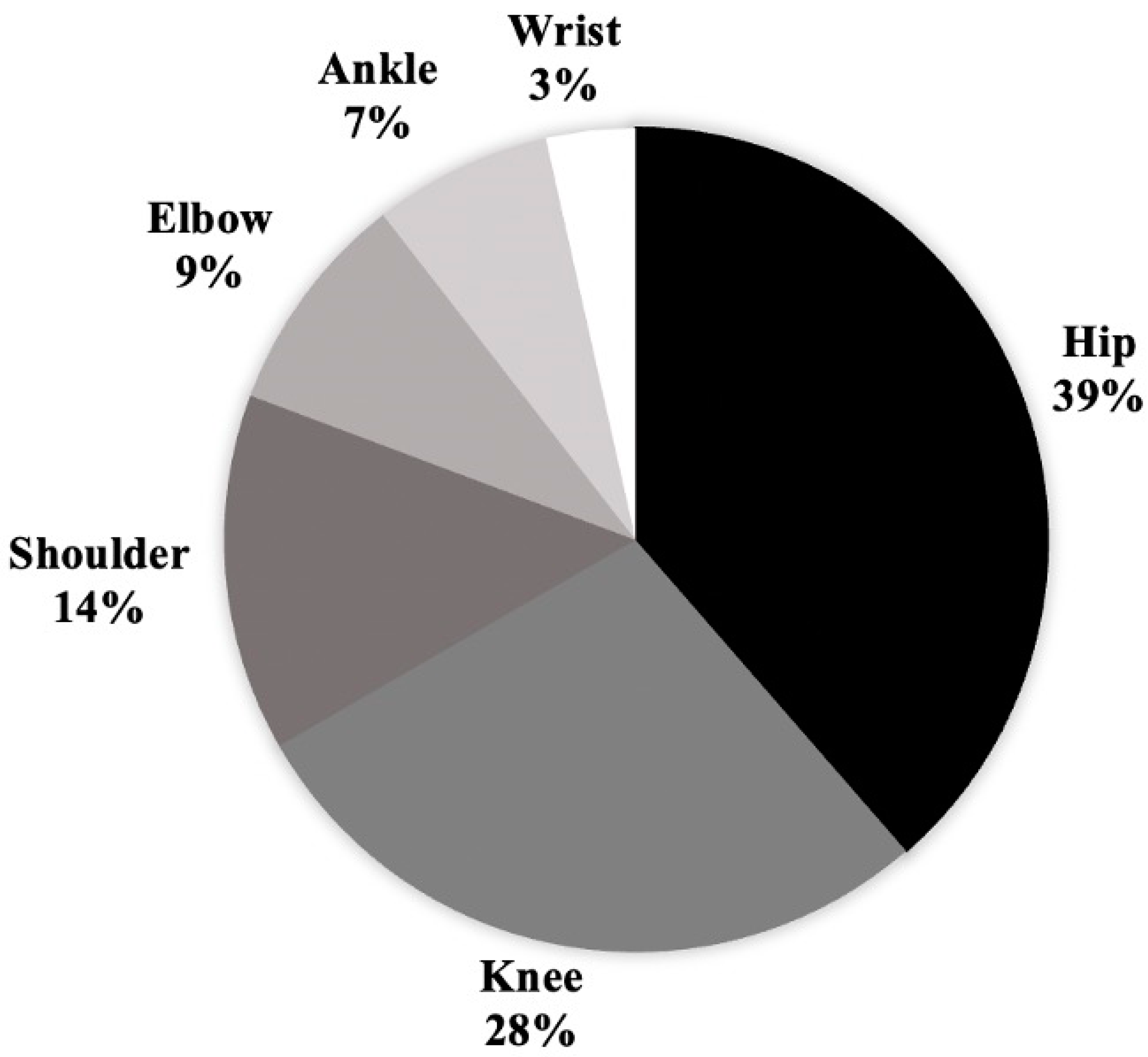
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gafur, O.A.; Copley, L.A.; Hollmig, S.T.; Browne, R.H.; Thornton, L.A.; Crawford, S.E. The impact of the current epidemiology of pediatric musculoskeletal infection on evaluation and treatment guidelines. J. Pediatr. Orthop. 2008, 28, 777–785. [Google Scholar] [CrossRef]
- Gornitzky, A.L.; Kim, A.E.; O’Donnell, J.M.; Swarup, I. Diagnosis and Management of Osteomyelitis in Children: A Critical Analysis Review. JBJS Rev. 2020, 8, e1900202. [Google Scholar] [CrossRef]
- Nguyen, A.; Kan, J.H.; Bisset, G.; Rosenfeld, S. Kocher Criteria Revisited in the Era of MRI: How Often Does the Kocher Criteria Identify Underlying Osteomyelitis? J. Pediatr. Orthop. 2017, 37, e114–e119. [Google Scholar] [CrossRef]
- Monsalve, J.; Kan, J.H.; Schallert, E.K.; Bisset, G.S.; Zhang, W.; Rosenfeld, S.B. Septic arthritis in children: Frequency of coexisting unsuspected osteomyelitis and implications on imaging work-up and management. AJR Am. J. Roentgenol. 2015, 204, 1289–1295. [Google Scholar] [CrossRef] [PubMed]
- Mignemi, M.E.; Menge, T.J.; Cole, H.A.; Mencio, G.A.; Martus, J.E.; Lovejoy, S.; Stutz, C.M.; Schoenecker, J.G. Epidemiology, diagnosis, and treatment of pericapsular pyomyositis of the hip in children. J. Pediatr. Orthop. 2014, 34, 316–325. [Google Scholar] [CrossRef]
- Hunter, S.; Kioa, G.; Baker, J.F. Predictive Algorithms in the Diagnosis and Management of Pediatric Hip and Periarticular Infection. J. Bone Jt. Surg. Am. 2022, 104, 649–658. [Google Scholar] [CrossRef]
- Michalowitz, A.; Yang, J.; Castaneda, P.; Litrenta, J. Existing and emerging methods of diagnosis and monitoring of pediatric musculoskeletal infection. Injury 2020, 51, 2110–2117. [Google Scholar] [CrossRef]
- Wu, J.P. Pediatric Anesthesia Concerns and Management for Orthopedic Procedures. Pediatr. Clin. N. Am. 2020, 67, 71–84. [Google Scholar] [CrossRef] [PubMed]
- Artunduaga, M.; Liu, C.A.; Morin, C.E.; Serai, S.D.; Udayasankar, U.; Greer, M.C.; Gee, M.S. Safety challenges related to the use of sedation and general anesthesia in pediatric patients undergoing magnetic resonance imaging examinations. Pediatr. Radiol. 2021, 51, 724–735. [Google Scholar] [CrossRef] [PubMed]
- Swarup, I.; LaValva, S.; Shah, R.; Sankar, W.N. Septic Arthritis of the Hip in Children: A Critical Analysis Review. JBJS Rev. 2020, 8, e0103. [Google Scholar] [CrossRef]
- Swarup, I.; Meza, B.C.; Weltsch, D.; Jina, A.A.; Lawrence, J.T.; Baldwin, K.D. Septic Arthritis of the Knee in Children: A Critical Analysis Review. JBJS Rev. 2020, 8, e0069. [Google Scholar] [CrossRef]
- Kocher, M.S.; Zurakowski, D.; Kasser, J.R. Differentiating between septic arthritis and transient synovitis of the hip in children: An evidence-based clinical prediction algorithm. J. Bone Jt. Surg. Am. 1999, 81, 1662–1670. [Google Scholar] [CrossRef]
- Hannon, M.; Lyons, T. Pediatric musculoskeletal infections. Curr. Opin. Pediatr. 2023, 35, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Erkilinc, M.; Gilmore, A.; Weber, M.; Mistovich, R.J. Current Concepts in Pediatric Septic Arthritis. J. Am. Acad. Orthop. Surg. 2021, 29, 196–206. [Google Scholar] [CrossRef]
- Saleh, E.S. Pediatric Obturator Internus Muscle Myxoma. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2021, 5, e20.00099. [Google Scholar] [CrossRef]
- Adam, M.; Ibrahim, B.; Khidir, R.; Elmahdi, E.; Ahmed, S.; Ahmed, A. Usefulness of MRI findings in differentiating between septic arthritis and transient synovitis of hip joint in children: A systematic review and meta-analysis. Eur. J. Radiol. Open. 2022, 9, 100439. [Google Scholar] [CrossRef] [PubMed]
- Griswold, B.G.; Sheppard, E.; Pitts, C.; Gilbert, S.R.; Khoury, J.G. The Introduction of a Preoperative MRI Protocol Significantly Reduces Unplanned Return to the Operating Room in the Treatment of Pediatric Osteoarticular Infections. J. Pediatr. Orthop. 2020, 40, 97–102. [Google Scholar] [CrossRef]
- Telleria, J.J.; Cotter, R.A.; Bompadre, V.; Steinman, S.E. Laboratory predictors for risk of revision surgery in pediatric septic arthritis. J. Child. Orthop. 2016, 10, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Nunn, T.R.; Cheung, W.Y.; Rollinson, P.D. A prospective study of pyogenic sepsis of the hip in childhood. J. Bone Jt. Surg. Br. 2007, 89, 100–106. [Google Scholar] [CrossRef]
- Rosenfeld, S.; Bernstein, D.T.; Daram, S.; Dawson, J.; Zhang, W. Predicting the Presence of Adjacent Infections in Septic Arthritis in Children. J. Pediatr. Orthop. 2016, 36, 70–74. [Google Scholar] [CrossRef]
- Murphy, R.F.; Plumblee, L.; Barfield, W.B.; Murphy, J.S.; Fuerstenau, N.; Spence, D.D.; Kelly, D.M.; Dow, M.A.; Mooney, J.F., 3rd. Septic Arthritis of the Hip-Risk Factors Associated With Secondary Surgery. J. Am. Acad. Orthop. Surg. 2019, 27, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, C.O.; Siegel, E.; Blasier, R.D.; Suva, L.J. Concurrent septic arthritis and osteomyelitis in children. J. Pediatr. Orthop. 2013, 33, 464–467. [Google Scholar] [CrossRef] [PubMed]
- Ernat, J.; Riccio, A.I.; Fitzpatrick, K.; Jo, C.; Wimberly, R.L. Osteomyelitis is Commonly Associated with Septic Arthritis of the Shoulder in Children. J. Pediatr. Orthop. 2017, 37, 547–552. [Google Scholar] [CrossRef]
- Singhal, R.; Perry, D.C.; Khan, F.N.; Cohen, D.; Stevenson, H.L.; James, L.A.; Sampath, J.S.; Bruce, C.E. The use of CRP within a clinical prediction algorithm for the differentiation of septic arthritis and transient synovitis in children. J. Bone Jt. Surg. Br. 2011, 93, 1556–1561. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.S.; McBride, D.; Wild, J.; Kwon, S.; Samet, J.; Gibly, R.F. A Rapid MRI Protocol for Acute Pediatric Musculoskeletal Infection Eliminates Contrast, Decreases Sedation, Scan and Interpretation Time, Hospital Length of Stay and Charges [Conference Presentation]. In Proceedings of the POSNA 2023 Annual Meeting, Nashville, TN, USA, 26–28 April 2023. [Google Scholar]
| No Preop MRI (N = 29) | Preop MRI (N = 75) | Overall (N = 104) | p-Value | |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 6.2/7.0 [1.0, 10.0] | 7.6/6.0 [3.0, 12.0] | 7.3/6.0 [3.0, 11.0] | 0.17 I |
| Female | 14 (48.3%) | 26 (34.7%) | 40 (38.5%) | 0.20 II |
| Presentation | ||||
| Symptom Duration (Days) | 6.6/4.0 [2.0, 7.0] | 7.5/5.0 [3.0, 12.0] | 7.3/5.0 [2.5, 7.0] | 0.58 III |
| Temperature (°C) | 37.8/37.6 [37.2, 38.3] | 37.5/37.4 [36.9, 38.1] | 37.6/37.5 [36.9, 38.2] | 0.18 I |
| ESR (mm/h) | 49.5/44.5 [30.0, 89.5] | 52.3/59.0 [37.0, 75.0] | 51.8/58.0 [32.0, 80.0] | 0.90 I |
| CRP (mg/dL) | 10.9/7.6 [3.2, 12.7] | 11.6/9.0 [4.1, 14.4] | 11.5/8.8 [3.5, 14.4] | 0.39 III |
| WBC (K/µL) | 16.7/14.0 [10.0, 18.9] | 14.2/13.8 [9.1, 16.7] | 14.8/13.9 [9.2, 17.6] | 0.31 III |
| Positive Blood Culture | 8 (27.6%) | 23 (30.7%) | 31 (29.8%) | 0.79 II |
| Preoperative Joint Aspiration | 21 (72.4%) | 21 (28.0%) | 42 (40.4%) | <0.0001 II |
| Positive Joint Aspiration | 18/21 (85.7%) | 14/21 (67.7%) | 32/42 (76.2%) | 0.15 II |
| Timing of OR | ||||
| Same Day as Admission | 13 (44.8%) | 15 (20.0%) | 28 (26.9%) | 0.0037 II |
| Day after Admission | 14 (48.3%) | 33 (44.0%) | 47 (45.2%) | - |
| 2 or More Days after MRI | 2 (6.9%) | 27 (36.0% | 29 (27.9%) | - |
| Final Diagnosis | ||||
| Osteomyelitis | 4 (13.8%) | 43 (57.3%) | 47 (45.2%) | <0.0001 II |
| Septic Joint | 19 (65.5%) | 15 (20.0%) | 34 (32.7%) | - |
| Septic Joint + Osteomyelitis | 6 (20.7%) | 17 (22.7%) | 23 (22.1%) | - |
| No Preop MRI (N = 29) | Preop MRI (N = 75) | Overall (N = 104) | p-Value | |
|---|---|---|---|---|
| Outcomes | ||||
| Time from OR to Discharge (Days) | 5.8/5.0 [4.0, 8.0] | 5.4/4.0 [3.0, 7.0] | 5.5/5.0 [3.0, 7.0] | 0.57 II |
| Total Number of Debridements | ||||
| 1 | 21 (72.4%) | 56 (74.7%) | 77 (74.0%) | 0.23 III |
| 2 | 7 (24.1%) | 10 (13.3%) | 17 (16.3%) | - |
| 3+ | 1 (3.4%) | 9 (12.0%) | 10 (9.6%) | - |
| Total Admissions | ||||
| 1 | 26 (89.7%) | 60 (80.0%) | 86 (82.7%) | 0.24 I |
| 2+ | 3 (10.3%) | 15 (20.0%) | 18 (17.3%) | - |
| Total MRIs | ||||
| 1 | 23 (79.3%) | 51 (68.0%) | 74 (71.2%) | 0.23 III |
| 2 | 5 (17.2%) | 12 (16.0%) | 17 (16.3%) | - |
| 3+ | 1 (3.4%) | 12 (16.0%) | 13 (12.5%) | - |
| No Preop MRI (N = 25) | Preop MRI (N = 32) | Overall (N = 57) | p-Value | |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 6.4/6.0 [3.0, 10.0] | 5.8/3.5 [2.0, 11.0] | 6.1/5.0 [2.0, 11.0] | 0.72 II |
| Female | 11 (44%) | 11 (34.4%) | 22 (38.6%) | 0.46 I |
| Presentation | ||||
| Symptom Duration (Days) | 5.0/6.4 [2.0, 7.0] | 6.8/4.5 [2.5, 7.0] | 6.1/5.0 [2.0, 7.0] | 0.71 II |
| Temperature (°C) | 37.8/37.6 [37.4, 38.3] | 37.6/37.5 [37.2, 38.0] | 37.7/37.6 [37.2, 38.1] | 0.27 II |
| ESR (mm/h) | 50.0/60.5 [31.0, 91.0] | 58.3/58.0 [31.0, 80.0] | 55.8/58.0 [31.0, 90.0] | 0.57 II |
| CRP (mg/dL) | 12.5/8.3 [4.0, 16.7] | 9.4/8.8 [4.7, 10.6] | 10.3/8.7 [4.1, 12.4] | 0.85 II |
| WBC (K/µL) | 15.5/12.8 [10.0, 18.0] | 14.3/14.4 [10.3, 15.9] | 14.8/14.0 [10.0, 17.0] | 0.58 II |
| Positive Blood Culture | 7 (28.0%) | 9 (28.1%) | 16 (28.1%) | 0.77 III |
| Preoperative Joint Aspiration | 20 (80.0%) | 15 (46.9%) | 35 (61.4%) | 0.01 I |
| Positive Joint Aspiration | 18/20 (92.0%) | 11/15 (73.3%) | 29/35 (50.9%) | 0.20 I |
| Timing of OR | ||||
| Same Day as Admission | 12 (48.0%) | 7 (21.9%) | 19 (33.3%) | 0.023 I |
| Day after Admission | 12 (48.0%) | 16 (50.0%) | 28 (49.1%) | - |
| 2 or More Days after MRI | 1 (4.0%) | 9 (28.1)% | 10 (17.5%) | - |
| No Preop MRI (N = 25) | Preop MRI (N = 32) | Overall (N = 57) | p-Value | |
|---|---|---|---|---|
| Outcomes | ||||
| Time from OR to Discharge (Days) | 6.7/5.0 [4.0, 8.0] | 6.2/5.0 [4.0, 7.5] | 6.4/5.0 [4.0, 8.0] | 0.77 I |
| Total Number of Debridements | ||||
| 1 | 17 (68.0%) | 27 (84.4%) | 44 (77.2%) | 0.17 II |
| 2 | 7 (28.0%) | 3 (9.4%) | 10 (17.5%) | - |
| 3+ | 1 (4.0%) | 2 (6.3%) | 3 (5.3%) | - |
| Total Admissions | ||||
| 1 | 22 (88.0%) | 27 (84.4%) | 49 (86.0%) | 1 II |
| 2+ | 3 (12.0%) | 5 (15.6%) | 8 (14.0%) | - |
| Total MRIs | ||||
| 1 | 20 (80.0%) | 22 (68.8%) | 42 (73.7%) | 0.46 II |
| 2 | 4 (16.0%) | 5 (15.6%) | 9 (15.8%) | - |
| 3+ | 1 (4.0%) | 5 (15.6%) | 6 (10.5%) | - |
| Joint | Preop MRI | No Preop MRI | Total | p-Value |
|---|---|---|---|---|
| Hip | 13 | 9 | 22 | |
| Concurrent OM | 8 | 2 | 10 | 0.068 I |
| OM Debridement | 3 | 0 | 3 | 0.121 I |
| Knee | 8 | 8 | 16 | |
| Concurrent OM | 4 | 4 | 4 | 1.000 I |
| OM Debridement | 0 | 0 | 0 | 1.000 I |
| Shoulder | 5 | 3 | 8 | |
| Concurrent OM | 3 | 1 | 4 | 0.465 I |
| OM Debridement | 1 | 0 | 1 | 0.408 I |
| Elbow | 3 | 2 | 5 | |
| Concurrent OM | 1 | 1 | 2 | 0.709 I |
| OM Debridement | 1 | 1 | 2 | 0.709 I |
| Ankle | 3 | 1 | 4 | |
| Concurrent OM | 3 | 0 | 3 | 0.046 I |
| OM Debridement | 3 | 0 | 3 | 0.046 I |
| Wrist | 0 | 2 | 2 | |
| Concurrent OM | 0 | 0 | 0 | 1.000 I |
| OM Debridement | 0 | 0 | 0 | 1.000 I |
| Total | 32 | 25 | 57 | |
| Concurrent OM | 17 | 6 | 23 | 0.026 I |
| OM Debridement | 8 | 1 | 9 | 0.031 I |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Englert, E.G.; Braithwaite, C.L.; Aguirre-Flores, M.E.; Lam, A.W.; Sarraj, M.; Kumagai, A.; Bednar, E.D.; Gordon, A.M.; Salama, I.; Keeley, J.; et al. Pediatric Patients with Osteomyelitis and/or Septic Joint Undergoing Surgical Debridement Have Equivalent Short-Term Outcomes with or without Preoperative MRI. Children 2024, 11, 300. https://doi.org/10.3390/children11030300
Englert EG, Braithwaite CL, Aguirre-Flores ME, Lam AW, Sarraj M, Kumagai A, Bednar ED, Gordon AM, Salama I, Keeley J, et al. Pediatric Patients with Osteomyelitis and/or Septic Joint Undergoing Surgical Debridement Have Equivalent Short-Term Outcomes with or without Preoperative MRI. Children. 2024; 11(3):300. https://doi.org/10.3390/children11030300
Chicago/Turabian StyleEnglert, E. Graham, Collin L. Braithwaite, Maria E. Aguirre-Flores, Aaron W. Lam, Mohamed Sarraj, Abigail Kumagai, E. Dimitra Bednar, Adam M. Gordon, Ibrahim Salama, Jacob Keeley, and et al. 2024. "Pediatric Patients with Osteomyelitis and/or Septic Joint Undergoing Surgical Debridement Have Equivalent Short-Term Outcomes with or without Preoperative MRI" Children 11, no. 3: 300. https://doi.org/10.3390/children11030300
APA StyleEnglert, E. G., Braithwaite, C. L., Aguirre-Flores, M. E., Lam, A. W., Sarraj, M., Kumagai, A., Bednar, E. D., Gordon, A. M., Salama, I., Keeley, J., Pathak, I., Kishta, W., Thabet, A. M., Abdelgawad, A., & Saleh, E. (2024). Pediatric Patients with Osteomyelitis and/or Septic Joint Undergoing Surgical Debridement Have Equivalent Short-Term Outcomes with or without Preoperative MRI. Children, 11(3), 300. https://doi.org/10.3390/children11030300






