Associations among Maternal Trauma History, Postnatal Maternal Sensitivity, and Infant Temperament
Abstract
1. Introduction
1.1. Trauma
1.1.1. Childhood Trauma
1.1.2. Disasters
1.1.3. Interpersonal Violence
1.1.4. Posttraumatic Stress Disorder
1.2. Maternal Sensitivity
1.3. Infant Temperament
1.4. Associations among Maternal Trauma History, Sensitivity, and Infant Temperament
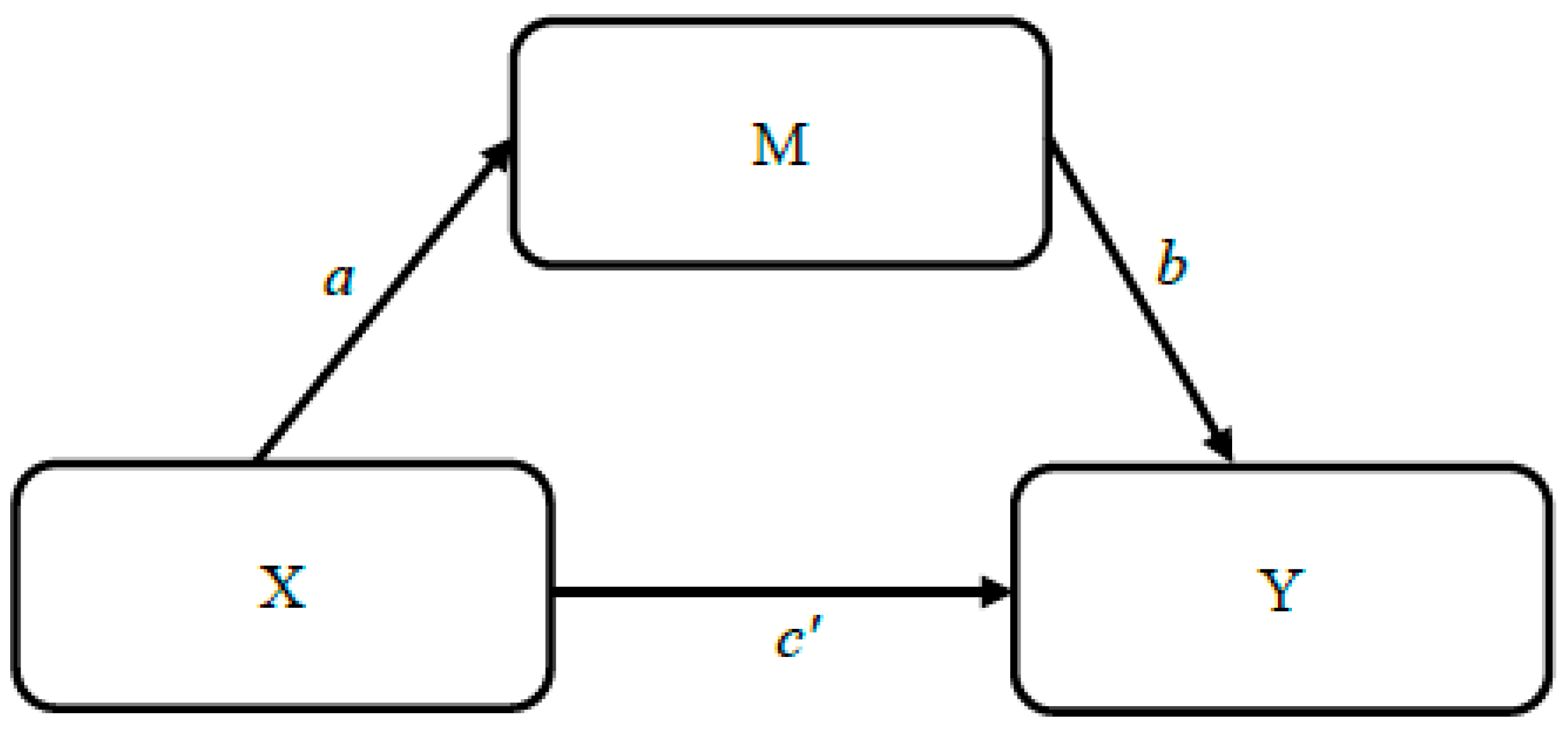
1.5. Proposed Model
1.6. Hypotheses
Hypothesis 1–3 (a–b)
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. Maternal Trauma History
2.3.2. Maternal Sensitivity
2.3.3. Infant Temperament
2.3.4. Covariates
2.4. Quantitative Analyses
3. Results
3.1. Descriptive Statistics and Covariates
3.2. Mediation Models
3.2.1. Model 1 (Hypothesis 1a)
3.2.2. Model 2 (Hypothesis 1b)
3.2.3. Model 3 (Hypothesis 2a)
3.2.4. Model 4 (Hypothesis 2b)
3.2.5. Model 5 (Hypothesis 3a)
3.2.6. Model 6 (Hypothesis 3b)
4. Discussion
4.1. Mediation Models
4.2. Infant Covariates
4.2.1. Infant Gender Differences
4.2.2. Maternal Trauma
4.2.3. Maternal Trauma and Infant Temperament
4.3. Study Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychological Association. Available online: https://www.apa.org/topics/women-girls/women-trauma (accessed on 29 November 2018).
- Wamser-Nanney, R.; Cherry, K.E. Children’s trauma-related symptoms following complex trauma exposure: Evidence of gender differences. Child Abuse Negl. 2018, 77, 188–197. [Google Scholar] [CrossRef]
- Braungart-Rieker, J.M.; Hill-Soderlund, A.L.; Karrass, J. Fear and anger reactivity trajectories from 4 to 16 months: The roles of temperament, regulation, and maternal sensitivity. Dev. Psychol. 2010, 46, 791. [Google Scholar] [CrossRef]
- Kivijärvi, M.; Räihä, H.; Kaljonen, A.; Tamminen, T.; Piha, J. Infant temperament and maternal sensitivity behavior in the first year of life. Scand. J. Psychol. 2005, 46, 421–428. [Google Scholar] [CrossRef]
- Leerkes, E.M.; Zhou, N. Maternal sensitivity to distress and attachment outcomes: Interactions with sensitivity to nondistress and infant temperament. J. Fam. Psychol. 2018, 32, 753. [Google Scholar] [CrossRef]
- Seng, J.; Taylor, J. Trauma Informed Care in the Perinatal Period; Dunedin Academic Press Ltd.: Edinburgh, UK, 2015. [Google Scholar]
- Howland, M.A.; Sandman, C.A.; Glynn, L.M. Developmental origins of the human hypothalamic-pituitary-adrenal axis. Expert Rev. Endocrinol Metab. 2017, 12, 321–339. [Google Scholar] [CrossRef]
- Juul, S.; Hendrix, C.; Robinson, B.; Stowe, Z.; Newport, D.; Brennan, P.; Johnson, K. Maternal early-life trauma and affective parenting style: The mediating role of HPA-axis function. Arch. Womens Ment. Health 2016, 19, 17–23. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Hughes, M.; Cossar, J. The relationship between maternal childhood emotional abuse/neglect and parenting outcomes: A systematic review. Child Abus. Rev. 2016, 25, 31–45. [Google Scholar] [CrossRef]
- Lang, A.J.; Gartstein, M.A.; Rodgers, C.S.; Lebeck, M.M. The impact of maternal childhood abuse on parenting and infant temperament. J. Child Adolesc. Psychiatr. Nurs. 2010, 23, 100–110. [Google Scholar] [CrossRef] [PubMed]
- Lyons-Ruth, K.; Block, D. The disturbed caregiving system: Relations among childhood trauma, maternal caregiving, and infant affect and attachment. Infant Ment. Health J. 1996, 17, 257–275. [Google Scholar] [CrossRef]
- Martinez-Torteya, C.; Dayton, C.J.; Beeghly, M.; Seng, J.S.; McGinnis, E.; Broderick, A.; Muzik, M. Maternal parenting predicts infant biobehavioral regulation among women with a history of childhood maltreatment. Dev. Psychopathol. 2014, 26, 379–392. [Google Scholar] [CrossRef] [PubMed]
- Harville, E.W.; Xiong, X.; Buekens, P. Disasters and perinatal health: A systematic review. Obstet. Gynecol. Surv. 2010, 65, 713. [Google Scholar] [CrossRef]
- May, C.L.; Wisco, B.E. Defining trauma: How level of exposure and proximity affect risk for posttraumatic stress disorder. Psychol. Trauma 2016, 8, 233. [Google Scholar] [CrossRef]
- Ahlfs-Dunn, S.M.; Huth-Bocks, A.C. Intimate partner violence and infant socioemotional development: The moderating effects of maternal trauma symptoms. Infant Ment. Health J. 2014, 35, 322–335. [Google Scholar] [CrossRef]
- Zou, S.; Zhang, Y.; Cao, Y.; Zhang, Y. Correlation of maternal abuse during pregnancy with infant temperament and development. Arch. Dis. Child 2015, 100, 938–943. [Google Scholar] [CrossRef]
- Enlow, M.B.; Kitts, R.L.; Blood, E.; Bizarro, A.; Hofmeister, M.; Wright, R.J. Maternal posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant Bev. Dev. 2011, 34, 487–503. [Google Scholar] [CrossRef]
- Bretherton, I. Revisiting Mary Ainsworth’s conceptualization and assessments of maternal sensitivity-insensitivity. Attach. Hum. Dev. 2013, 15, 460–484. [Google Scholar] [CrossRef]
- Koren-Karie, N.; Oppenheim, D.; Dolev, S.; Sher, E.; Etzion-Carasso, A. Mothers’ insightfulness regarding their infants’ internal experience: Relations with maternal sensitivity and infant attachment. Dev. Psychol. 2002, 38, 534. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.; Park, Y.J.; Kim, M.J. Predictors of maternal sensitivity during the early postpartum period. J. Adv. Nurs. 2006, 55, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Mesman, J.; Emmen, R.A. Mary Ainsworth’s legacy: A systematic review of observational instruments measuring parental sensitivity. Attach. Hum. Dev. 2013, 15, 485–506. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.; Park, Y.J.; Ryu, H.; Seomun, G.A. Maternal sensitivity: A concept analysis. J. Adv. Nurs. 2008, 64, 304–314. [Google Scholar] [CrossRef] [PubMed]
- Rothbart, M.K. Becoming Who We Are: Temperament and Personality in Development; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Rothbart, M.K. Longitudinal observation of infant temperament. Dev. Psychol. 1986, 22, 356. [Google Scholar] [CrossRef]
- Kaitz, M.; Levy, M.; Ebstein, R.; Faraone, S.V.; Mankuta, D. The intergenerational effects of trauma from terror: A real possibility. Infant Ment. Health J. 2009, 30, 158–179. [Google Scholar] [CrossRef] [PubMed]
- Aubuchon-Endsley, N.; Gee, B.; Devine, N.; Ramsdell-Hudock, H.; Swann, H.; Brumley, M.R. A cohort study of relations among caregiver-infant co-occupation and reciprocity. OTRJ Occup. Particip. Health 2020, 40, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Brand, S.R.; Engel, S.M.; Canfield, R.L.; Yehuda, R. The effect of maternal PTSD following in utero trauma exposure on behavior and temperament in the 9-month-old infant. Ann. N. Y. Acad. Sci. 2006, 1071, 454–458. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Hooper, L.M.; Stockton, P.; Krupnick, J.L.; Green, B.L. Development, use, and psychometric properties of the Trauma History Questionnaire. J. Loss Trauma 2011, 16, 258–283. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53. [Google Scholar] [CrossRef]
- Bengtson, L.; Aubuchon-Endsley, N. Prenatal depression moderates the relationship between maternal trauma exposure and cortisol production and predicts breastfeeding behavior. Women Health 2023, 63, 334–345. [Google Scholar] [CrossRef]
- Mangold International GmbH. Mangold [INTERACT Lab Suite Software], Version 2017; Mangold International GmbH: Arnstorf, Germany, 2017. Available online: www.mangold-international.com (accessed on 17 October 2019).
- Putnam, S.P.; Helbig, A.L.; Gartstein, M.A.; Rothbart, M.K.; Leerkes, E. Development and assessment of short and very short forms of the Infant Behavior Questionnaire–Revised. J. Pers. Assess. 2014, 96, 445–458. [Google Scholar] [CrossRef]
- Sarason, I.G.; Sarason, B.R.; Shearin, E.N.; Pierce, G.R. A brief measure of social support: Practical and theoretical implications. J. Soc. Pers. Relat. 1987, 4, 497–510. [Google Scholar] [CrossRef]
- Maas, A.J.B.; de Cock, E.S.; Vreeswijk, C.M.; Vingerhoets, A.J.; van Bakel, H.J. A longitudinal study on the maternal–fetal relationship and postnatal maternal sensitivity. J. Reprod. Infant Psychol. 2015, 34, 110–121. [Google Scholar] [CrossRef]
- Neuhauser, A. Predictors of maternal sensitivity in at-risk families. Early Child Dev. Care 2016, 188, 126–142. [Google Scholar] [CrossRef]
- Hardner, K.; Wolf, M.R.; Rinfrette, E.S. Examining the relationship between higher educational attainment, trauma symptoms, and internalizing behaviors in child sexual abuse survivors. Child Abuse Negl. 2017, 86, 375–383. [Google Scholar] [CrossRef]
- Polimanti, R.; Ratanatharathorn, A.; Maihofer, A.X.; Choi, K.W.; Stein, M.B.; Morey, R.A.; Gelernter, J. Association of economic status and educational attainment with posttraumatic stress disorder: A mendelian randomization study. JAMA Netw. Open 2019, 2, e193447. [Google Scholar] [CrossRef] [PubMed]
- Jansen, P.W.; Raat, H.; Mackenbach, J.P.; Jaddoe, V.W.; Hofman, A.; Verhulst, F.C.; Tiemeier, H. Socioeconomic inequalities in infant temperament. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.; Weakliem, D.L.; August, B. Hollingshead’s “Four Factor Index of Social Status”: From unpublished paper to citation classic. Yale J. Sociol. 2011, 8, 11–17. [Google Scholar]
- Hollingshead, A.B. Four factor index of social status. Yale J. Sociol. 1975, 8, 21–53. [Google Scholar]
- Duncan, G.J.; Magnuson, K.A. Off with Hollingshead: Socioeconomic resources, parenting, and child development. In Socioeconomic Status, Parenting, and Child Development; Bornstein, M.H., Bradley, R.H., Eds.; Routledge: New York, NY, USA, 2001; pp. 123–126. [Google Scholar]
- Huang, Z.H.; Hou, C.L.; Huang, Y.H.; He, X.Y.; Wang, Q.W.; Chen, X.; Jia, F.J. Individuals at high risk for psychosis experience more childhood trauma, life events and social support deficit in comparison to healthy controls. Psychiatry Res. 2019, 273, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Sjögren, E.; Leanderson, P.; Kristenson, M. Diurnal saliva cortisol levels and relations to psychosocial factors in a population sample of middle-aged Swedish men and women. Int. J. Behav. Med. 2006, 13, 193–200. [Google Scholar] [CrossRef]
- Enlow, M.B.; Devick, K.L.; Brunst, K.J.; Lipton, L.R.; Coull, B.A.; Wright, R.J. Maternal lifetime trauma exposure, prenatal cortisol, and infant negative affectivity. Infancy 2017, 22, 492–513. [Google Scholar] [CrossRef]
- Van den Bergh, B.R.; van den Heuvel, M.I.; Lahti, M.; Braeken, M.; de Rooij, S.R.; Entringer, S.; King, S. Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neurosci. Biobehav. Rev. 2017, 117, 26–64. [Google Scholar] [CrossRef]
- Braithwaite, E.C.; Pickles, A.; Sharp, H.; Glover, V.; O’Donnell, K.J.; Tibu, F.; Hill, J. Maternal prenatal cortisol predicts infant negative emotionality in a sex-dependent manner. Physiol. Behav. 2017, 175, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Sandman, C.A.; Glynn, L.M.; Davis, E.P. Is there a viability–vulnerability tradeoff? Sex differences in fetal programming. J. Psychosom. Res. 2013, 75, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Macaulay, S.; Buchmann, E.J.; Dunger, D.B.; Norris, S.A. Reliability and validity of last menstrual period for gestational age estimation in a low-to-middle-income setting. J. Obstet. Gynaecol. Res. 2019, 45, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, R.E.; Ahmed, A.N.U.; Ahmed, S.; Saha, S.K.; Chowdhury, M.A.; Black, R.E.; Darmstadt, G.L. Determining gestational age in a low-resource setting: Validity of last menstrual period. J. Health Popul. Nutr. 2009, 27, 332. [Google Scholar] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; 12 Lawrence Erlbaum Associates Inc.: Hillsdale, NJ, USA, 1988; Volume 13. [Google Scholar]
- Fritz, M.S.; MacKinnon, D.P. Required sample size to detect the mediated effect. Psychol. Sci. 2007, 18, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Resnick, H.S.; Kilpatrick, D.G.; Dansky, B.S.; Saunders, B.E.; Best, C.L. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J. Consult. Clin. Psychol 1993, 61, 984. [Google Scholar] [CrossRef] [PubMed]
- Ning, J.; Tang, X.; Shi, H.; Yao, D.; Zhao, Z.; Li, J. Social support and posttraumatic growth: A meta-analysis. J. Affect. Disord. 2023, 320, 117–132. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.C.; Letourneau, N.; Campbell, T.S.; Tomfohr-Madsen, L.; Giesbrecht, G.F. Developmental origins of infant emotion regulation: Mediation by temperamental negativity and moderation by maternal sensitivity. Dev. Psychol. 2017, 53, 611. [Google Scholar] [CrossRef]
- Cook, J.M.; Elhai, J.D.; Cassidy, E.L.; Ruzek, J.I.; Ram, G.D.; Sheikh, J.I. Assessment of trauma exposure and post-traumatic stress in long-term care veterans: Preliminary data on psychometrics and post-traumatic stress disorder prevalence. Mil. Med. 2005, 170, 862–866. [Google Scholar] [CrossRef]
- Ford, J.D. Polyvictimization and developmental trauma in childhood. Eur. J. Psychotraumatol. 2021, 12 (Suppl. S1), 1866394. [Google Scholar] [CrossRef]
- Masten, A.S.; Wright, M.O.D. Cumulative risk and protection models of child maltreatment. J. Aggress. Maltreat. Trauma 1998, 2, 7–30. [Google Scholar] [CrossRef]
- Yehuda, R.; Engel, S.M.; Brand, S.R.; Seckl, J.; Marcus, S.M.; Berkowitz, G.S. Transgenerational effects of posttraumatic stress disorder in babies of mothers exposed to the World Trade Center attacks during pregnancy. J. Clin. Endocrinol. Metab. 2005, 90, 4115–4118. [Google Scholar] [CrossRef]
- Bublitz, M.H.; Stroud, L.R. Childhood sexual abuse is associated with cortisol awakening response over pregnancy: Preliminary findings. Psychoneuroendocrinology 2012, 37, 1425–1430. [Google Scholar] [CrossRef]
- Finegood, E.D.; Blair, C.; Granger, D.A.; Hibel, L.C.; Mills-Koonce, R. Psychobiological influences on maternal sensitivity in the context of adversity. Dev. Psychol. 2016, 52, 1073. [Google Scholar] [CrossRef]
- Crockenberg, S.C.; Leerkes, E.M. Infant and maternal behavior moderate reactivity to novelty to predict anxious behavior at 2.5 years. Dev. Psychopathol. 2006, 18, 17. [Google Scholar] [CrossRef]

| Model | Maternal Sensitivity (M) | Maternal Trauma (X) | Infant Temperament (Y) |
|---|---|---|---|
| Hypothesis 1a | Total Frequency | Past Year Impairment | Surgency/Reactivity |
| Hypothesis 1b | Total Frequency | Exposure | Surgency/Reactivity |
| Hypothesis 2a | Total Frequency | Past Year Impairment | Negative Affectivity |
| Hypothesis 2b | Total Frequency | Exposure | Negative Affectivity |
| Hypothesis 3a | Total Frequency | Past Year Impairment | Regulation/Orienting |
| Hypothesis 3b | Total Frequency | Exposure | Regulation/Orienting |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hambleton, J.L.; Aubuchon-Endsley, N.L.; Kurien, J. Associations among Maternal Trauma History, Postnatal Maternal Sensitivity, and Infant Temperament. Children 2024, 11, 301. https://doi.org/10.3390/children11030301
Hambleton JL, Aubuchon-Endsley NL, Kurien J. Associations among Maternal Trauma History, Postnatal Maternal Sensitivity, and Infant Temperament. Children. 2024; 11(3):301. https://doi.org/10.3390/children11030301
Chicago/Turabian StyleHambleton, Jennifer Lynn, Nicki Lynn Aubuchon-Endsley, and Jasmin Kurien. 2024. "Associations among Maternal Trauma History, Postnatal Maternal Sensitivity, and Infant Temperament" Children 11, no. 3: 301. https://doi.org/10.3390/children11030301
APA StyleHambleton, J. L., Aubuchon-Endsley, N. L., & Kurien, J. (2024). Associations among Maternal Trauma History, Postnatal Maternal Sensitivity, and Infant Temperament. Children, 11(3), 301. https://doi.org/10.3390/children11030301







