Perceptions and Expectations of Youth Regarding the Respect for Their Rights in the Hospital
Abstract
1. Introduction
2. Materials and Methods
- the gross description of the content, along with details about colors, drawing size, and relationships between people;
- the assessment of basic and social emotions (i.e., fear, sadness, anger, embarrassment, shame, shyness) and the emotions felt when they moved to the level of representation and imagined their ideal hospital (i.e., joy, surprise/security). Finally, drawings with similar categorized emotions were grouped together.
3. Results
3.1. Age-Specific Assessment Tools
3.1.1. Tool Questionnaire for Children Aged 6–11 Years
3.1.2. Tool Questionnaire for Children Aged 12–18 Years
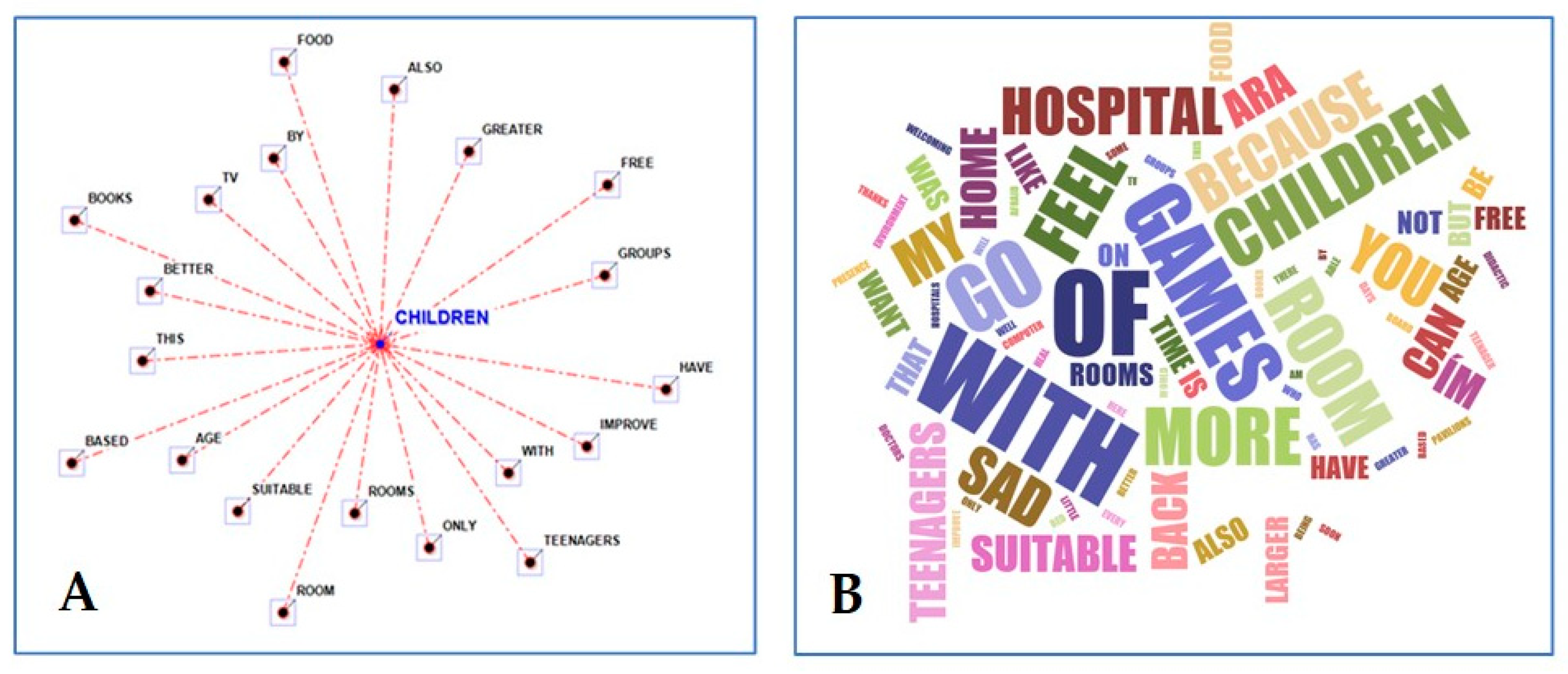
3.2. Open Questions
3.3. Drawings Analysis
3.4. Narrative Content Analysis
4. Discussion
5. Conclusions and Study Implications
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Busch, I.M.; Moretti, F.; Travaini, G.; Wu, A.W.; Rimondini, M. Humanization of Care: Key Elements Identified by Patients, Caregivers, and Healthcare Providers. A Systematic Review. Patient 2019, 12, 461–474. [Google Scholar] [CrossRef] [PubMed]
- Borbasi, S.; Galvin, K.T.; Adams, T.; Todres, L.; Farrelly, B. Demonstration of the Usefulness of a Theoretical Framework for Humanising Care with Reference to a Residential Aged Care Service in Australia. J. Clin. Nurs. 2013, 22, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Tripodi, M.; Siano, M.A.; Mandato, C.; De Anseris, A.G.E.; Quitadamo, P.; Guercio Nuzio, S.; Viggiano, C.; Fasolino, F.; Bellopede, A.; Annunziata, M.; et al. Humanization of Pediatric Care in the World: Focus and Review of Existing Models and Measurement Tools. Ital. J. Pediatr. 2017, 43, 76. [Google Scholar] [CrossRef]
- Borghi, C.A.; Szylit, R.; Ichikawa, C.R.D.F.; Baliza, M.F.; Camara, U.T.J.; Frizzo, H.C.F. Use of Social Networking Websites as a Care Instrument for Hospitalized Adolescents. Esc. Anna Nery 2017, 22, e20170159. [Google Scholar] [CrossRef][Green Version]
- Marin, M.J.S.; Storniolo, L.V.; Moravcik, M.Y. Humanization of Care from the Perspective of the Family Health Strategy Teams in a City in the Interior of São Paulo, Brazil. Rev. Lat.-Am. Enferm. 2010, 18, 763–769. [Google Scholar] [CrossRef]
- UN-Declaration-Rights-Child UNCR. Available online: https://www.unicef.org/child-rights-convention/convention-text-childrens-version (accessed on 28 January 2024).
- Runeson, I.; Hallström, I.; Elander, G.; Hermerén, G. Children’s Needs during Hospitalization: An Observational Study of Hospitalized Boys. Int. J. Nurs. Pract. 2002, 8, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Lambert, V.; Glacken, M.; McCarron, M. Meeting the Information Needs of Children in Hospital. J. Child. Health Care 2013, 17, 338–353. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.E.; Megel, M.E.; Enenbach, L.; Carlson, K.L. The Voices of Children: Stories About Hospitalization. J. Pediatr. Health Care 2010, 24, 95–102. [Google Scholar] [CrossRef]
- Coyne, I.; Kirwan, L. Ascertaining Children’s Wishes and Feelings about Hospital Life. J. Child. Health Care 2012, 16, 293–304. [Google Scholar] [CrossRef]
- Silva, C.D.C.; Ribeiro, N.R.R. Percepções Da Criança Acerca do Cuidado Recebido Durante a Hospitalização. Rev. Bras. Enferm. 2000, 53, 311–323. [Google Scholar] [CrossRef]
- UNICEF. Convention on the Rights of the Child. Available online: https://www.unicef.org/child-rights-convention (accessed on 28 January 2024).
- Koukourikos, K.; Tzeha, L.; Pantelidou, P.; Tsaloglidou, A. The Importance of Play during Hospitalization of Children. Mater. Sociomed. 2015, 27, 438. [Google Scholar] [CrossRef]
- Dasso, N.; Catania, G.; Zanini, M.; Rossi, S.; Aleo, G.; Signori, A.; Scelsi, S.; Petralia, P.; Watson, R.; Hayter, M.; et al. Informal Carers’ Experiences with Their Children’s Care during Hospitalization in Italy: Child HCAHPS Results from RN4CAST@IT-Ped Cross-Sectional Study. J. Pediatr. Nurs. 2024, 74, 10–16. [Google Scholar] [CrossRef]
- Foster, M.; Whitehead, L.; Arabiat, D. Development and Validation of the Needs of Children Questionnaire: An Instrument to Measure Children’s Self-reported Needs in Hospital. J. Adv. Nurs. 2019, 75, 2246–2258. [Google Scholar] [CrossRef] [PubMed]
- Hargreaves, D.S.; Sizmur, S.; Pitchforth, J.; Tallett, A.; Toomey, S.L.; Hopwood, B.; Schuster, M.A.; Viner, R.M. Children and Young People’s versus Parents’ Responses in an English National Inpatient Survey. Arch. Dis. Child. 2018, 103, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Mandato, C.; Siano, M.A.; De Anseris, A.G.E.; Tripodi, M.; Massa, G.; De Rosa, R.; Buffoli, M.; Lamanna, A.; Siani, P.; Vajro, P. Humanization of Care in Pediatric Wards: Differences between Perceptions of Users and Staff According to Department Type. Ital. J. Pediatr. 2020, 46, 65. [Google Scholar] [CrossRef]
- Pelander, T.; Lehtonen, K.; Leino-Kilpi, H. Children in the hospital: Elements of quality in drawings. J. Pediatr. Nurs. 2007, 22, 333–341. [Google Scholar] [CrossRef]
- Cannoni, E. Il Disegno dei Bambini, 1st ed.; Le bussole Psicologia; Carocci: Roma, Italy, 2003; ISBN 978-88-430-2644-9. [Google Scholar]
- Jolley, R.P. Children and Pictures: Drawing and Understanding; Wiley-Blackwell: Malden, MA, USA, 2010; ISBN 978-1-4051-0543-9. [Google Scholar]
- Guerreiro Fernandes, A.I.; Kuttumuratova, A.; Monolbaev, K.; Boderscova, L.; Pirova, Z.; Weber, M.W. Assessing and Improving Children’s Rights in Hospitals: Case Studies from Kyrgyzstan, Tajikistan, and Moldova. Health Hum. Rights 2016, 18, 235–248. [Google Scholar]
- International Network of Health Promoting Hospitals, and Health Services. Task Force on Health Promotion for Children and Adolescents in & by Hospitals (HPH-CA). In Self-Evaluation Model and Tool on the Respect of Children’s Rights in Hospital, 1st ed.; Editors Simonelli F and Fernandes Guerreiro AI: Florence, Italy, 2009. [Google Scholar]
- Fernandes Guerreiro, A.I. Manual and Tools for the Assessment and Improvement of Children’s Rights in Hospitals. March 2012. Available online: https://www.hphnet.org/wp-content/uploads/2021/02/Childrens-rights-in-Hospital-and-Health-Services-assessment-t.pdf (accessed on 28 January 2024).
- The International Network of Health Promoting Hospitals & Health Services. 2024. Available online: https://www.hphnet.org/about-us/#content-network (accessed on 28 January 2024).
- United Nation Convention on the Rights of the Child. Available online: https://www.ohchr.org/en/instruments-mechanisms/instruments/convention-rights-child (accessed on 28 January 2024).
- Guerreiro Fernandes, A.I.; Kuttumuratova, A.; Babamuradova, M.; Atajanova, Z.; Weber, M.W.; WHO. Assessment and Improvement of Children’s Rights in Health Care: Piloting Training and Tools in Uzbekistan. Public Health Panor. 2015, 1, 241–245. [Google Scholar]
- Fernandes Guerreiro, A.I. (International Network of Health Promotion Hospitals and Health Services (HPH), Taskforce on Children & Adolescents (HPH-CA), Trento, Italy and Independent Consultant on Children’s Rights in Health Care, Albufeira, Portugal.). Personal Communication, November 2016. [Google Scholar]
- Koppitz, E.M. Psychological Evaluation of Children’s Human Figure Drawings; Grune & Stratton: New York, NY, USA, 1968; ISBN 978-0-8089-0240-9. [Google Scholar]
- Zlateva, A. How to Read Children’s Drawings; University of Malta. Centre for Resilience & Socio-Emotional Health: Msida, Malta, 2019; ISBN 978-99957-890-4-6. [Google Scholar]
- Clatworthy, S.; Simon, K.; Tiedeman, M. Child Drawing: Hospital Manual. J. Pediatr. Nurs. 1999, 14, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Crotti, E.; Magni, A. Come Interpretare Gli Scarabocchi; Red ed.; Piccoli e Grandi Manuali: Como, Italy, 1996; ISBN 978-88-7031-546-2. [Google Scholar]
- Carlino Bandinelli, A.; Manes, S. Il Disegno del Bambino in Difficoltà: Guida All’interpretazione dei Test della Figura Umana, della Famiglia, Dell’albero e della Casa; Strumenti per il Lavoro Psico-Sociale ed Educativo; Angeli: Milano, Italy, 2004; ISBN 978-88-464-5735-6. [Google Scholar]
- TLAB—A Comprehensive and Easy-to-Use Software for Text Analysis and Text Mining. Available online: www.tlab.it (accessed on 28 January 2024).
- Coyne, I. Consultation with Children in Hospital: Children, Parents’ and Nurses’ Perspectives. J. Clin. Nurs. 2006, 15, 61–71. [Google Scholar] [CrossRef]
- Bray, L.; Appleton, V.; Sharpe, A. ‘We Should Have Been Told What Would Happen’: Children’s and Parents’ Procedural Knowledge Levels and Information-Seeking Behaviours When Coming to Hospital for a Planned Procedure. J. Child. Health Care 2022, 26, 96–109. [Google Scholar] [CrossRef]
- Lapa, D.D.F.; Souza, T.V.D. A Percepção do Escolar Sobre a Hospitalização: Contribuições Para o Cuidado de Enfermagem. Rev. Esc. Enferm. USP 2011, 45, 811–817. [Google Scholar] [CrossRef][Green Version]
- Curtis, K.; Liabo, K.; Roberts, H.; Barker, M. Consulted but Not Heard: A Qualitative Study of Young People’s Views of Their Local Health Service. Health Expect. 2004, 7, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Coyne, I. Children’s Experiences of Hospitalization. J. Child. Health Care 2006, 10, 326–336. [Google Scholar] [CrossRef] [PubMed]
- Coyne, I.; Cowley, S. Challenging the Philosophy of Partnership with Parents: A Grounded Theory Study. Int. J. Nurs. Stud. 2007, 44, 893–904. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.E.; Megel, M.E.; Barton, P.H.; Bell, J.; Marget, A.; Ranck, S.; Schneiss-Protaskey, J.; Witcofski, E.; Wolf, L. Revision and Psychometric Testing of the Barton Hospital Picture Test. J. Pediatr. Nurs. 2007, 22, 206–214. [Google Scholar] [CrossRef] [PubMed]
- Bellack, J.P.; Fleming, J.W. The Use of Projective Techniques in Pediatric Nursing Research from 1984 to 1993. J. Pediatr. Nurs. 1996, 11, 10–28. [Google Scholar] [CrossRef] [PubMed]
- Forsner, M.; Jansson, L.; Sørlie, V. The Experience of Being Ill as Narrated by Hospitalized Children Aged 7–10 Years with Short-Term Illness. J. Child. Health Care 2005, 9, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Bull, A.; Gillies, M. Spiritual Needs of Children with Complex Healthcare Needs in Hospital. Paediatr. Care 2007, 19, 34–38. [Google Scholar] [CrossRef]
- Pelander, T.; Leino-Kilpi, H. Quality In Pediatric Nursing Care: Children’s Expectations. Issues Compr. Pediatr. Nurs. 2004, 27, 139–151. [Google Scholar] [CrossRef]
- Noreña Peña, A.L.; Cibanal Juan, L. The Experience of Hospitalized Children Regarding Their Interactions with Nursing Professionals. Rev. Lat.-Am. Enferm. 2011, 19, 1429–1436. [Google Scholar] [CrossRef] [PubMed]
- Lindeke, L.; Nakai, M.; Johnson, L. Capturing Children’s Voices for Quality Improvement. MCN Am. J. Matern./Child. Nurs. 2006, 31, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.S.; Jackson, K.; Kolbæk, R.; Glasdam, S. Children’s Experiences of Acute Hospitalisation to a Paediatric Emergency and Assessment Unit—A Qualitative Study. J. Child. Health Care 2012, 16, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Karisalmi, N.; Mäenpää, K.; Kaipio, J.; Lahdenne, P. Measuring Patient Experiences in a Children’s Hospital with a Medical Clowning Intervention: A Case-Control Study. BMC Health Serv. Res. 2020, 20, 360. [Google Scholar] [CrossRef] [PubMed]
- Carley, K. Coding Choices for Textual Analysis: A Comparison of Content Analysis and Map Analysis. Sociol. Methodol. 1993, 23, 75. [Google Scholar] [CrossRef]
- Rollins, J.A. Tell Me About It: Drawing as a Communication Tool for Children with Cancer. J. Pediatr. Oncol. Nurs. 2005, 22, 203–221. [Google Scholar] [CrossRef]
- Rubin, J.A. Child Art Therapy: Understanding and Helping Children Grow through Art, 2nd ed.; Van Nostrand Reinhold: New York, NY, USA, 1984; ISBN 978-0-442-27767-3. [Google Scholar]
- Massimo, L.M.; Zarri, D.A. In Tribute to Luigi Castagnetta—Drawings: A Narrative Approach for Children with Cancer. Ann. N. Y. Acad. Sci. 2006, 1089, xvi–xxiii. [Google Scholar] [CrossRef]
- Woodgate, R.L.; West, C.H.; Tailor, K. Existential Anxiety and Growth: An Exploration of Computerized Drawings and Perspectives of Children and Adolescents with Cancer. Cancer Nurs. 2014, 37, 146–159. [Google Scholar] [CrossRef]
- Curtis, P.; Northcott, A. The Impact of Single and Shared Rooms on Family-centred Care in Children’s Hospitals. J. Clin. Nurs. 2017, 26, 1584–1596. [Google Scholar] [CrossRef] [PubMed]
- Farokhi, M.; Hashemi, M. The Analysis of Children’s Drawings: Social, Emotional, Physical, and Psychological Aspects. Procedia-Sociol. Behav. Sci. 2011, 30, 2219–2224. [Google Scholar] [CrossRef]
- Cassemiro, L.K.D.D.S.; Okido, A.C.C.; Furtado, M.C.D.C.; Lima, R.A.G.D. The Hospital Designed by Hospitalized Children and Adolescents. Rev. Bras. Enferm. 2020, 73, e20190399. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, M.; Kilkelly, U. The Child’s Right to Be Heard in the Healthcare Setting: Perspectives of Children, Parents and Health Professionals; Office of the Minister for Children: Dublin, Ireland, 2006. [Google Scholar]
- Associazione Ospedali Pediatrici Italiani. Available online: https://www.aopi.it (accessed on 28 January 2024).
- Badarau, D.O.; De Clercq, E.; Wangmo, T.; Dragomir, M.; Miron, I.; Kühne, T.; Elger, B.S. Cancer Care in Romania: Challenges and Pitfalls of Children’s and Adolescents’ Multifaceted Involvement. J. Med. Ethics 2016, 42, 757–761. [Google Scholar] [CrossRef] [PubMed]
- Haiat, H.; Bar-Mor, G.; Shochat, M. The World of the Child: A World of Play Even in the Hospital. J. Pediatr. Nurs. 2003, 18, 209–214. [Google Scholar] [CrossRef] [PubMed]




| 6–11 Years (n = 350) | 12–18 Years (n = 350) | |
|---|---|---|
| Main clinical diagnoses | acute diarrhea, asthma, febrile seizure, salmonella gastroenteritis, bronchitis, pneumonia, urinary tract infection, otitis media, viral illness, purpura | acute and chronic diarrhea, pneumonia, bronchitis, otitis media, trauma, urinary tract infection, eating disorder, febrile viral illness, infectious mononucleosis. |
| Hospital stay duration before interview | 5 ± 3 days | 6 ± 1 days |
| Question | % Yes µ (± SD) | % No µ (± SD) | % N.A. µ (± SD) |
|---|---|---|---|
| 1. Can you please let us know how your stay in hospital was for you? | 100 (±0) | 0 (±0) | 0 (±0) |
| 2. Did you play while you were in hospital? | 85.8 (±8.2) | 14.2 (±8.2) | 0 (±0) |
| 3. Who did you play with? *** | |||
| 4. Did you have the opportunity of going to school in the hospital? | 25.7 (±21.1) | 73.6 (±21.8) | 0.7 (±1.3) |
| 5. Do you like the school in the hospital? | 20.7 (±17.3) | 3.9 (±5.8) | 75.4 (±19.1) |
| 6. Did anyone tell you why you came to hospital? | 84.4 (±15.3) | 15.6 (±15.3) | 0 (±0) |
| 7. Did the doctor explain why you were hurting/what was wrong with you? | 65.7 (±25.3) | 33.3 (±25.5) | 1 (±1.5) |
| 8. Did you understand what s/he said? | 63.3 (±15.2) | 22.3 (±10.5) | 14.4 (±13.5) |
| 9. Did someone tell you how you can get better? | 79.6 (±13.4) | 16.3 (±10.9) | 4.1 (±8.8) |
| 10. Do you feel comfortable saying if something is making you unhappy in the hospital? | 61.7 (±21.3) | 36 (±21.4) | 2.3 (±4.1) |
| 11. Do you know who to talk to if you are not happy in the hospital? | 86.9 (±16.3) | 12.9 (±15.6) | 0.2 (±0.8) |
| 12. Were your parents always with you during your stay in hospital? | 99 (±1.3) | 1 (±1.3) | 0 (±0) |
| 13. Did your parents stay in the hospital overnight? | 100 (±0) | 0 (±0) | 0 (±0) |
| 14. Have you felt pain while you were in the hospital? | 65.1 (±24) | 34.9 (±24) | 0 (±0) |
| 15. Did anyone ask you if you were feeling pain? | 84.4 (±13.4) | 15.3 (±12.3) | 0.3 (±0.8) |
| 16. Did anyone try to make the pain better? | 79.4 (±17.1) | 13.6 (±13.7) | 7 (±5.5) |
| Total Rights | 73.6 (±24.1) | 19.6 (±19,1) | 6.7 (±2.4) |
| STANDARD | % Yes µ (± SD) | % No µ (± SD) | % N.A. µ (± SD) |
|---|---|---|---|
| 1: Quality services for children | 63.40 (±8.05) | 28.54 (±5.35) | 8.06 (±5.19) |
| 2: Equality and non-discrimination | 55.71 (±7.92) | 17.61 (±8.32) | 26.68 (±6.69) |
| 3: Play and learning | 44.04 (±12.66) | 39.55 (±9.79) | 16.41 (±7.35) |
| 4: Information and participation | 57.36 (±8.91) | 32.55 (±9.70) | 10.09 (±5.66) |
| 5: Safety and environment | 76.00 (±8.68) | 11.96 (±5.64) | 12.04 (±5.66) |
| 6: Pain management & palliative care | 76.79 (±9.89) | 16.43 (±6.85) | 6.79 (±4.05) |
| (A) | |||||
| POSITIVE THINGS | % µ (±SD) | NEGATIVE THINGS | % µ (±SD) | IMPROVE/ IDEAL | % µ (±SD) |
| Hospital staff expertise | 65.14 (±13.10) | Sanitary facilities | 29 (±17.8) | Environment comfort | 36 (±10.84) |
| Playroom | 31.5 (±2.12) | Food | 45 (±10.8) | Entertainment/leisure | 43.16 (±20.30) |
| I do not know | 23.16 (±13.69) | I do not know | 48.33 (±14.43) | Hygiene | 19.5 (±11.44) |
| Food | 21.66 (±20.82) | ||||
| (B) | |||||
| POSITIVE THINGS | % µ (±SD) | NEGATIVE THINGS | % µ (±SD) | IMPROVE/ IDEAL | % µ (±SD) |
| Hospital staff expertise | 49.86 (±10.2) | Sanitary facilities | 19.83 (±8.25) | Environmental comfort | 23.33 (±5.77) |
| Reception | 22.5 (±3.53) | Food | 28.2 (±13.64) | Entertainment/leisure | 36.6 (±23.09) |
| Environmental comfort | 6.3 (±3.05) | Hygiene | 12.5 (±5) | ||
| Patient care | 4.5 (±0.70) | ||||
| Kindness/courtesy | 15.8 (±11.90) | ||||
| Quiet environment | 5 (±0) | ||||
| Playroom | 20 (±13.23) | ||||
| “State of Mind during Hospital Stay” | “Hospital I Would Like” [Ideal Hospital] | ||
|---|---|---|---|
| BASIC EMOTIONS | SOCIAL EMOTIONS | BASIC EMOTIONS | SOCIAL EMOTIONS |
| Fear (Figure 1B,C) | Embarrassment | Joy (Figure 2A–F) | Stability/Security (Figure 2C) |
| Sadness (Figure 1A,B) | Shame | Surprise | Welcome (Figure 2A) |
| Anger | Shyness | Trust (Figure 2D) | |
| Fluctuating (Figure 1D) | |||
| Colors | - Warm (Yellow, Orange, Pink, Red) - Cold (Black, Gray, Brown). |
| Drawing size | - It develops in height - It occupies only the lateral spaces of the sheet - It develops only in the lower and upper part of the sheet - Presence of curved lines - The drawing takes up all the space on the sheet |
| Size relationships between people | - Short and non-existent legs compared to the body - Triangular head and of different dimensions |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Rosa, R.; Siano, M.A.; Colucci, A.; De Anseris, A.G.E.; Siani, P.; Vajro, P.; Savarese, G.; Mandato, C. Perceptions and Expectations of Youth Regarding the Respect for Their Rights in the Hospital. Children 2024, 11, 222. https://doi.org/10.3390/children11020222
De Rosa R, Siano MA, Colucci A, De Anseris AGE, Siani P, Vajro P, Savarese G, Mandato C. Perceptions and Expectations of Youth Regarding the Respect for Their Rights in the Hospital. Children. 2024; 11(2):222. https://doi.org/10.3390/children11020222
Chicago/Turabian StyleDe Rosa, Roberta, Maria Anna Siano, Angelo Colucci, Anna Giulia Elena De Anseris, Paolo Siani, Pietro Vajro, Giulia Savarese, and Claudia Mandato. 2024. "Perceptions and Expectations of Youth Regarding the Respect for Their Rights in the Hospital" Children 11, no. 2: 222. https://doi.org/10.3390/children11020222
APA StyleDe Rosa, R., Siano, M. A., Colucci, A., De Anseris, A. G. E., Siani, P., Vajro, P., Savarese, G., & Mandato, C. (2024). Perceptions and Expectations of Youth Regarding the Respect for Their Rights in the Hospital. Children, 11(2), 222. https://doi.org/10.3390/children11020222








