Efficacy of Lower Limb Orthoses in the Rehabilitation of Children Affected by Cerebral Palsy: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria and Data Extraction
2.3. Quality Assessment, Risk of Bias, and Evidence Synthesis
3. Results
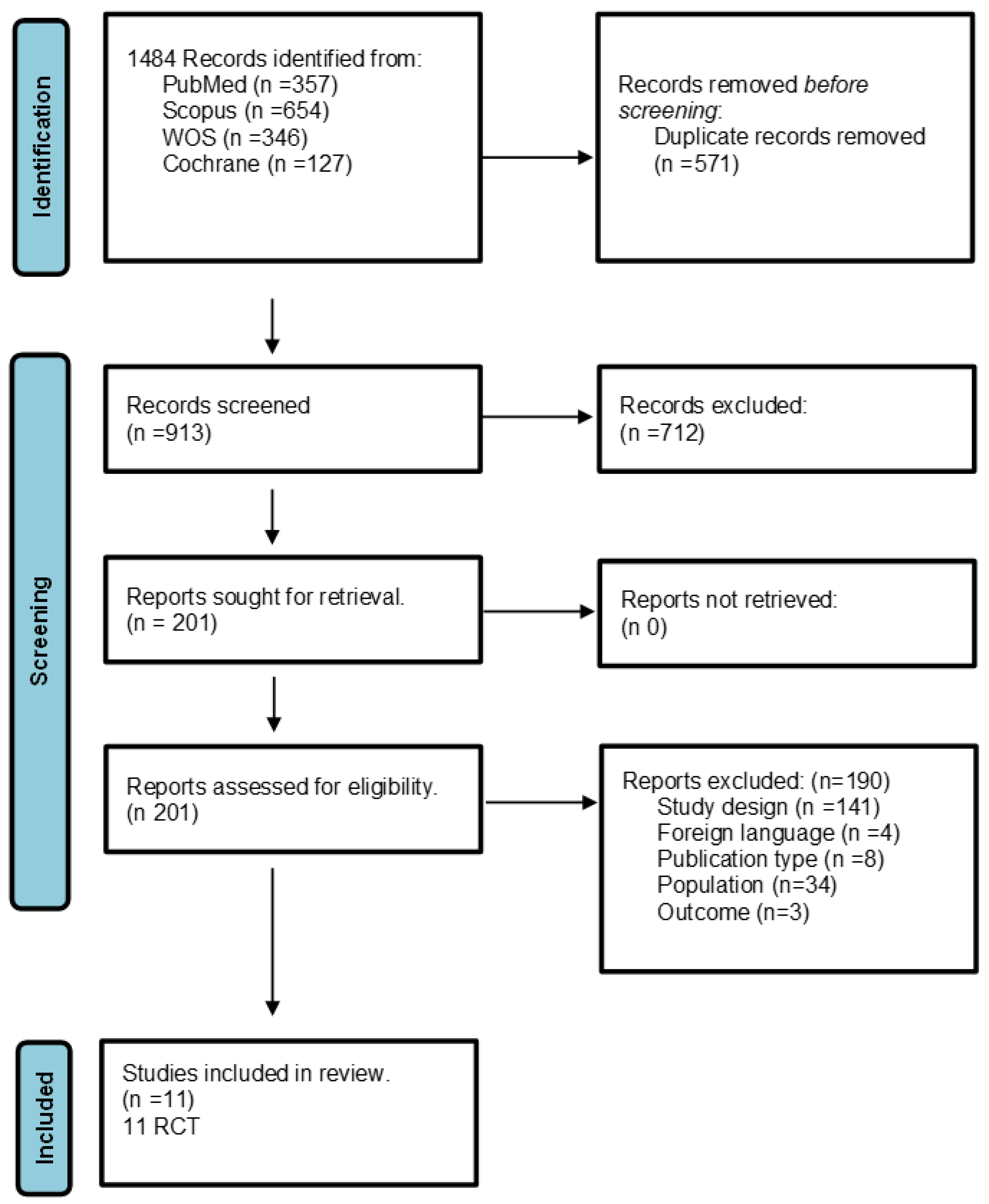
3.1. Study Selection
3.2. Study Characteristics
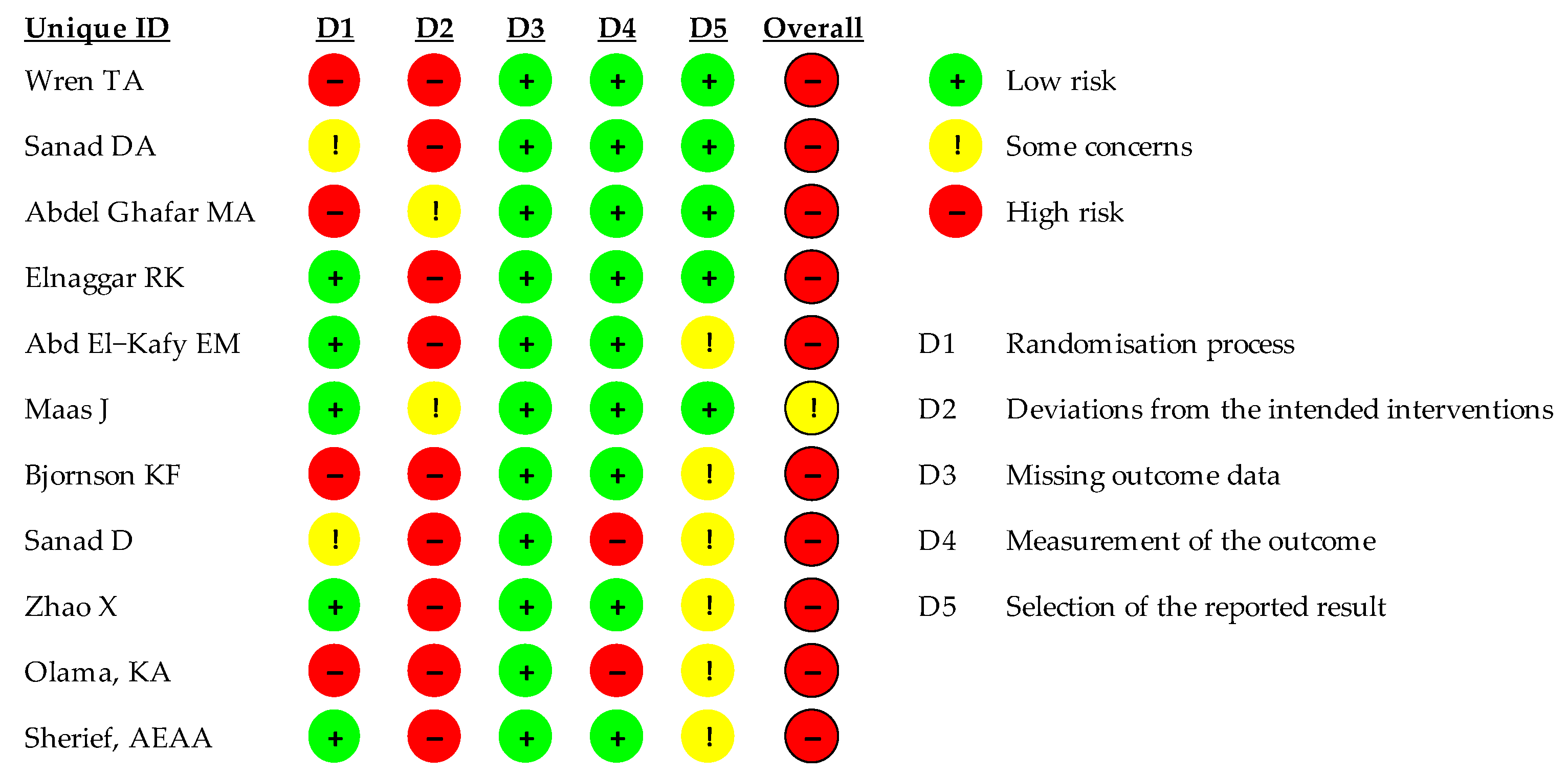
3.3. Quality of Included Studies
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Search Strategy
References
- Bax, M.; Goldstein, M.; Rosenbaum, P.; Leviton, A.; Paneth, N.; Dan, B.; Jacobsson, B.; Damiano, D. Executive Committee for the Definition of Cerebral Palsy. Proposed definition and classification of cerebral palsy, April 2005. Dev. Med. Child Neurol. 2005, 47, 571–576. [Google Scholar] [CrossRef]
- Vitrikas, K.; Dalton, H.; Breish, D. Cerebral Palsy: An Overview. Am. Fam. Physician 2020, 101, 213–220. [Google Scholar] [PubMed]
- Wimalasundera, N.; Stevenson, V.L. Cerebral palsy. Pract. Neurol. 2016, 16, 184–194. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.; Bowers, R.; Ross, K.; Stevens, P.; Phillips, D. Orthotic management of cerebral palsy: Recommendations from a consensus conference. NeuroRehabilitation 2011, 28, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Aboutorabi, A.; Arazpour, M.; Ahmadi Bani, M.; Saeedi, H.; Head, J.S. Efficacy of ankle foot orthoses types on walking in children with cerebral palsy: A systematic review. Ann. Phys. Rehabil. Med. 2017, 60, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Brehm, M.-A.; Harlaar, J.; Schwartz, M. Effect of ankle-foot orthoses on walking efficiency and gait in children with cerebral palsy. J. Rehabil. Med. 2008, 40, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Balaban, B.; Yasar, E.; Dal, U.; Yazicioglu, K.; Mohur, H.; Kalyon, T.A. The effect of hinged ankle-foot orthosis on gait and energy expenditure in spastic hemiplegic cerebral palsy. Disabil. Rehabil. 2007, 29, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Dalvand, H.; Dehghan, L.; Feizi, A.; Hosseini, S.A.; Amirsalari, S. The impacts of hinged and solid ankle-foot orthoses on standing and walking in children with spastic diplegia. Iran. J. Child. Neurol. 2013, 7, 12–19. [Google Scholar]
- Wren, T.A.; Dryden, J.W.; Mueske, N.M.; Dennis, S.W.; Healy, B.S.; Rethlefsen, S.A. Comparison of 2 orthotic approaches in children with cerebral palsy. Pediatr. Phys. Ther. 2015, 27, 218–226. [Google Scholar] [CrossRef]
- Ofluoğlu, D. Beyin felcinde ortez uygulamalari [Orthotic management in cerebral palsy]. Acta Orthop. Traumatol. Turc. 2009, 43, 165–172. (In Turkish) [Google Scholar] [CrossRef]
- Firouzeh, P.; Sonnenberg, L.K.; Morris, C.; Pritchard-Wiart, L. Ankle foot orthoses for young children with cerebral palsy: A scoping review. Disabil. Rehabil. 2021, 43, 726–738. [Google Scholar] [CrossRef]
- Autti-Rämö, I.; Suoranta, J.; Anttila, H.; Malmivaara, A.; Mäkelä, M. Effectiveness of upper and lower limb casting and orthoses in children with cerebral palsy: An overview of review articles. Am. J. Phys. Med. Rehabil. 2006, 85, 89–103. [Google Scholar] [CrossRef]
- Demont, A.; Gedda, M.; Lager, C.; de Lattre, C.; Gary, Y.; Keroulle, E.; Feuillerat, B.; Caudan, H.; Sancelme, Z.; Isapof, A.; et al. Evidence-Based, Implementable Motor Rehabilitation Guidelines for Individuals with Cerebral Palsy. Neurology 2022, 99, 283–297. [Google Scholar] [CrossRef]
- Wright, E.; DiBello, S.A. Principles of Ankle-Foot Orthosis Prescription in Ambulatory Bilateral Cerebral Palsy. Phys. Med. Rehabil. Clin. N. Am. 2020, 31, 69–89. [Google Scholar] [CrossRef] [PubMed]
- Tardieu, C.; Lespargot, A.; Tabary, C.; Bret, M.D. For how long must the soleus muscle be stretched each day to prevent contracture? Dev. Med. Child Neurol. 1988, 30, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Brown, D. A Review of the PubMed PICO Tool: Using Evidence-Based Practice in Health Education. Health Promot. Pract. 2020, 21, 496–498. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Abdel Ghafar, M.A.; Abdelraouf, O.R.; Abdel-Aziem, A.A.; Mousa, G.S.; Selim, A.O.; Mohamed, M.E. Combination taping technique versus ankle foot orthosis on improving gait parameters in spastic cerebral palsy: A controlled randomized study. J. Rehabil. Med. 2021, 53, jrm00240. [Google Scholar] [CrossRef] [PubMed]
- Elnaggar, R.K.; Abd-Elmonem, A.M. Effects of Radial Shockwave Therapy and Orthotics Applied with Physical Training on Motor Function of Children with Spastic Diplegia: A Randomized Trial. Phys. Occup. Ther. Pediatr. 2019, 39, 692–707. [Google Scholar] [CrossRef] [PubMed]
- Abd El-Kafy, E.M. The clinical impact of orthotic correction of lower limb rotational deformities in children with cerebral palsy: A randomized controlled trial. Clin. Rehabil. 2014, 28, 1004–1014. [Google Scholar] [CrossRef]
- Bjornson, K.F.; Schmale, G.A.; Adamczyk-Foster, A.; McLaughlin, J. The effect of dynamic ankle foot orthoses on function in children with cerebral palsy. J. Pediatr. Orthop. 2006, 26, 773–776. [Google Scholar] [CrossRef] [PubMed]
- Sherief, A.E.A.A.; Abo Gazya, A.A.; Abd El Gafaar, M.A. Integrated effect of treadmill training combined with dynamic ankle foot orthosis on balance in children with hemiplegic cerebral palsy. Egypt. J. Med. Hum. Genet. 2015, 16, 173–179. [Google Scholar] [CrossRef]
- Sanad, D.A. Moderate effect of ankle foot orthosis versus ground reaction ankle foot orthosis on balance in children with diplegic cerebral palsy. Prosthet. Orthot. Int. 2022, 46, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Sanad, D.A.; Ayoub, H.; Abdelkader, A. Immediate effect of solid ankle foot orthosis versus ground reaction ankle foot orthosis on balance in children with spastic diplegia. Biosci. Res. 2018, 15, 2893–2898. [Google Scholar]
- Olama, K.A.; El-Din, S.M.N.; Ibrahem, M.B. Role of three side support ankle-foot orthosis in improving the balance in children with spastic diplegic cerebral palsy. Egypt. J. Med. Hum. Genet. 2013, 14, 77–85. [Google Scholar] [CrossRef][Green Version]
- Maas, J.; Dallmeijer, A.; Huijing, P.; Brunstrom-Hernandez, J.; van Kampen, P.; Bolster, E.; Dunn, C.; Herndon, K.; Jaspers, R.; Becher, J. A randomized controlled trial studying efficacy and tolerance of a knee-ankle-foot orthosis used to prevent equinus in children with spastic cerebral palsy. Clin. Rehabil. 2014, 28, 1025–1038. [Google Scholar] [CrossRef]
- Zhao, X.; Xiao, N.; Li, H.; Du, S. Day vs. day-night use of ankle-foot orthoses in young children with spastic diplegia: A randomized controlled study. Am. J. Phys. Med. Rehabil. 2013, 92, 905–911. [Google Scholar] [CrossRef]
| Patient, Population, or Problem | Intervention or Exposure | Comparison | Outcome |
|---|---|---|---|
| Children affected by CP | Orthosis use | Control group | Trunk control, balance, walking, prevention of muscle contractures, quality of life |
| Author and Year | Design and Aim | Population | Interventions | Outcome and Follow Up | Results |
|---|---|---|---|---|---|
| Wren 2015 [9] | RCT Comparison of two different kinds of orthoses in children affected by CP | 10 children affected by CP between 4 and 12 years of age with tiptoe walking or flexed knee deambulation | Participants wore DAFO and ADR-AFO for 4 weeks in a random order | StepWatch activity monitor, gait analysis, OPUS (Orthotics and Prosthetics Users’ Survey), PODCI (Pediatric Outcomes Data Collection Instruments) Barefoot evaluation at baseline, at 4 weeks, and at 8 weeks | Both orthoses improve step length, hip extension during the stance phase and foot dorsiflexion during the swing phase compared to barefoot evaluation. DAFO improves gait kinematics in the last stance phase and ADR-AFO improves gait kinematics during the initial swing phase. Parents preferred DAFOs since they were lighter and easier to use |
| Sanad 2022 [25] | RCT. AFO versus GRAFO for balance in diplegic CP children | 30 children between 6 and 9 years of age | First group (n 15): AFO and rehabilitation for 3 months Second group (n 15): GRAFO and rehabilitation for 3 months | Biodex balance system at baseline and after 3 months | GRAFO is significantly better than AFO in balance control |
| Abdel Ghafar 2021 [20] | Single-blind RCT neuromuscular taping versus AFO in gait parameters improvement | 39 children with spastic CP. Level l o ll GMF and hyperton 1 or 1+ on the Ashworth Scale | Control group (n 11) AFO treatment group (n 12) Taping group (n 13) | GAITRite System evaluation at baseline and after 4 weeks | Significant improvement in velocity, step length, and single support phase in both AFO and taping groups with respect to baseline |
| Elnaggar 2019 [21] | Single-blind RCT. Shock waves and orthoses therapy combined with physiotherapy in CP children with spastic diplegia | 53 children between 5 and 8 years of age with CP, diplegia, spasticity between 1 and 1+ in MAS, and level I or II in GMF | First group (n 18): rehabilitation and shock waves Second group (n 16): rehabilitation and orthoses Third group (n 19): rehabilitation, orthoses, and shock waves | EMG, ePediatric Balance Scale, 3D-motion capture system Evaluations at baseline and after 3 months | No significant differences in gait and balance improvement Significant improvement in spasticity reduction in the third group |
| Ehab Mohamed Abd El-Kafy 2014 [22] | RCT. Orthotics correction impact on lower limb deformity in children affected by CP | 57 children affected by CP that are 6 to 8 years of age | First group (n 18): rehabilitation with stance and gait exercises without orthoses Second group (n16): rehabilitation with stance and gait exercises with TheraTogs™ orthoses for both lower limbs Third group (n 17): rehabilitation with stance and gait exercises with TheraTogs™ orthoses and GRAFO Treatment length: 12 weeks | Gait analysis, ROM measurement in hip and knee rotation during stance phase, and gait parameters measurement (step length, velocity, cadence) Evalutaion before and after treatment | Combined use of GRAFO and TheraTogs™, during rehabilitation gives better results than rehabilitation without orthoses or with TheraTogs™ |
| Maas 2014 [28] | Single-blind RCT. Efficacy and tolerance of KAFO in clubfoot prevention in CP | Children of 4 to 16 years of age affected by CP are able to walk | First group (n 15): usual rehabilitation + KAFO night use one leg at a time for one year Second group (n 13): control group, usual rehabilitation, no KAFO | Digital inclinometer (for ROM in dorsiflexion measurement) together with a dynamometer, video recording of gait and knee, foot and ankle for ROM measurement during demabulation, GMFM Evaluations at baseline and at 3, 6, 9, and 12 months | No significant differnces. Kafo is not well tolerated during sleep |
| Bjorson 2006 [23] | RCT. DAFO efficacy on motricity | 23 children affected by CP between 12 months and 8 years of age having used DAFO for at least 4 h for one month | Two measurements one after the other with and without DAFO on the same day | GMFM-88-66 (crawling, kneeling down, standing, walking, running, jumping) | Significant increase in motricity |
| Sanad 2018 [26] | RCT. Immediate effect of SAFO vs. GRAFO on the balance of diplegic spastic children affected by CP | 30 children affected by CP, diplegia, and spasticity between 5 and 8 years of age | First group (n 15): SAFO wearing Second group (n 15): GRAFO wearing | Biodex balance Board barefoot and with orthoses | GRAFO is better than SAFO in balance improvement |
| Zhao 2013 [29] | Single-blind RCT. Day use vs. day and night use of AFO in spastic diplegic CP children | 112 spastic diplegic CP children | First group (n 53): daily AFO Second group (n 52): AFO night and day Both groups performed the usual rehabilitative treatment 5 days a week for 8 weeks | EMG, dynamometer, GMFM, passive angle measurement. Evaluation was performed at baseline and the end of treatment (8 weeks) | No significant differences between the two groups |
| Olama 2013 [27] | RCT. Three sides supported AFO’s role in balance improvement in children affected by CP and spastic diplegia | 30 children affected by CP and spastic diplegia | First group (n 15): AFO and rehabilitation for 30 min, three times per week for 6 months Second group (n 15): rehabilitation | Ashworth Scale for spasticity assessment, dynamic balance test with a Biodex balance board for balance assessment Evaluations at baseline and after 6 months | Improvement of posture and balance with AFO |
| Sherief 2015 [24] | RCT. Efficacy of treadmill treatment combined with DAFO in balance improvement in CP emiplegic children | 30 spastic emiplegic children affected by CP | First group (n 15): rehabilitation for 60 min, three times per week for three months Second group (n 15): rehabilitation for 60 min, three times per week for three months + training on a treadmill wearing DAFO for 30 min | Evaluation at baseline and after three months with The Peabody Developmental Test of Motor Proficiency and a Biodex balance board | 12 weeks of treatment with treadmill, and DAFO improves gross motor function (standing and walking) and balance |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miccinilli, S.; Santacaterina, F.; Della Rocca, R.; Sterzi, S.; Bressi, F.; Bravi, M. Efficacy of Lower Limb Orthoses in the Rehabilitation of Children Affected by Cerebral Palsy: A Systematic Review. Children 2024, 11, 212. https://doi.org/10.3390/children11020212
Miccinilli S, Santacaterina F, Della Rocca R, Sterzi S, Bressi F, Bravi M. Efficacy of Lower Limb Orthoses in the Rehabilitation of Children Affected by Cerebral Palsy: A Systematic Review. Children. 2024; 11(2):212. https://doi.org/10.3390/children11020212
Chicago/Turabian StyleMiccinilli, Sandra, Fabio Santacaterina, Rebecca Della Rocca, Silvia Sterzi, Federica Bressi, and Marco Bravi. 2024. "Efficacy of Lower Limb Orthoses in the Rehabilitation of Children Affected by Cerebral Palsy: A Systematic Review" Children 11, no. 2: 212. https://doi.org/10.3390/children11020212
APA StyleMiccinilli, S., Santacaterina, F., Della Rocca, R., Sterzi, S., Bressi, F., & Bravi, M. (2024). Efficacy of Lower Limb Orthoses in the Rehabilitation of Children Affected by Cerebral Palsy: A Systematic Review. Children, 11(2), 212. https://doi.org/10.3390/children11020212






