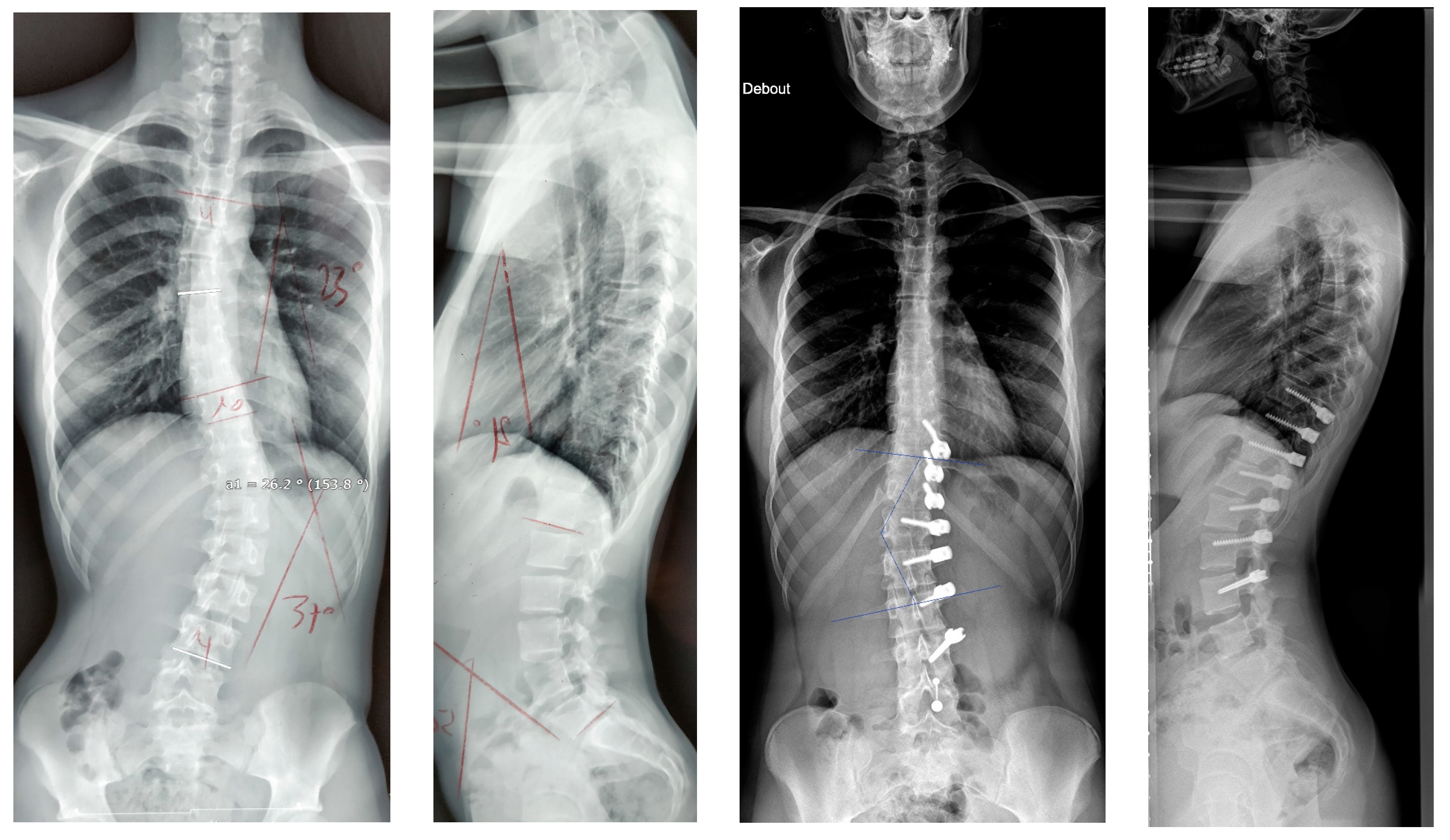
Posterior Vertebral Body Tethering: A Preliminary Study of a New Technique to Correct Lenke 5C Lumbar Curves in Adolescent Idiopathic Scoliosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
- -
- Diagnosis of idiopathic scoliosis from 11 to 16 years old;
- -
- Severe progressive curves: >35°;
- -
- Type 5C on the Lenke Classification;
- -
- Surgical treatment using a “Posterior Vertebral Body Tethering” as described in the operative technique;
- -
- A minimum follow-up of 2 years.
- -
- Curves other than Lenke 5C;
- -
- Curves < 35° or >60°;
- -
- Secondary scoliosis.
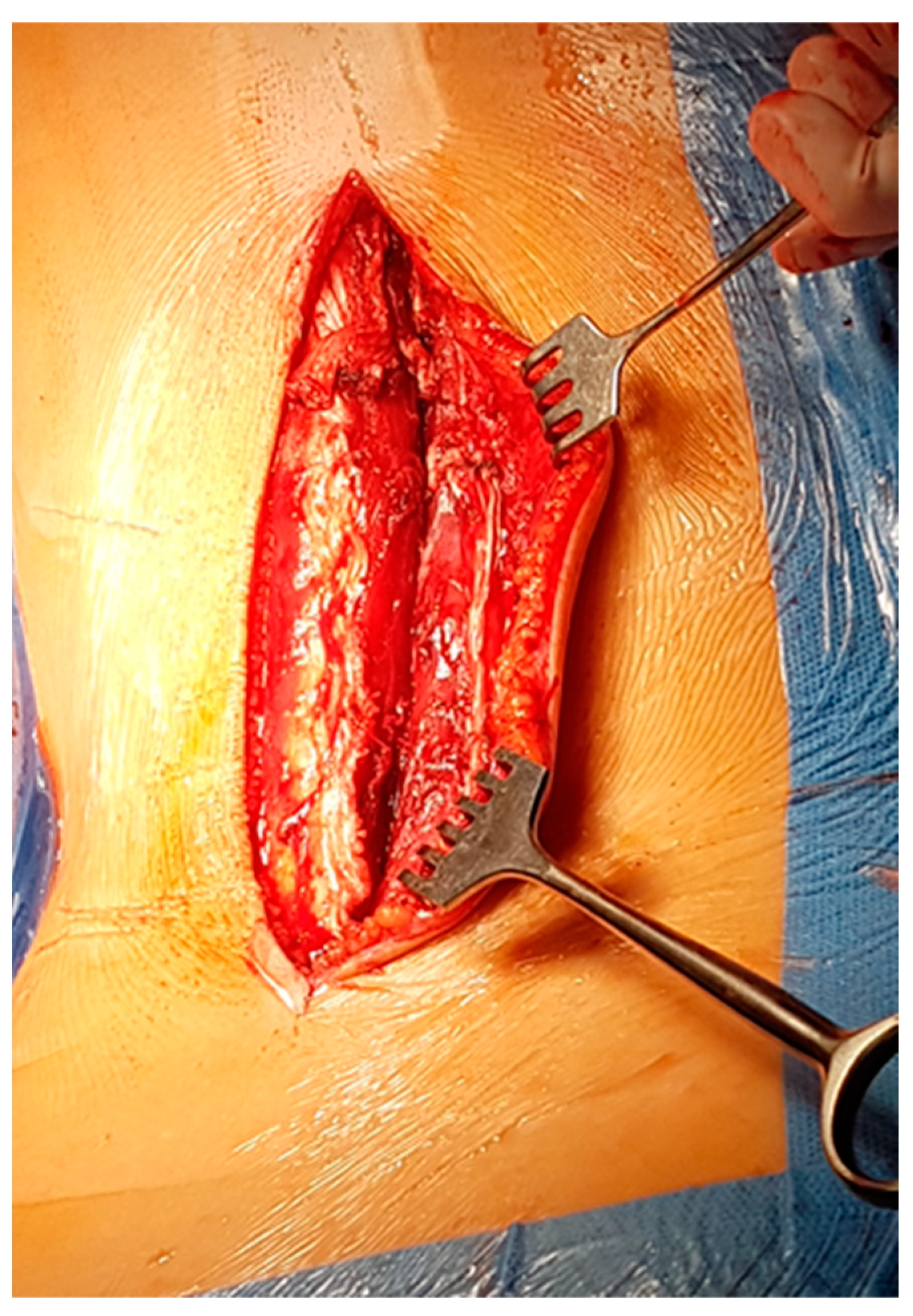
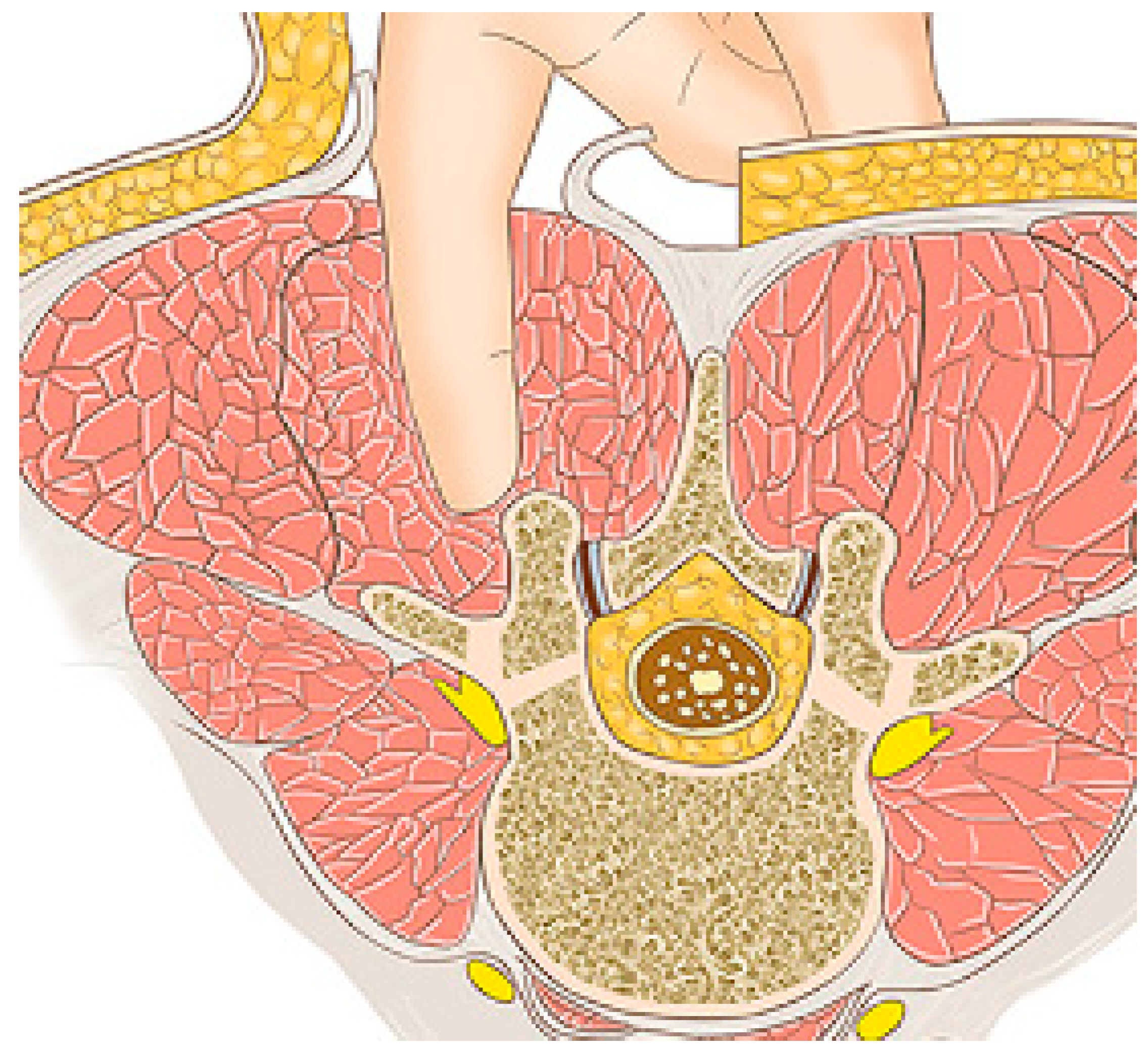
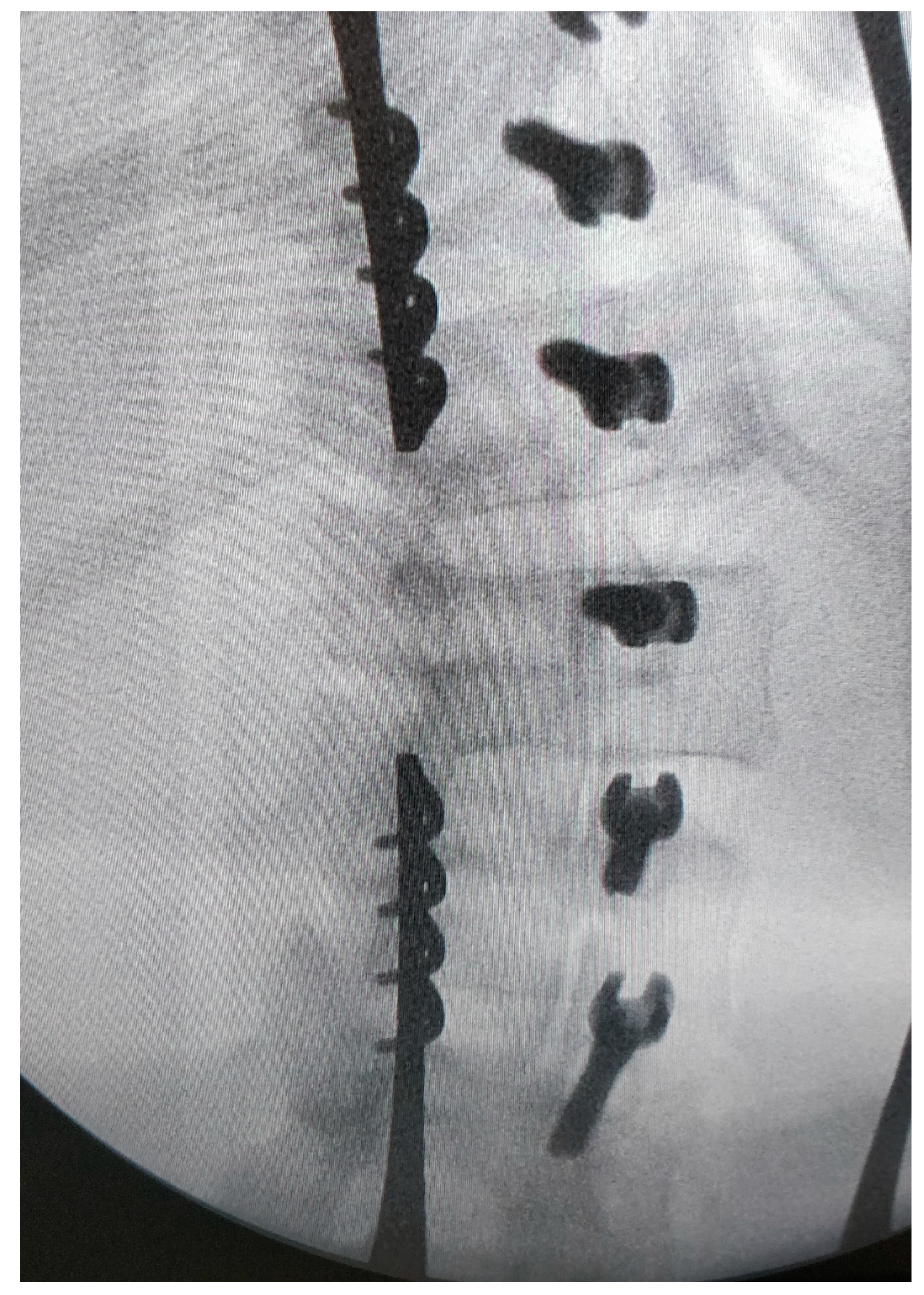
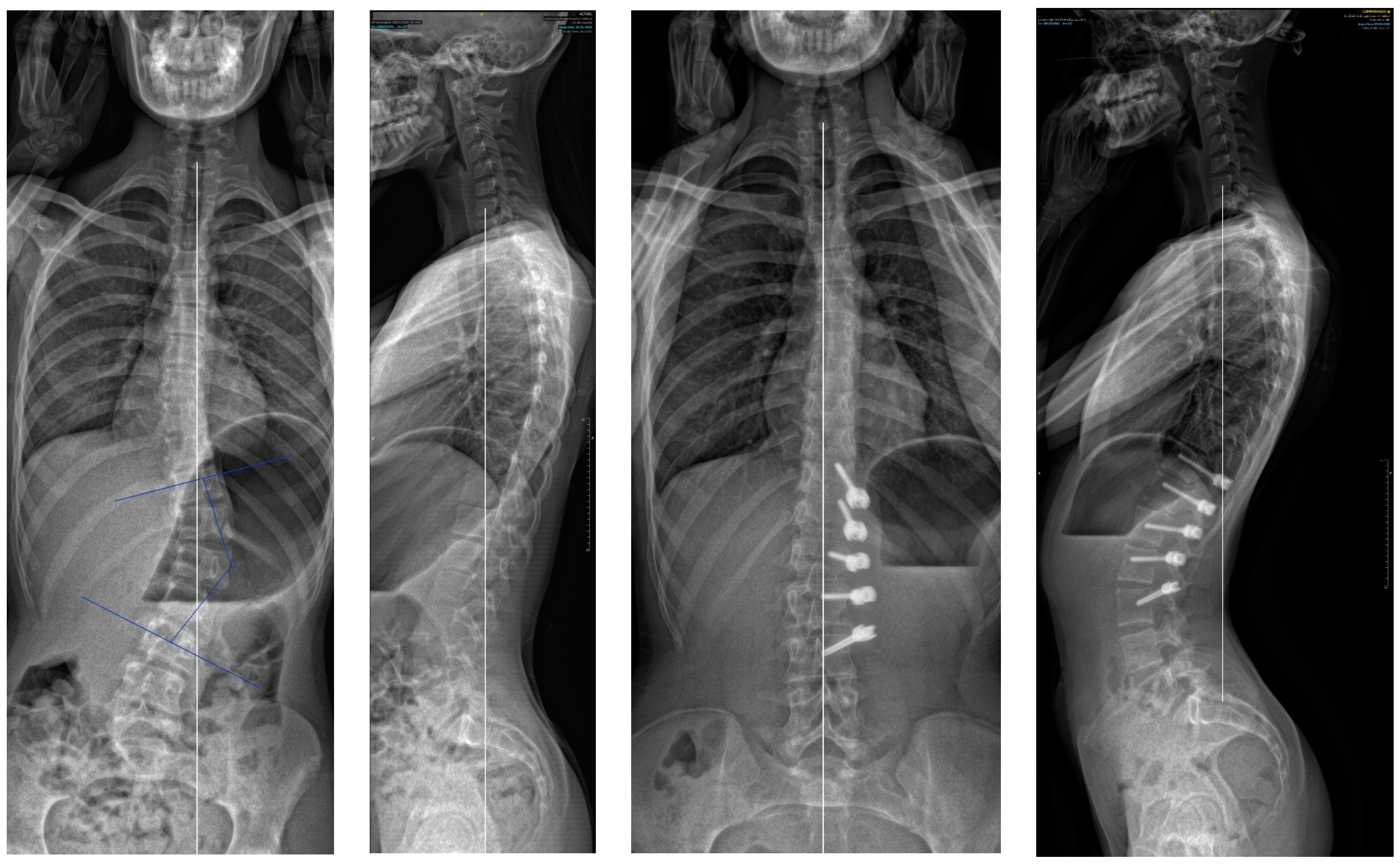
2.2. Surgical Technique
2.3. Post-Operative Management
2.4. Outcomes of Interest
2.5. Statistical Analysis
3. Results
3.1. Patient Selection and Demographic Data
3.2. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Courvoisier, A.; Baroncini, A.; Jeandel, C.; Barra, C.; Lefevre, Y.; Solla, F.; Gouron, R.; Métaizeau, J.-D.; Maximin, M.-C.; Cunin, V. Vertebral Body Tethering in AIS Management—A Preliminary Report. Children 2023, 10, 192. [Google Scholar] [CrossRef]
- Helenius, L.; Diarbakerli, E.; Grauers, A.; Lastikka, M.; Oksanen, H.; Pajulo, O.; Löyttyniemi, E.; Manner, T.; Gerdhem, P.; Helenius, I. Back Pain and Quality of Life After Surgical Treatment for Adolescent Idiopathic Scoliosis at 5-Year Follow-up: Comparison with Healthy Controls and Patients with Untreated Idiopathic Scoliosis. J. Bone Joint Surg. Am. 2019, 101, 1460–1466. [Google Scholar] [CrossRef]
- von Treuheim, T.D.P.; Eaker, L.; Markowitz, J.; Shankar, D.; Meyers, J.; Lonner, B. Anterior Vertebral Body Tethering for Scoliosis Patients with and without Skeletal Growth Remaining: A Retrospective Review with Minimum 2-Year Follow-Up. Int. J. Spine Surg. 2023, 17, 6–16. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Zavala, D.C.; Ponseti, I.V. Idiopathic scoliosis: Long-term follow-up and prognosis in untreated patients. J. Bone Joint Surg. Am. 1981, 63, 702–712. [Google Scholar] [CrossRef]
- Boeyer, M.E.; Farid, S.; Wiesemann, S.; Hoernschemeyer, D.G. Outcomes of vertebral body tethering in the lumbar spine. Spine Deform. 2023, 11, 909–918. [Google Scholar] [CrossRef] [PubMed]
- Miyanji, F.; Pawelek, J.; Nasto, L.A.; Rushton, P.; Simmonds, A.; Parent, S. Safety and efficacy of anterior vertebral body tethering in the treatment of idiopathic scoliosis. Bone Jt. J. 2020, 102-B, 1703–1708. [Google Scholar] [CrossRef] [PubMed]
- Newton, P.O.; Bartley, C.E.; Bastrom, T.P.; Kluck, D.G.; Saito, W.; Yaszay, B. Anterior Spinal Growth Modulation in Skeletally Immature Patients with Idiopathic Scoliosis: A Comparison with Posterior Spinal Fusion at 2 to 5 Years Postoperatively. J. Bone Joint Surg. Am. 2020, 102, 769–777. [Google Scholar] [CrossRef] [PubMed]
- Raitio, A.; Syvänen, J.; Helenius, I. Vertebral Body Tethering: Indications, Surgical Technique, and a Systematic Review of Published Results. J. Clin. Med. 2022, 11, 2576. [Google Scholar] [CrossRef] [PubMed]
- Danielsson, A.J.; Romberg, K.; Nachemson, A.L. Spinal Range of Motion, Muscle Endurance, and Back Pain and Function at Least 20 Years after Fusion or Brace Treatment for Adolescent Idiopathic Scoliosis: A Case-Control Study. Spine 2006, 31, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Helenius, I.; Remes, V.; Yrjönen, T.; Ylikoski, M.; Schlenzka, D.; Helenius, M.; Poussa, M. Harrington and Cotrel-Dubousset Instrumentation in Adolescent Idiopathic Scoliosis: Long-Term Functional and Radiographic Outcomes. J. Bone Jt. Surg.-Am. Vol. 2003, 85, 2303–2309. [Google Scholar] [CrossRef] [PubMed]
- Suk, S.-I.; Lee, S.-M.; Chung, E.-R.; Kim, J.-H.; Kim, S.-S. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: More than 5-year follow-up. Spine 2005, 30, 1602–1609. [Google Scholar] [CrossRef]
- Trobisch, P.D.; Baroncini, A. Preliminary outcomes after vertebral body tethering (VBT) for lumbar curves and subanalysis of a 1- versus 2-tether construct. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2021, 30, 3570–3576. [Google Scholar] [CrossRef] [PubMed]
- Guiroy, A.; Sícoli, A.; Masanés, N.; Ciancio, A.; Gagliardi, M.; Falavigna, A. How to perform the wiltse posterolateral spinal approach: Technical note. Surg. Neurol. Int. 2018, 9, 38. [Google Scholar] [CrossRef] [PubMed]
- Kieser, D.C.; Thakar, C.; Cunningham, G.; Vidakovic, H.; Hammer, N.; Nnadi, C. The Value of a Modified Wiltse Approach for Deformity Correction in Neuromuscular Scoliosis. Int. J. Spine Surg. 2020, 14, 170–174. [Google Scholar] [CrossRef]
- Lu, Y.; Miao, Y.; Zhu, T.; Wu, Q.; Shen, X.; Lu, D.; Zhu, X.; Gan, M. Comparison of the Wiltse Approach and Percutaneous Pedicle Screw Fixation Under O-arm Navigation for the Treatment of Thoracolumbar Fractures. Orthop. Surg. 2021, 13, 1618–1627. [Google Scholar] [CrossRef] [PubMed]
- Pehlivanoglu, T.; Oltulu, I.; Erdag, Y.; Korkmaz, E.; Sarioglu, E.; Ofluoglu, E.; Aydogan, M. Double-sided vertebral body tethering of double adolescent idiopathic scoliosis curves: Radiographic outcomes of the first 13 patients with 2 years of follow-up. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2021, 30, 1896–1904. [Google Scholar] [CrossRef] [PubMed]
- Newton, P.O. Spinal growth tethering: Indications and limits. Ann. Transl. Med. 2020, 8, 27. [Google Scholar] [CrossRef]
- Newton, P.O.; Upasani, V.V.; Farnsworth, C.L.; Oka, R.; Chambers, R.C.; Dwek, J.; Kim, J.R.; Perry, A.; Mahar, A.T. Spinal growth modulation with use of a tether in an immature porcine model. J. Bone Joint Surg. Am. 2008, 90, 2695–2706. [Google Scholar] [CrossRef]
- Cobetto, N.; Parent, S.; Aubin, C.E. 3D correction over 2years with anterior vertebral body growth modulation: A finite element analysis of screw positioning, cable tensioning and postoperative functional activities. Clin. Biomech. Bristol. Avon. Janv. 2018, 51, 26–33. [Google Scholar] [CrossRef]
- Cobetto, N.; Aubin, C.E.; Parent, S. Anterior Vertebral Body Growth Modulation: Assessment of the 2-year Predictive Capability of a Patient-specific Finite-element Planning Tool and of the Growth Modulation Biomechanics. Spine 2020, 45, E1203–E1209. [Google Scholar] [CrossRef]
- Mathew, S.; Larson, A.N.; Potter, D.D.; Milbrandt, T.A. Defining the learning curve in CT-guided navigated thoracoscopic vertebral body tethering. Spine Deform. 2021, 9, 1581–1589. [Google Scholar] [CrossRef] [PubMed]
- Baroncini, A.; Trobisch, P.D.; Berrer, A.; Kobbe, P.; Tingart, M.; Eschweiler, J.; Da Paz, S.; Migliorini, F. Return to sport and daily life activities after vertebral body tethering for AIS: Analysis of the sport activity questionnaire. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2021, 30, 1998–2006. [Google Scholar] [CrossRef] [PubMed]
- Buyuk, A.F.; Milbrandt, T.A.; Mathew, S.E.; Larson, A.N. Measurable Thoracic Motion Remains at 1 Year following Anterior Vertebral Body Tethering, with Sagittal Motion Greater Than Coronal Motion. J. Bone Joint Surg. Am. 2021, 103, 2299–2305. [Google Scholar] [CrossRef] [PubMed]
- Marks, M.C.; Bastrom, T.P.; Petcharaporn, M.; Shah, S.A.; Betz, R.R.; Samdani, A.; Lonner, B.; Miyanji, F.; Newton, P.O. The Effect of Time and Fusion Length on Motion of the Unfused Lumbar Segments in Adolescent Idiopathic Scoliosis. Spine Deform. 2015, 3, 549–553. [Google Scholar] [CrossRef] [PubMed]
- Nicolini, L.F.; Kobbe, P.; Seggewiß, J.; Greven, J.; Ribeiro, M.; Beckmann, A.; Da Paz, S.; Eschweiler, J.; Prescher, A.; Markert, B.; et al. Motion preservation surgery for scoliosis with a vertebral body tethering system: A biomechanical study. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2022, 31, 1013–1021. [Google Scholar] [CrossRef] [PubMed]
- Parsch, D.; Gaertner, V.; Brocai, D.R.; Carstens, C. The effect of spinal fusion on the long-term outcome of idiopathic scoliosis. A case-control study. J. Bone Joint Surg. Br. 2001, 83, 1133–1136. [Google Scholar] [CrossRef]
- Mariscal, G.; Morales, J.; Pérez, S.; Rubio-Belmar, P.A.; Bovea-Marco, M.; Bas, J.L.; Bas, P.; Bas, T. Meta-analysis on the efficacy and safety of anterior vertebral body tethering in adolescent idiopathic scoliosis. Eur. Spine J. 2023, 32, 140–148. [Google Scholar] [CrossRef]
- Baroncini, A.; Trobisch, P.; Eschweiler, J.; Migliorini, F. Analysis of the risk factors for early tether breakage following vertebral body tethering in adolescent idiopathic scoliosis. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2022, 31, 2348–2354. [Google Scholar] [CrossRef]
- Wu, H.-H.; Saggi, S.; Katyal, T.; Allahabadi, S.; Siu, J.; Diab, M. 167. Combined thoracic anterior and lumbar posterior tethering vs anterior vertebral body tethering: Outcomes in skeletally immature idiopathic scoliosis. Spine J. 2021, 21, S84. [Google Scholar] [CrossRef]




| Pre-Operative | First Standing | Two Years | |
|---|---|---|---|
| Major curve bending | 15.6° (8.8) | Not applicable | Not applicable |
| Major curve | 43.9° (9.2) | 20.3° (16.2) | 13.2° (28.2) |
| Secondary curve | 29.1° (12.6) | 21.9° (11.2) | 19.9° (13.9) |
| Kyphosis (T4T12) | 23.2° (7.8) | 25.1° (9.5) | 26.9° (12.6) |
| Lordosis (L1L5) | 41.7° (7.8) | 42.4° (10.1) | 42.8° (7.5) |
| Main Curve Improvement in Percentages | Main Curve Improvement in Degrees | p Value | |
|---|---|---|---|
| 2Y to POB | 15% | 2.4° | 0.96 |
| FS to POS | 54% | 23.6° | 0.00000002 |
| 2Y to POS | 70% | 30.7° | 0.00005 |
| 2Y to FS | 35% | 7.1° | 0.56 |
| Number of Patients (%) | Treatment | Final Result Consequence | |
|---|---|---|---|
| Pain | 3 (13.6%) | 1 painkiller, physiotherapy 1 screw removed (intra-canal) 1 material remove | none |
| Overcorrection | 4 (18.1%) | 1 tether section 1 posterior fusion 2 material remove | 1 posterior fusion none for the others |
| Screw pulled out or screw breakage | 4 (18.1%) | 2 revisions 2 without consequence | none |
| Curve progression | 2 (9%) | 2 posterior fusion | 2 posteriors fusions |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Metaizeau, J.-D.; Denis, D. Posterior Vertebral Body Tethering: A Preliminary Study of a New Technique to Correct Lenke 5C Lumbar Curves in Adolescent Idiopathic Scoliosis. Children 2024, 11, 157. https://doi.org/10.3390/children11020157
Metaizeau J-D, Denis D. Posterior Vertebral Body Tethering: A Preliminary Study of a New Technique to Correct Lenke 5C Lumbar Curves in Adolescent Idiopathic Scoliosis. Children. 2024; 11(2):157. https://doi.org/10.3390/children11020157
Chicago/Turabian StyleMetaizeau, Jean-Damien, and Delphy Denis. 2024. "Posterior Vertebral Body Tethering: A Preliminary Study of a New Technique to Correct Lenke 5C Lumbar Curves in Adolescent Idiopathic Scoliosis" Children 11, no. 2: 157. https://doi.org/10.3390/children11020157
APA StyleMetaizeau, J.-D., & Denis, D. (2024). Posterior Vertebral Body Tethering: A Preliminary Study of a New Technique to Correct Lenke 5C Lumbar Curves in Adolescent Idiopathic Scoliosis. Children, 11(2), 157. https://doi.org/10.3390/children11020157




