Comparing Management Strategies for Thoracolumbar Injury Classification and Severity Score of 4 (TLICS = 4) in the Pediatric Population: A Single-Institutional Experience
Abstract
1. Introduction
2. Materials and Methods
2.1. Variables
2.2. Preoperative Surgical Decision Making
2.3. Treatment Technique
2.4. Alignment
2.5. Statistical Analysis
3. Results
3.1. Demographics
3.2. Injury Characteristics
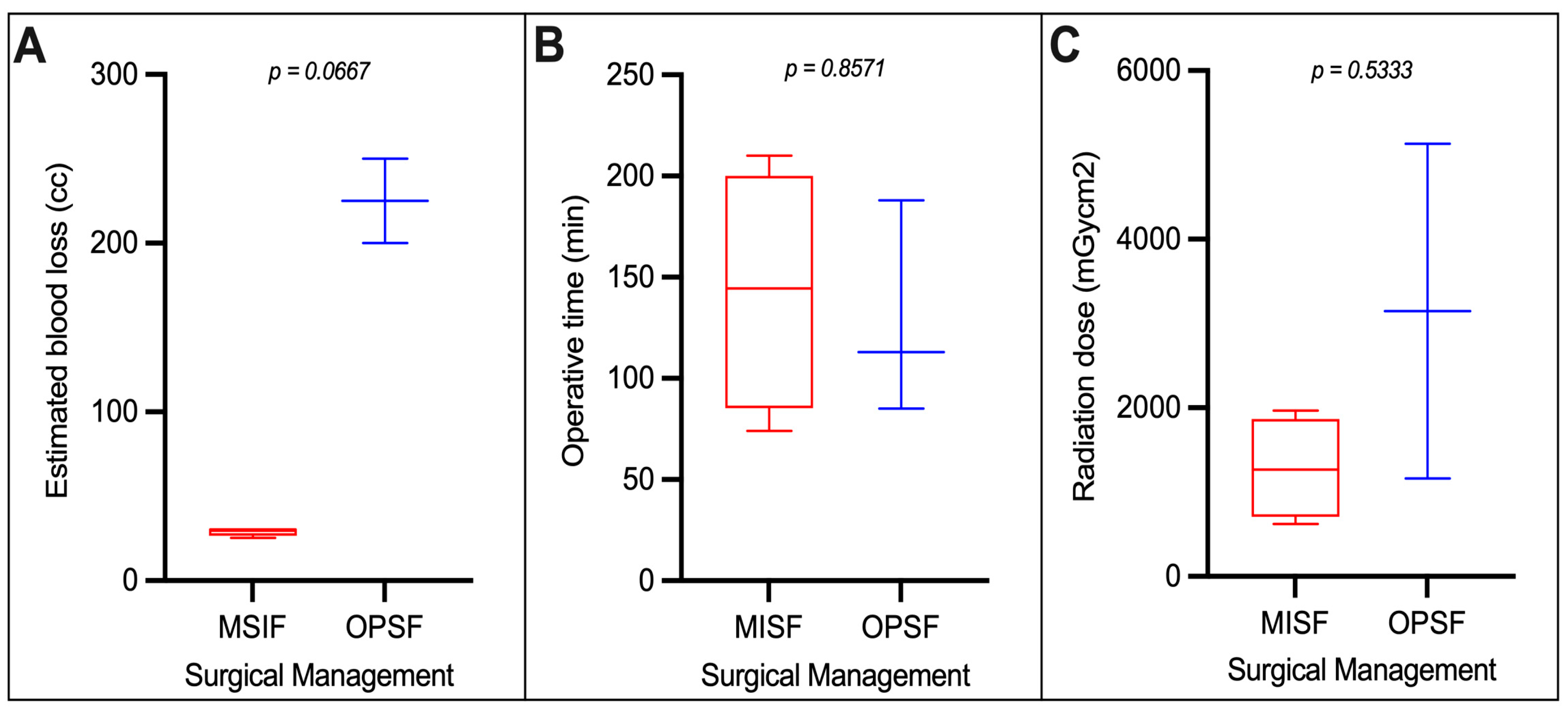
3.3. Operative Characteristics
3.4. Radiation Exposure
3.5. Complications
3.6. Length of Stay
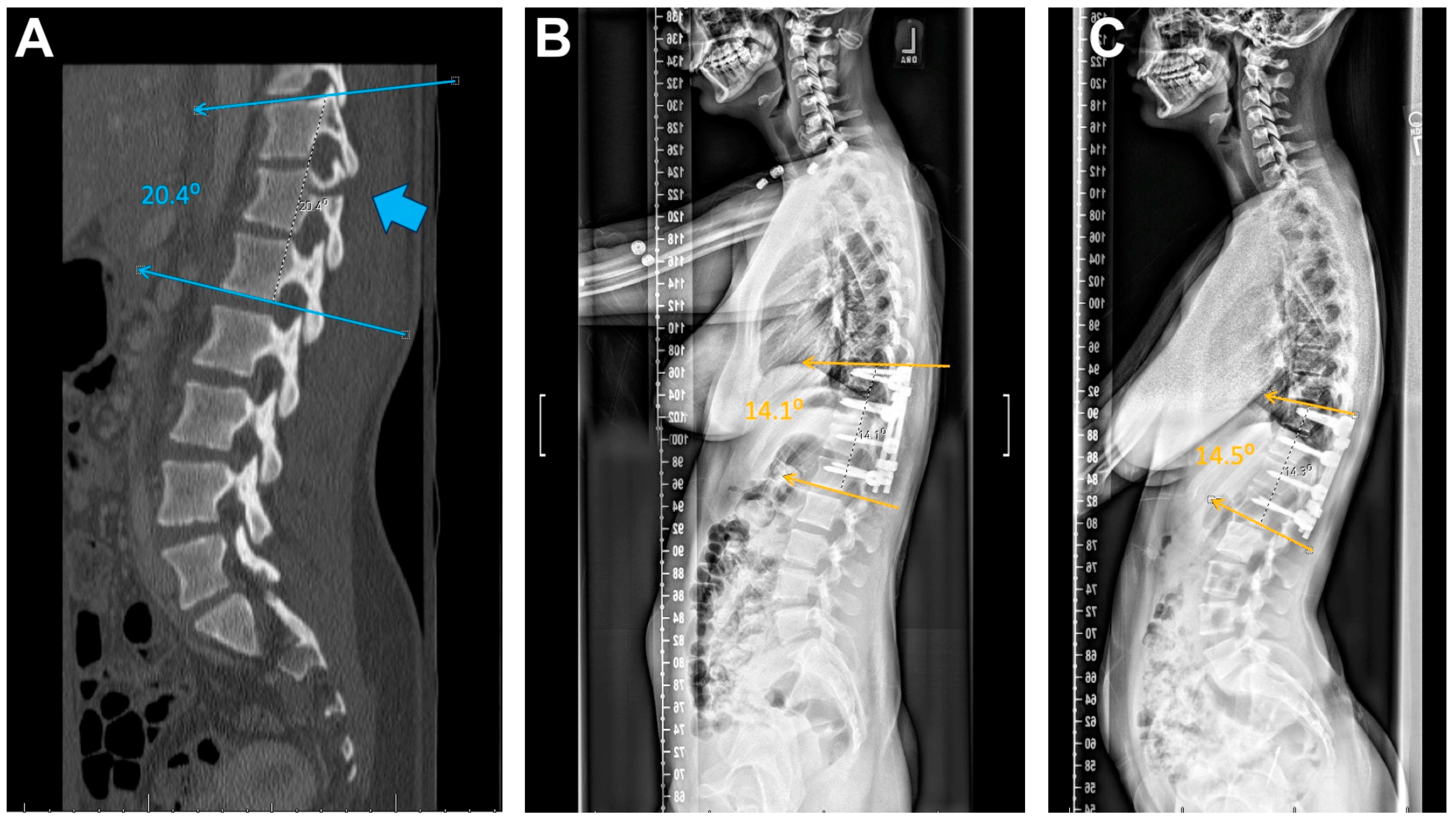
3.7. Alignment
4. Discussion
4.1. Injury Characteristics
4.2. Clinical Exam
4.3. Radiation Exposure
4.4. OR Time and Blood Loss
4.5. Length of Stay and Complications
4.6. Alignment
4.7. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Akbarnia, B.A. Pediatric spine fractures. Orthop. Clin. N. Am. 1999, 30, 521–536. [Google Scholar] [CrossRef] [PubMed]
- Bronsard, N.; Boli, T.; Challali, M.; De Dompsure, R.; Amoretti, N.; Padovani, B.; Bruneton, G.; Fuchs, A.; De Peretti, F. Comparison between percutaneous and traditional fixation of lumbar spine fracture: Intraoperative radiation exposure levels and outcomes. Orthop. Traumatol. Surg. Res. 2013, 99, 162–168. [Google Scholar] [CrossRef]
- Dai, L.-Y.; Jiang, S.-D.; Wang, X.-Y.; Jiang, L.-S. A review of the management of thoracolumbar burst fractures. Surg. Neurol. 2007, 67, 221–231; discussion 231. [Google Scholar] [CrossRef] [PubMed]
- Gavira, N.; Amelot, A.; Cook, A.-R.; Hamel, A.; Buffenoir, K.; Cristini, J. Thoracolumbar spinal fracture in children: Conservative or surgical treatment? Neurochirurgie 2022, 68, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Parisini, P.; Di Silvestre, M.; Greggi, T. Treatment of spinal fractures in children and adolescents: Long-term results in 44 patients. Spine 2002, 27, 1989–1994. [Google Scholar] [CrossRef]
- Leroux, J.; Vivier, P.-H.; Ould Slimane, M.; Foulongne, E.; Abu-Amara, S.; Lechevallier, J.; Griffet, J. Early diagnosis of thoracolumbar spine fractures in children. A prospective study. Orthop. Traumatol. Surg. Res. 2013, 99, 60–65. [Google Scholar] [CrossRef]
- Saul, D.; Dresing, K. Epidemiology of vertebral fractures in pediatric and adolescent patients. Pediatr. Rep. 2018, 10, 7232. [Google Scholar] [CrossRef]
- Bartels, D.D.; McCann, M.E.; Davidson, A.J.; Polaner, D.M.; Whitlock, E.L.; Bateman, B.T. Estimating pediatric general anesthesia exposure: Quantifying duration and risk. Paediatr. Anaesth. 2018, 28, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Goodman, T.R.; Mustafa, A.; Rowe, E. Pediatric CT radiation exposure: Where we were, and where we are now. Pediatr. Radiol. 2019, 49, 469–478. [Google Scholar] [CrossRef]
- Kalkman, C.J.; Peelen, L.; Moons, K.G.; Veenhuizen, M.; Bruens, M.; Sinnema, G.; de Jong, T.P. Behavior and development in children and age at the time of first anesthetic exposure. Anesthesiology 2009, 110, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, D.; Than, K.D.; Wang, A.C.; La Marca, F.; Wang, P.I.; Schermerhorn, T.C.; Park, P. Radiation safety and spine surgery: Systematic review of exposure limits and methods to minimize radiation exposure. World Neurosurg. 2014, 82, 1337–1343. [Google Scholar] [CrossRef]
- Gallagher, D.J.; Heinrich, S.D. Pediatric chance fracture. J. Orthop. Trauma. 1990, 4, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Fishman, D.S.; Andropoulos, D.B.; Lightdale, J.R. Sedation and the Food and Drug Administration Warning: What a Pediatric Gastroenterologist, Hepatologist, and Pancreatologist Should Know. J. Pediatr. Gastroenterol. Nutr. 2019, 69, 3–5. [Google Scholar] [CrossRef] [PubMed]
- McAfee, P.C.; Phillips, F.M.; Andersson, G.; Buvenenadran, A.; Kim, C.W.; Lauryssen, C.; Isaacs, R.E.; Youssef, J.A.; Brodke, D.S.; Cappuccino, A.; et al. Minimally invasive spine surgery. Spine 2010, 35, S271–S273. [Google Scholar] [CrossRef] [PubMed]
- Mikhail, C.; Pennington, Z.; Arnold, P.M.; Brodke, D.S.; Chapman, J.R.; Chutkan, N.; Daubs, M.D.; DeVine, J.G.; Fehlings, M.G.; Gelb, D.E.; et al. Minimizing Blood Loss in Spine Surgery. Global Spine J. 2020, 10, 71S–83S. [Google Scholar] [CrossRef]
- Schömig, F.; Taheri, N.; Kalaf, H.; Muellner, M.; Becker, L.; Pumberger, M. Validation of the TLICS and AOSpine injury score for surgical management of paediatric traumatic spinal injuries. Arch. Orthop. Trauma. Surg. 2023, 143, 2011–2017. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.; Yen, D. Late neurologic deterioration after nonoperative treatment of a Chance fracture in an adolescent. Can. J. Surg. 2003, 46, 383–385. [Google Scholar] [PubMed]
- Agha, R.A.; Sohrabi, C.; Mathew, G.; Franchi, T.; Kerwan, A.; O’Neill, N.; PROCESS Group. The PROCESS 2020 Guideline: Updating Consensus Preferred Reporting of CasESeries in Surgery (PROCESS) Guidelines. Int. J. Surg. 2020, 84, 231–235. [Google Scholar] [CrossRef]
- Stagi, S.; Cavalli, L.; Iurato, C.; Seminara, S.; Brandi, M.L.; de Martino, M. Bone metabolism in children and adolescents: Main characteristics of the determinants of peak bone mass. Clin. Cases Miner. Bone Metab. 2013, 10, 172–179. [Google Scholar] [PubMed]
- Vedantam, A.; Fridley, J.S.; Navarro, J.C.; Gopinath, S.P. Management of Acute Unilateral Nondisplaced Subaxial Cervical Facet Fractures. Oper. Neurosurg. 2018, 14, 104–111. [Google Scholar] [CrossRef]
- Sravisht, I. Available online: https://www.hss.edu/condition-list_spondylolysis-pars-fracture.asp#:~:text=The%20initial%20treatment%20for%20these,treatment%2C%20surgery%20may%20be%20required (accessed on 10 June 2021).
- Arkader, A.; Warner, W.C.; Tolo, V.T.; Sponseller, P.D.; Skaggs, D.L. Pediatric Chance Fractures: A Multicenter Perspective. J. Pediatr. Orthop. 2011, 31, 741–744. [Google Scholar] [CrossRef]
- Gilsanz, V.; Gibbens, D.T.; Roe, T.F.; Carlson, M.; Senac, M.O.; Boechat, M.I.; Huang, H.K.; Schulz, E.E.; Libanati, C.R.; Cann, C.C. Vertebral bone density in children: Effect of puberty. Radiology 1988, 166, 847–850. [Google Scholar] [CrossRef] [PubMed]
- Subotic, U.; Holland-Cunz, S.; Bardenheuer, M.; Loff, S.; Wessel, L.M. Chance fracture—A rare injury in pediatric patients? Eur. J. Pediatr. Surg. 2007, 17, 207–209. [Google Scholar] [CrossRef] [PubMed]



| Operative | Non-Operative | Total | p-Value | ||
|---|---|---|---|---|---|
| OPSF | MISF | ||||
| Number of patients | 3 | 4 | 4 | 11 | |
| Mean age (years) | 16 | 10.5 | 10.25 | 11.9 | 0.052 |
| Gender | 0.77 | ||||
| Female | 1 | 1 | 2 | 4 | |
| Male | 2 | 3 | 2 | 7 | |
| Race | >0.99 | ||||
| White | 3 | 2 | 2 | 7 | |
| Asian | 0 | 1 | 1 | 2 | |
| Other | 0 | 1 | 1 | 2 | |
| Ethnicity | 0.055 | ||||
| Hispanic | 0 | 0 | 3 | 3 | |
| Non-Hispanic | 3 | 4 | 1 | 8 | |
| Mean height (cm) | 167.6 | 151.6 | 142.85 | 151.3 | 0.78 |
| Mean weight (kg) | 63.7 | 37.5 | 49.7 | 49.1 | 0.17 |
| Injury type | >0.99 | ||||
| MVC | 2 | 2 | 2 | 6 | |
| ATV | 0 | 1 | 0 | 1 | |
| Fall | 1 | 1 | 0 | 2 | |
| Auto vs. Peds | 0 | 0 | 1 | 1 | |
| Penetrating injury | 0 | 0 | 1 | 1 | |
| Fracture level location | 0.39 | ||||
| T2–T8 | 2 | 0 | 2 | 4 | |
| T9–T12 | 0 | 1 | 0 | 1 | |
| L1–L5 | 1 | 3 | 2 | 6 | |
| Morphology | 0.76 | ||||
| Chance fracture | 2 | 2 | 1 | 5 | |
| Posterior column fracture | 1 | 2 | 3 | 6 | |
| Number of fractured levels | 0.34 | ||||
| 1 | 1 | 2 | 1 | 4 | |
| 2 | 0 | 1 | 3 | 4 | |
| >2 | 2 | 2 | 0 | 4 | |
| Polytrauma | 3 | 4 | 3 | 10 | 0.6 |
| Mobility-limiting | 0 | 0 | 1 | 1 | |
| Not mobility-limiting | 3 | 4 | 2 | 9 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castillo, J.; Le, M.N.; Soufi, K.; Zhou, J.; Kulubya, E.; Moskalik, A.; Javidan, Y.; Ebinu, J.O. Comparing Management Strategies for Thoracolumbar Injury Classification and Severity Score of 4 (TLICS = 4) in the Pediatric Population: A Single-Institutional Experience. Children 2024, 11, 1529. https://doi.org/10.3390/children11121529
Castillo J, Le MN, Soufi K, Zhou J, Kulubya E, Moskalik A, Javidan Y, Ebinu JO. Comparing Management Strategies for Thoracolumbar Injury Classification and Severity Score of 4 (TLICS = 4) in the Pediatric Population: A Single-Institutional Experience. Children. 2024; 11(12):1529. https://doi.org/10.3390/children11121529
Chicago/Turabian StyleCastillo, Jose, Michael Nhien Le, Khadija Soufi, James Zhou, Edwin Kulubya, Anzhela Moskalik, Yashar Javidan, and Julius O. Ebinu. 2024. "Comparing Management Strategies for Thoracolumbar Injury Classification and Severity Score of 4 (TLICS = 4) in the Pediatric Population: A Single-Institutional Experience" Children 11, no. 12: 1529. https://doi.org/10.3390/children11121529
APA StyleCastillo, J., Le, M. N., Soufi, K., Zhou, J., Kulubya, E., Moskalik, A., Javidan, Y., & Ebinu, J. O. (2024). Comparing Management Strategies for Thoracolumbar Injury Classification and Severity Score of 4 (TLICS = 4) in the Pediatric Population: A Single-Institutional Experience. Children, 11(12), 1529. https://doi.org/10.3390/children11121529







