Disease Trends in Children and Adolescents in Japan: A Retrospective Observational Study Using the Nationwide Claims Data for 2012–2016
Abstract
1. Introduction
2. Methods
2.1. Study Design and Setting
Study Population and Data Source
2.2. Variables and Data Description
2.3. Data Analysis
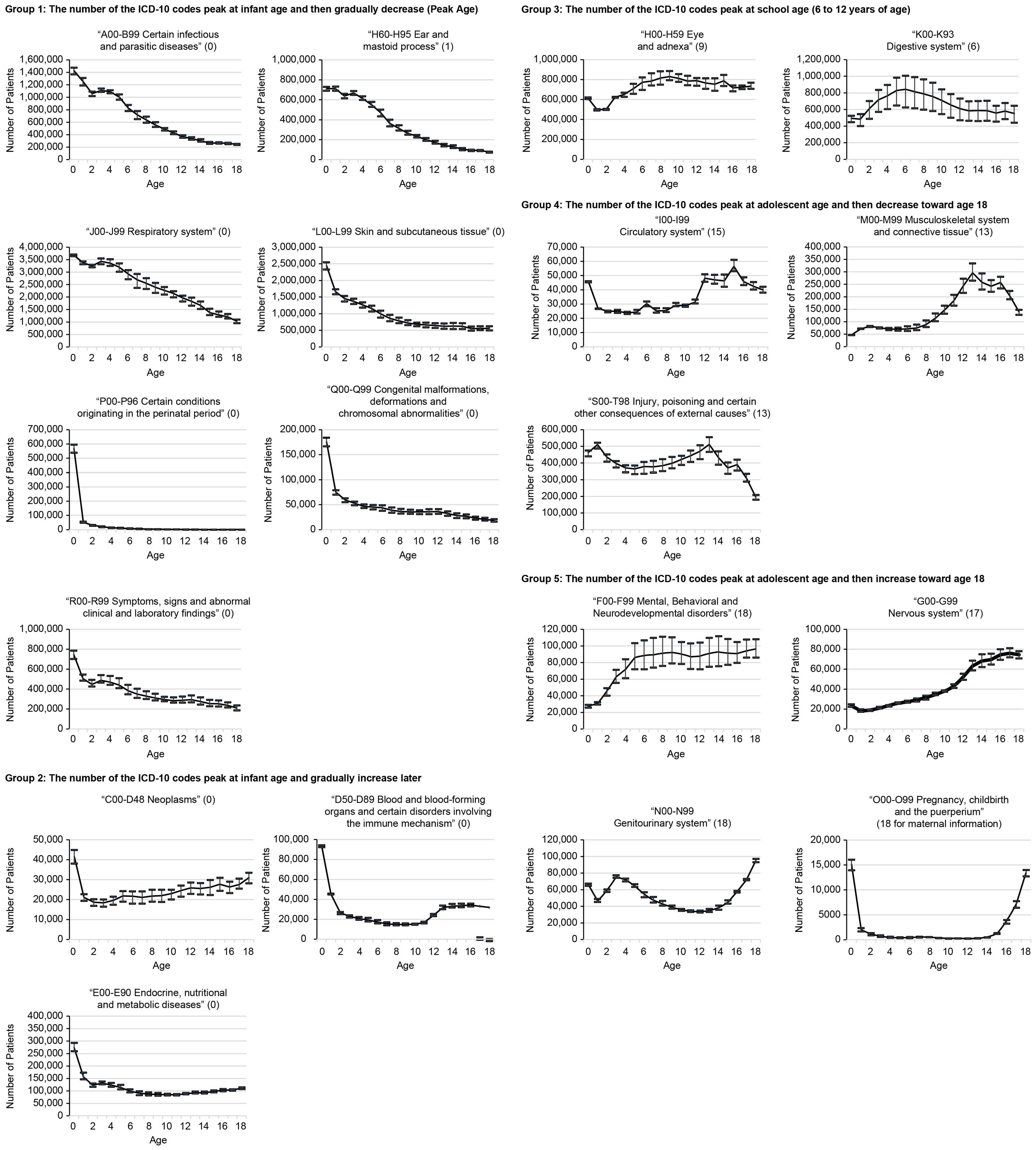
3. Results
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Kassebaum, N.; Kyu, H.H.; Zoeckler, L.; Olsen, H.E.; Thomas, K.; Pinho, C.; Bhutta, Z.A.; Dandona, L.; Ferrari, A.; Ghiwot, T.T.; et al. Child and adolescent health from 1990 to 2015: Findings from the Global Burden of Diseases, Injuries, and Risk Factors 2015 Study. JAMA Pediatr. 2017, 171, 573–592. [Google Scholar] [PubMed]
- UNICEF. Non-Communicable Diseases. Available online: https://www.unicef.org/health/non-communicable-diseases (accessed on 12 December 2023).
- UNICEF. Child and Adolescent Injuries. Available online: https://www.unicef.org/health/injuries (accessed on 12 December 2023).
- Whitlock, E.P.; Williams, S.B.; Gold, R.; Smith, P.R.; Shipman, S.A. Screening and interventions for childhood overweight: A summary of evidence for the US preventive services task force. Pediatrics 2005, 116, e125-44. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Bassi, S.; Nazar, G.P.; Saluja, K.; Park, M.; Kinra, S.; Arora, M. Impact of school policies on non-communicable disease risk factors—A systematic review. BMC Public Health 2017, 17, 292. [Google Scholar] [CrossRef] [PubMed]
- Harris, S.K.; Aalsma, M.C.; Weitzman, E.R.; Garcia-Huidobro, D.; Wong, C.; Hadland, S.E.; Santelli, J.; Park, M.J.; Ozer, E.M. Research on clinical preventive services for adolescents and young adults: Where are we and where do we need to go? J. Adolesc. Health 2017, 60, 249–260. [Google Scholar] [CrossRef] [PubMed]
- Finnell, S.M.; Stanton, J.L.; Downs, S.M. Actionable recommendations in the Bright Futures child health supervision guidelines. Appl. Clin. Inform. 2014, 5, 651–659. [Google Scholar] [PubMed]
- Melnyk, B.M.; Grossman, D.C.; Chou, R.; Mabry-Hernandez, I.; Nicholson, W.; DeWitt, T.G.; Cantu, A.G.; Flores, G. USPSTF perspective on evidence-based preventive recommendations for children. Pediatrics 2012, 130, e399–e407. [Google Scholar] [CrossRef]
- Strong, K.L.; Pedersen, J.; White Johansson, E.; Cao, B.; Diaz, T.; Guthold, R.; You, D.; Requejo, J.; Liu, L. Patterns and trends in causes of child and adolescent mortality 2000–2016: Setting the scene for child health redesign. BMJ Glob. Health 2021, 6, e004760. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare, Japan. On the Use of the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Available online: https://www.mhlw.go.jp/stf/shingi/2r9852000002ss9z-att/2r9852000002ssfg.pdf (accessed on 24 December 2020).
- Toyokawa, S.; Maeda, E.; Kobayashi, Y. Estimation of the number of children with cerebral palsy using nationwide health insurance claims data in Japan. Dev. Med. Child Neurol. 2017, 59, 317–321. [Google Scholar] [CrossRef]
- Kuniyoshi, Y.; Tokutake, H.; Takahashi, N.; Kamura, A.; Yasuda, S.; Tashiro, M. Regional variation in the development of neonatal hyperbilirubinemia and relation with sunshine duration in Japan: An ecological study. J. Matern Fetal. Neonatal. Med. 2021, 35, 4946–4951. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare, Japan. Status of Health Insurance Claims (April 2016). Available online: https://www.ssk.or.jp/tokeijoho/tokeijoho_rezept/tokeijoho_04_h28.files/seikyu_2804.pdf (accessed on 24 December 2020).
- Ministry of Health, Labour and Welfare, Japan. Summary of Patient Survey. 2017. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/kanja/17/index.html (accessed on 19 March 2021).
- Ministry of Education, Culture, Sports, Science and Technology of Japan. School Health Statistics Research: Summary of the Results of the Survey. 2019. Available online: https://www.mext.go.jp/b_menu/toukei/chousa05/hoken/kekka/k_detail/1411711_00003.htm (accessed on 18 March 2021).
- National Health Service. Common Childhood Illnesses & Well-Being. Available online: https://childrensguide.sesandspccg.nhs.uk/live/childhood-illnesses.html (accessed on 25 December 2023).
- Solmi, M.; Radua, J.; Olivola, M.; Croce, E.; Soardo, L.; Salazar de Pablo, G.; Il Shin, J.; Kirkbride, J.B.; Jones, P.; Kim, J.H.; et al. Age at onset of mental disorders worldwide: Large-scale meta-analysis of 192 epidemiological studies. Mol. Psychiatry 2022, 27, 281–295. [Google Scholar] [CrossRef]
- World Health Organization. The Global Health Observatory. WHO’s Global Health Estimate. Available online: http://www.who.int/healthinfo/mortality_data/en/ (accessed on 7 April 2021).
- Keeley, B. The State of the World’s Children. 2021. Available online: https://files.eric.ed.gov/fulltext/ED615261.pdf (accessed on 22 December 2023).
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Werner-Seidler, A.; Perry, Y.; Calear, A.L.; Newby, J.M.; Christensen, H. School-based depression and anxiety prevention programs for young people: A systematic review and meta-analysis. Clin. Psychol. Rev. 2017, 51, 30–47. [Google Scholar] [CrossRef] [PubMed]
- Werner-Seidler, A.; Spanos, S.; Calear, A.L.; Perry, Y.; Torok, M.; O’Dea, B.; Christensen, H.; Newby, J.M. School-based depression and anxiety prevention programs: An updated systematic review and meta-analysis. Clin. Psychol. Rev. 2021, 89, 102079. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatrics. Bright Futures Guidelines Pocket Guide. Available online: https://downloads.aap.org/AAP/PDF/Bright%20Futures/BF4_POCKETGUIDE.pdf (accessed on 4 December 2023).
- Kubo, S.; Noda, T.; Myojin, T.; Higashino, T.; Matsui, H.; Kato, G.; Imamura, T. The need and key points for patient matching in clinical studies using the National Database of Health Insurance Claims and Specific Health Checkups of Japan (NDB). Jpn. J. Health Res. 2017, 38, 11–19. [Google Scholar]
- Ministry of Health, Labour and Welfare, Japan. Vital Statistics. Available online: https://www.mhlw.go.jp/toukei/list/81-1a.html (accessed on 7 April 2021).
- World Health Organization. Global Status Report on Road Safety. 2018. Available online: https://www.who.int/publications/i/item/9789241565684 (accessed on 18 December 2023).
| 1st | ICD Code | 2nd | ICD Code | 3rd | ICD Code | 4th | ICD Code | 5th | ICD Code | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age_0 | Acute upper respiratory infections | J00-06 | Dermatitis and eczema | L20-30 | Other acute lower respiratory infections | J20-22 | Intestinal infectious diseases | A00-09 | Chronic lower respiratory diseases | J40-47 |
| Age_1 | Acute upper respiratory infections | J00-06 | Dermatitis and eczema | L20-30 | Other acute lower respiratory infections | J20-22 | Intestinal infectious diseases | A00-09 | Chronic lower respiratory diseases | J40-47 |
| Age_2 | Acute upper respiratory infections | J00-06 | Other acute lower respiratory infections | J20-22 | Chronic lower respiratory diseases | J40-47 | Dermatitis and eczema | L20-30 | Other diseases of upper respiratory tract | J30-39 |
| Age_3 | Acute upper respiratory infections | J00-06 | Other acute lower respiratory infections | J20-22 | Chronic lower respiratory diseases | J40-47 | Other diseases of upper respiratory tract | J30-39 | Dermatitis and eczema | L20-30 |
| Age_4 | Acute upper respiratory infections | J00-06 | Other acute lower respiratory infections | J20-22 | Chronic lower respiratory diseases | J40-47 | Other diseases of upper respiratory tract | J30-39 | Diseases of oral cavity and salivary glands | K00-14 |
| Age_5 | Acute upper respiratory infections | J00-06 | Diseases of oral cavity and salivary glands | K00-14 | Other diseases of upper respiratory tract | J30-39 | Chronic lower respiratory diseases | J40-47 | Other acute lower respiratory infections | J20-22 |
| Age_6 | Acute upper respiratory infections | J00-06 | Diseases of oral cavity and salivary glands | K00-14 | Other diseases of upper respiratory tract | J30-39 | Chronic lower respiratory diseases | J40-47 | Other acute lower respiratory infections | J20-22 |
| Age_7 | Acute upper respiratory infections | J00-06 | Diseases of oral cavity and salivary glands | K00-14 | Other diseases of upper respiratory tract | J30-39 | Chronic lower respiratory diseases | J40-47 | Other acute lower respiratory infections | J20-22 |
| Age_8 | Acute upper respiratory infections | J00-06 | Diseases of oral cavity and salivary glands | K00-14 | Other diseases of upper respiratory tract | J30-39 | Other acute lower respiratory infections | J20-22 | Chronic lower respiratory diseases | J40-47 |
| Age_9 | Acute upper respiratory infections | J00-06 | Diseases of oral cavity and salivary glands | K00-14 | Other diseases of upper respiratory tract | J30-39 | Other acute lower respiratory infections | J20-22 | Chronic lower respiratory diseases | J40-47 |
| Age_10 | Acute upper respiratory infections | J00-06 | Diseases of oral cavity and salivary glands | K00-14 | Other diseases of upper respiratory tract | J30-39 | Other acute lower respiratory infections | J20-22 | Chronic lower respiratory diseases | J40-47 |
| Age_11 | Acute upper respiratory infections | J00-06 | Other diseases of upper respiratory tract | J30-39 | Diseases of oral cavity and salivary glands | K00-14 | Other acute lower respiratory infections | J20-22 | Disorders of ocular muscles, binocular movement, accommodation, and refraction | H49-52 |
| Age_12 | Acute upper respiratory infections | J00-06 | Other diseases of upper respiratory tract | J30-39 | Diseases of oral cavity and salivary glands | K00-14 | Disorders of ocular muscles, binocular movement, accommodation, and refraction | H49-52 | Other acute lower respiratory infections | J20-22 |
| Age_13 | Acute upper respiratory infections | J00-06 | Other diseases of upper respiratory tract | J30-39 | Diseases of oral cavity and salivary glands | K00-14 | Disorders of ocular muscles, binocular movement, accommodation, and refraction | H49-52 | Other acute lower respiratory infections | J20-22 |
| Age_14 | Acute upper respiratory infections | J00-06 | Other diseases of upper respiratory tract | J30-39 | Diseases of oral cavity and salivary glands | K00-14 | Disorders of ocular muscles, binocular movement, accommodation, and refraction | H49-52 | Other acute lower respiratory infections | J20-22 |
| Age_15 | Acute upper respiratory infections | J00-06 | Disorders of ocular muscles, binocular movement, accommodation, and refraction | H49-52 | Other diseases of upper respiratory tract | J30-39 | Diseases of oral cavity and salivary glands | K00-14 | Other acute lower respiratory infections | J20-22 |
| Age_16 | Acute upper respiratory infections | J00-06 | Disorders of ocular muscles, binocular movement, accommodation, and refraction | H49-52 | Other diseases of upper respiratory tract | J30-39 | Diseases of oral cavity and salivary glands | K00-14 | Other acute lower respiratory infections | J20-22 |
| Age_17 | Acute upper respiratory infections | J00-06 | Disorders of ocular muscles, binocular movement, accommodation, and refraction | H49-52 | Diseases of oral cavity and salivary glands | K00-14 | Other diseases of upper respiratory tract | J30-39 | Dermatitis and eczema | L20-30 |
| Age_18 | Disorders of ocular muscles, binocular movement, accommodation, and refraction | H49-52 | Acute upper respiratory infections | J00-06 | Diseases of oral cavity and salivary glands | K00-14 | Other diseases of upper respiratory tract | J30-39 | Dermatitis and eczema | L20-30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suto, M.; Takehara, K.; Morisaki, N.; Moriichi, A.; Gai, R.; Mori, R. Disease Trends in Children and Adolescents in Japan: A Retrospective Observational Study Using the Nationwide Claims Data for 2012–2016. Children 2024, 11, 81. https://doi.org/10.3390/children11010081
Suto M, Takehara K, Morisaki N, Moriichi A, Gai R, Mori R. Disease Trends in Children and Adolescents in Japan: A Retrospective Observational Study Using the Nationwide Claims Data for 2012–2016. Children. 2024; 11(1):81. https://doi.org/10.3390/children11010081
Chicago/Turabian StyleSuto, Maiko, Kenji Takehara, Naho Morisaki, Akinori Moriichi, Ruoyan Gai, and Rintaro Mori. 2024. "Disease Trends in Children and Adolescents in Japan: A Retrospective Observational Study Using the Nationwide Claims Data for 2012–2016" Children 11, no. 1: 81. https://doi.org/10.3390/children11010081
APA StyleSuto, M., Takehara, K., Morisaki, N., Moriichi, A., Gai, R., & Mori, R. (2024). Disease Trends in Children and Adolescents in Japan: A Retrospective Observational Study Using the Nationwide Claims Data for 2012–2016. Children, 11(1), 81. https://doi.org/10.3390/children11010081






