The Relationship of the PROMIS® Pediatric Physical Activity Measure with Cardiorespiratory Fitness
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Setting
2.2. Measurements
2.2.1. Physical Activity
2.2.2. Self-Efficacy
2.2.3. Step-Test
2.3. Data Analysis
3. Results
3.1. Demographics
3.2. Measurement Scores
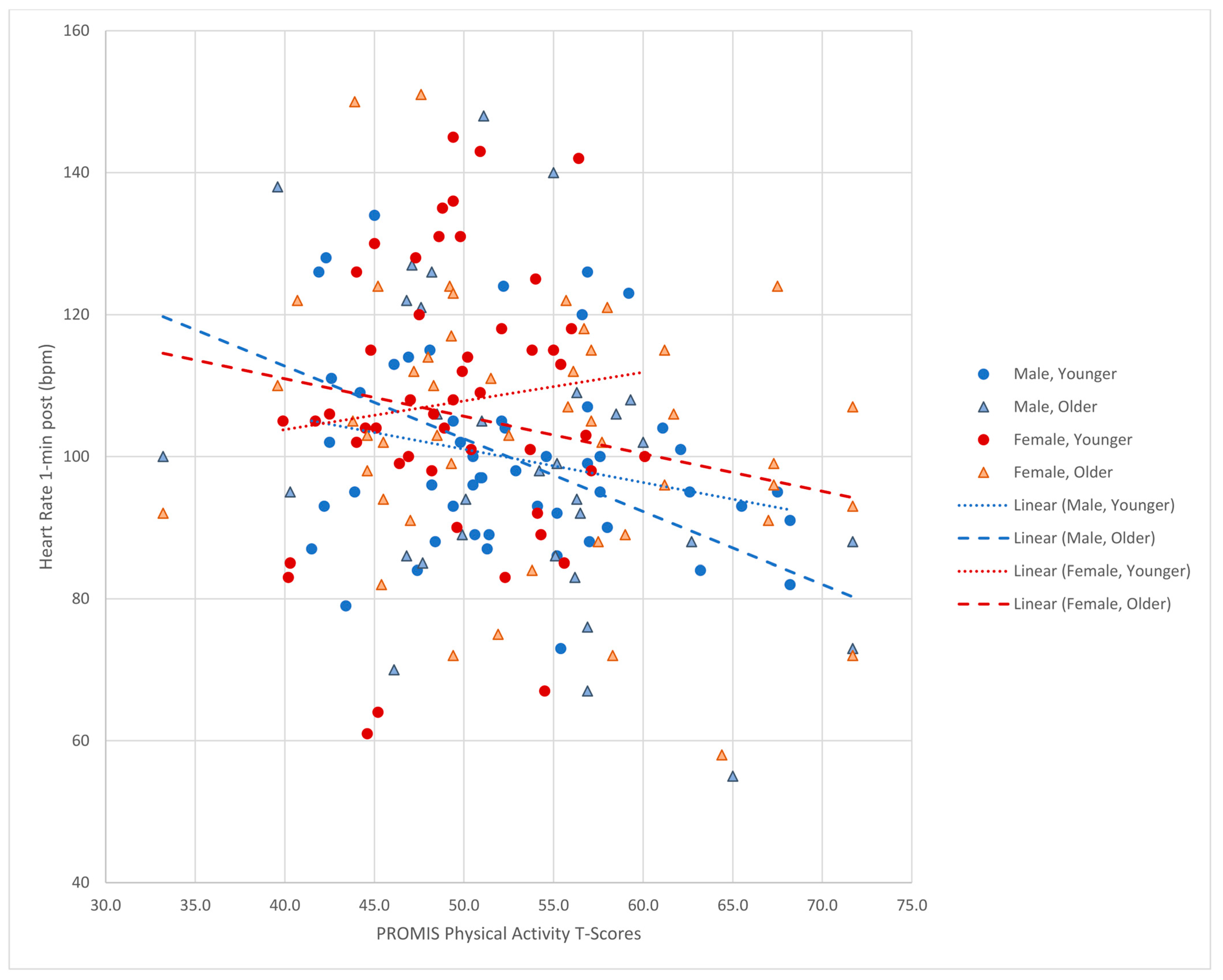
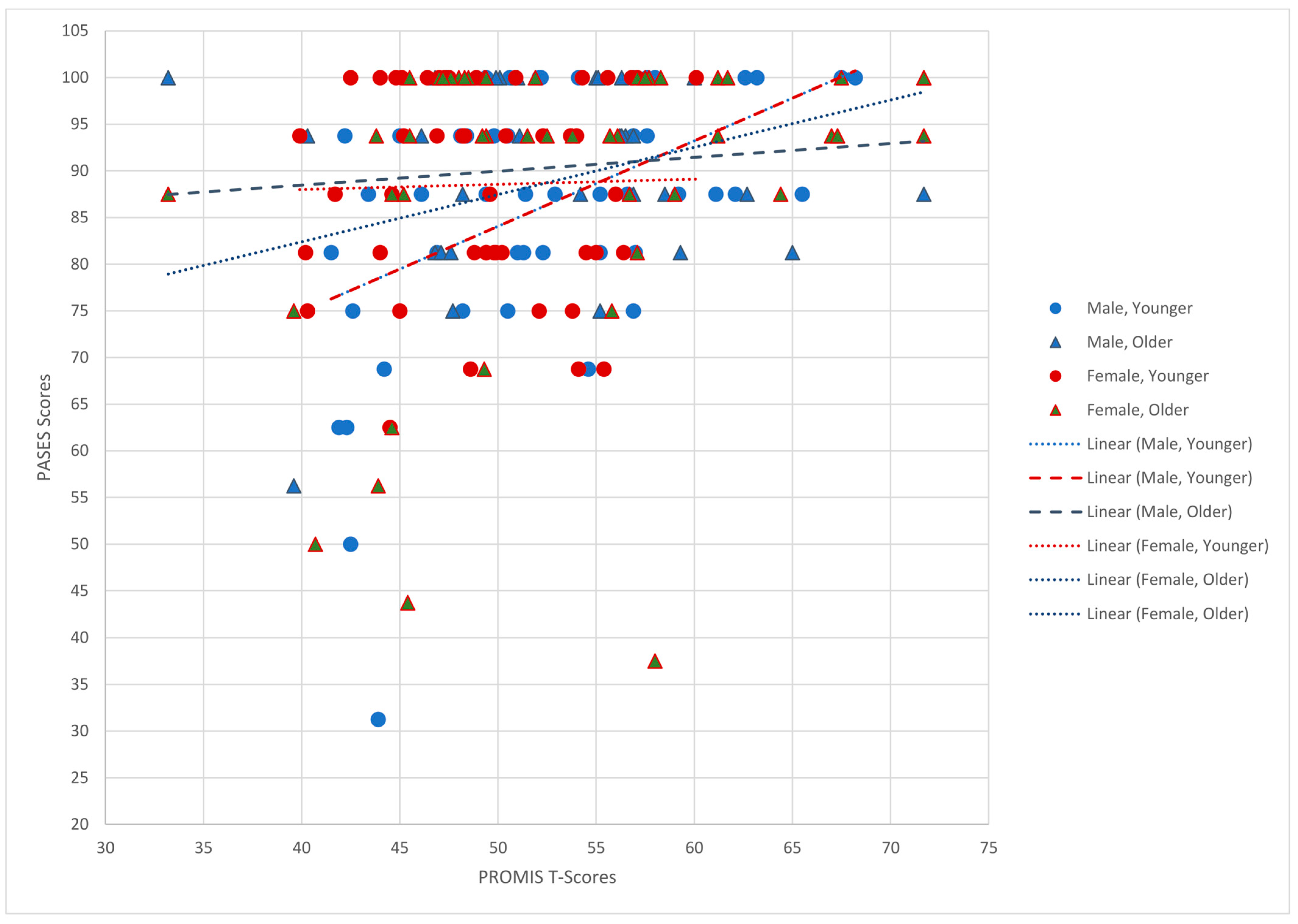
3.3. Relationships among Variables
3.4. Difference between Variables
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- Chaput, J.-P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Jago, R.; Ortega, F.B.; Katzmarzyk, P.T. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: Summary of the evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 141. [Google Scholar] [CrossRef] [PubMed]
- Haskell, W.L. Physical Activity by Self-Report: A Brief History and Future Issues. J. Phys. Act. Health 2012, 9 (Suppl. 1), S5–S10. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, K.K.P.; Morrow, J.R.; Woolsey, A.-L.T. Framework for Physical Activity as a Complex and Multidimensional Behavior. J. Phys. Act. Health 2012, 9 (Suppl. 1), S11–S18. [Google Scholar] [CrossRef] [PubMed]
- Cain, K.L.; Sallis, J.F.; Conway, T.L.; Van Dyck, D.; Calhoon, L. Using Accelerometers in Youth Physical Activity Studies: A Review of Methods. J. Phys. Act. Health 2013, 10, 437–450. [Google Scholar] [CrossRef] [PubMed]
- Feehan, L.M.; Goldsmith, C.H.; Leung, A.Y.F.; Li, L.C. SenseWearMini and Actigraph GT3X Accelerometer Classification of Observed Sedentary and Light-Intensity Physical Activities in a Laboratory Setting. Physiother. Can. 2016, 68, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Sternfeld, B.; Goldman-Rosas, L. A Systematic Approach to Selecting an Appropriate Measure of Self-Reported Physical Activity or Sedentary Behavior. J. Phys. Act. Health 2012, 9 (Suppl. 1), S19–S28. [Google Scholar] [CrossRef]
- Sirard, J.R.; Pate, R.R. Physical Activity Assessment in Children and Adolescents. Sports Med. 2001, 31, 439–454. [Google Scholar] [CrossRef]
- Mâsse, L.C.; de Niet, J.E. Sources of Validity Evidence Needed with Self-Report Measures of Physical Activity. J. Phys. Act. Health 2012, 9 (Suppl. 1), S44–S55. [Google Scholar] [CrossRef]
- Cella, D.; Yount, S.; Rothrock, N.; Gershon, R.; Cook, K.; Reeve, B.; Ader, D.; Fries, J.F.; Bruce, B.; Rose, M. The Patient-Reported Outcomes Measurement Information System (PROMIS®): Progress of an NIH Roadmap cooperative group during its first two years. Med. Care 2007, 45, S3–S11. [Google Scholar] [CrossRef]
- Gershon, R.C.; Rothrock, N.; Hanrahan, R.; Bass, M.; Cella, D. The use of PROMIS and assessment center to deliver patient-reported outcome measures in clinical research. Pediatrics 2010, 11, 304–314. [Google Scholar]
- Broderick, J.; DeWit, E.M.; Rothrock, N.; Crane, P.; Forrest, C.B. Advances in Patient Reported Outcomes: The NIH PROMIS Measures. eGEMs 2013, 1, 12. [Google Scholar] [CrossRef] [PubMed]
- Tucker, C.A.; Bevans, K.B.; Teneralli, R.E.; Smith, A.W.; Bowles, H.R.; Forrest, C.B. Self-reported Pediatric Measures of Physical Activity, Sedentary Behavior, and Strength Impact for PROMIS: Conceptual framework. Pediatr. Phys. Ther. 2014, 26, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Tucker, C.A.; Bevans, K.B.; Teneralli, R.E.M.; Smith, A.W.P.; Bowles, H.R.; Forrest, C.B. Self-reported Pediatric Measures of Physical Activity, Sedentary Behavior, and Strength Impact for PROMIS: Item development. Pediatr. Phys. Ther. 2014, 26, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Tucker, C.A.; Bevans, K.B.; Becker, B.D.; Teneralli, R.; Forrest, C.B. Development of the PROMIS Pediatric Physical Activity Item Banks. Phys. Ther. 2020, 100, 1393–1410. [Google Scholar] [CrossRef] [PubMed]
- Algheryafi, R.A.; Bevans, K.B.; Hiremath, S.V.; Lai, J.-S.; Tucker, C.A. Convergent Validity of the Patient Reported Outcome Measurement Information System-Pediatric Physical Activity Instrument (PROMIS®-PA) with Wearable Devices in Adolescents. Children 2023, 10, 940. [Google Scholar] [CrossRef]
- Bennett, H.; Parfitt, G.; Davison, K.; Eston, R. Validity of Submaximal Step Tests to Estimate Maximal Oxygen Uptake in Healthy Adults. Sports Med. 2016, 46, 737–750. [Google Scholar] [CrossRef]
- Jamnick, N.A.; By, S.; Pettitt, C.D.; Pettitt, R.W. Comparison of the YMCA and a Custom Submaximal Exercise Test for Determining V˙O2max. Med. Sci. Sports Exerc. 2016, 48, 254–259. [Google Scholar] [CrossRef]
- Jankowski, M.; Niedzielska, A.; Brzezinski, M.; Drabik, J. Cardiorespiratory Fitness in Children: A Simple Screening Test for Population Studies. Pediatr. Cardiol. 2015, 36, 27–32. [Google Scholar] [CrossRef]
- Hayes, R.M.; Maldonado, D.; Gossett, T.; Shepherd, T.; Mehta, S.P.; Flesher, S.L. Developing and Validating a Step Test of Aerobic Fitness among Elementary School Children. Physiother. Can. 2019, 71, 187–194. [Google Scholar] [CrossRef]
- Armstrong, N. Top 10 Research Questions Related to Youth Aerobic Fitness. Res. Q. Exerc. Sport 2017, 88, 130–148. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Hammond-Bennett, A.; Hypnar, A.; Mason, S. Health-related physical fitness and physical activity in elementary school students. BMC Public Health 2018, 18, 195. [Google Scholar] [CrossRef] [PubMed]
- Burden, S.J.; Weedon, B.D.; Turner, A.; Whaymand, L.; Meaney, A.; Dawes, H.; Jones, A. Intensity and Duration of Physical Activity and Cardiorespiratory Fitness. Pediatrics 2022, 150, e2021056003. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Encyclopedia of Human Behavior. 1994. Available online: https://www.uky.edu/~eushe2/Bandura/BanEncy.html#sources (accessed on 8 June 2023).
- Wójcicki, T.R.; McAuley, E., II. Physical activity: Measurement and behavioral patterns in children and youth. Monogr. Soc. Res. Child Dev. 2014, 79, 7–24. [Google Scholar] [CrossRef] [PubMed]
- Strauss, R.S.; Rodzilsky, D.; Burack, G.; Colin, M. Psychosocial correlates of physical activity in healthy children. Arch. Pediatr. Adolesc. Med. 2001, 155, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Annesi, J.J. Relations of physical self-concept and self-efficacy with frequency of voluntary physical activity in preadolescents: Implications for after-school care programming. J. Psychosom. Res. 2006, 61, 515–520. [Google Scholar] [CrossRef]
- Sallis, J.F.; Prochaska, J.J.; Taylor, W.C. A review of correlates of physical activity of children and adolescents. Med. Sci. Sports Exerc. 2000, 32, 963–975. [Google Scholar] [CrossRef]
- Peers, C.; Issartel, J.; Behan, S.; O’Connor, N.; Belton, S. Movement competence: Association with physical self-efficacy and physical activity. Hum. Mov. Sci. 2020, 70, 102582. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. BMI Percentile Calculator for Child and Teen. Available online: https://www.cdc.gov/healthyweight/bmi/calculator.html (accessed on 8 June 2023).
- Suton, D.; Pfeiffer, K.A.; Feltz, D.L.; Yee, K.E.; Eisenmann, J.C.; Carlson, J.J. Physical Activity and Self-efficacy in Normal and Over-fat Children. Am. J. Health Behav. 2013, 37, 635–640. [Google Scholar] [CrossRef]
- University of Minnesota D2D: The Driven to Discover Research Facility. Available online: http://d2d.umn.edu/ (accessed on 18 October 2023).
- Bartholomew, J.B.; Loukas, A.; Jowers, E.M.; Allua, S. Validation of the Physical Activity Self-Efficacy Scale: Testing Measurement Invariance between Hispanic and Caucasian Children. J. Phys. Act. Health 2006, 3, 70–78. [Google Scholar] [CrossRef]
- National Institutes of Health. American Medical Associations’ Age Designations. Available online: https://www.nih.gov/nih-style-guide/age (accessed on 21 October 2023).
- United States Census Bureau. Quick facts Minnesota V. 2022. Available online: https://www.census.gov/quickfacts/MN (accessed on 8 June 2023).
- Fryar, C.D.; Carroll, M.D.; Afful, J. Prevalence of Overweight, Obesity, and Severe Obesity among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 through 2017–2018. CDC. Available online: https://www.cdc.gov/nchs/data/hestat/obesity-child-17-18/obesity-child.htm (accessed on 8 June 2023).
- Minnesota State Fair. Available online: https://www.mnstatefair.org/general-info/history-overview/ (accessed on 18 October 2023).
- Spence, J.C.; Blanchard, C.M.; Clark, M.; Plotnikoff, R.C.; Storey, K.E.; McCargar, L. The Role of Self-Efficacy in Explaining Gender Differences in Physical Activity Among Adolescents: A Multilevel Analysis. J. Phys. Act. Health 2010, 7, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Trost, S.; Kerr, L.; Ward, D.; Pate, R. Physical activity and determinants of physical activity in obese and non-obese children. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 822–829. [Google Scholar] [CrossRef] [PubMed]
- Jakubowski, T.L.; Faigenbaum, A.D.; Lindberg, C. Increasing Physical Activity in Children: From evidence to action. MCN Am. J. Matern. Nurs. 2015, 40, 213–219. [Google Scholar] [CrossRef]
- Sember, V.; Jurak, G.; Kovač, M.; Đurić, S.; Starc, G. Decline of physical activity in early adolescence: A 3-year cohort study. PLoS ONE 2020, 15, e0229305. [Google Scholar] [CrossRef]
- Farooq, M.A.; Parkinson, K.N.; Adamson, A.J.; Pearce, M.S.; Reilly, J.K.; Hughes, A.R.; Janssen, X.; Basterfield, L.; Reilly, J.J. Timing of the decline in physical activity in childhood and adolescence: Gateshead Millennium Cohort Study. Br. J. Sports Med. 2018, 52, 1002–1006. [Google Scholar] [CrossRef]
| Characteristic | n | % |
|---|---|---|
| Sex | ||
| Male | 85 | 47 |
| Female | 97 | 53 |
| Race | ||
| White | 164 | 90 |
| Asian | 9 | 5 |
| Black-African/American & White | 4 | 2 |
| Black-African/American | 3 | 2 |
| Asian & White | 2 | 1 |
| Ethnicity | ||
| Hispanic/Latino | 6 | 3 |
| Non-Hispanic | 176 | 97 |
| RUCA * | ||
| 1 | 140 | |
| 2 | 29 | |
| 3 | 1 | |
| 4 | 5 | |
| 7 | 1 | |
| 9 | 1 | |
| 10 | 5 | |
| Weight status by BMI percentile | ||
| Underweight | 6 | 3 |
| Healthy weight | 134 | 74 |
| Overweight | 23 | 13 |
| Obese | 19 | 10 |
| Age group | ||
| School-age (8 to 12 years) | 103 | 57 |
| Male | 53 | 29 |
| Female | 50 | 27 |
| Adolescent (13 to 18 years) | 79 | 43 |
| Male | 32 | 18 |
| Female | 47 | 26 |
| M | Range | |
| Age | 12.2 | 8–18 |
| BMI percentile | 53.4 | 3–99 |
| Measurement | M | Range | SD |
|---|---|---|---|
| PROMIS® PA a T Score | 52.13 | 33.2–71.7 | 7.58 |
| Heart rate 1 min post step test | 103.39 | 55–222 | 20.25 |
| PASES b summed score | 14.15 | 5–16 | 2.10 |
| Variable | Heart Rate b | PASES c Summed Score |
|---|---|---|
| PROMIS® PA a T score All (n = 182) | −0.23 ** | 0.27 ** |
| PROMIS® PA a T score Males Age 13 to 18 years (n = 32) | −0.35 * | 0.12 |
| PROMIS® PA a T score Female Age 13 to 18 years (n = 47) | −0.25 | 0.29 |
| PROMIS® PA a T score Males Age 8 to 12 years (n = 53) | −0.26 | 0.46 * |
| PROMIS® PA a T score Females Age 8 to 12 years (n = 50) | 0.10 | 0.02 |
| Characteristic | PROMIS® PA a T Score | PASES b Summed Score | Heart Rate c | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| Male (n = 85) | 52.82 | 7.58 | 14.07 | 2.06 | 100.78 | 21.41 |
| Female (n = 97) | 51.52 | 7.56 | 14.23 | 2.13 | 105.68 | 18.98 |
| Difference p value | 0.25 | 0.62 | 0.10 | |||
| Age 8 to 12 years (n = 103) | 51.22 | 6.52 | 14.01 | 2.02 | 103.75 | 17.00 |
| Age 13 to 18 years (n = 79) | 53.30 | 8.66 | 14.34 | 2.19 | 102.92 | 23.93 |
| Difference p value | 0.07 | 0.29 | 0.79 | |||
| Under weight (n = 6) | 52.37 | 4.89 | 14.67 | 2.16 | 110.50 | 17.29 |
| Healthy weight (n = 134) | 52.42 | 7.88 | 14.29 | 2.01 | 101.01 | 19.83 |
| Overweight (n = 23) | 51.11 | 8.10 | 14.04 | 2.53 | 102.91 | 20.02 |
| Obese (n = 19) | 51.17 | 5.30 | 13.16 | 1.95 | 118.53 | 18.50 |
| Difference p value | 0.82 | 0.15 | <0.01 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tucker, C.A.; Lawrence, H.S.; Hooke, M.C. The Relationship of the PROMIS® Pediatric Physical Activity Measure with Cardiorespiratory Fitness. Children 2024, 11, 22. https://doi.org/10.3390/children11010022
Tucker CA, Lawrence HS, Hooke MC. The Relationship of the PROMIS® Pediatric Physical Activity Measure with Cardiorespiratory Fitness. Children. 2024; 11(1):22. https://doi.org/10.3390/children11010022
Chicago/Turabian StyleTucker, Carole A., Hannah S. Lawrence, and Mary C. Hooke. 2024. "The Relationship of the PROMIS® Pediatric Physical Activity Measure with Cardiorespiratory Fitness" Children 11, no. 1: 22. https://doi.org/10.3390/children11010022
APA StyleTucker, C. A., Lawrence, H. S., & Hooke, M. C. (2024). The Relationship of the PROMIS® Pediatric Physical Activity Measure with Cardiorespiratory Fitness. Children, 11(1), 22. https://doi.org/10.3390/children11010022





