Characteristics of Adolescents Admitted with Acute Alcohol Intoxication: A Retrospective Multicentre Study in Antwerp, Belgium, in the Period 2015–2021
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection
2.4. Statistical Analysis
3. Results
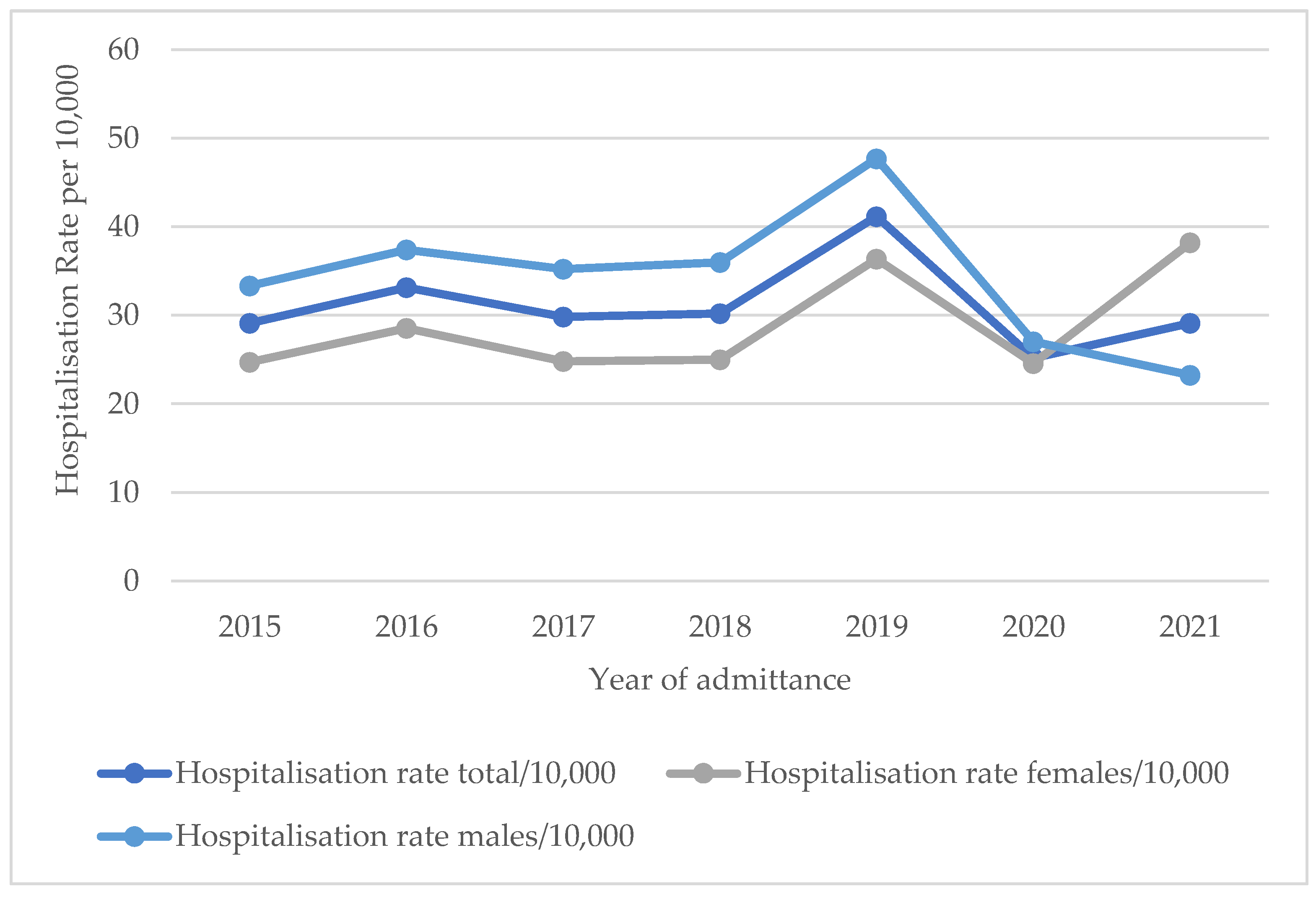
3.1. Hospitalisation Rate
3.2. General Characteristics
3.3. Recurrence Rate
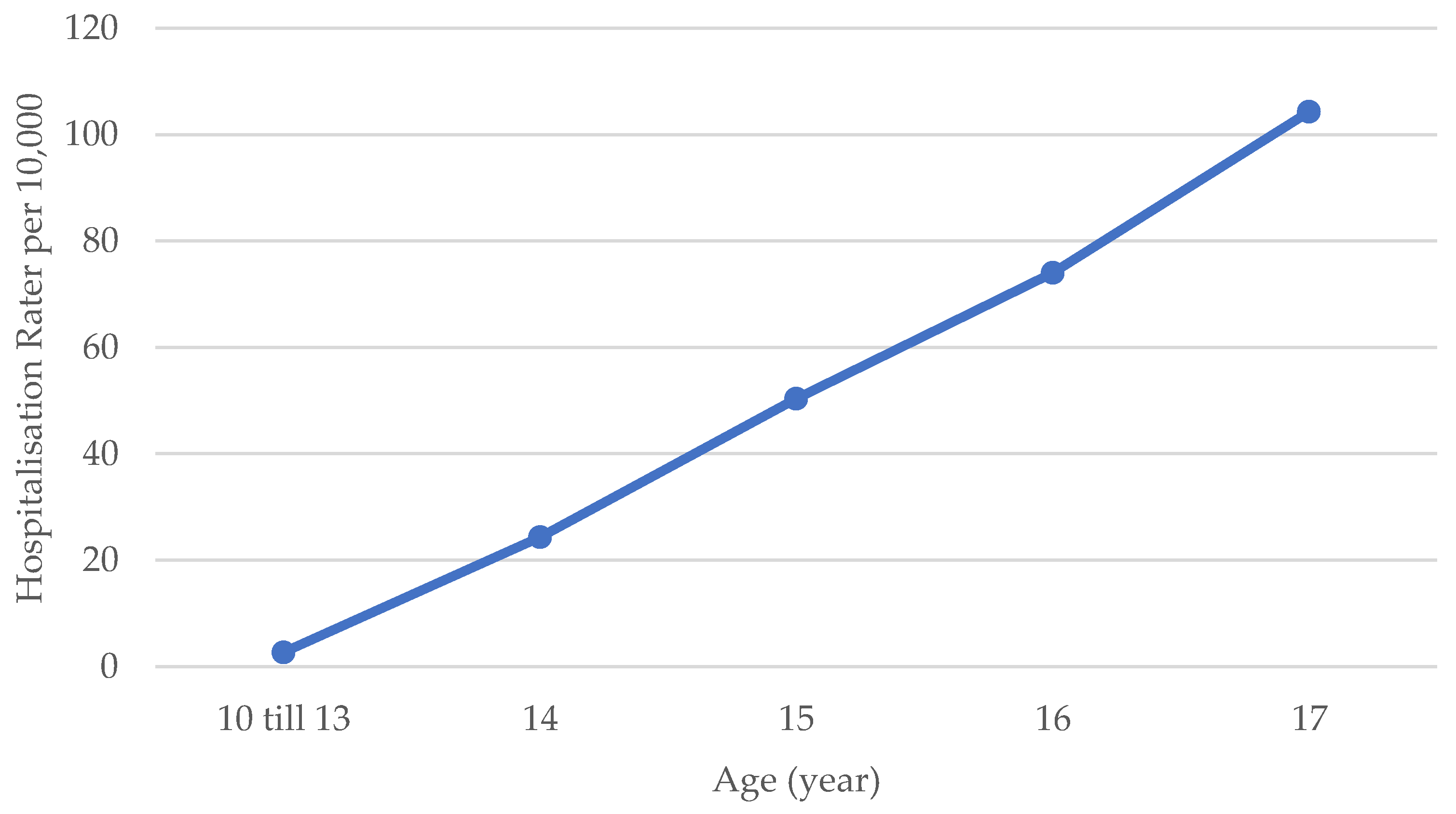
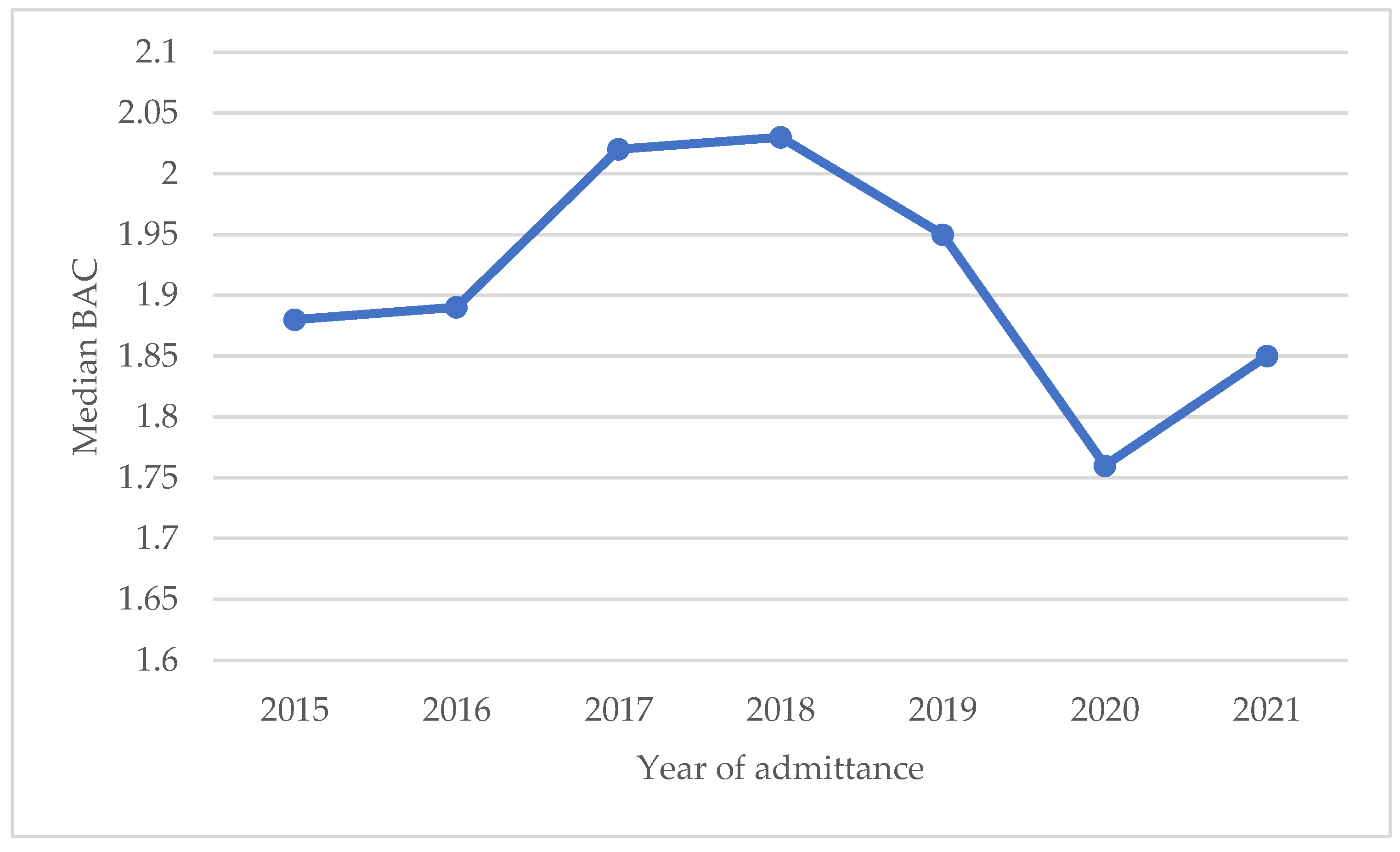
3.4. Severeness of AAI
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shield, K.; Manthey, J.; Rylett, M.; Probst, C.; Wettlaufer, A.; Parry, C.D.H.; Rehm, J. National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: A comparative risk assessment study. Lancet Public Health 2020, 5, e51–e61. [Google Scholar] [CrossRef]
- Casey, B.J.; Jones, R.M. Neurobiology of the adolescent brain and behavior: Implications for substance use disorders. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 1189–1201. [Google Scholar] [CrossRef]
- Sawyer, S.M.; Azzopardi, P.S.; Wickremarathne, D.; Patton, G.C. The age of adolescence. Lancet Child Adolesc. Health 2018, 2, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Report to Congress on the Prevention and Reduction of Underage Drinking; Department of Health and Human Services U.S., Substance Abuse and Mental Health Services Administration (SAMHSA): Washington, DC, USA, 2020.
- Van Deun, P. Alcohol en jongeren. Visietekst; Vlaams expertisecentrum Alcohol en andere Drugs (VAD): Brussel, Belgium, 2016. [Google Scholar]
- Vonghia, L.; Leggio, L.; Ferrulli, A.; Bertini, M.; Gasbarrini, G.; Addolorato, G. Acute alcohol intoxication. Eur. J. Intern. Med. 2008, 19, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Inchley, J.; Currie, D.; Budisavljevic, S.; Torsheim, T.; Jåstad, A.; Cosma, A.; Kelly, C.; Arnarsson, Á.M.; Barnekow, V.; Weber, M.M. (Eds.) Spotlight on Adolescent Health and Well-Being. Findings from the 2017/2018 Health Behaviour in School-Aged Children (HBSC) Survey in Europe and Canada. International Report. Volume 1. Key Findings; WHO Regional Office for Europe: Copenhagen, Denmark, 2020. [Google Scholar]
- Rosiers, J. VAD-Leerlingenbevraging In het kader van een Drugbeleid op School. Syntheserapport Schooljaar 2018–2019; VAD: Brussel, Belgium, 2020. [Google Scholar]
- Gisle, L.; Demarest, S.; Drieskens, S. Gezondheidsenquête 2018: Gebruik van Alcohol; Rapportnummer: D/2019/14.440/56; Sciensano: Brussel, Belgium, 2018. [Google Scholar]
- Miller, J.W.; Naimi, T.S.; Brewer, R.D.; Jones, S.E. Binge drinking and associated health risk behaviors among high school students. Pediatrics 2007, 119, 76–85. [Google Scholar] [CrossRef]
- Ewing, S.W.; Sakhardande, A.; Blakemore, S.J. The effect of alcohol consumption on the adolescent brain: A systematic review of MRI and fMRI studies of alcohol-using youth. Neuroimage Clin. 2014, 5, 420–437. [Google Scholar] [CrossRef]
- Bonomo, Y.A.; Bowes, G.; Coffey, C.; Carlin, J.B.; Patton, G.C. Teenage drinking and the onset of alcohol dependence: A cohort study over seven years. Addiction 2004, 99, 1520–1528. [Google Scholar] [CrossRef]
- Connor, J. Alcohol consumption as a cause of cancer. Addiction 2017, 112, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Praud, D.; Rota, M.; Rehm, J.; Shield, K.; Zatoński, W.; Hashibe, M.; La Vecchia, C.; Boffetta, P. Cancer incidence and mortality attributable to alcohol consumption. Int. J. Cancer 2016, 138, 1380–1387. [Google Scholar] [CrossRef]
- Turning Down the Alcohol Flow. Background Document on the European Framework for Action on Alcohol, 2022–2025; WHO Regional Office for Europe: Copenhagen, Denmark, 2022.
- Verniest, R.; Callens, M. Alcoholgebruik bij jongeren in België is verontrustend. CM-Informatie 2020, 279, 20–25. [Google Scholar]
- Stad in Cijfers: Statistieken over de stad Antwerpen. Available online: https://stadincijfers.antwerpen.be/databank (accessed on 25 January 2023).
- Trefan, L.; Gartner, A.; Alcock, A.; Farewell, D.; Morgan, J.; Fone, D.; Paranjothy, S. Epidemiology of alcohol-related emergency hospital admissions in children and adolescents: An e-cohort analysis in Wales in 2006–2011. PLoS ONE 2019, 14, e0217598. [Google Scholar] [CrossRef]
- Green, M.A.; Strong, M.; Conway, L.; Maheswaran, R. Trends in alcohol-related admissions to hospital by age, sex and socioeconomic deprivation in England, 2002/03 to 2013/14. BMC Public Health 2017, 17, 412. [Google Scholar] [CrossRef] [PubMed]
- Van Zanten, E.; Van der Ploeg, T.; Van Hoof, J.J.; Van der Lely, N. Gender, age, and educational level attribute to blood alcohol concentration in hospitalized intoxicated adolescents; a cohort study. Alcohol. Clin. Exp. Res. 2013, 37, 1188–1194. [Google Scholar] [CrossRef] [PubMed]
- de Veld, L.; van Hoof, J.J.; Ouwehand, S.; van der Lely, N. Age at First Alcohol Use as a Possible Risk Factor for Adolescent Acute Alcohol Intoxication Hospital Admission in the Netherlands. Alcohol. Clin. Exp. Res. 2020, 44, 219–224. [Google Scholar] [CrossRef]
- Weinberg, L.; Wyatt, J.P. Children presenting to hospital with acute alcohol intoxication. Emerg. Med. J. 2006, 23, 774–776. [Google Scholar] [CrossRef]
- Rosiers, J. Syntheserapport Leerlingenbevraging 2000–2019. Evoluties en Inzichten; VAD: Brussel, Belgium, 2021. [Google Scholar]
- Pigeaud, L.; de Veld, L.; van Hoof, J.; van der Lely, N. Acute Alcohol Intoxication in Dutch Adolescents Before, During, and After the First COVID-19 Lockdown. J. Adolesc. Health 2021, 69, 905–909. [Google Scholar] [CrossRef]
- Grigoletto, V.; Cognigni, M.; Occhipinti, A.A.; Abbracciavento, G.; Carrozzi, M.; Barbi, E.; Cozzi, G. Rebound of Severe Alcoholic Intoxications in Adolescents and Young Adults After COVID-19 Lockdown. J. Adolesc. Health 2020, 67, 727–729. [Google Scholar] [CrossRef] [PubMed]
- van Hoof, J.; van Zanten, E.; van der Lely, N. Four Years of Reports of Alcohol-Related Harm to Pediatricians in the Netherlands. J. Child Adoles. Subst. 2015, 24, 191–197. [Google Scholar] [CrossRef]
- Nienhuis, K.; Van der Lely, N.; van Hoof, J. Ten Years of Alcohol Intoxication in Adolescents and Treatment in Paediatric Departments in Dutch Hospitals. J. Addict. Res. 2017, 1, D2384. [Google Scholar]
- Newton-Howes, G.; Cook, S.; Martin, G.; Foulds, J.A.; Boden, J.M. Comparison of age of first drink and age of first intoxication as predictors of substance use and mental health problems in adulthood. Drug Alcohol Depend. 2019, 194, 238–243. [Google Scholar] [CrossRef]
- Dawson, D.A.; Goldstein, R.B.; Chou, S.P.; Ruan, W.J.; Grant, B.F. Age at first drink and the first incidence of adult-onset DSM-IV alcohol use disorders. Alcohol. Clin. Exp. Res. 2008, 32, 2149–2160. [Google Scholar] [CrossRef] [PubMed]
- Lovrecic, M.; Lovrecic, B.; Rok Simon, M.; Korosec, A.; Della Rocca, F.; Maremmani, A.G.I.; Maremmani, I. Trends of Hospitalization for Acute Alcohol Intoxication in Slovenian Children and Adolescents with and without Dual Disorder. Implications for a Correct Intervention. J. Clin. Med. 2020, 9, 2122. [Google Scholar] [CrossRef] [PubMed]
- Pawlowska-Kamieniak, A.; Mroczkowska-Juchkiewicz, A.; Kominek, K.; Krawiec, P.; Mełges, B.; Pac-Kożuchowska, E. Alcohol intoxication among adolescents and children in urban and rural environments—A retrospective analysis. Ann. Agric. Environ. Med. 2018, 25, 1–3. [Google Scholar] [CrossRef]
- Raimondo Maria, P.; Domenicali, M.; Marani, S.; Caputo, F.; Mazzoni, M. Visits of adolescents for acute alcohol intoxication to emergency departments in Northern Italy: Natives and non-natives. J. Subst. Use 2019, 25, 118–122. [Google Scholar] [CrossRef]
- Rodrigues, M.; Pontes, T.; Almeida, J.; Estrada, A.; Carvalho, S. Alcohol use in adolescence: 5 years admissions at a pediatric emergency department. Int. J. Adolesc. Med. Health 2018, 32, 20170166. [Google Scholar] [CrossRef]
- Christie, D.; Viner, R. Adolescent development. BMJ 2005, 330, 301–304. [Google Scholar] [CrossRef]
- Loukova, A. Study of acute alcohol poisoning in Children admitted to a emergency hospital Pirogov in Sofia, Bulgaria. Maced. J. Med. Sci. 2011, 4, 275–280. [Google Scholar] [CrossRef]
- Kuzelová, M.; Harárová, A.; Ondriasová, E.; Wawruch, M.; Riedel, R.; Benedeková, M.; Kovács, L.; Plaková, S. Alcohol intoxication requiring hospital admission in children and adolescents: Retrospective analysis at the University Children’s Hospital in the Slovak Republic. Clin. Toxicol. 2009, 47, 556–561. [Google Scholar] [CrossRef]
- van Hoof, J.J.; Van Der Lely, N.; Bouthoorn, S.H.; Van Dalen, W.E.; Pereira, R.R. Adolescent alcohol intoxication in the Dutch hospital departments of pediatrics: A 2-year comparison study. J. Adolesc. Health 2011, 48, 212–214. [Google Scholar] [CrossRef] [PubMed]
- Sanvisens, A.; Sanjeevan, I.; Zuluaga, P.; Túnez, A.; de Francisco, A.; Papaseit, E.; García-Eroles, L.; Muga, R. Five-Year Incidence of Hospital-Based Emergencies Related to Acute Recreational Intoxication in Minors. Alcohol. Clin. Exp. Res. 2019, 43, 2179–2186. [Google Scholar] [CrossRef] [PubMed]
| Year of Admittance | Median Age (Years) [IQR] | Minimum Age | Maximum Age |
|---|---|---|---|
| 2015 | 16.8 [15.9–17.5] | 12.6 | 17.9 |
| 2016 | 16.8 [15.8–17.4] | 13.1 | 17.9 |
| 2017 | 16.8 [15.4–17.5] | 13.4 | 17.9 |
| 2018 | 16.7 [15.5–17.4] | 13.0 | 17.9 |
| 2019 | 16.5 [15.5–17.4] | 11.7 | 17.9 |
| 2020 | 16.3 [15.3–17.2] | 11.1 | 17.9 |
| 2021 | 16.5 [15.4–17.2] | 11.2 | 17.9 |
| Characteristic | Total Group of Patients |
|---|---|
| n = 1016 | |
| Sex, n (%) | |
| Male | 572 (56.3) |
| Female | 444 (43.7) |
| Age (years) | |
| Median [IQR] | 16.6 [15.6–17.4] |
| Range | 11.1–17.9 |
| Year of admission, n (%) | |
| 2015 | 126 (12.4) |
| 2016 | 146 (14.4) |
| 2017 | 135 (13.3) |
| 2018 | 141 (13.9) |
| 2019 | 197 (19.4) |
| 2020 | 124 (12.2) |
| 2021 | 147 (14.5) |
| Blood alcohol concentration (BAC, g/L), (n = 841) | |
| Median [IQR] | 1.95 [1.40–2.34] |
| Range | 0.03–4.09 |
| Urine drug screening (n = 308), n(%) | |
| Negative | 254 (82.5) |
| Positive for cannabis | 35 (11.4) |
| Positive for cocaine | 3 (1.0) |
| Positive for XTC/amphetamines | 17 (5.5) |
| Positive for benzodiazepines | 12 (3.9) |
| Glasgow Coma Scale (GCS, points), (n = 839) | |
| Median [IQR] | 14 [12–15] |
| Range | 3–15 |
| 3–14 points, n(%) | 431 (51.4) |
| 15 points, n(%) | 408 (48.6) |
| Duration of stay (hours) (n = 1015) | |
| Median [IQR] | 7.5 [4–11.5] |
| Range | <0.5–549 |
| <24 h, n(%) | 906 (89.3) |
| Reason for admittance (900), n (%) | |
| Reduced consciousness | 453 (50.3) |
| (Traffic) accident | 125 (13.9) |
| Other (somatic/psychiatric) | 322 (35.8) |
| Decreased consciousness, n (%) | |
| GCS ≤ 14 and/or reason for admittance = reduced consciousness | 566 (55.7) |
| Time of admittance, n (%) | |
| Night (0:00–6:00 a.m.) | 555 (54.6) |
| Morning (6:00 a.m.–12:00) | 45 (4.4) |
| Afternoon (12:00–6:00 p.m.) | 89 (8.8) |
| Evening (6:00 p.m.–0:00) | 327 (32.3) |
| Day of admittance, n (%) | |
| Monday–Thursday | 300 (29.5) |
| Friday–Sunday | 716 (70.5) |
| Intensive care unit (ICU), n (%) | |
| Admittance at ICU | 56 (5.5) |
| Transport to emergency department (ED, n = 824), n(%) | |
| Ambulance | 539 (65.4) |
| Ambulance with specialised care | 147 (17.8) |
| Police car | 9 (1.1) |
| Attended by themselves | 12 (1.5) |
| Attended with family or friends | 117 (14.2) |
| Police involvement, n (%) | |
| 155 (15.3) | |
| Referral after admittance (n = 697), n (%) | |
| None | 509 (73) |
| Paediatrician | 25 (3.6) |
| General practitioner | 48 (6.9) |
| Psychosocial assistance | 32 (4.6) |
| Child and adolescent psychiatry | 63 (9.0) |
| Addiction care | 7 (1.0) |
| Characteristic | n (% of total) | Median BAC (g/L) [IQR] | Univariate p-Value |
|---|---|---|---|
| Total | 841 (82.8) | 1.95 [1.4–2.3] | |
| Age (year) | <0.001 * | ||
| 10–13 | 44 (93.6) | 1.39 [0.06–1.93] | |
| 14 | 84 (86.6) | 1.79 [1.24–2.2] | |
| 15 | 158 (81.0) | 1.86 [1.38–2.2] | |
| 16 | 228 (80.9) | 1.99 [1.50–2.36] | |
| 17 | 327 (82.8) | 2.03 [1.56–2.44] | |
| Sex | 0.03 * | ||
| Male | 479 (83.7) | 1.99 [1.48–2.37] | |
| Female | 362 (81.5) | 1.85 [1.33–2.30] | |
| Combined drugs use | <0.001 * | ||
| No combined drug use | 233 (95.1) | 1.91 [1.43–2.39] | |
| Unknown | 523 (78.3) | 1.99 [1.48–2.37] | |
| Combined drug use | 84 (82.4) | 1.60 [0.97–2.03] | |
| Reason for admittance | <0.001 * | ||
| (Traffic) accident | 108 (86.4) | 0.78 [0.06–2.14] | |
| Other (somatic/psychiatric) | 249 (77.3) | 1.60 [0.85–2.05] | |
| Unknown | 95 (81.9) | 2.01 [1.65–2.37] | |
| Reduced consciousness | 389 (85.9) | 2.13 [1.77–2.48] | |
| Type of transport | 0.28 | ||
| Without ambulance | 295 (89.4) | 1.88 [1.31–2.30] | |
| Ambulance | 546 (79.6) | 1.98 [1.46–2.37] | |
| Location of drinking | 0.08 | ||
| At home (or at another person’s home) | 66 (88.0) | 1.94 [1.36–2.38] | |
| In public | 60 (85.7) | 2.12 [1.59–2.37] | |
| At school/work | 19 (76.0) | 2.11 [1.58–2.77] | |
| Youth organisation/sports club | 33 (82.5) | 2.26 [1.79–2.51] | |
| Commercial/event | 152 (84.4) | 2.13 [1.78–2.49] | |
| Day of admittance | 0.001 * | ||
| Monday-Thursday | 260 (86.7) | 1.81 [1.03–2.27] | |
| Friday-Sunday | 581 (81.1) | 1.99 [1.50–2.37] |
| Variable | B Unstandardised Regression Coefficient | 95% Confidence Interval | Multiple Regression p-Value |
|---|---|---|---|
| Age | 0.145 | [0.107, 0.183] | <0.001 * |
| Sex | −0.064 | [−0.161, 0.034] | 0.2 |
| Combined drug use | −0.236 | [−0.401, −0.072] | 0.005 * |
| Reason for admittance | 0.683 | [0.597, 0.769] | <0.001 * |
| Day of admittance | 0.081 | [−0.24, 0.186] | 0.13 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Roozendaal, H.; Verhulst, S.; Glazemakers, I.; De Meulder, F.; Vander Auwera, A.; Bael, A.; Van Damme, E.; Vlemincx, I.; De Dooy, J.; van der Lely, N.; et al. Characteristics of Adolescents Admitted with Acute Alcohol Intoxication: A Retrospective Multicentre Study in Antwerp, Belgium, in the Period 2015–2021. Children 2023, 10, 1378. https://doi.org/10.3390/children10081378
van Roozendaal H, Verhulst S, Glazemakers I, De Meulder F, Vander Auwera A, Bael A, Van Damme E, Vlemincx I, De Dooy J, van der Lely N, et al. Characteristics of Adolescents Admitted with Acute Alcohol Intoxication: A Retrospective Multicentre Study in Antwerp, Belgium, in the Period 2015–2021. Children. 2023; 10(8):1378. https://doi.org/10.3390/children10081378
Chicago/Turabian Stylevan Roozendaal, Hanna, Stijn Verhulst, Inge Glazemakers, Frederic De Meulder, Ann Vander Auwera, Anna Bael, Emmi Van Damme, Ilse Vlemincx, Jozef De Dooy, Nico van der Lely, and et al. 2023. "Characteristics of Adolescents Admitted with Acute Alcohol Intoxication: A Retrospective Multicentre Study in Antwerp, Belgium, in the Period 2015–2021" Children 10, no. 8: 1378. https://doi.org/10.3390/children10081378
APA Stylevan Roozendaal, H., Verhulst, S., Glazemakers, I., De Meulder, F., Vander Auwera, A., Bael, A., Van Damme, E., Vlemincx, I., De Dooy, J., van der Lely, N., & Van Hal, G. (2023). Characteristics of Adolescents Admitted with Acute Alcohol Intoxication: A Retrospective Multicentre Study in Antwerp, Belgium, in the Period 2015–2021. Children, 10(8), 1378. https://doi.org/10.3390/children10081378







