Pediatric Trauma and Trauma Team Activation in a Swiss Pediatric Emergency Department: An Observational Cohort Study
Abstract
1. Background
2. Methods
2.1. Setting
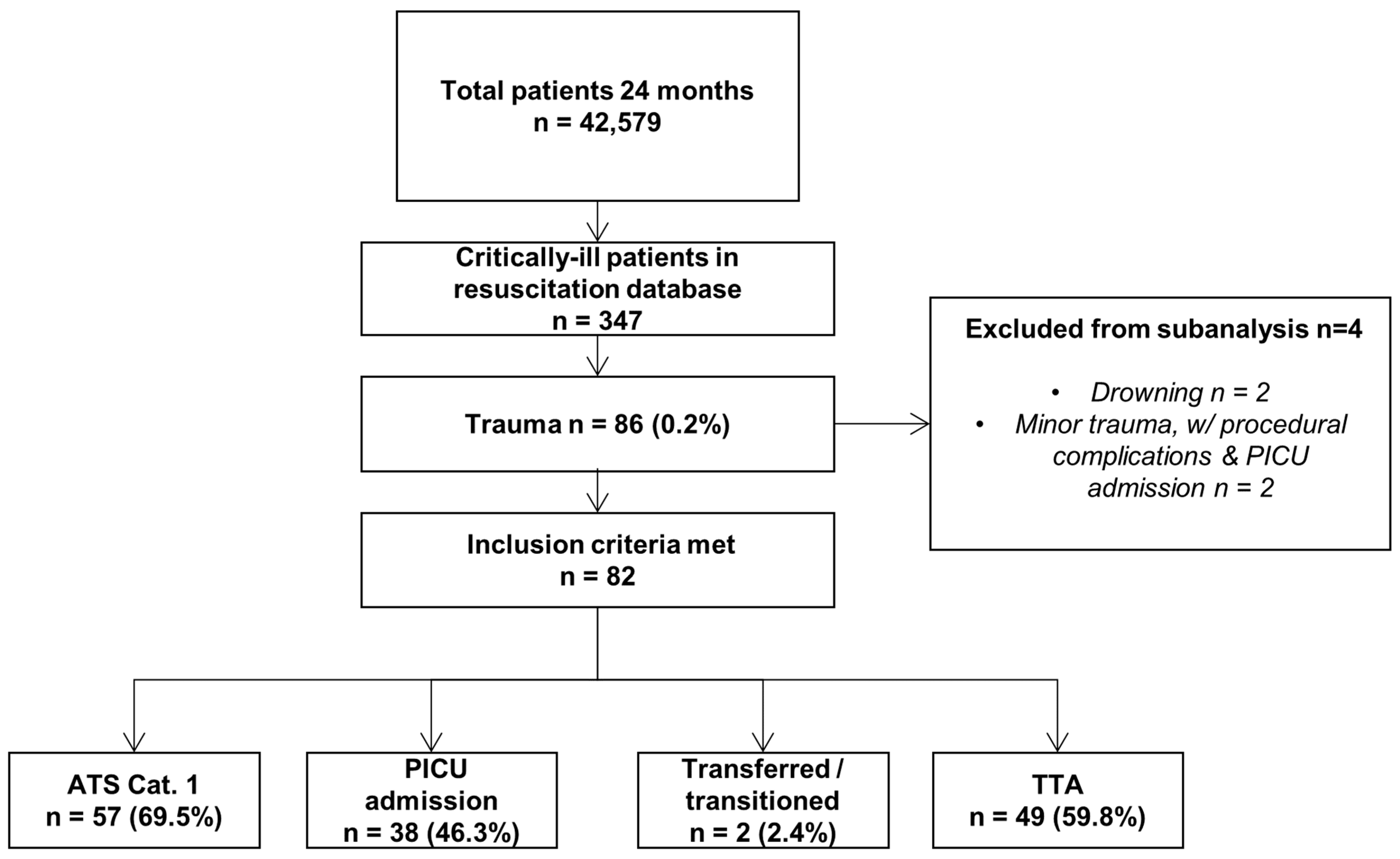
2.2. Inclusion Criteria and Exclusion Criteria
- -
- ATS category 1;
- -
- admitted to PICU from PED, whether directly or via the operating room (OR);
- -
- received TTA;
- -
- transferred to an outside hospital;
- -
- died in PED.
2.3. Data Sources and Variables
2.4. Bias
2.5. Statistics
3. Results
3.1. Patient Characteristics and Mechanism of Injury
3.2. Mode and Time of Arrival
3.3. Trauma Team Activation and Triage
3.4. Imaging
3.5. ED Disposition and Outcomes
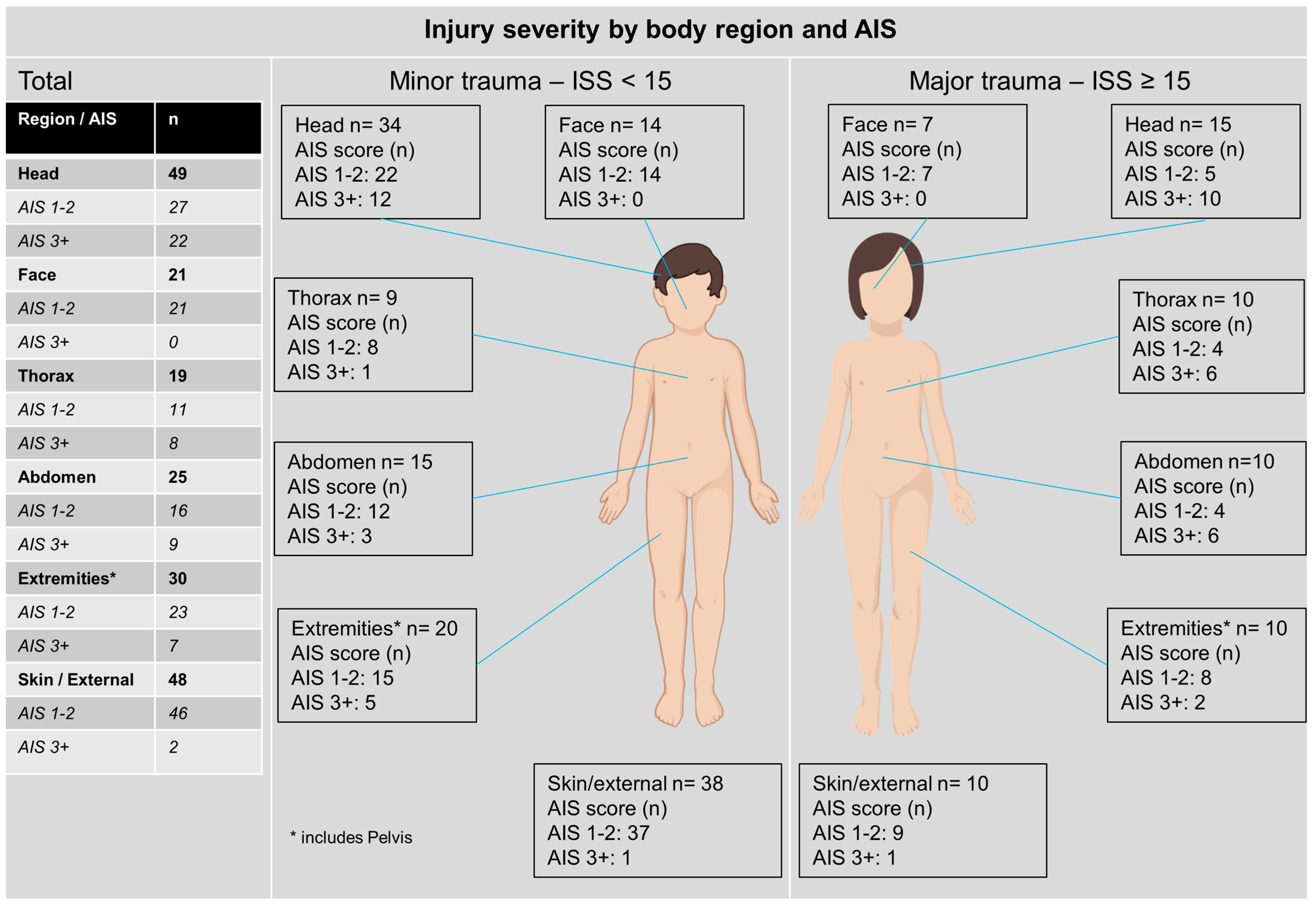
3.6. Injury Severity
4. Discussion
4.1. Key Results
4.2. Trauma Team Activation
4.3. Imaging
4.4. Limitations
4.5. Outlook, Measures, and Prevention
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Condello, A.S.; Hancock, B.J.; Hoppensack, M.; Tenenbein, M.; Stewart, T.C.; Kirwin, D.; Williamson, J.; Findlay, C.; Moffatt, M.; Wiseman, N.; et al. Pediatric trauma registries: The foundation of quality care. J. Pediatr. Surg. 2001, 36, 685–689. [Google Scholar] [CrossRef]
- Peden, M.; Oyegbite, K.; Ozanne-Smith, J.; Hyder, A.A.; Branche, C.; Rahman, A.K.M.F.; Rivara, F.; Bartolomeos, K. (Eds.) World Report on Child Injury Prevention; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Schoeneberg, C.; Schilling, M.; Keitel, J.; Burggraf, M.; Hussmann, B.; Lendemans, S. Mortality in severely injured children: Experiences of a German level 1 trauma center (2002–2011). BMC Pediatr. 2014, 14, 194. [Google Scholar] [CrossRef]
- Kenefake, M.E.; Swarm, M.; Walthall, J. Nuances in Pediatric Trauma. Emerg. Med. Clin. N. Am. 2013, 31, 627–652. [Google Scholar] [CrossRef]
- Kissoon, N.; Dreyer, J.; Walia, M. Pediatric trauma: Differences in pathophysiology, injury patterns and treatment compared with adult trauma. Can. Med. Assoc. J. 1990, 142, 27–34. [Google Scholar]
- Svantner, J.; Dolci, M.; Heim, C.; Schoettker, P. Pediatric Trauma: Six Years of Experience in a Swiss Trauma Center. Pediatr. Emerg. Care 2019, 37, e1133–e1138. [Google Scholar] [CrossRef] [PubMed]
- Entscheid zur Planung der hochspezialisierten Medizin (HSM) im Bereich der Behandlung von schweren Traumata und Polytrauma, inklusive Schädel-Hirn-Traumata bei Kindern [Decision on Planning highly Specialized Medicine (HSM) Treatment of Severe Trauma and Poly-Trauma, Including Traumatic Brain Injuries in Children]. 2011. Available online: https://www.gdk-cds.ch/fileadmin/docs/public/gdk/themen/hsm/hsm_spitalliste/bb_dc_trauma-kinder_20111220_d.pdf (accessed on 21 April 2021).
- Simmen, H.-P.; Jensen, K.-O.; Sprengel, K.; Pape, H.-C. Polytraumaversorgung als Bereich der hochspezialisierten Medizin. Schweiz Ärzteztg. 2021, 102, 836–838. [Google Scholar] [CrossRef]
- Heim, C.; Bosisio, F.; Roth, A.; Bloch, J.; Borens, O.; Daniel, R.T.; Denys, A.; Oddo, M.; Pasquier, M.; Schmidt, S.; et al. Is trauma in Switzerland any different? Epidemiology and patterns of injury in major trauma–a 5-year review from a Swiss trauma centre. Swiss Med. Wkly. 2014, 144, w13958. [Google Scholar] [CrossRef]
- Stocker, S. Triage in Schweizer Kinder-Notfallstationen. Paediatrica 2006, 17, 35–37. [Google Scholar]
- Lehner, M.; Jung, P.; Olivieri, M.; Schmittenbecher, P.P.; on behalf of the Interdisziplinäre Arbeitsgruppe Leitlinie Polytraumaversorgung im Kindesalter. Polytraumaversorgung im Kindesalter–praktische und pragmatische Zusammenfassung [Multiple trauma care in childhood—Practical and pragmatic summary of the new guideline]. Notf. + Rettungsmedizin 2021, 24, 32–42. [Google Scholar] [CrossRef]
- Baker, S.P.; O’Neill, B.; Haddon, W., Jr.; Long, W.B. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J. Trauma 1974, 14, 187–196. [Google Scholar] [CrossRef]
- Copes, W.S.; Champion, H.R.; Sacco, W.J.; Lawnick, M.M.; Keast, S.L.; Bain, L.W. The Injury Severity Score Revisited. J. Trauma Inj. Infect. Crit. Care 1988, 28, 69–77. [Google Scholar] [CrossRef]
- Palmer, C. Major trauma and the injury severity score--where should we set the bar? Annu. Proc. Assoc. Adv. Automot. Med. 2007, 51, 13–29. [Google Scholar]
- Brown, J.B.; Gestring, M.L.; Leeper, C.M.; Sperry, J.L.; Peitzman, A.B.; Billiar, T.R.; Gaines, B.A. The value of the injury severity score in pediatric trauma: Time for a new definition of severe injury? J. Trauma Inj. Infect. Crit. Care 2017, 82, 995–1001. [Google Scholar] [CrossRef]
- Lerner, E.B.; Drendel, A.L.; Falcone, R.A.J.; Weitze, K.C.; Badawy, M.K.; Cooper, A.; Cushman, J.T.; Drayna, P.C.; Gourlay, D.M.; Gray, M.P.; et al. A consensus-based criterion standard definition for pediatric patients who needed the highest-level trauma team activation. J. Trauma Inj. Infect. Crit. Care 2015, 78, 634–638. [Google Scholar] [CrossRef]
- Franzén, L.; Örtenwall, P.; Backteman, T. Children in Sweden admitted to intensive care after trauma. Injury 2007, 38, 91–97. [Google Scholar] [CrossRef]
- Nesje, E.; Valøy, N.N.; Krüger, A.J.; Uleberg, O. Epidemiology of paediatric trauma in Norway: A single-trauma centre observational study. Int. J. Emerg. Med. 2019, 12, 18. [Google Scholar] [CrossRef]
- Beck, B.; Teague, W.; Cameron, P.; Gabbe, B.J. Causes and characteristics of injury in paediatric major trauma and trends over time. Arch. Dis. Child. 2019, 104, 256–261. [Google Scholar] [CrossRef]
- Jones, S.; Tyson, S.; Young, M.; Gittins, M.; Davis, N. Patterns of moderate and severe injury in children after the introduction of major trauma networks. Arch. Dis. Child. 2019, 104, 366–371. [Google Scholar] [CrossRef]
- Bläsius, F.M.; Horst, K.; Brokmann, J.C.; Lefering, R.; Andruszkow, H.; Hildebrand, F.; TraumaRegister, D. Helicopter Emergency Medical Service and Hospital Treatment Levels Affect Survival in Pediatric Trauma Patients. J. Clin. Med. 2021, 10, 837. [Google Scholar] [CrossRef]
- Navascués, J.A.; Matute, J.; Soleto, J.; García Casillas, M.A.; Hernández, E.; Sánchez-París, O.; Molina, E.; De Tomás, E.; Cerdá, J.; Romero, R.; et al. Paediatric trauma in Spain: A report from the HUGM Trauma Registry. Eur. J. Pediatr. Surg. 2005, 15, 30–37. [Google Scholar] [CrossRef]
- Oliver, J.; Avraham, J.; Frangos, S.; Tomita, S.; DiMaggio, C. The epidemiology of inpatient pediatric trauma in United States hospitals 2000 to 2011. J. Pediatr. Surg. 2018, 53, 758–764. [Google Scholar] [CrossRef]
- Faergemann, C. Characteristics of severely injured children admitted to a Danish trauma centre. Dan. Med. J. 2021, 68, A02210129. [Google Scholar]
- Palmer, C.S.; Gabbe, B.J.; Cameron, P.A. Defining major trauma using the 2008 Abbreviated Injury Scale. Injury 2016, 47, 109–115. [Google Scholar] [CrossRef]
- Drendel, A.L.; Gray, M.P.; Lerner, E.B. A Systematic Review of Hospital Trauma Team Activation Criteria for Children. Pediatr. Emerg. Care 2019, 35, 8–15. [Google Scholar] [CrossRef]
- Waydhas, C.; Trentzsch, H.; Hardcastle, T.C.; Jensen, K.O.; Abdelmotaleb, K.T.Y.; Saad, G.A.; Baacke, M.; Baftiu, N.; Bartsokas, C.; Becker, L.; et al. Survey on worldwide trauma team activation requirement. Eur. J. Trauma Emerg. Surg. 2020, 47, 1569–1580. [Google Scholar] [CrossRef]
- Lee, Y.T.; Feng, X.Y.J.; Lin, Y.-C.; Chiang, L.W. Pediatric Trauma Team Activation: Are We Making the Right Call? Eur. J. Pediatr. Surg. 2014, 24, 46–50. [Google Scholar] [CrossRef]
- Williams, D.; Foglia, R.; Megison, S.; Garcia, N.; Foglia, M.; Vinson, L. Trauma activation: Are we making the right call? A 3-year experience at a Level I pediatric trauma center. J. Pediatr. Surg. 2011, 46, 1985–1991. [Google Scholar] [CrossRef]
- Roden-Foreman, J.W.; Rapier, N.R.; Foreman, M.L.; Zagel, A.L.; Sexton, K.W.; Beck, W.C.; McGraw, C.; Coniglio, R.A.; Blackmore, A.R.; Holzmacher, J.; et al. Rethinking the definition of major trauma: The need for trauma intervention outperforms Injury Severity Score and Revised Trauma Score in 38 adult and pediatric trauma centers. J. Trauma Inj. Infect. Crit. Care 2019, 87, 658–665. [Google Scholar] [CrossRef]
- Gurien, L.A.; Nichols, L.; Williamson, P.; Letton, R.W. Rethinking pediatric trauma triage. Semin. Pediatr. Surg. 2022, 31, 151214. [Google Scholar] [CrossRef]
- Bressan, S.; Franklin, K.L.; Jowett, H.E.; King, S.K.; Oakley, E.; Palmer, C.S. Establishing a standard for assessing the appropriateness of trauma team activation: A retrospective evaluation of two outcome measures. Emerg. Med. J. 2015, 32, 716–721. [Google Scholar] [CrossRef]
- Qazi, K.; Wright, M.S.; Kippes, C. Stable pediatric blunt trauma patients: Is trauma team activation always necessary? J. Trauma Inj. Infect. Crit. Care 1998, 45, 562–564. [Google Scholar] [CrossRef]
- Cohen, N.; Davis, A.L.; Test, G.; Singer–Harel, D.; Pasternak, Y.; Beno, S.; Scolnik, D. Evaluation of activation criteria in paediatric multi-trauma. Paediatr. Child Health 2023, 28, 17–23. [Google Scholar] [CrossRef]
- Hershkovitz, Y.; Zoarets, I.; Stepansky, A.; Kozer, E.; Shapira, Z.; Klin, B.; Halevy, A.; Jeroukhimov, I. Computed tomography is not justified in every pediatric blunt trauma patient with a suspicious mechanism of injury. Am. J. Emerg. Med. 2014, 32, 697–699. [Google Scholar] [CrossRef]
- Halaweish, I.; Riebe-Rodgers, J.; Randall, A.; Ehrlich, P.F. Compliance with evidence-based guidelines for computed tomography of children with head and abdominal trauma. J. Pediatr. Surg. 2018, 53, 748–751. [Google Scholar] [CrossRef]
- Strait, L.; Sussman, R.; Ata, A.; Edwards, M.J. Utilization of CT imaging in minor pediatric head, thoracic, and abdominal trauma in the United States. J. Pediatr. Surg. 2020, 55, 1766–1772. [Google Scholar] [CrossRef]
- Nellensteijn, D.R.; Greuter, M.J.; el Moumni, M.; Hulscher, J.B. The Use of CT Scan in Hemodynamically Stable Children with Blunt Abdominal Trauma: Look before You Leap. Eur. J. Pediatr. Surg. 2016, 26, 332–335. [Google Scholar] [CrossRef]
- Marin, J.R.; Wang, L.; Winger, D.G.; Mannix, R.C. Variation in Computed Tomography Imaging for Pediatric Injury-Related Emergency Visits. J. Pediatr. 2015, 167, 897–904.e3. [Google Scholar] [CrossRef]
- Wiitala, E.L.; Parker, J.L.; Jones, J.S.; Benner, C.A. Comparison of Computed Tomography Use and Mortality in Severe Pediatric Blunt Trauma at Pediatric Level I Trauma Centers Versus Adult Level 1 and 2 or Pediatric Level 2 Trauma Centers. Pediatr. Emerg. Care 2020, 38, e138–e142. [Google Scholar] [CrossRef]
- Simma, L.; Fornaro, J.; Stahr, N.; Lehner, M.; Roos, J.E.; Lima, T.V.M. Optimising whole body computed tomography doses for paediatric trauma patients: A Swiss retrospective analysis. J. Radiol. Prot. 2022, 42, 021521. [Google Scholar] [CrossRef]
- Beno, S.; Paluck, F.; Greenspoon, T.; Rosenfield, D.; Principi, T. Safely reducing abdominal/pelvic computed tomography imaging in pediatric trauma: A quality improvement initiative. Can. J. Emerg. Med. 2022, 24, 535–543. [Google Scholar] [CrossRef]
- Wadman, M.C.; Muelleman, R.L.; Coto, J.A.; Kellermann, A.L. The pyramid of injury: Using ecodes to accurately describe the burden of injury. Ann. Emerg. Med. 2003, 42, 468–478. [Google Scholar] [CrossRef]
- Niemann, S.; Fahrni, S.; Hayoz, R.; Brügger, O.; Cavegn, M. Status 2022:Statistik der Nichtberufsunfälle und des Sicherheitsniveaus in der Schweiz; BFU, Beratungsstelle für Unfallverhütung: Berne, Switzerland, 2022. [Google Scholar]
- Adams, M.; Natalucci, G.; Bassler, D. A narrative review of the Swiss Neonatal Network & Follow-up Group (SwissNeoNet). Pediatr. Med. 2021. epub ahead of print. [Google Scholar] [CrossRef]
- Simma, L.; Stocker, M.; Lehner, M.; Wehrli, L.; Righini-Grunder, F. Critically Ill Children in a Swiss Pediatric Emergency Department With an Interdisciplinary Approach: A Prospective Cohort Study. Front. Pediatr. 2021, 9, 721646. [Google Scholar] [CrossRef]
| Minor (ISS < 15) | Major (ISS ≥ 15) | Total n (%) | Significance Testing | |
|---|---|---|---|---|
| Sex | p = 0.768 | |||
| Male | 45 (54.9) | 15 (18.3) | 60 (73.2) | |
| Female | 18 (22.0) | 4 (4.9) | 22 (26.8) | |
| Total | 63 (76.8) | 19 (21.2) | 82(100) | |
| Age | p = 0.631 | |||
| 0–3 | 10 (12.2) | 4 (4.8) | 14 (17.1) | |
| 4–7 | 17 (20.7) | 7 (8.5) | 24 (29.3) | |
| 8–11 | 14 (17.1) | 2 (2.4) | 16 (19.5) | |
| 12–15 | 22 (26.8) | 6 (7.3) | 28 (34.1) | |
| Mechanism of injury | p = 0.388 | |||
| Sports | 18 (22.0) | 2 (2.4) | 20 (24.4) | |
| Road traffic related # | 12 (14.6) | 5 (6.1) | 17 (20.7) | |
| Falls * | 24 (29.3) * | 8 (9.8) | 32 (39.0) | |
| Blunt trauma | 8 (9.8) | 3 (3.7) | 11 (13.4) | |
| Burns | 1 (1.2) | 1 (1.2) | 2 (2.4) | |
| Seasonality | ||||
| Q1 (Jan–Mar) | 11 (13.4) | 3 (3.7) | 14 (17.1) | |
| Q2 (Apr–Jun) | 19 (23.2) | 9 (11.0) | 28 (34.1) | |
| Q3 (Jul–Sep) | 21 (25.6) | 3 (3.7) | 24 (29.3) | |
| Q4 (Oct–Dec) | 12 (14.6) | 4 (4.9) | 16 (19.5) |
| TTA | No TTA | Total n (%) | Significance Testing | |
|---|---|---|---|---|
| Transport mode | p = 0.027 | |||
| Walk-in | 4 (4.9) | 7 (8.5) | 11 (13.4) | |
| Primary care * | 0 | 2 (2.4) | 2 (2.4) | |
| Ambulance | 25(30.5) | 18 (22.0) | 43 (52.4) | |
| HEMS | 20 (24.4) | 6 (7.3) | 26 (31.7) | |
| 49 (59.8) | 33 (40.2) | 82 (100) | ||
| Triage category | p = 0.013 | |||
| ATS1 | 39 (47.6) | 18 (22.0) | 57 (69.5) | |
| ATS2 | 9 (11.0) | 9 (11.0) | 18 (22.0) | |
| ATS 3&4 | 1 (1.2) | 6 (7.3) | 7 (8.5) | |
| Day of presentation | p = 0.344 | |||
| Weekday | 35 (42.7) | 20 (24.4) | 55 (67.1) | |
| Weekend | 14 (17.1) | 13 (15.9) | 27 (32.9) | |
| Shift of presentation | p = 0.872 | |||
| 08:00 h–16:00 h | 27 (32.9) | 16 (19.5) | 43 (52.4) | |
| 16:00 h–23:00 h | 19 (23.2) | 15 (18.3) | 34 (31.5) | |
| 23:00 h–08:00 h | 3 (3.7) | 2 (2.4) | 5 (6.1) | |
| Trauma severity | p = 0.795 | |||
| Major (ISS ≥ 15) | 12 (14.6) | 7 (8.5) | 19 (23.2) | |
| Minor (ISS < 15) | 37 (45.1) | 26 (31.7) | 63 (76.8) |
| Mechanism of Injury | <6 Years n (%) | >6 Years n (%) | Total n (%) |
|---|---|---|---|
| Falls | |||
| Fall > 3 m | 7 (8.5) | 15 (18.3) | 22 (26.8) |
| Fall < 3 m | 6 (7.3) | 4 (4.9) | 10 (12.2) |
| Sports injury | |||
| Sporting/play injury | 2 (2.4) | 9 (11.0) | 11 (13.4) |
| Winter sports injury | - | 9 (11.0) | 9 (11.0) |
| Road traffic | |||
| Pedestrian vs. MV | 3 (3.7) | 6 (7.3) | 9 (11.0) |
| MVA | 2 (2) | 6 (7.3) | 8 (9.8) |
| Blunt trauma, NS | 6 (7.3) | 5 (6.1) | 11 (13.4) |
| Burns | 2 (2.4) | - | 2 (2.4) |
| Total | 28 (34.1) | 54 (65.9) | 82 (100) |
| Minor (ISS < 15), n = 63 | Major (ISS ≥ 15), n = 19 | Total n (%) | Significance Testing | |
|---|---|---|---|---|
| Imaging | ||||
| No imaging | 5 (6.1) | 1 (1.2) | 6 (7.3) | p = 0.014 |
| X-ray only | 5 (6.1) | 1 (1.2) | 6 (7.3) | |
| Ultrasound | 11 (13.4) | 1 (1.2) | 12 (14.6) | |
| CT focused | 21 (25.9) | 5 (6.1) | 26 (31.7) | |
| WBCT | 7 (8.5) | 10 (12.2) | 17 (20.7) | |
| MRI | 1 (1.2) | 0 | 1 (1.2) | |
| US & X-ray | 10 (12.2) | 0 | 10 (12.2) | |
| WBCT & MRI | 3 (3.7) | 1 (1.2) | 4 (4.9) | |
| Imaging categories | p = 0.008 (n = 76) * | |||
| Simple Imaging * (XR, US) | 26 (34.2) | 2 (2.6) | 28 (36.8) * | |
| Advanced Imaging * (CT, WBCT, MRI) | 32 (42.1) | 16 (21.1) | 48 (63.2) * | |
| CT imaging analysis (n = 43) | p = 0.011 | |||
| 21 (48.8) | 5 (11.6) | 26 (60.5) | |
| 7 (16.3) | 10 (23.3) | 17 (39.5) | |
| Disposition + | p < 0.001 + | |||
| Outpatient | 3 (3.7) | 0 | 3 (3.7) | |
| Inpatient | 36 (44.4) | 2 (2.5) | 38 (46.9) | |
| PICU | 22 (27.2) | 16 (19.8) | 38 (46.9) | |
| Transfer | 2 (2.5) | 0 | 2 (2.4) | |
| Death in PED | 0 | 1 (1.2) | 1 (1.2) | |
| Total | 63 (77.8) | 18 (22.2) | 82 (100) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herren, A.; Palmer, C.S.; Landolt, M.A.; Lehner, M.; Neuhaus, T.J.; Simma, L. Pediatric Trauma and Trauma Team Activation in a Swiss Pediatric Emergency Department: An Observational Cohort Study. Children 2023, 10, 1377. https://doi.org/10.3390/children10081377
Herren A, Palmer CS, Landolt MA, Lehner M, Neuhaus TJ, Simma L. Pediatric Trauma and Trauma Team Activation in a Swiss Pediatric Emergency Department: An Observational Cohort Study. Children. 2023; 10(8):1377. https://doi.org/10.3390/children10081377
Chicago/Turabian StyleHerren, Anouk, Cameron S. Palmer, Markus A. Landolt, Markus Lehner, Thomas J. Neuhaus, and Leopold Simma. 2023. "Pediatric Trauma and Trauma Team Activation in a Swiss Pediatric Emergency Department: An Observational Cohort Study" Children 10, no. 8: 1377. https://doi.org/10.3390/children10081377
APA StyleHerren, A., Palmer, C. S., Landolt, M. A., Lehner, M., Neuhaus, T. J., & Simma, L. (2023). Pediatric Trauma and Trauma Team Activation in a Swiss Pediatric Emergency Department: An Observational Cohort Study. Children, 10(8), 1377. https://doi.org/10.3390/children10081377






