Treatment Provided in Children and Adolescents with Functional Seizures—A Danish Nationwide Cohort
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
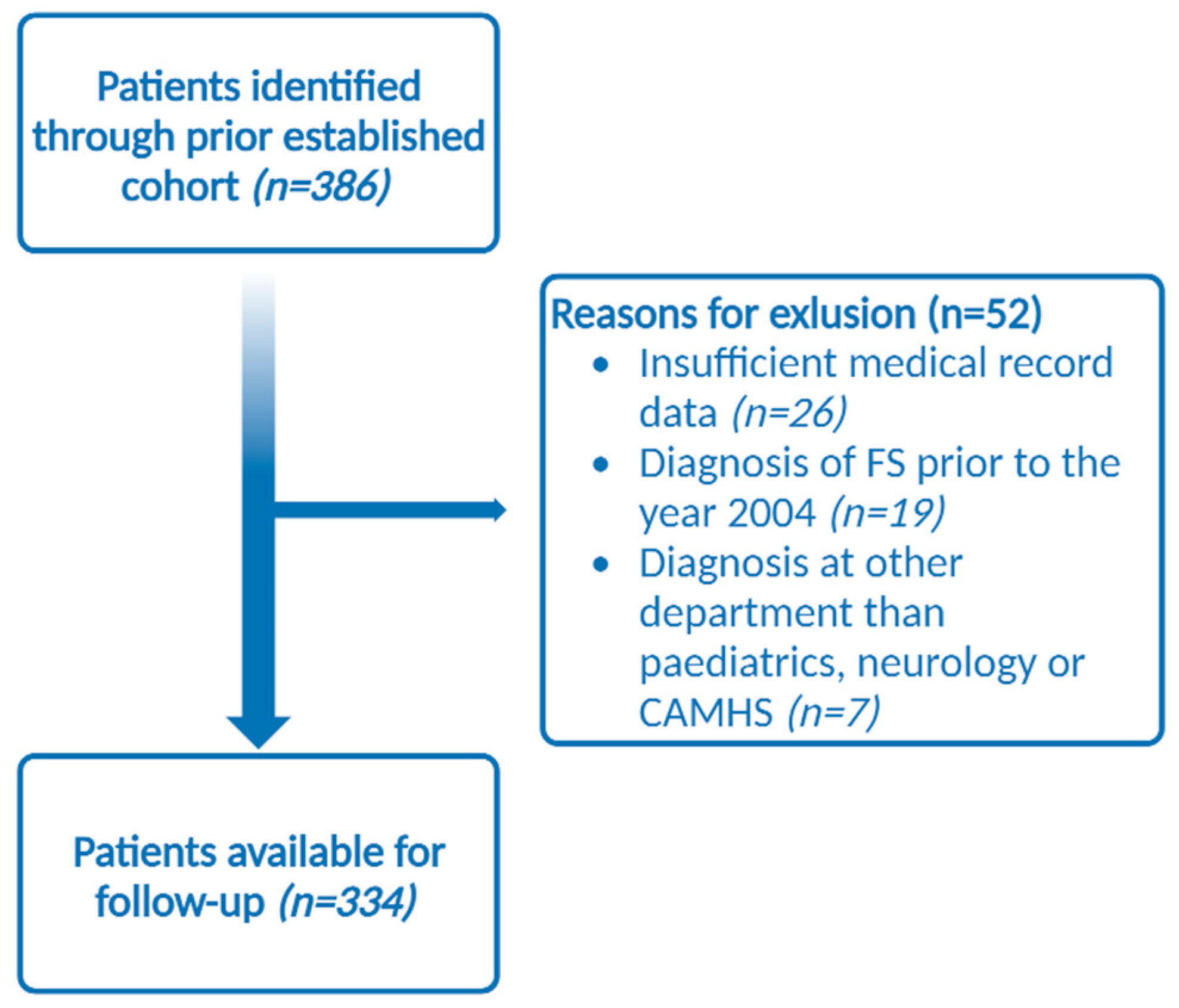
2.2. Population
2.3. The Study Population
2.4. Outcomes
3. Results
3.1. Patient Characteristics
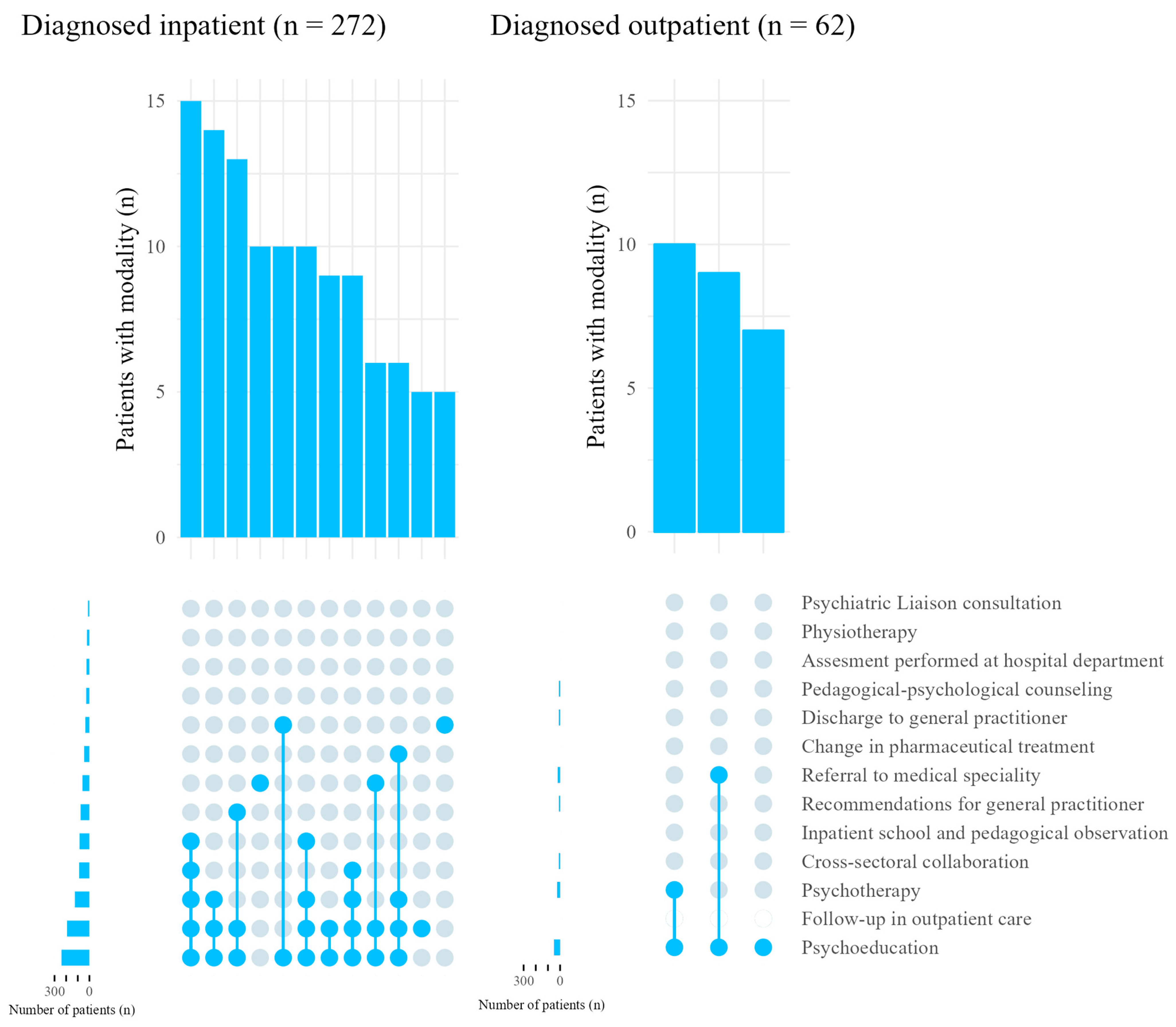
3.2. Management and Treatment Modalities
3.3. Stratified Analyses
4. Discussion
4.1. The Multidisciplinary Approach and the Cross-Sectoral Collaboration
4.2. Psychoeducation and Psychotherapy
4.3. Pharmaceuticals
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hansen, A.S.; Rask, C.U.; Rodrigo-Domingo, M.; Pristed, S.G.; Christensen, J.; Nielsen, R.E. Incidence rates and characteristics of pediatric onset psychogenic nonepileptic seizures. Pediatr. Res. 2020, 88, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Reuber, M.; Brown, R.J. Understanding psychogenic nonepileptic seizures—Phenomenology, semiology and the Integrative Cognitive Model. Seizure 2017, 44, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Asadi-Pooya, A.A.; Bahrami, Z. Social aspects of life in patients with functional seizures: Closing the gap in the biopsychosocial formulation. Epilepsy Behav. 2018, 117, 119–121. [Google Scholar] [CrossRef]
- Reilly, C.; Menlove, L.; Fenton, V.; Das, K.B. Psychogenic nonepileptic seizures in children: A review. Epilepsia 2013, 54, 1715–1724. [Google Scholar] [CrossRef]
- Doss, J.; Plioplys, S. Pediatric Psychogenic Nonepileptic Seizures: A Concise Review. Child Adolesc. Clin. N. Am. 2018, 27, 53–61. [Google Scholar] [CrossRef]
- Irwin, K.; Edwards, M.; Robinson, R. Psychogenic non-epileptic seizures: Management and prognosis. Arch. Dis. Child. 2000, 82, 474–478. [Google Scholar] [CrossRef]
- Heyman, I.; Reilly, C. Seize the opportunity—Recognition and management of functional seizures in children. Eur. J. Paediatr. Neurol. 2018, 22, 734–735. [Google Scholar] [CrossRef] [PubMed]
- Rask, C.U.; Bonvanie, I.J.; Garralda, E.M. Risk and Protective Factors and Course of Functional Somatic Symptoms in Young People. In Understanding Uniqueness and Diversity in Child and Adolescent Mental Health; Academic Press: Cambridge, MA, USA, 2018. [Google Scholar]
- Velani, H.; Gledhill, J. The effectiveness of psychological interventions for children and adolescents with non-epileptic seizures. Seizure 2021, 93, 20–31. [Google Scholar] [CrossRef]
- The Danish Health Authority. Treatment of Somatoform Disorders in the Danish Child and Adolescent Psychiatric Departments. 2019. Available online: https://www.sst.dk/-/media/Viden/Specialplaner/Specialeplan-for-børne--og-ungdomspsykiatri/SST_Specialevejledning-for-boeerne-og-ungdomspsykiatri-11april-2019.ashx?la=da&hash=BCF7C83B6D6DB5291B621A6805C841CADD2EA137 (accessed on 21 December 2021).
- Caplan, R.; Doss, J.; Plioplys, S.; Jones, J.E. Short-Term Treatment. In Pediatric Psychogenic Non-Epileptic Seizures; Springer International Publishing: Cham, Switzerland, 2017; pp. 27–48. [Google Scholar]
- Caplan, R.; Doss, J.; Plioplys, S.; Jones, J.E. Long-Term Treatment. In Pediatric Psychogenic Non-Epileptic Seizures; Springer International Publishing: Cham, Switzerland, 2017; pp. 49–62. [Google Scholar]
- Nielsen, E.S.; Wichaidit, B.T.; Østergaard, J.R.; Rask, C.U. Paediatricians’ attitudes to and management of functional seizures in children. Eur. J. Paediatr. Neurol. 2018, 22, 774–781. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Stata Statistical Software, Release 17; StataCorp: College Station, TX, USA, 2021.
- Thompson, N.C.; Gibson, P.A. Models of Care: The Roles of Nurses and Social Workers in the Diagnosis and Management of Patients with Nonepileptic Seizures in Gates and Rowan’s Nonepileptic Seizures, 3rd ed.; Schacter, S.C., LaFrance, W.C., Jr., Eds.; Cambridge University Press: Cambridge, UK, 2010; p. 253258. [Google Scholar]
- Terry, D.; Enciso, L.; Trott, K.; Burch, M.; Albert, D.V.F. Outcomes in children and adolescents with psychogenic nonepileptic events using a multidisciplinary clinic approach. J. Child Neurol. 2020, 35, 918–923. [Google Scholar] [CrossRef] [PubMed]
- Kozlowska, K.; Chudleigh, C.; Cruz, C.; Lim, M.; McClure, G.; Savage, B.; Shah, U.; Cook, A.; Scher, S.; Carrive, P.; et al. Psychogenic nonepileptic seizures in children and adolescents: Part II—Explanations to families, treatment, and group outcomes. Clin. Child Psychol. Psychiatry 2018, 23, 160–176. [Google Scholar] [CrossRef] [PubMed]
- McFarlane, F.A.; Allcott-Watson, H.; Hadji-Michael, M.; McAllister, E.; Stark, D.; Reilly, C.; Bennett, S.D.; McWillliams, A.; Heyman, I. Cognitive-behavioural treatment of functional neurological symptoms (conversion disorder) in children and adolescents: A case series. Eur. J. Paediatr. Neurol. 2019, 23, 317–328. [Google Scholar] [CrossRef]
- Flewelling, K.D.; Koehler, A.; Shaffer, J.; Dill, E.J. Medical and psychosocial outcomes of youth with psychogenic nonepileptic seizures: An observational study. Epilepsy Behav. 2020, 112, 107383. [Google Scholar] [CrossRef]
- Chandra, P.; Kozlowska, K.; Cruz, C.; Baslet, G.C.; Perez, D.L.; Garralda, M.E. Hyperventilation-induced non-epileptic seizures in an adolescent boy with pediatric medical traumatic stress. Harv. Rev. Psychiatry 2017, 25, 80–190. [Google Scholar] [CrossRef] [PubMed]
- Chudleigh, C.; Kozlowska, K.; Kothur, K.; Davies, F.; Baxter, H.; Landini, A.; Hazell, P.; Baslet, G. Managing nonepileptic seizures and psychogenic dystonia in an adolescent girl with preterm brain injury. Harv. Rev. Psychiatry 2016, 21, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Malhi, P.; Kumar, C.; Singhi, P.; Sankhyan, N. Outcome of Conversion Symptoms in Children. Indian J. Pediatr. 2021, 88, 367–369. [Google Scholar] [CrossRef] [PubMed]
- Fobian, A.D.; Long, D.M.; Szaflarski, J.P. Retraining and control psychotherapy for pediatric psychogenic non-epileptic seizures. Ann. Clin. Transl. Neurol. 2020, 7, 1410–1419. [Google Scholar] [CrossRef]
- Tolchin, B.; Dworetzky, B.A.; Martino, S.; Blumenfeld, H.; Hirsch, L.J.; Baslet, G. Adherence with psychotherapy and treatment outcomes for psychogenic nonepileptic seizures. Neurology 2019, 92, E675–E679. [Google Scholar] [CrossRef]
- Buonsenso, D.; Plosnic, M.; Bersani, G.; Monaco, S.; Ferrara, P.; Chiaretti, A. Paroxysmal non-epileptic events in the pediatric emergency department. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 2188–2193. [Google Scholar] [CrossRef]
- Mandli, A.; Desai, N.; Badheka, R.; Udani, V. Paroxysmal nonepileptic events in a pediatric epilepsy clinic. J. Pediatr. Neurosci. 2021, 16, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Caplan, R.; Doss, J.; Plioplys, S.; Jones, J.E. Diagnosis of Peadiatric PNES. In Pediatric Psychogenic Non-Epileptic Seizures; Springer International Publishing: Cham, Switzerland, 2017; pp. 3–14. [Google Scholar]
- Plioplys, S.; Siddarth, P.; Asato, M.R.; Caplan, R. Clinicians’ Views on Antiepileptic Medication Management in Nonepileptic Seizures. J. Child Neurol. 2014, 29, 746–750. [Google Scholar] [CrossRef] [PubMed]
| Total N = 334 | Neurology n = 142 | Paediatrics n = 165 | CAMHS n = 27 | |
|---|---|---|---|---|
| Female sex | 276 (82.6) | 123 (86.6) | 132 (80.0) | 21 (77.8) |
| Age at diagnosis (Median, [IQR]) b | 15.7 [14.1–16.8] | 16.8 [16.3–17.3] | 14.3 [12.6–15.3] | 15.1 [13.7–16.2] |
| Duration of medical record data in days (median, [IQR]) b | 49.0 [8.0–78.0] | 48.0 [8.0–73.0] | 45.0 [5.0–77.0] | 74.0 [53.0–89.0] |
| Comorbid epilepsy c | 54 (19.2) | <30 | 27 (16.4) | <5 |
| Comorbid severe somatic illness c | 23 (6.9) | 13 (9.2) | 10 (6.1) | 0 (0.0) |
| Comorbid psychiatric disorders c | <67 (<20.1) | 33 (23.2) | 29 (17.6) | <5 |
| Pharmaceutical treatment at time of diagnosis | 103 (30.8) d | 50 (35.2) | 47 (28.5) | 6 (22.2) |
| ASMs e | 81 (78.6) | 42 (84.0) | >34 (>72.3) | <5 |
| Psychotropic drugs e | 27 (26.2) | >10 (>20.0) | 12 (25.5) | <5 |
| Diagnosis given as inpatient | 271 (81.4) | 112 (78.9) | 148 (89.7) | 11 (40.7) |
| Total N = 334 | Neurology n = 142 | Paediatrics n = 165 | CAMHS n = 27 | p-Value b | |
|---|---|---|---|---|---|
| Psychoeducation | 289 (86.5) | 121 (85.2) | 146 (88.5) | 22 (81.5) | 0.46 |
| Psychotherapy | 148 (44.3) | 53 (37.3) | 73 (44.2) | 22 (81.5) | <0.001 |
| Change in pharmaceutical treatment | 51 (15.3) | 25 (17.6) | 21 (12.7) | 5 (18.5) | 0.44 |
| Cross-sectoral collaboration c | 98 (29.3) | 17 (12.0) | 67 (40.6) | 14 (51.9) | <0.001 |
| Inpatient school and pedagogical observation | 85 (25.4) | 23 (16.2) | 62 (37.6) | 0 (0.0) | <0.001 |
| Physiotherapy | 23 (6.9) | <5 | 17 (10.3) | <5 | <0.001 |
| Assessment performed at hospital department | <32 (<9.6) | 16 (11.3) | 11 (6.7) | <5 | 0.32 |
| Psychiatric liaison consultation | <15 (<4.5) | 10 (7.0) | <5 | 0 (0.0) | 0.052 |
| Pedagogical–psychological counselling | <38 (<11.4) | <5 | 23 (13.9) | 10 (37.0) | <0.001 |
| If inpatient diagnosis (n = 272): follow-up in outpatient care | 192 (70.6) | 76 (67.9) | 107 (71.8) | 9 (81.8) | 0.59 |
| Referral to medical specialty | 79 (23.7) | 34 (23.9) | 38 (23.0) | 7 (25.9) | 0.92 |
| Discharge to general practitioner d | <47 (<14.1) | 18 (12.7) | 24 (14.5) | <5 | 0.71 |
| Suggestions for general practitioner | <86 (<25.7) | 39 (27.5) | 42 (25.5) | <5 | 0.13 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sørensen, N.B.; Nielsen, R.E.; Christensen, A.-E.; Kjeldsen, M.K.; Rask, C.U.; Christensen, J.; Hansen, A.S. Treatment Provided in Children and Adolescents with Functional Seizures—A Danish Nationwide Cohort. Children 2023, 10, 1218. https://doi.org/10.3390/children10071218
Sørensen NB, Nielsen RE, Christensen A-E, Kjeldsen MK, Rask CU, Christensen J, Hansen AS. Treatment Provided in Children and Adolescents with Functional Seizures—A Danish Nationwide Cohort. Children. 2023; 10(7):1218. https://doi.org/10.3390/children10071218
Chicago/Turabian StyleSørensen, Nana Brandborg, René Ernst Nielsen, Ann-Eva Christensen, Mikkel Kristian Kjeldsen, Charlotte Ulrikka Rask, Jakob Christensen, and Anne Sofie Hansen. 2023. "Treatment Provided in Children and Adolescents with Functional Seizures—A Danish Nationwide Cohort" Children 10, no. 7: 1218. https://doi.org/10.3390/children10071218
APA StyleSørensen, N. B., Nielsen, R. E., Christensen, A.-E., Kjeldsen, M. K., Rask, C. U., Christensen, J., & Hansen, A. S. (2023). Treatment Provided in Children and Adolescents with Functional Seizures—A Danish Nationwide Cohort. Children, 10(7), 1218. https://doi.org/10.3390/children10071218







