Developmental Coordination Disorder and Unhealthy Weight Status in Taiwanese Children: The Roles of Sex and Age
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Measures
2.3.1. Unhealthy Weight Status
2.3.2. Developmental Coordination Disorder
2.4. Statistical Analysis
3. Results
3.1. Overview of Participants
3.2. Prevalence of Preschool and School-Aged Children with rDCD
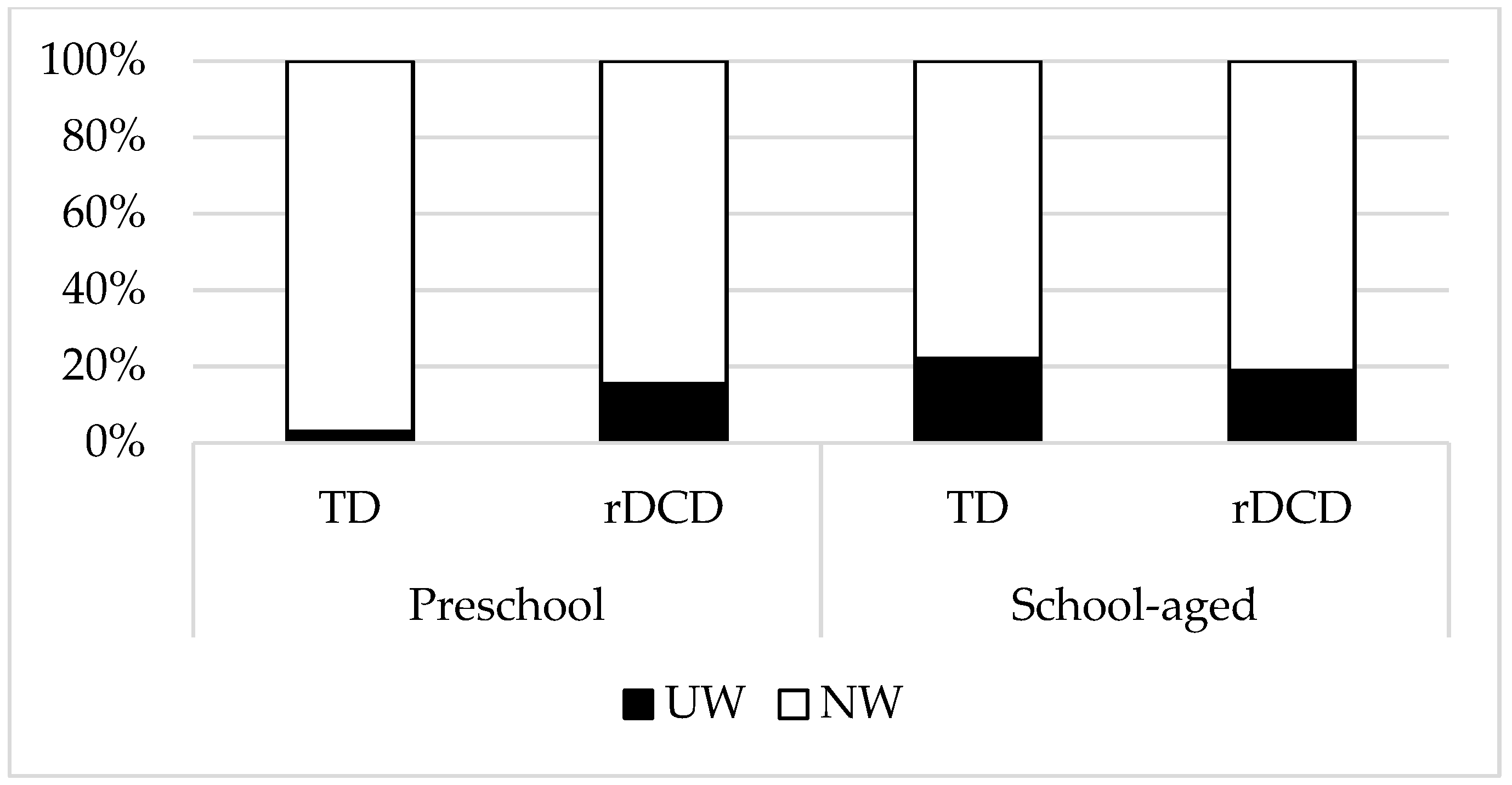
3.3. DCD and Underweight
3.4. DCD and Overweight/Obesity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Onis, M.; Blossner, M.; Borghi, E.; Frongillo, E.A.; Morris, R. Estimates of global prevalence of childhood underweight in 1990 and 2015. JAMA 2004, 291, 2600–2606. [Google Scholar] [CrossRef]
- Jebeile, H.; Kelly, A.S.; O’Malley, G.; Baur, L.A. Obesity in children and adolescents: Epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022, 10, 351–365. [Google Scholar] [CrossRef]
- Di Cesare, M.; Soric, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef]
- Chiang, T.L.; Lin, S.J.; Lin, Y.H. Infographics of Child Health in New Era’s Taiwanese Preschool Children; Health Promotion Administration, Ministry of Health and Welfare: Taipei, Taiwan, 2018. (In Chinese)
- Health Promotion Administration. Statistics of Health Promotion 2020; Ministry of Health and Welfare: Taipei, Taiwan, 2022.
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef] [PubMed]
- Hendrix, C.G.; Prins, M.R.; Dekkers, H. Developmental coordination disorder and overweight and obesity in children: A systematic review. Obes. Rev. 2014, 15, 408–423. [Google Scholar] [CrossRef]
- American Pyshiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Cairney, J.; Veldhuizen, S. Organized sport and physical activity participation and body mass index in children and youth: A longitudinal study. Prev. Med. Rep. 2017, 6, 336–338. [Google Scholar] [CrossRef] [PubMed]
- Kwan, M.Y.; King-Dowling, S.; Hay, J.A.; Faught, B.E.; Cairney, J. Longitudinal examination of objectively-measured physical activity and sedentary time among children with and without significant movement impairments. Hum. Mov. Sci. 2016, 47, 159–165. [Google Scholar] [CrossRef]
- Zhu, Y.C.; Wu, S.K.; Cairney, J. Obesity and motor coordination ability in Taiwanese children with and without developmental coordination disorder. Res. Dev. Disabil. 2011, 32, 801–807. [Google Scholar] [CrossRef]
- Zhu, Y.C.; Wu, S.K.; Cairney, J.; Li, Y.C.; Chen, W.Y.; Chen, F.C. High risk for obesity in children with a subtype of developmental coordination disorder. Res. Dev. Disabil. 2014, 35, 1727–1733. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, M.L.; Perry, K.E.; Thapa, B.; Adhikari, R.P.; Weissman, A. Malnutrition matters: Association of stunting and underweight with early childhood development indicators in Nepal. Matern. Child Nutr. 2022, 18, e13321. [Google Scholar] [CrossRef]
- Joshi, D.; Missiuna, C.; Hanna, S.; Hay, J.; Faught, B.E.; Cairney, J. Relationship between BMI, waist circumference, physical activity and probable developmental coordination disorder over time. Hum. Mov. Sci. 2015, 40, 237–247. [Google Scholar] [CrossRef]
- Schott, N.; Alof, V.; Hultsch, D.; Meermann, D. Physical fitness in children with developmental coordination disorder. Res. Q Exerc Sport 2007, 78, 438–450. [Google Scholar] [CrossRef]
- Chen, W.; Chang, M.H. New growth charts for Taiwanese children and adolescents based on World Health Organization standards and health-related physical fitness. Pediatr. Neonatol. 2010, 51, 69–79. [Google Scholar] [CrossRef]
- Henderson, S.E.; Sugden, D.A.; Barnett, A.L. Movement Assessment Battery for Children, 2nd ed.; Pearson Assessment: London, UK, 2007. [Google Scholar]
- Wuang, Y.P.; Su, J.H.; Su, C.Y. Reliability and responsiveness of the Movement Assessment Battery for Children–Second Edition Test in children with developmental coordination disorder. Dev. Med. Child Neurol. 2012, 54, 160–165. [Google Scholar] [CrossRef]
- Blank, R.; Barnett, A.L.; Cairney, J.; Green, D.; Kirby, A.; Polatajko, H.; Rosenblum, S.; Smits-Engelsman, B.; Sugden, D.; Wilson, P.; et al. International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Dev. Med. Child Neurol. 2019, 61, 242–285. [Google Scholar] [CrossRef] [PubMed]
- Blank, R.; Smits-Engelsman, B.; Polatajko, H.; Wilson, P. European Academy of Childhood Disability Recommendations (EACD): Recommendations on the definition, diagnosis and intervention of Developmental Coordination Disorder (long version). Dev. Med. Child Neurol. 2012, 54, 54–93. [Google Scholar] [CrossRef]
- Lin, H.T.; Wu, T.W.; Hu, S.T.; Kuo, C.C.; Tsai, C.C.; Wang, J.D. The Chinese Version of the Test of Nonverbal Intelligence, 4th ed.; Psychological Publishing Co., Ltd.: Taipei, Taiwan, 2016. [Google Scholar]
- Li, Y.C.; Wu, S.K. Prevalence of eleven to twelve year-old Taiwanese children with Developmental Coordination Disorder. Health Promot. Sci. 2007, 2, 55–67. (In Chinese) [Google Scholar]
- Lin, K.H.; Wu, S.K. Seven to eight year-old children with developmental coordination disorder in Taiwan. Formos. J. Phys. Ther. 2002, 27, 238–248. (In Chinese) [Google Scholar]
- Hsu, Y.W.; Cherng, R.J.; Yu, T.Y.; Chen-Sea, M.J. Comparison of the performance of preschoolers from Taiwan and USA in the Movement Assessment Battery for Children. Formos. J. Phys. Ther. 2004, 29, 307–316. (In Chinese) [Google Scholar]
- Miller, L.T.; Missiuna, C.A.; Macnab, J.J.; Malloy-Miller, T.; Polatajko, H.J. Clinical description of children with developmental coordination disorder. Can. J. Occup. Ther. 2001, 68, 5–15. [Google Scholar] [CrossRef]
- Zwicker, J.G.; Harris, S.R.; Klassen, A.F. Quality of life domains affected in children with developmental coordination disorder: A systematic review. Child Care Health Dev. 2013, 39, 562–580. [Google Scholar] [CrossRef]
- Summers, J.; Larkin, D.; Dewey, D. Activities of daily living in children with developmental coordination disorder: Dressing, personal hygiene, and eating skills. Hum. Mov. Sci. 2008, 27, 215–229. [Google Scholar] [CrossRef] [PubMed]
- Gualdi-Russo, E.; Manzon, V.S.; Masotti, S.; Toselli, S.; Albertini, A.; Celenza, F.; Zaccagni, L. Weight status and perception of body image in children: The effect of maternal immigrant status. Nutr. J. 2012, 11, 85. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, F.K.; dos Santos, M.A.M.; Almeida, M.B.; Nobre, I.G.; Nobre, G.G.; Silva, W.T.F.E.; Gomes, T.N.; Maia, J.A.R.; Leandro, C.G. Biological and behavioral correlates of body weight status among rural Northeast Brazilian school children. Am. J. Hum. Biol. 2018, 30, e23096. [Google Scholar] [CrossRef]
- Mak, K.K.; Tan, S.H. Underweight problems in Asian children and adolescents. Eur. J. Pediatr. 2012, 171, 779–785. [Google Scholar] [CrossRef]
- De Toia, D.; Klein, D.; Weber, S.; Wessely, N.; Koch, B.; Tokarski, W.; Dordel, S.; Struder, H.; Graf, C. Relationship between anthropometry and motor abilities at pre-school age. Obes. Facts. 2009, 2, 221–225. [Google Scholar] [CrossRef]
- Gouladins, J.B.; Rigoli, D.; Piek, J.P.; Kane, R.; Palacio, S.G.; Casella, E.B.; Nascimento, R.O.; Hasue, R.H.; Oliveira, J.A. The relationship between motor skills, ADHD symptoms, and childhood body weight. Res. Dev. Disabil. 2016, 55, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.C.; Wu, S.K.; Cairney, J.; Hsieh, C.H. Motor coordination and health-related physical fitness of children with developmental coordination disorder: A three-year follow-up study. Res. Dev. Disabil. 2011, 32, 2993–3002. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.C.; Kwan, M.Y.W.; Clark, H.; Hay, J.A.; Faught, B.E.; Cairney, J. A test of the Environmental Stress Hypothesis in children with and without Developmental Coordination Disorder. Psychol. Sport Exerc. 2018, 37, 244–250. [Google Scholar] [CrossRef]
- Cairney, J.; Kwan, M.Y.W.; Hay, J.A.; Faught, B. Developmental Coordination Disorder, gender, and body weight: Examining the impact of participation in active play. Res. Dev. Disabil. 2012, 33, 1566–1573. [Google Scholar] [CrossRef] [PubMed]
- King-Dowling, S.; Rodriguez, C.; Missiuna, C.; Timmons, B.W.; Cairney, J. Health-related fitness in preschool children with and without motor delays. Med. Sci. Sport Exer. 2018, 50, 1442–1448. [Google Scholar] [CrossRef] [PubMed]
- Yam, T.T.T.; Fong, S.S.M.; Tsang, W.W.N. Foot posture index and body composition measures in children with and without developmental coordination disorder. PLoS ONE 2022, 17, e0265280. [Google Scholar] [CrossRef] [PubMed]
| TD (n = 745) | rDCD (n = 80) | p Value | |
|---|---|---|---|
| Age | |||
| Years | 8.37 ± 2.69 | 7.97 ± 2.49 | 0.090 |
| Preschool (n, %) a | 278 (37.3%) | 32 (40.0%) | 0.629 |
| Boys (n, %) a | 372 (49.9%) | 57 (71.2%) | <0.001 |
| Height (cm) | 128.84 ± 16.95 | 127.48 ± 17.52 | 0.591 |
| Weight (kg) | 28.68 ± 11.29 | 28.53 ± 11.32 | 0.844 |
| Body mass index | 16.65 ± 3.21 | 16.83 ± 3.04 | 0.418 |
| Weight status a | |||
| Underweight | 92 (12.3%) | 11 (13.8%) | 0.483 |
| Normal weight | 530 (71.1%) | 52 (65.0%) | |
| Overweight/obesity | 123 (16.5%) | 17 (21.2%) | |
| MABC-2 component score | |||
| Manual dexterity | 31.20 ± 5.10 | 19.29 ± 5.07 | <0.001 |
| Aiming & catching | 19.45 ± 4.88 | 12.94 ± 3.99 | <0.001 |
| Balance | 34.40 ± 3.37 | 26.53 ± 6.26 | <0.001 |
| Total score | 85.06 ± 8.71 | 58.75 ± 7.59 | <0.001 |
| Preschool | School-Aged | Total | |||
|---|---|---|---|---|---|
| TD | rDCD | TD | rDCD | ||
| underweight | 6/1 | 3/1 | 37/48 | 6/1 | 52/51 |
| normal weight | 102/128 | 16/6 | 154/146 | 21/9 | 293/289 |
| overweight/obesity | 27/14 | 5/1 | 46/36 | 6/5 | 84/56 |
| Total | 135/143 | 24/8 | 237/230 | 33/15 | 429/396 |
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| B (SE) | OR | B (SE) | OR | B (SE) | OR | |
| Group | ||||||
| TD | reference | reference | reference | |||
| rDCD | 0.20 (0.35) | 1.22 | 0.27 (0.37) | 1.32 | 1.89 (0.75) | 6.62 * |
| Sex | ||||||
| Boy | reference | reference | ||||
| Girl | 0.06 (0.22) | 1.07 | 0.13 (0.24) | 1.14 | ||
| Age | ||||||
| Preschool | reference | reference | ||||
| School-aged | 1.86 (0.33) | 6.43 *** | 2.24 (0.40) | 9.37 *** | ||
| Group × sex | −0.25 (0.1.27) | 0.78 | ||||
| Group × age | −1.82 (0.88) | 0.16 * | ||||
| Group × sex × age | −0.83 (1.70) | 0.44 | ||||
| Constant | −1.75 (0.11) | 0.17 *** | −3.20 (0.34) | 0.04 *** | −3.57 (0.41) | 0.03 *** |
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| B (SE) | OR | B (SE) | OR | B (SE) | OR | |
| Group | ||||||
| TD | reference | reference | reference | |||
| rDCD | 0.34 (0.30) | 1.41 | 0.28 (0.30) | 1.32 | 0.35 (0.55) | 1.42 |
| Sex | ||||||
| Boy | reference | reference | ||||
| Girl | −0.36 (0.19) | 0.70 † | −0.43 (0.20) | 0.65 * | ||
| Age | ||||||
| Preschool | reference | reference | ||||
| School-aged | 0.40 (0.20) | 1.50 * | 0.41 (0.21) | 1.51 † | ||
| Group × sex | −0.20 (1.21) | 0.82 | ||||
| Group × age | −0.50 (0.72) | 0.61 | ||||
| Group × sex × age | 1.29 (1.40) | 3.65 | ||||
| Constant | −1.46 (0.10) | 0.23 *** | −1.54 (0.19) | 0.21 *** | −1.52 (0.19) | 0.22 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.-C.; Tseng, Y.-T.; Hsu, F.-Y.; Chao, H.-C.; Wu, S.K. Developmental Coordination Disorder and Unhealthy Weight Status in Taiwanese Children: The Roles of Sex and Age. Children 2023, 10, 1171. https://doi.org/10.3390/children10071171
Li Y-C, Tseng Y-T, Hsu F-Y, Chao H-C, Wu SK. Developmental Coordination Disorder and Unhealthy Weight Status in Taiwanese Children: The Roles of Sex and Age. Children. 2023; 10(7):1171. https://doi.org/10.3390/children10071171
Chicago/Turabian StyleLi, Yao-Chuen, Yu-Ting Tseng, Fang-Yu Hsu, Hsuan-Chu Chao, and Sheng K. Wu. 2023. "Developmental Coordination Disorder and Unhealthy Weight Status in Taiwanese Children: The Roles of Sex and Age" Children 10, no. 7: 1171. https://doi.org/10.3390/children10071171
APA StyleLi, Y.-C., Tseng, Y.-T., Hsu, F.-Y., Chao, H.-C., & Wu, S. K. (2023). Developmental Coordination Disorder and Unhealthy Weight Status in Taiwanese Children: The Roles of Sex and Age. Children, 10(7), 1171. https://doi.org/10.3390/children10071171







