Prognosis Communication in Pediatric Oncology: A Systematic Review
Abstract
1. Introduction
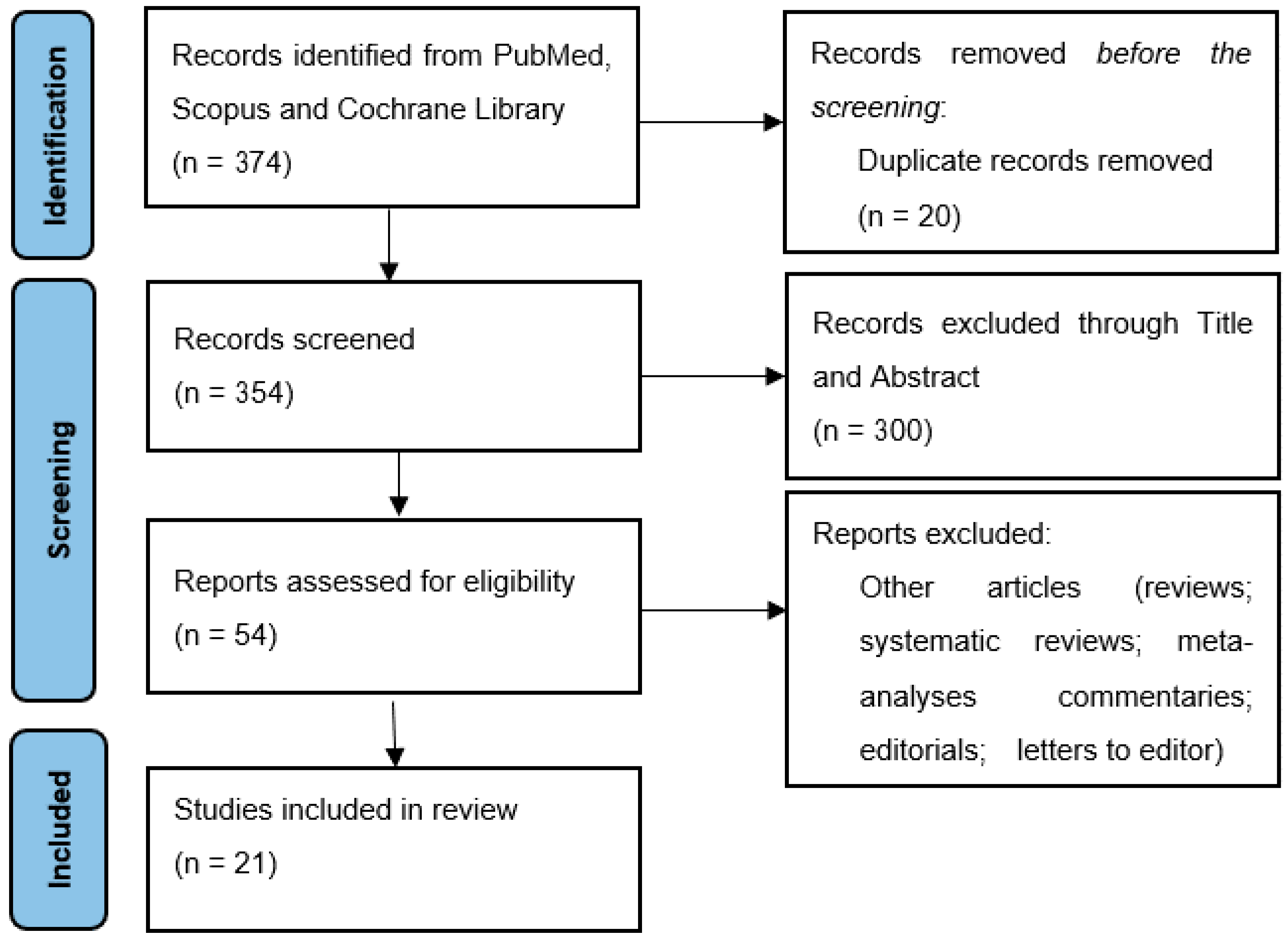
2. Materials and Methods
2.1. Study Design
2.2. Selection Criteria
2.3. Data Extraction
2.4. Quality Assessment
3. Results
3.1. Overview
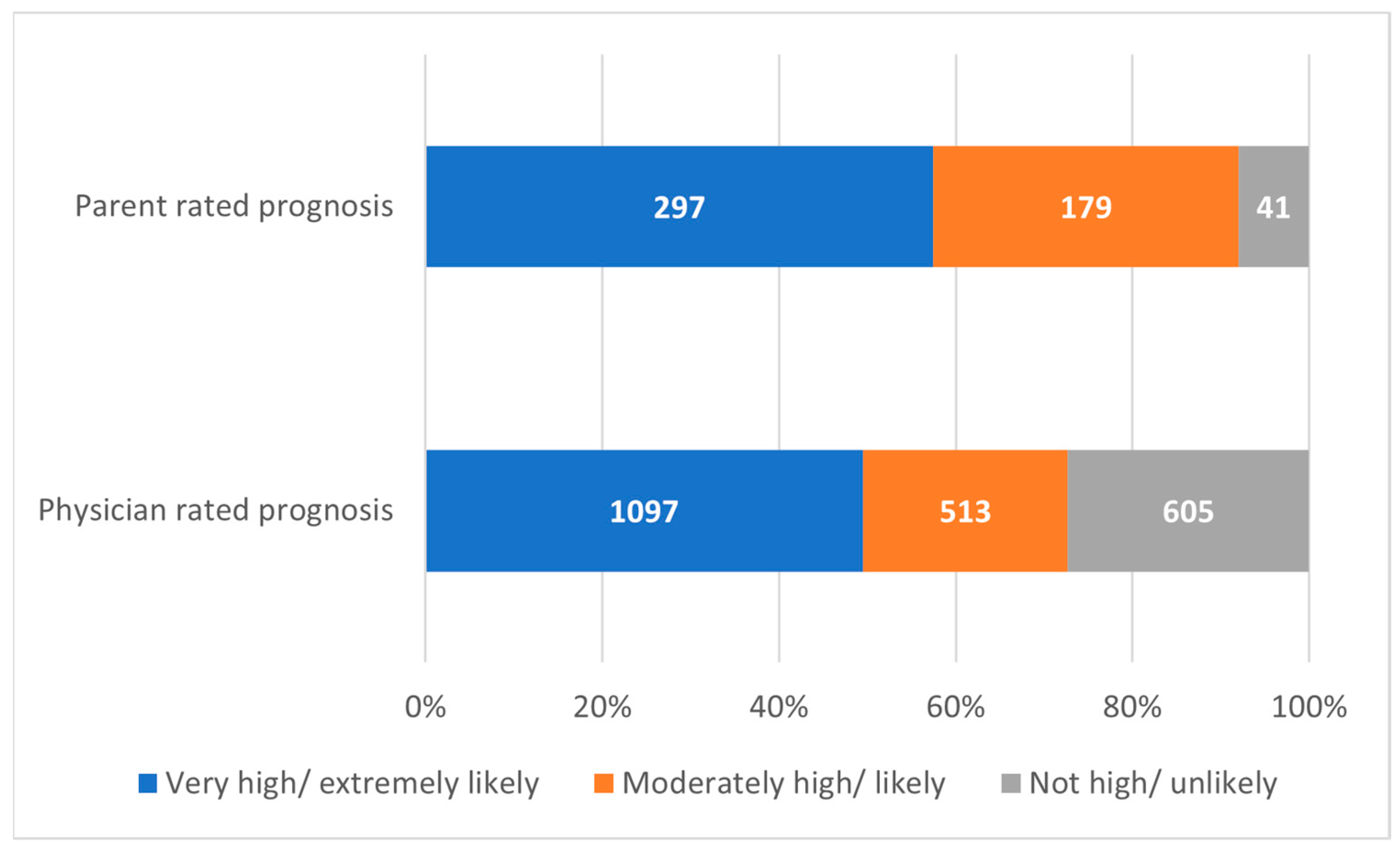
3.2. Parents
3.3. Pediatric Oncology Patients
3.4. Physicians
4. Discussion
4.1. Parents
4.2. Pediatric Oncology Patients
4.3. Physicians
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hrdlickova, L.; Polakova, K.; Loucka, M. Important Aspects Influencing Delivery of Serious News in Pediatric Oncology: A Scoping Review. Children 2021, 8, 166. [Google Scholar] [CrossRef] [PubMed]
- Stein, A.; Dalton, L.; Rapa, E.; Bluebond-Langner, M.; Hanington, L.; Stein, K.F.; Ziebland, S.; Rochat, T.; Harrop, E.; Kelly, B.; et al. Communication with children and adolescents about the diagnosis of their own life-threatening condition. Lancet 2019, 393, 1150–1163. [Google Scholar] [CrossRef] [PubMed]
- Sisk, B.A.; Bluebond-Langner, M.; Wiener, L.; Mack, J.; Wolfe, J. Prognostic Disclosures to Children: A Historical Perspective. Pediatrics 2016, 138, e20161278. [Google Scholar] [CrossRef]
- Blazin, L.J.; Cecchini, C.; Habashy, C.; Kaye, E.C.; Baker, J.N. Communicating Effectively in Pediatric Cancer Care: Translating Evidence into Practice. Children 2018, 5, 40. [Google Scholar] [CrossRef]
- Sisk, B.A.; Harvey, K.; Friedrich, A.B.; Antes, A.L.; Yaeger, L.H.; Mack, J.W.; DuBois, J.M. Multilevel barriers and facilitators of communication in pediatric oncology: A systematic review. Pediatr. Blood Cancer 2022, 69, e29405. [Google Scholar] [CrossRef]
- Epstein, R.M.; Street, R.L., Jr. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering; National Cancer Institute: Bethesda, MD, USA, 2007; NIH Publication No. 07-6225.
- Marsac, M.L.; Kindler, C.; Weiss, D.; Ragsdale, L. Let’s Talk About It: Supporting Family Communication during End-of-Life Care of Pediatric Patients. J. Palliat. Med. 2018, 21, 862–878. [Google Scholar] [CrossRef] [PubMed]
- Sisk, B.A.; Mack, J.W.; Ashworth, R.; DuBois, J. Communication in pediatric oncology: State of the field and research agenda. Pediatr. Blood Cancer 2017, 65, e26727. [Google Scholar] [CrossRef]
- Lin, B.; Gutman, T.; Hanson, C.S.; Ju, A.; Manera, K.; Butow, P.; Cohn, R.J.; Dalla-Pozza, L.; Greenzang, K.A.; Mack, J.; et al. Communication during childhood cancer: Systematic review of patient perspectives. Cancer 2020, 126, 701–716. [Google Scholar] [CrossRef]
- Madden, K.; Wolfe, J.; Collura, C. Pediatric Palliative Care in the Intensive Care Unit. Crit. Care Nurs. Clin. N. Am. 2015, 27, 341–354. [Google Scholar] [CrossRef]
- Ilowite, M.F.; Cronin, A.M.; Kang, T.I.; Mack, J.W. Disparities in prognosis communication among parents of children with cancer: The impact of race and ethnicity. Cancer 2017, 123, 3995–4003. [Google Scholar] [CrossRef]
- Kaye, E.C.; Gattas, M.; Bluebond-Langner, M.; Baker, J.N. Longitudinal investigation of prognostic communication: Feasibility and acceptability of studying serial disease reevaluation conversations in children with high-risk cancer. Cancer 2019, 126, 131–139. [Google Scholar] [CrossRef]
- McCarthy, S.R.B.; Kang, T.I.; Mack, J.W. Inclusion of children in the initial conversation about their cancer diagnosis: Impact on parent experiences of the communication process. Support. Care Cancer 2019, 27, 1319–1324. [Google Scholar] [CrossRef] [PubMed]
- Sisk, B.A.; Kang, T.I.; Mack, J.W. How Parents of Children With Cancer Learn About Their Children’s Prognosis. Pediatrics 2017, 141, e20172241. [Google Scholar] [CrossRef] [PubMed]
- Levine, D.R.; Cuviello, A.; Nelson, C.; Lu, Z.; Mandrell, B.N.; Baker, J.N. Hope-Colored Glasses: Perceptions of Prognosis Among Pediatric Oncology Patients and Their Parents. JCO Oncol. Pract. 2021, 17, e730–e739. [Google Scholar] [CrossRef] [PubMed]
- Marron, J.M.; Cronin, A.M.; Kang, T.I.; Mack, J.W. Intended and unintended consequences: Ethics, communication, and prognostic disclosure in pediatric oncology. Cancer 2018, 124, 1232–1241. [Google Scholar] [CrossRef]
- Sisk, B.A.; Kang, T.I.; Mack, J.W. Prognostic disclosures over time: Parental preferences and physician practices. Cancer 2017, 123, 4031–4038. [Google Scholar] [CrossRef]
- Bluebond-Langner, M.; Hall, N.; Vincent, K.; Henderson, E.M.; Russell, J.; Beecham, E.; Bryan, G.; Gains, J.E.; Gaze, M.N.; Slater, O.; et al. Parents’ responses to prognostic disclosure at diagnosis of a child with a high-risk brain tumor: Analysis of clinician-parent interactions and implications for clinical practice. Pediatr. Blood Cancer 2021, 68, e28802. [Google Scholar] [CrossRef]
- Brand, S.R.; Fasciano, K.; Mack, J.W. Communication preferences of pediatric cancer patients: Talking about prognosis and their future life. Support. Care Cancer 2017, 25, 769–774. [Google Scholar] [CrossRef]
- Greenzang, K.A.; Cronin, A.M.; Kang, T.I.; Mack, J.W. Parental distress and desire for information regarding long-term implications of pediatric cancer treatment. Cancer 2018, 124, 4529–4537. [Google Scholar] [CrossRef]
- Kim, M.S.; Lee, J.; Sim, J.-A.; Kwon, J.H.; Kang, E.J.; Kim, Y.J.; Lee, J.; Song, E.-K.; Kang, J.H.; Nam, E.M.; et al. Discordance between Physician and the General Public Perceptions of Prognostic Disclosure to Children with Serious Illness: A Korean Nationwide Study. J. Korean Med. Sci. 2018, 33, e327, Erratum in J. Korean Med. Sci. 2019, 34, e30; Erratum in J. Korean Med. Sci. 2020, 35, e74. [Google Scholar] [CrossRef]
- Nelson, M.; Kelly, D.; McAndrew, R.; Smith, P. ‘Just gripping my heart and squeezing’: Naming and explaining the emotional experience of receiving bad news in the paediatric oncology setting. Patient Educ. Couns. 2017, 100, 1751–1757. [Google Scholar] [CrossRef] [PubMed]
- Porter, A.S.; Woods, C.; Stall, M.; Velrajan, S.; Baker, J.N.; Mack, J.W.; Kaye, E.C. Oncologist approaches to communicating uncertain disease status in pediatric cancer: A qualitative study. BMC Cancer 2022, 22, 1109. [Google Scholar] [CrossRef] [PubMed]
- Bartholdson, C.; Kreicbergs, U.; Sveen, J.; Lövgren, M.; Pohlkamp, L. Communication about diagnosis and prognosis—A population-based survey among bereaved parents in pediatric oncology. Psychooncology 2022, 31, 2149–2158. [Google Scholar] [CrossRef] [PubMed]
- Sisk, B.A.; Kang, T.I.; Mack, J.W. Racial and Ethnic Differences in Parental Decision-Making Roles in Pediatric Oncology. J. Palliat. Med. 2020, 23, 192–197. [Google Scholar] [CrossRef]
- Sisk, B.A.; Friedrich, A.; Blazin, L.J.; Baker, J.N.; Mack, J.W.; DuBois, J. Communication in Pediatric Oncology: A Qualitative Study. Pediatrics 2020, 146, e20201193. [Google Scholar] [CrossRef]
- Mack, J.W.; Kang, T.I. Care experiences that foster trust between parents and physicians of children with cancer. Pediatr. Blood Cancer 2020, 67, e28399. [Google Scholar] [CrossRef]
- Mack, J.W.; Cronin, A.M.; Uno, H.; Shusterman, S.; Twist, C.J.; Bagatell, R.; Rosenberg, A.; Marachelian, A.; Granger, M.M.; Bender, J.G.; et al. Unrealistic parental expectations for cure in poor-prognosis childhood cancer. Cancer 2020, 126, 416–424. [Google Scholar] [CrossRef]
- Sisk, B.A.; Friedrich, A.B.; Kaye, E.C.; Baker, J.N.; Mack, J.W.; DuBois, J.M. Multilevel barriers to communication in pediatric oncology: Clinicians’ perspectives. Cancer 2021, 127, 2130–2138. [Google Scholar] [CrossRef]
- Cicero-Oneto, C.E.; Valdez-Martinez, E.; Bedolla, M. Decision-making on therapeutic futility in Mexican adolescents with cancer: A qualitative study. BMC Med. Ethics 2017, 18, 74. [Google Scholar] [CrossRef]
- Mant, J.; Kirby, A.; Cox, K.J.; Burke, A. Children’s experiences of being diagnosed with cancer at the early stages of treatment; an interpretive phenomenological analysis. Clin. Child Psychol. Psychiatry 2019, 24, 3–18. [Google Scholar] [CrossRef]
- Kaye, E.C.; Kiefer, A.; Zalud, K.; Gattas, M.; Snyder, I.; Spraker-Perlman, H.; Baker, J.N. Advancing the field of communication research in pediatric oncology: A systematic review of the literature analyzing medical dialogue. Pediatr. Blood Cancer 2018, 65, e27378. [Google Scholar] [CrossRef] [PubMed]
- Snaman, J.M.; Kaye, E.C.; Baker, J.; Wolfe, J. Pediatric palliative oncology: The state of the science and art of caring for children with cancer. Curr. Opin. Pediatr. 2018, 30, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Zanon, B.P.; Cremonese, L.; Ribeiro, A.C.; Padoin, S.M.D.M.; De Paula, C.C. Communication of bad news in pediatrics: Integrative review. Rev. Bras. Enferm. 2020, 73 (Suppl. 4), e20190059. [Google Scholar] [CrossRef] [PubMed]
- Mack, J.W.; Hilden, J.M.; Watterson, J.; Moore, C.; Turner, B.; Grier, H.E.; Weeks, J.C.; Wolfe, J. Parent and Physician Perspectives on Quality of Care at the End of Life in Children With Cancer. J. Clin. Oncol. 2005, 23, 9155–9161. [Google Scholar] [CrossRef]
- Sisk, B.A.; Greenzang, K.A.; Kang, T.I.; Mack, J.W. Longitudinal parental preferences for late effects communication during cancer treatment. Pediatr. Blood Cancer 2018, 65, e26760. [Google Scholar] [CrossRef]
- Sisk, B.A.; Fasciano, K.; Block, S.D.; Mack, J.W. Longitudinal prognostic communication needs of adolescents and young adults with cancer. Cancer 2020, 126, 400–407. [Google Scholar] [CrossRef]
- Weaver, M.S.; Heinze, K.E.; Kelly, K.P.; Wiener, L.; Casey, R.L.; Bell, C.J.; Wolfe, J.; Garee, A.M.; Watson, A.; Hinds, P.S. Palliative Care as a Standard of Care in Pediatric Oncology. Pediatr. Blood Cancer 2015, 62 (Suppl. 5), S829–S833. [Google Scholar] [CrossRef]
- Miller, K.S.; Vannatta, K.; Compas, B.E.; Vasey, M.; McGoron, K.D.; Salley, C.; Gerhardt, C.A. The Role of Coping and Temperament in the Adjustment of Children with Cancer. J. Pediatr. Psychol. 2009, 34, 1135–1143. [Google Scholar] [CrossRef]
- Verrill, J.R.; Schafer, J.; Vannatta, K.; Noll, R.B. Aggression, Antisocial Behavior, and Substance Abuse in Survivors of Pediatric Cancer: Possible Protective Effects of Cancer and Its Treatment. J. Pediatr. Psychol. 2000, 25, 493–502. [Google Scholar] [CrossRef]
- Horhat, R.M.; Vlaicu, B.; Bagiu, R.; Putnoky, S.; Bagiu, I.C.; Horhat, D.I.; Szuhanek, C.; Sinescu, C.; Negrutiu, M.L.; Nica, L. A Ten-year Time Laps, Regarding Drug Consumption in the Western Part of Romania. Rev. Chim. 2018, 69, 1371–1375. [Google Scholar] [CrossRef]
- Marjerrison, S.; Hendershot, E.; Empringham, B.; Nathan, P.C. Smoking, Binge Drinking, and Drug Use Among Childhood Cancer Survivors: A Meta-Analysis. Pediatr. Blood Cancer 2016, 63, 1254–1263. [Google Scholar] [CrossRef]
- Graetz, D.E.; Garza, M.; Rodriguez-Galindo, C.; Mack, J.W. Pediatric cancer communication in low- and middle-income countries: A scoping review. Cancer 2020, 126, 5030–5039. [Google Scholar] [CrossRef] [PubMed]
- Porter, A.S.; Chow, E.; Woods, C.; Lemmon, M.E.; Baker, J.N.; Mack, J.W.; Kaye, E.C. Navigating prognostic communication when children with poor-prognosis cancer experience prolonged disease stability. Pediatr. Blood Cancer 2023, 70, e29920. [Google Scholar] [CrossRef] [PubMed]
- Feraco, A.M.; Brand, S.R.; Mack, J.W.; Kesselheim, J.C.; Block, S.D.; Wolfe, J. Communication Skills Training in Pediatric Oncology: Moving Beyond Role Modeling. Pediatr. Blood Cancer 2016, 63, 966–972. [Google Scholar] [CrossRef]
- Mu, P.-F.; Lee, M.-Y.; Sheng, C.-C.; Tung, P.-C.; Huang, L.-Y.; Chen, Y.-W. The experiences of family members in the year following the diagnosis of a child or adolescent with cancer: A qualitative systematic review. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 293–329. [Google Scholar] [CrossRef]
| Nr. | Study Type | Country | Year | Focus on | Quality Score |
|---|---|---|---|---|---|
| 1 [11] | Prospective questionnaire cohort | USA | 2017 | Parents and clinicians | good |
| 2 [12] | Prospective questionnaire/interview cohort | USA | 2019 | Parents | fair |
| 3 [13] | Prospective questionnaire cohort | USA | 2019 | Parents and children | fair |
| 4 [14] | Prospective questionnaire cohort | USA | 2017 | Parents | fair |
| 5 [15] | Prospective questionnaire cohort | USA | 2021 | Parents and children | fair |
| 6 [16] | Prospective questionnaire cohort | USA | 2018 | Parents | fair |
| 7 [17] | Prospective questionnaire cohort | USA | 2017 | Parents | fair |
| 8 [18] | Prospective interview cohort | UK | 2020 | Parents | good |
| 9 [19] | Prospective interview cohort | USA | 2017 | Children | fair |
| 10 [20] | Prospective questionnaire cohort | USA | 2018 | Parents | fair |
| 11 [21] | Prospective questionnaire cohort | Republic of Korea | 2018 | Clinicians and general population | good |
| 12 [22] | Retrospective interview cohort | UK | 2017 | Parents | fair |
| 13 [23] | Prospective interview cohort | USA | 2022 | Parents, children and clinicians | fair |
| 14 [24] | Prospective questionnaire cohort—population-based nationwide survey | Sweden | 2022 | Parents and children | fair |
| 15 [25] | Prospective questionnaire cohort | USA | 2020 | Parents | fair |
| 16 [26] | Prospective interview cohort | USA | 2020 | Parents | fair |
| 17 [27] | Prospective questionnaire cohort | USA | 2020 | Parents | good |
| 18 [28] | Prospective questionnaire cohort | USA | 2020 | Parents | fair |
| 19 [29] | Prospective interview cohort—focus groups | USA | 2021 | Clinicians | fair |
| 20 [30] | Prospective interview cohort | Mexico | 2017 | Parents, children and clinicians | fair |
| 21 [31] | Prospective interview cohort | UK | 2018 | Children | fair |
| Prognosis Disclosure | Trust | Parental Distress | Decision Making | ||||
|---|---|---|---|---|---|---|---|
| Total | 2221 | Total | 1560 | Total | 782 | Total | 827 |
| Yes | 92.17% | High levels | 73.01% | High | 34.40% | Parent-led | 48.00% |
| No | 7.83% | Moderate levels | 6.09% | Moderate | 46.68% | Oncologist-led | 23.58% |
| Low levels | 20.90% | Low/None | 18.93% | Shared | 28.42% | ||
| NR * | 5 | NR * | 9 | NR * | 10 | NR * | 8 |
| QD * | 12 | QD * | 6 | QD * | 4 | QD * | 4 |
| NQD * | 0 | NQD * | 2 | NQD * | 3 | NQD * | 5 |
| Parents (%) | QD | NQD | |
|---|---|---|---|
| Accurate understanding | 43.15% | 3 | 3 |
| Acknowledgment of barriers | 15.38% | 1 | 1 |
| Desire for more information about disease | 86.98% | 3 | - |
| Desire for more information about curability | 78.84% | 2 | - |
| Parent rated high-quality information | 56.71% | 5 | - |
| Parent rated low-quality information | 40.24% | 5 | - |
| Parent rated high-quality communication | 52.73% | 5 | - |
| Parent rated low-quality communication | 46.32% | 5 | - |
| Parent rated the usefulness of study | 62.07% | 1 | - |
| Respectful/sensitive/softened manner of communication | 90.78% | 1 | 3 |
| Racial discrepancies in communication | - | - | 2 |
| Parents (%) | QD | NQD | |
|---|---|---|---|
| Pessimism or struggle | 36.36% | 5 | - |
| Optimism | 48.52% | 4 | 1 |
| Depression | 29.52% | 2 | - |
| Anxiety | 51.41% | 2 | - |
| Hope | 52.67% | 2 | 2 |
| Acceptance or peace of mind | 56.30% | 4 | 1 |
| Help in managing uncertainty | 66.10% | 2 | 1 |
| Decisional regret | 23.33% | 2 | - |
| Strong religious/spiritual beliefs | 37.18% | 2 | 2 |
| Total * n = 3080 | % | QD | % | QD | % | QD | ||
|---|---|---|---|---|---|---|---|---|
| Hematologic Malignancies | 46.56% | 14 | Solid Tumors | 39.51% | 14 | Brain Tumors | 13.93% | 13 |
| Leukemia | 28.92% | 4 | Ewing sarcoma | 8.64% | 2 | Medulloblastoma | 5.42% | 2 |
| AML | 16.07% | 3 | Rhabdomyosarcoma | 6.17% | 2 | Glioma | 6.19% | 2 |
| ALL | 12.85% | 3 | Neuroblastoma | 9.88% | 3 | Teratoma | 2.32% | 1 |
| Lymphoma | 17.64% | 2 | Melanoma | 2.47% | 1 | |||
| Hodgkin | 8.82% | 1 | Wilms tumor | 1.23% | 1 | |||
| Non- Hodgkin | 8.82% | 1 | Germ cell tumor | 2.47% | 2 | |||
| Hepatoblastoma | 1.23% | 1 | ||||||
| Colon adeno-carcinoma | 2.47% | 1 | ||||||
| Osteosarcoma | 4.94% | 1 |
| Children (%) | QD | NQD | |
|---|---|---|---|
| Discrepancies in meeting presence due to age | - | - | 1 |
| Direct disclosure | 42.49% | 2 | 1 |
| Softening the message | - | - | 1 |
| Desire to know more about disease | - | - | 3 |
| Desire to know more about treatment | - | - | 3 |
| Involved in decision making | 33.33% | 1 | 1 |
| Children (n, %) | QD | NQD | |
|---|---|---|---|
| Pessimism | 15.00% | 1 | 1 |
| Optimism | 43.00% | 1 | - |
| Distress and/or anxiety | 66.67% | 1 | 2 |
| Required emotional management and reassurance | 100.00% | 1 | 2 |
| Need for management of uncertainty | 47.50% | 1 | 2 |
| Strong religious/spiritual beliefs | 100.00% | 1 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boeriu, E.; Borda, A.; Miclea, E.; Boeriu, A.-I.; Vulcanescu, D.D.; Bagiu, I.C.; Horhat, F.G.; Kovacs, A.F.; Avram, C.R.; Diaconu, M.M.; et al. Prognosis Communication in Pediatric Oncology: A Systematic Review. Children 2023, 10, 972. https://doi.org/10.3390/children10060972
Boeriu E, Borda A, Miclea E, Boeriu A-I, Vulcanescu DD, Bagiu IC, Horhat FG, Kovacs AF, Avram CR, Diaconu MM, et al. Prognosis Communication in Pediatric Oncology: A Systematic Review. Children. 2023; 10(6):972. https://doi.org/10.3390/children10060972
Chicago/Turabian StyleBoeriu, Estera, Alexandra Borda, Eunice Miclea, Amalia-Iulia Boeriu, Dan Dumitru Vulcanescu, Iulia Cristina Bagiu, Florin George Horhat, Alexandra Flavia Kovacs, Cecilia Roberta Avram, Mircea Mihai Diaconu, and et al. 2023. "Prognosis Communication in Pediatric Oncology: A Systematic Review" Children 10, no. 6: 972. https://doi.org/10.3390/children10060972
APA StyleBoeriu, E., Borda, A., Miclea, E., Boeriu, A.-I., Vulcanescu, D. D., Bagiu, I. C., Horhat, F. G., Kovacs, A. F., Avram, C. R., Diaconu, M. M., Vlaicu, L. F., Sirb, O. D., & Arghirescu, S. T. (2023). Prognosis Communication in Pediatric Oncology: A Systematic Review. Children, 10(6), 972. https://doi.org/10.3390/children10060972







