Oral Health in migrants children in Melilla, Spain
Abstract
1. Introduction
2. Materials and Methods
2.1. Type of Study and Design
2.2. Statistical Methods
3. Results
4. Discussion
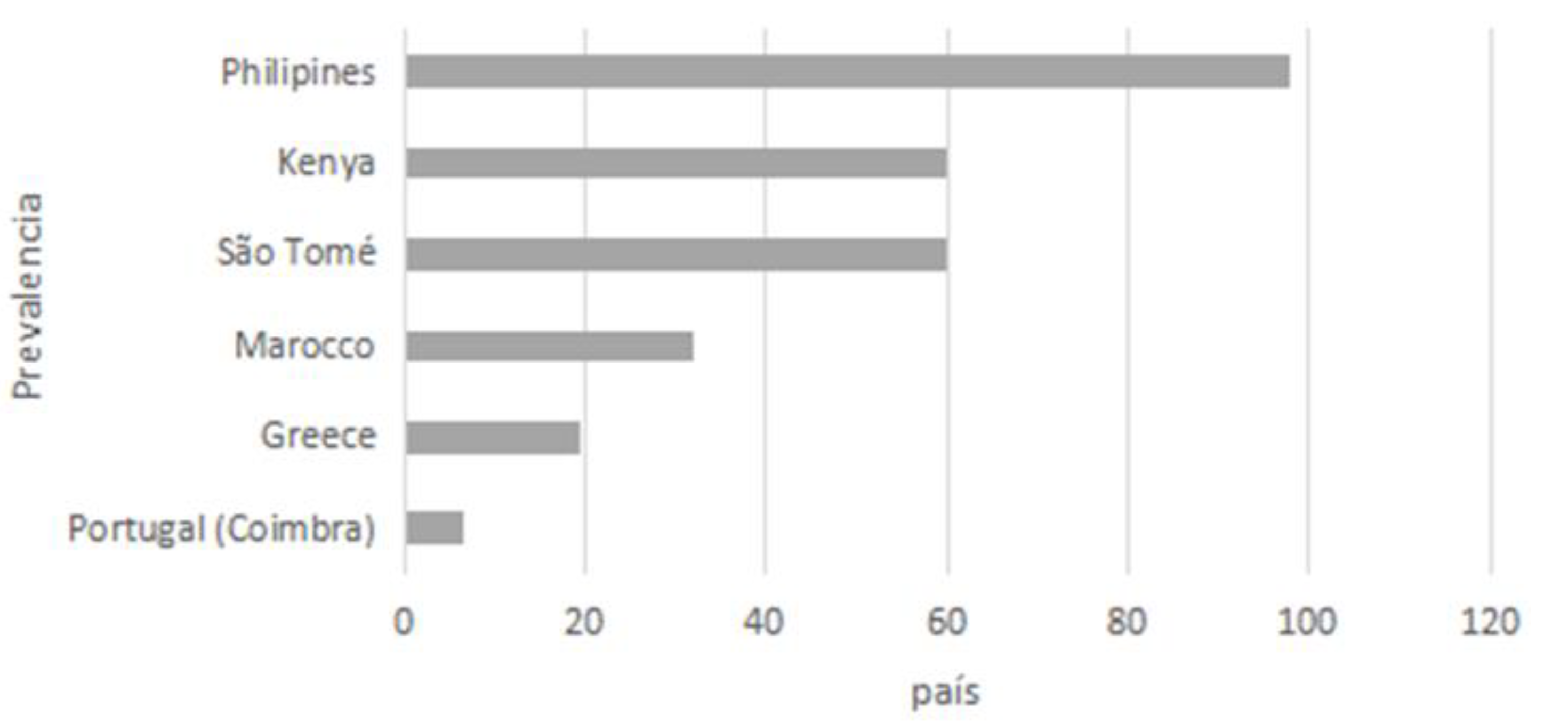
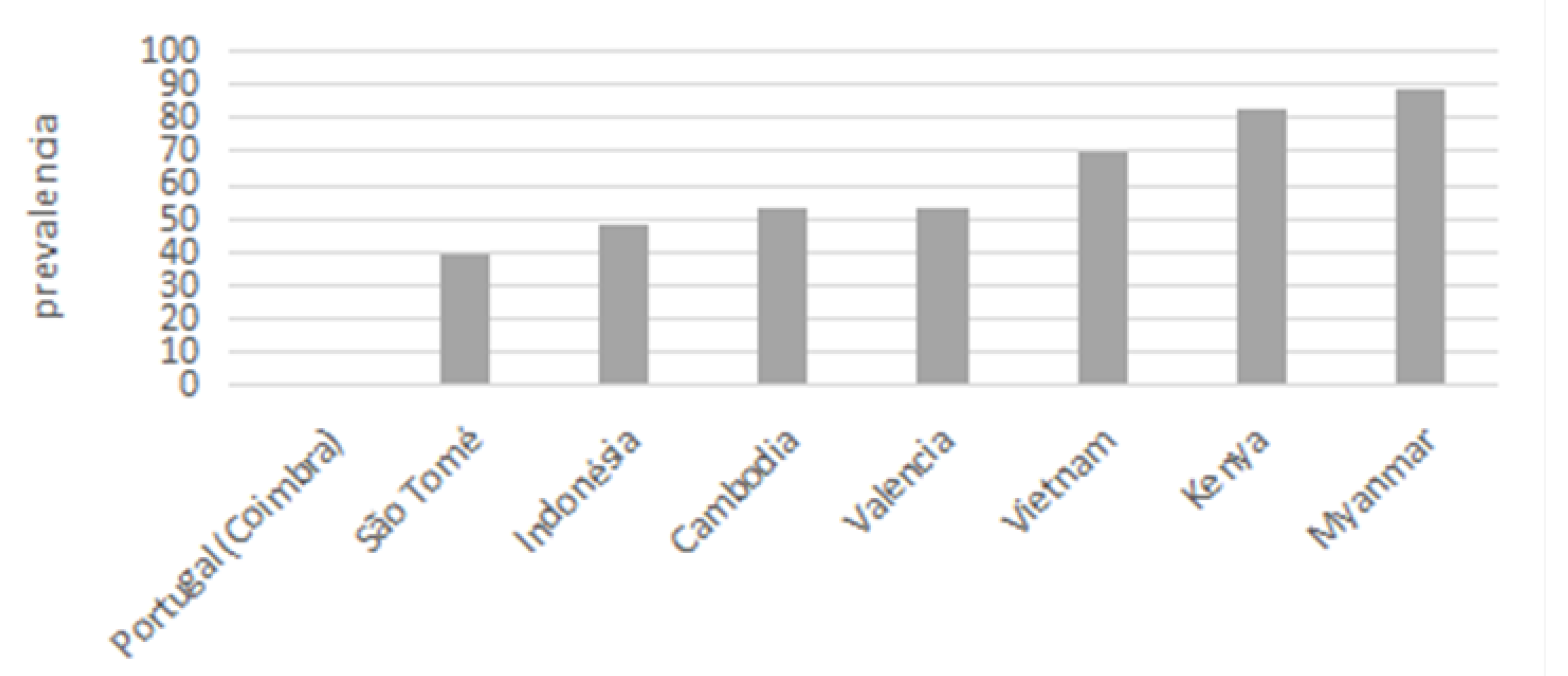
4.1. Caries
4.2. Significant Caries Index
4.3. Restauration Index
4.4. Treatment Needs
4.5. Periodontal Status
4.6. Need for Resources and Specific Oral Health Program
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cotanda, F.L. Manual de Administración y Gestión Sanitaria; Ediciones Díaz de Santos: Madrid, Spain, 1998. [Google Scholar]
- Ortiz, A. Claves del Triángulo Marruecos, Ceuta y Melilla: Inmigración, Economía y Política; Grupo de Estudios Estratégicos (GEES): Madrid, Spain, 2010. [Google Scholar]
- Achotegui, J. Emigrar Hoy En Situaciones Extremas. El síndrome De Ulises. Aloma Rev. De Psicol. Ciències De L’educació I De L’esport Blanquerna 2012, 30, 79–86. Available online: https://raco.cat/index.php/Aloma/article/view/263043 (accessed on 14 February 2021).
- Castaño, A.; Ribas, D. Odontología Preventiva y Comunitaria. La Odontología Social un Deber, una Necesidad, un Reto, 1st ed.; Universidad de Sevilla: Sevilla, Spain, 2012; pp. 927–932. [Google Scholar]
- Bleiker, R.; Campbell, D.; Hutchison, E.; Nicholson, X. The visual dehumanisation of refugees. Aust. J. Political Sci. 2013, 48, 398–416. [Google Scholar] [CrossRef]
- Salehyan, I.; Gleditsch, K.S. Refugees and the Spread of Civil War. Int. Organ. 2006, 60, 335–366. [Google Scholar] [CrossRef]
- Wennhall, I. El proyecto Rosengard. Prevención para prescolares con carencias sociales en Castaño A, Ribas D. In Odontología Preventiva y Comunitaria. La Odontología Social un Deber, una Necesidad, un Reto; Fundación Odontología Social: Sevilla, Spain, 2012; pp. 1065–1080. [Google Scholar]
- Kupský, A. History and changes of Swedish migration policy. J. Geogr. Politics Soc. 2017, 7, 50–56. [Google Scholar]
- Menardia, V.; Casá, A. Clínica Odontológica Solidaria del Colegio Oficial de Odontólogos y Estomatólogos de Catalunya (COEC). Atención a Refugiados en Grecia en Castaño A. Odontología Social. Un Proyecto Iberoamericano Para el Mundo; Huelva, Ed.; Diputación de Huelva, 2017; pp. 115–120. [Google Scholar]
- Castaño, A.; Carroquino, R.; Rubiano, S. Atención Odontológica Para Refugiados en la Frontera Sur de Europa. Melilla-España en Castaño A. Odontología Social. Un Proyecto Iberoamericano Para el Mundo; Huelva, Ed.; Diputación de Huelva, 2017; pp. 121–130. [Google Scholar]
- López Guzmán, T.J.; González Fernández, V.; Herrera Torres, L.; Lorenzo Quiles, O. Melilla: Ciudad fronteriza internacional e intercontinental. Análisis histórico, económico y educativo. Front. Norte 2007, 19, 7–33. [Google Scholar]
- Briones, R.; Salguero, O.; Tarrés, S. Diversidad Religiosa en Ceuta y Melilla; Icaria Editorial: Barcelona, Spain, 2013. [Google Scholar]
- Ferrer Gallardo, X. Acrobacias Fronterizas en Ceuta y Melilla. Explorando la Gestión de los Perímetros Terrestres de la Unión Europea en el Continente Africano. Doc. d’Anàlisi Geogràfica 2008, 51, 129–149. Available online: https://raco.cat/index.php/DocumentsAnalisi/article/view/120014 (accessed on 15 January 2021).
- González Enríquez, C.; Pérez González, A. Ceuta y Melilla: Nuevos Elementos en el Escenario. Boletín Elcano 2008, 109, 7. Available online: http://www.realinstitutoelcano.org/wps/portal/rielcano/BoletinVista?WCM_GLOBAL_CONTEXT=/elcano/elcano_es/boletines/bolet_n+109 (accessed on 15 January 2021).
- López Bueno, J.M. Melilla: Lecciones Inadvertidas de Integración. Boletín Elcano 2010, 10. Melilla: Lecciones Inadvertidas de Integración (ARI)-Real Instituto Elcano, España. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=3611016 (accessed on 15 January 2021).
- López-Sala, A. La Inmigración Irregular En Ceuta Y Melilla En 2014: Prácticas De Control Y Debate Público. Anu. CIDOB De La Inmigr. 2015, 169–192. Available online: https://raco.cat/index.php/AnuarioCIDOBInmigracion/article/view/312793 (accessed on 15 January 2021).
- Sánchez, M.Á.A. Las fronteras terrestres de España en Melilla: Delimitación, vallas fronterizas y tierra de nadie. Rev. Electrónica Estud. Int. (REEI) 2014, 28, 7–34. [Google Scholar] [CrossRef]
- García, I.G. Rechazon en las Fronteras Exteriores Europeas con Marruecos: Immigración y Derechos Humanos en las Vallas de Ceuta y Melilla 2005–2017. Rev. Gen. Derecho Eur. 2017, 43, 17–57. [Google Scholar]
- Soddu, P. Ceuta y Melilla: Gestión Fronteriza, Derechos Humanos y Seguridad; IEMed-CIDOB, Ed.; Anuario IEMed del Mediterráneo, Instituto Europeo del Mediterráneo, España, 2006; pp. 216–218. Available online: http://europa.eu/rapid/pressReleasesAction.do?reference=MEMO/05/380&format=PDF&aged=1&language=EN&guiLanguage=en (accessed on 15 January 2021).
- Bondanini, F.B. Migración de Tránsito: Entre Temporalidad y Largas Esperas. El Caso del CETI de Melilla. Antropol. Exp. 2014, 14, 189–206, Recuperado a Partir de. Available online: https://revistaselectronicas.ujaen.es/index.php/rae/article/view/1791 (accessed on 15 January 2021).
- Gonçalves Riatto, S. Estudio Epidemológico de Salud Oral en una Poblacion Infantil del Centro de Estancia Tempotal de Inmigrantes de Melilla. Doctoral Thesis, Universidad de Salamanca, Salamanca, Spain, 2016. [Google Scholar]
- Ahmed, R.A. El Habitar de los Refugiados: El Caso del CETI de Melilla; Universidad de Sevilla: Sevilla, Spain, 2020. [Google Scholar]
- Martín, J.A.M. La inmigración ilegal en la ciudad de Melilla: Flujos migratorios. In Inmigracion y Desarrollo Regional: IX Congreso de la Asociación Andaluza de Ciencia Regional: Almería, 2007; Universidad de Almería: Almería, Spain, 2009; pp. 303–320. [Google Scholar]
- Sevillano Garcés, D. Estudio de Salud Bucodental y Calidad de Vida Oral en Niños Sirios del “Centro de Estancia Temporal de Inmigrantes”(CETI, Melilla); Universidad de Sevilla: Sevilla, Spain, 2018. [Google Scholar]
- Mizzian, S.A.; Alonso, M.F. Migrantes Subsaharianos en sus primeros asentamientos pre y post frontera española. Aposta. Rev. Cienc. Soc. 2019, 80, 27–43. [Google Scholar]
- Sagnella, A. En los pliegues del Mediterráneo: Ceuta y Melilla. Rev. Urug. Antropol. Etnogr. 2020, 5, 31–49. [Google Scholar]
- Cañas, R.C. El número de nuestros colegiados se triplicará en tres años, lo que llevará a una saturación de profesionales: Doctor Rafael Carroquino, presidente del Colegio Oficial de Odontólogos y Estomatólogos de Melilla. Gac. Dent. Ind. Y Prof. España 2012, 239, 82–85. [Google Scholar]
- Fernández Sánchez, R.D.M. Fundación Odontológica Social. Doctoral Thesis, University of Sevilla, Sevilla, Spain, 2016. [Google Scholar]
- Goncalves, S.; Montero, J.; Ribas, D.; Castaño-Séiquer, A.; Dib, A. Oral Health Status of Syrian Children in the Refugee Center of Melilla, Spain. Int. J. Dent. 2018, 2018, 2637508. [Google Scholar] [CrossRef]
- WHO. Oral Health Surveys: Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Kloning, T.; Nowotny, T.; Alberer, M.; Hoelscher, M.; Hoffmann, A.; Froeschl, G. Morbidity profile and sociodemographic characteristics of unaccompanied refugee minors seen by paediatric practices between October 2014 and February 2016 in Bavaria, Germany. BMC Public Health 2018, 7, 983. [Google Scholar] [CrossRef]
- World Vision. Syrian Refugee Crisis: Facts FAQ and How to Help. Available online: https://www.worldvision.org/refugees-news-stories/syrian-refugee-crisis-facts (accessed on 3 August 2019).
- Coimbra, F.; Mendes, S.; Bernardo, M. Prevalência e gravidade de cárie dentária numa população infantil de S. Tomé. Rev. Port. Estomatol. Med. Dentária Cir. Maxilofac. 2013, 54, 20–26. [Google Scholar] [CrossRef]
- Bourgeois, D.M.; Llodra, J.C. Global burden of dental condition among children in nine countries participating in an international oral health promotion program, 2012–2013. Int. Dent. J. 2014, 64, 27–34. [Google Scholar] [CrossRef]
- Branco, V.I.S. Cárie Dentária Infantil: Estudo de Prevalência de Cárie Dentária e Seus Determinantes Sociais, Numa Amostra de Crianças Entre os 6 e os 11 Anos de Idade, do Distrito de Coimbra; Dissertação Apresentada à Universidade de Coimbra para Cumprimento dos Requisitos Necessários à Obtenção do Grau de Mestre em Antropologia Médica; Universidade de Coimbra: Coimbra, Portugal, 2015. [Google Scholar]
- Bratthall, D. Introducing the Significant Caries Index together with a proposal for a new global oral health goal for 12-year-olds. Int. Dent. J. 2000, 50, 378–384. [Google Scholar] [CrossRef]
- Almerich-Silla, J.M. Montiel-Company JM. Influence of immigration and other factors on caries in 12- and 15-yr-old children. Eur. J. Oral Sci. 2007, 115, 378–383. [Google Scholar] [CrossRef]
- Llodra-Calvo, J.C. Encuesta de Salud Oral de España 2010. RCOE 2012, 17, 13–46. [Google Scholar]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.; Marcenes, W. Global burden of untreated caries: A systematic review and metaregression. J. Dent. Res. 2015, 94, 650–658. [Google Scholar] [CrossRef]
- Lemos, D.; Schaefer, A.L. El Programa de Odontología Social de la Universidad Federal de Santa Catarina (Brasil) en Castaño A. Odontología Social. Un Proyecto Iberoamericano para el Mundo; Huelva, Ed.; Diputación de Huelva: Huelva, Spain, 2017; pp. 433–444. [Google Scholar]
- Chukwumah, N.M. Prevalence and risk factors for periodontal diseases seen in children attending the University of Benin Teaching Hospital for dental treatment. Ann. Med. Health Sci. Res. 2017, 7, 325–330. [Google Scholar]
- Soroye, M.O.; Braimoh, O.B. Oral Health status of children in government and private secondary schools in Lagos State, Nigeria. Nig. J. Dent. Res. 2016, 1, 34–40. [Google Scholar]
- Ghaffari, M.; Rakhshanderou, S.; Ramezankhani, A.; Noroozi, M.; Armoon, B. Oral Health Education and Promotion Programmes: Meta-Analysis of 17-Year Intervention. Int. J. Dent. Hyg. 2018, 16, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Fraihat, N.; Madae’en, S.; Bencze, Z.; Herczeg, A.; Varga, O. Clinical Effectiveness and Cost-Effectiveness of Oral-Health Promotion in Dental Caries Prevention among Children: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 2668. [Google Scholar] [CrossRef]
| COUNTRY | n | % |
|---|---|---|
| Syria | 172 | 86.9 |
| Palestine | 6 | 3.0 |
| Morocco | 12 | 6.1 |
| Ivory Coast | 2 | 1.0 |
| Liberia | 2 | 1.0 |
| Algeria | 4 | 2.0 |
| SEX | ||
| Boys | 114 | 57.6 |
| Girls | 84 | 42.4 |
| AGE (YEARS) | ||
| 1–3 | 37 | 18.7 |
| 4–5 | 31 | 15.7 |
| 6–8 | 51 | 25.8 |
| 9–11 | 38 | 19.2 |
| 12–13 | 21 | 10.6 |
| 14–17 | 20 | 10.1 |
| TYPE OF DENTITION | ||
| Temporal | 68 | 34.3 |
| Mixed | 89 | 44.9 |
| Permanent | 41 | 20.7 |
| <6 Years (n = 68; 34.3%) | 6–11 Years (n = 89; 44.9%) | 12–17 Years (n = 41; 20.7%) | ||||
|---|---|---|---|---|---|---|
| Temporary Teeth | Mean | SD | Mean | SD | Mean | SD |
| decayed | 6.3 | 6.3 | 4.7 | 3.9 | 0.0 | 0.0 |
| filled | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| missing | 0.1 | 0.5 | 0.8 | 1.3 | 0.0 | 0.0 |
| dmft | 6.4 | 6.3 | 4.7 | 3.9 | 0.0 | 0.0 |
| Temporary-RI * % | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Permanent teeth | ||||||
| Decayed | 0.1 | 0.6 | 2.0 | 2.0 | 4.4 | 4.0 |
| Filled | 0.0 | 0.0 | 0.0 | 0.2 | 0.2 | 1.1 |
| Missing | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.3 |
| DMFT | 0.1 | 0.6 | 2.0 | 2.0 | 4.7 | 4.2 |
| Permanent-RI * % | 0.0 | 0.0 | 2.0 | 0 | 2.9 | 13.0 |
| RI *-Total % | 0.0 | 0.0 | 0.5 | 3.5 | 2.8 | 13.0 |
| SiC ** | 6.4 | 6.4 | 10.1 | 6.0 | 9.3 | 2.6 |
| <6 Years Temporal Dentition (n = 68; 34.3%) | 6–11 Years Mixed Dentition (n = 89; 44.9%) | 12–17 Years Permanent Dentition (n = 41; 20.7%) | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Fillings | 4.2 | 4.5 | 4.8 | 3.0 | 4.1 | 3.7 |
| Invasive Treatment | 2.3 | 4.5 | 1.8 | 3.0 | 0.3 | 0.9 |
| Space Mantainer | 0.0 | 0.1 | 0.3 | 1.0 | 0.0 | 0.0 |
| N | % | N | % | n | % | |
| Distribution of need of fillings | ||||||
| None | 24 | 35.3 | 10 | 11.2 | 11 | 26.8 |
| 1–2 fillings | 6 | 8.8 | 12 | 13.5 | 5 | 12.2 |
| 3 or more | 38 | 55.9 | 67 | 75.3 | 25 | 61.0 |
| Distribution of need for invasive treatment (endo or exodontics) | ||||||
| None | 42 | 61.8 | 38 | 42.7 | 34 | 82.9 |
| 1–2 treatments | 5 | 7.4 | 27 | 30.3 | 5 | 12.2 |
| 3 or more | 21 | 30.9 | 24 | 27.0 | 2 | 4.9 |
| Mean of Sextants and Value | Mean | SD |
|---|---|---|
| Number of sextants with CPI = 0 | 2.0 | 2.6 |
| Number of sextants with CPI = 1 | 3.9 | 2.5 |
| Number of sextants with CPI = 2 | 0.1 | 0.3 |
| Needs of periodontal treatment | n | % |
| None | 11 | 26.8 |
| Prophylaxis and Oral hygiene | 30 | 73.2 |
| <6 Years Temporal Dentition (n = 68; 34.3%) | 6–11 Years Mixed Dentition (n = 89; 44.9%) | 12–17 Years Permanent Dentition (n = 41; 20.7%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Needs of | Boys (n = 41) | Girls (n = 27) | Boys (n = 47) | Girls (n = 42) | Boys (n = 26) | Girls (n = 15) | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Fillings | 4.2 | 4.7 | 4.2 | 4.4 | 4.5 | 3.0 | 5.1 | 3.1 | 4.1 | 3.7 | 4.1 | 3.7 |
| Crowns | 0.1 | 0.3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total restorations | 4.3 | 4.7 | 4.2 | 4.4 | 4.5 | 3.0 | 5.2 | 3.1 | 4.1 | 3.7 | 4.1 | 3.7 |
| Invasive Treatments | 3.0 * | 4.7 | 1.2 * | 2.4 | 2.1 | 2.7 | 1.5 | 2.2 | 0.3 | 0.8 | 0.3 | 0.6 |
| Space Mantainers | 0.0 | 0.2 | 0.0 | 0.0 | 0.5 * | 1.3 | 0.1 * | 0.5 | 0.0 | 0.0 | 0.0 | 0.0 |
| Boys (n = 26) | Girls (n = 15) | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Healthy CPI = 0 | 2.2 | 2.5 | 1.7 | 2.7 |
| Bleeding gums CPI = 1 | 3.9 | 2.5 | 4.1 | 2.7 |
| Calculus CPI = 2 | 0.0 | 0.0 | 0.1 | 0.5 |
| Boys (n = 26) | Girls (n = 15) | |||
|---|---|---|---|---|
| Visits to the Dentist | n | % | n | % |
| No in last year | 5 | 71.4 | 2 | 28.6 |
| Sometimes in last year | 9 | 64.3 | 5 | 35.7 |
| Never | 12 | 60.0 | 8 | 40.0 |
| Toothbrushing | n | % | n | % |
| Rarely | 11 | 64.7 | 6 | 35.3 |
| Every week | 5 | 83.3 | 1 | 16.7 |
| Daily | 10 | 55.6 | 8 | 44.4 |
| <6 Years Temporal Dentition (n = 68; 34.3%) | 6–11 Years Mixed Dentition (n = 89; 44.9%) | 12–17 Years Permanent Dentition (n = 41; 20.7%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Needs of Fillings | Boys | Girls | Boys | Girls | Boys | Girls | ||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| None | 16 | 39.0 | 8 | 29.6 | 6 | 12.8 | 4 | 9.5 | 7 | 26.9 | 4 | 26.7 |
| 1–2 | 3 | 7.3 | 3 | 11.1 | 7 | 14.9 | 5 | 11.9 | 3 | 11.5 | 2 | 13.3 |
| 3 | 22 | 53.7 | 16 | 59.3 | 34 | 72.3 | 33 | 78.6 | 16 | 61.5 | 9 | 60.0 |
| Type of Malocclusion | Boys | Girls | Total | ||
|---|---|---|---|---|---|
| n | % | n | % | n | |
| None | 1 | 100.0 | 0 | 0.0 | 1 |
| Slight | 10 | 59.0 | 7 | 41.2 | 17 |
| Moderate | 14 | 67.0 | 7 | 33.3 | 21 |
| Severe | 1 | 50.0 | 1 | 50.0 | 2 |
| Total | 26 | 63.4 | 15 | 37.0 | 41 |
| Pain/discomfort | Boys | Girls | Total | ||
| n | % | n | % | n | |
| Never | 26 | 65.0 | 14 | 35.0 | 40 |
| Sometimes | 0 | 0.0 | 1 | 100.0 | 1 |
| Total | 26 | 63.4 | 15 | 36.6 | 41 |
| Problems at eating | Boys | Girls | Total | ||
| n | % | n | % | n | |
| Never | 26 | 65.0 | 14 | 35.0 | 40 |
| Hardly ever | 0 | 0.0 | 1 | 100.0 | 1 |
| Total | 26 | 63.4 | 15 | 36.6 | 41 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kizi, G.; Raquel Barata, A.; Ventura, I.; Flores-Fraile, J.; Ribas-Perez, D.; Castaño-Seiquer, A. Oral Health in migrants children in Melilla, Spain. Children 2023, 10, 888. https://doi.org/10.3390/children10050888
Kizi G, Raquel Barata A, Ventura I, Flores-Fraile J, Ribas-Perez D, Castaño-Seiquer A. Oral Health in migrants children in Melilla, Spain. Children. 2023; 10(5):888. https://doi.org/10.3390/children10050888
Chicago/Turabian StyleKizi, Gunel, Ana Raquel Barata, Irene Ventura, Javier Flores-Fraile, David Ribas-Perez, and Antonio Castaño-Seiquer. 2023. "Oral Health in migrants children in Melilla, Spain" Children 10, no. 5: 888. https://doi.org/10.3390/children10050888
APA StyleKizi, G., Raquel Barata, A., Ventura, I., Flores-Fraile, J., Ribas-Perez, D., & Castaño-Seiquer, A. (2023). Oral Health in migrants children in Melilla, Spain. Children, 10(5), 888. https://doi.org/10.3390/children10050888






