Echo-Endoscopy Combined with Virtual Reality: A Whole Perspective of Laparoscopic Common Bile Duct Exploration in Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Methods
2.2.1. Endoscopic Instrumentation
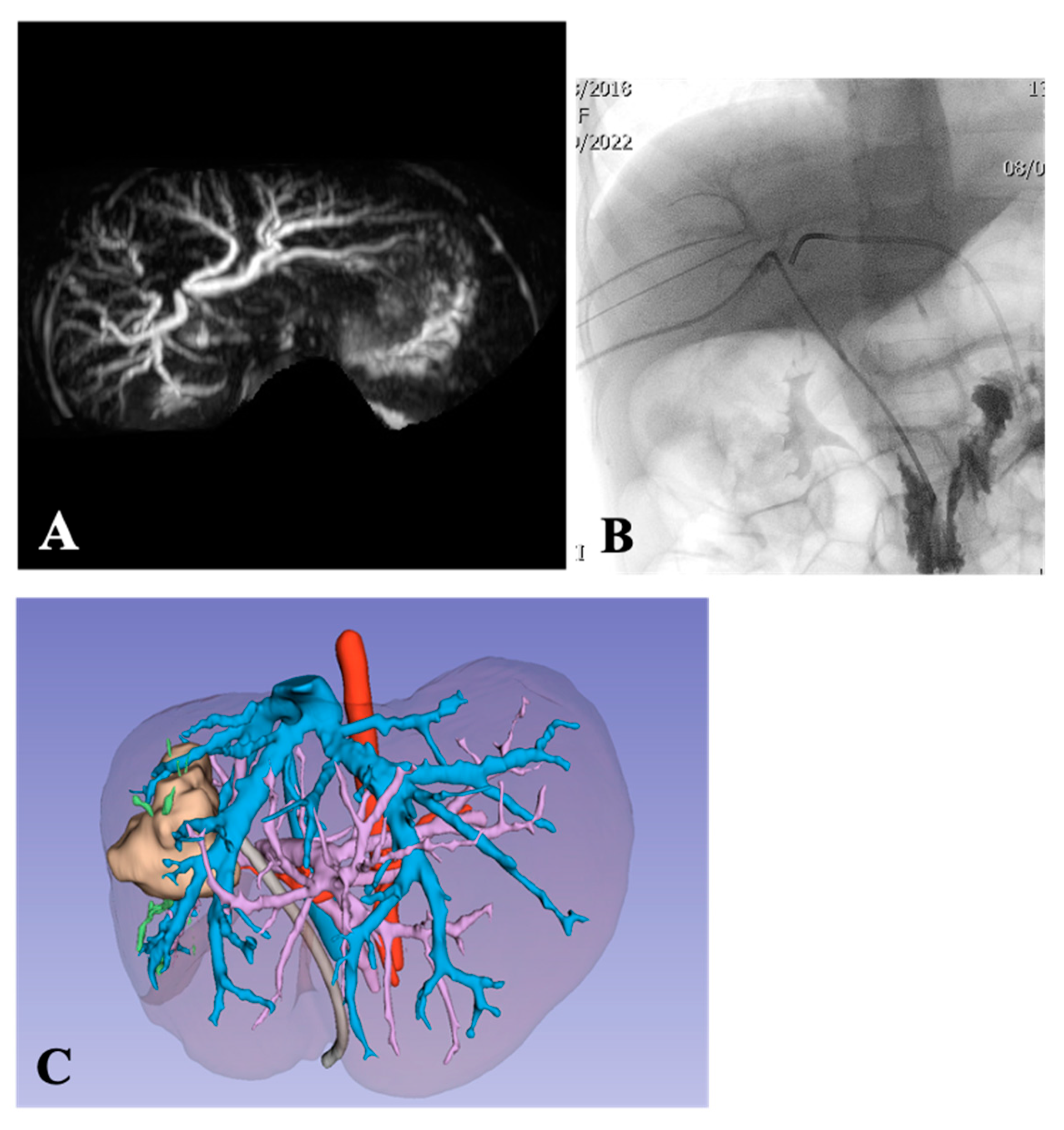
2.2.2. Three-Dimensional (3D) Models
2.2.3. Virtual Reality HMD Model
2.2.4. Preoperative Virtual Reality HMD Setup Evaluation
2.2.5. Surgical Approach
3. Results
3.1. Patients’ Data
3.2. Preoperative Planning and Operations
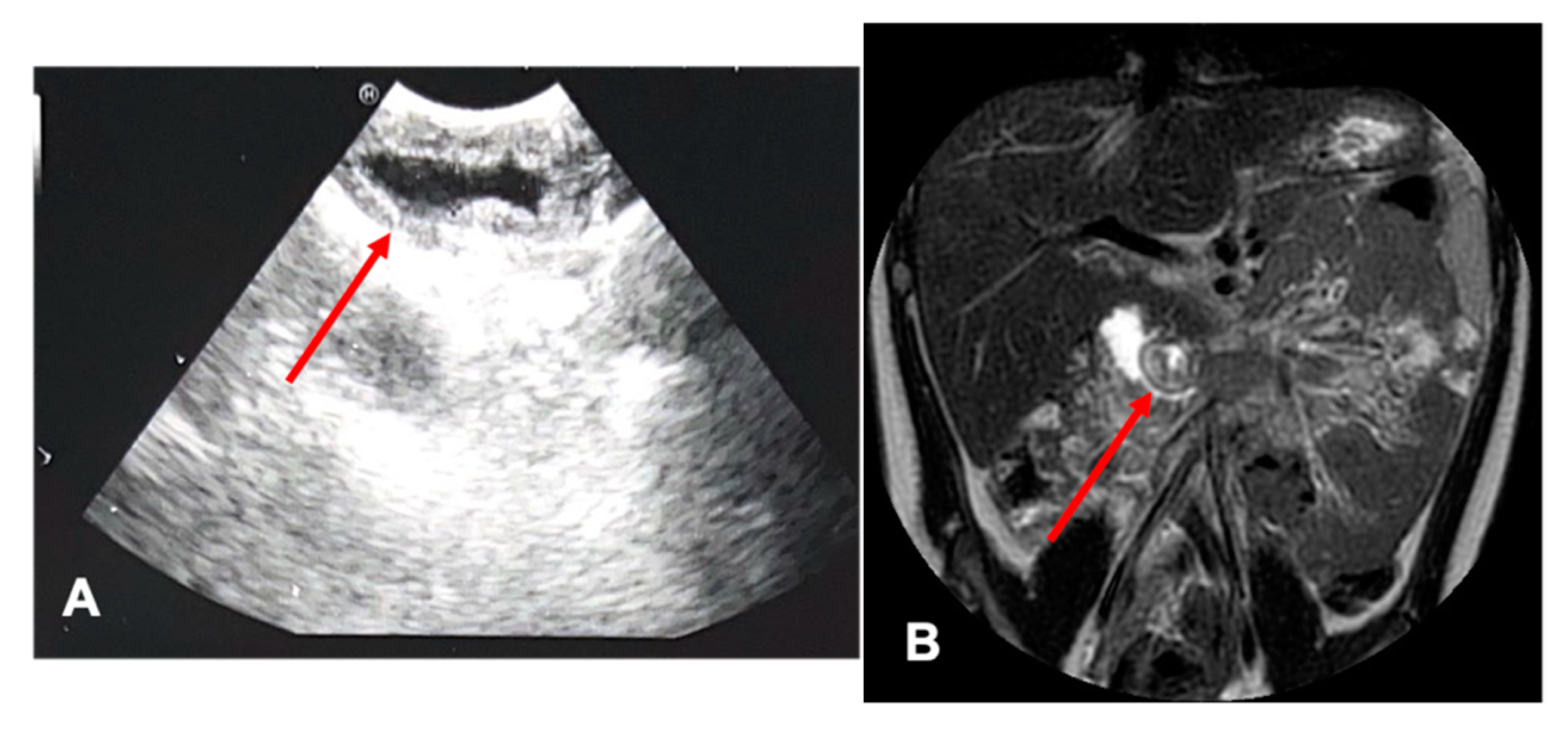
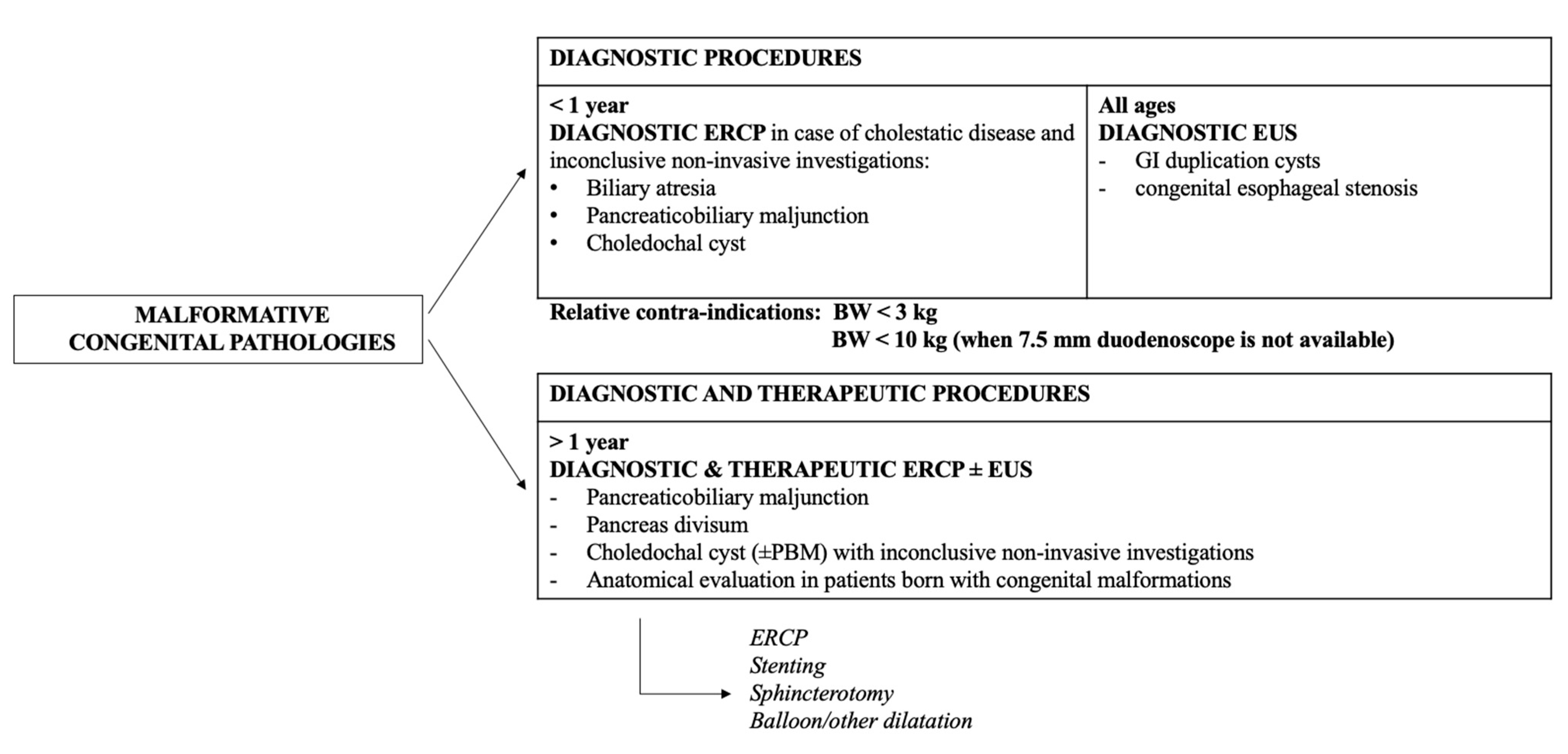
3.2.1. Congenital Malformations (Duplication Cysts)
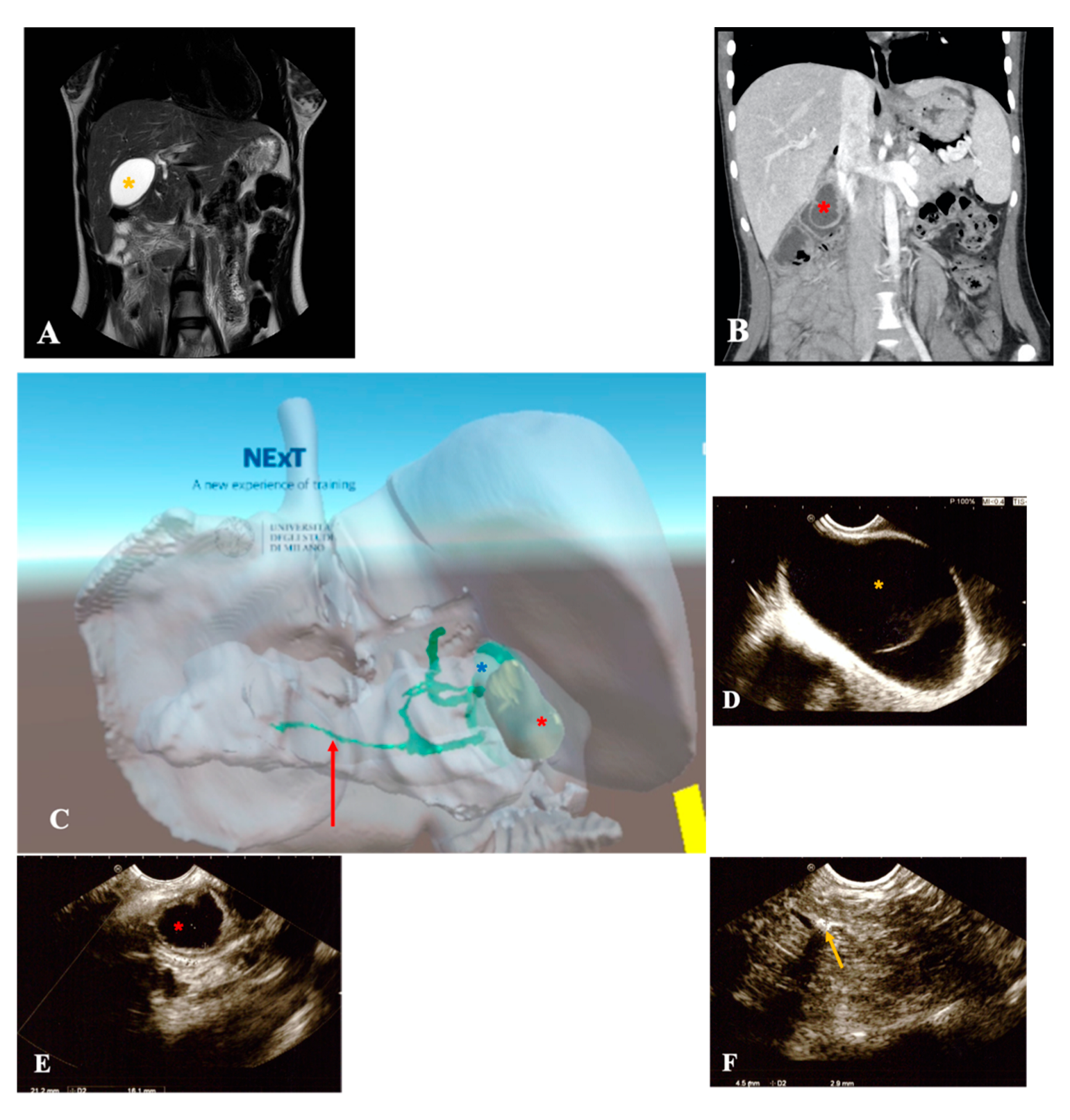
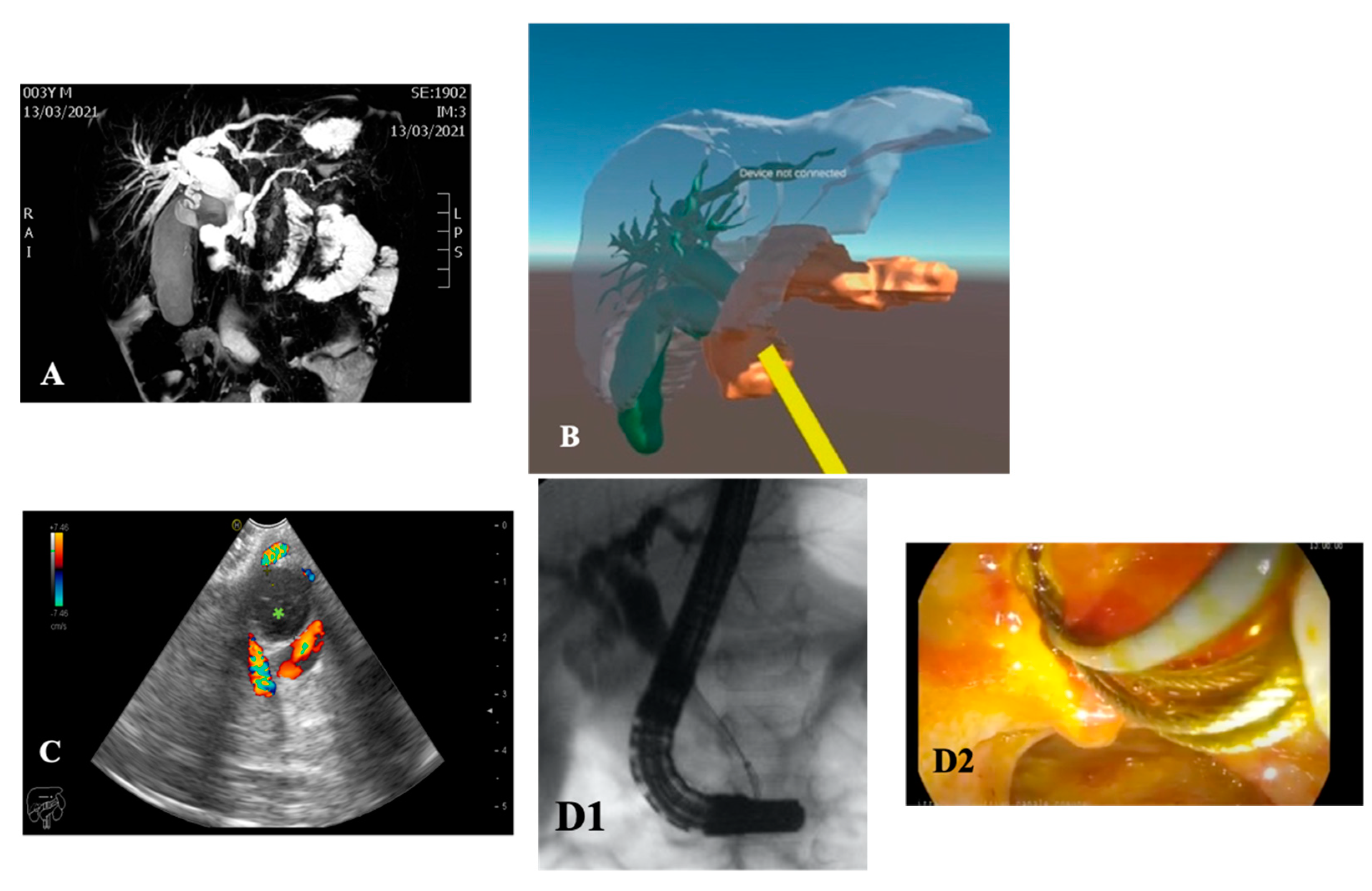
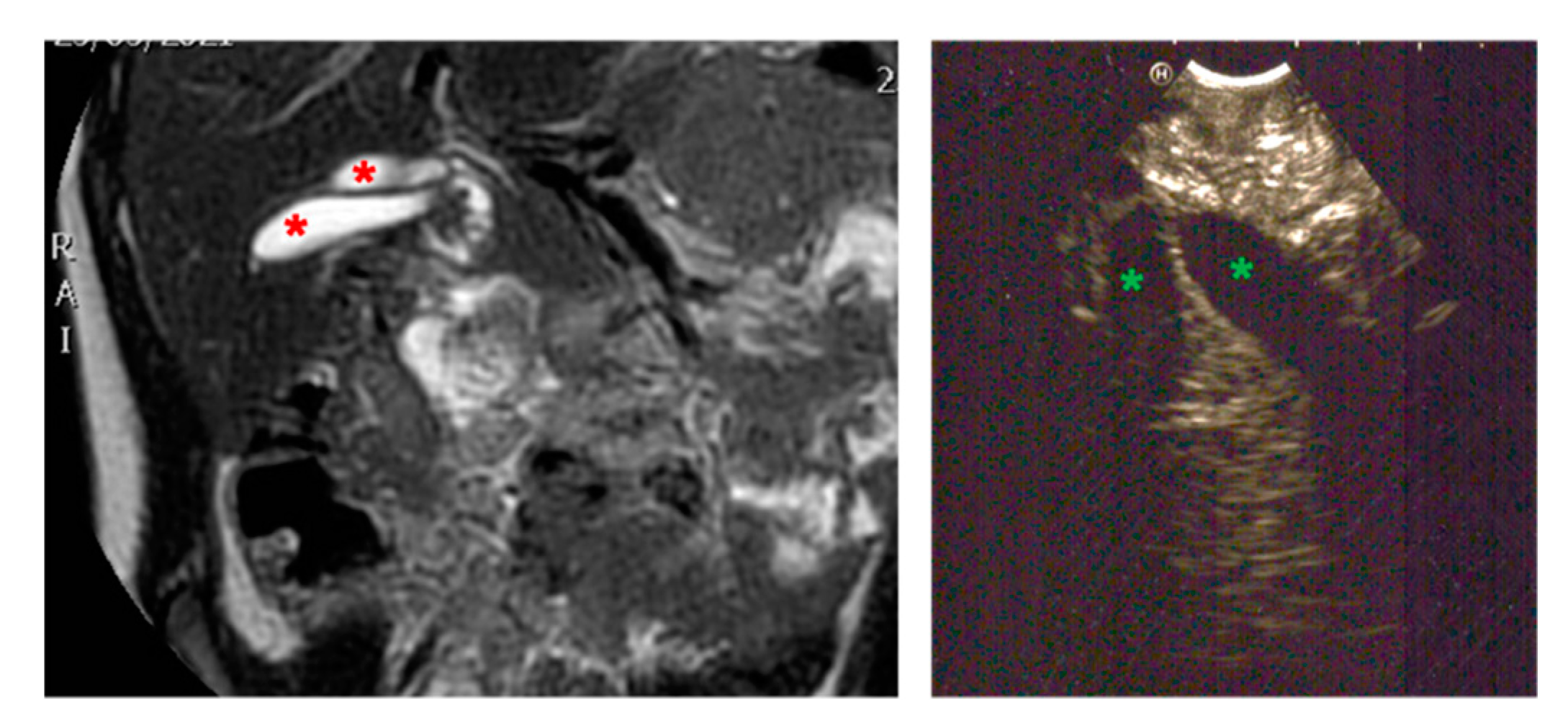
3.2.2. Biliary Tree Abnormalities
3.2.3. Proliferative Disorders
3.3. Post-Operative Management
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Isoldi, S.; Cucchiara, S.; Repici, A.; Lerner, D.G.; Thomson, M.; Oliva, S. Gastrointestinal endoscopy in children and adults: How do they differ? Dig. Liver Dis. 2021, 53, 697–705. [Google Scholar] [CrossRef] [PubMed]
- Nabi, Z.; Reddy, D.N. Advanced Therapeutic Gastrointestinal Endoscopy in Children—Today and Tomorrow. Clin. Endosc. 2018, 51, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Piester, T.L.; Liu, Q.Y. EUS in Pediatrics: A Multicenter Experience and Review. Front. Pediatr. 2021, 9, 709461. [Google Scholar] [CrossRef]
- Tringali, A.; Thomson, M.; Dumonceau, J.-M.; Tavares, M.; Tabbers, M.M.; Furlano, R.; Spaander, M.; Hassan, C.; Tzvinikos, C.; Ijsselstijn, H.; et al. Pediatric gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy (ESGE) and European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) Guideline Executive summary. Endoscopy 2017, 49, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Bosley, M.E.; Zamora, I.J.; Neff, L.P. Choledocholithiasis—A new clinical pathway. Transl. Gastroenterol. Hepatol. 2021, 6, 35. [Google Scholar] [CrossRef] [PubMed]
- Pogorelić, Z.; Lovrić, M.; Jukić, M.; Perko, Z. The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis. Children 2022, 9, 1583. [Google Scholar] [CrossRef]
- Cox, C.B.; Laborda, T.; Kynes, J.M.; Hiremath, G. Evolution in the Practice of Pediatric Endoscopy and Sedation. Front. Pediatr. 2021, 9, 687635. [Google Scholar] [CrossRef]
- Barth, B.A.; Banerjee, S.; Bhat, Y.M.; Desilets, D.J.; Gottlieb, K.T.; Maple, J.T.; Pfau, P.R.; Pleskow, D.K.; Siddiqui, U.D.; Tokar, J.L.; et al. Equipment for pediatric endoscopy. Gastrointest. Endosc. 2012, 76, 8–17. [Google Scholar] [CrossRef]
- ASGE Standards of Practice Committee; Lightdale, J.R.; Acosta, R.; Baron, T.H.; Banerjee, S.; Cash, B.D.; Dominitz, J.A.; Gan, S.-I.; Harrison, M.E.; Ikenberry, S.O.; et al. Modifications in endoscopic practice for pediatric patients. Gastrointest. Endosc. 2014, 79, 699–710. [Google Scholar] [CrossRef]
- Thomson, M.; Tringali, A.; Dumonceau, J.M.; Tavares, M.; Tabbers, M.M.; Furlano, R.; Spaander, M.; Hassan, C.; Tzvinikos, C.; Ijsselstijn, H.; et al. Paediatric gastrointestinal endoscopy: European society for paediatric gastro-enterology hepatology and nutrition and European society of gastrointestinal endoscopy guidelines. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 133–153. [Google Scholar] [CrossRef]
- Rodriguez, S.A.; Banerjee, S.; Desilets, D.; Diehl, D.L.; Farraye, F.A.; Kaul, V.; Kwon, R.S.; Mamula, P.; Pedrosa, M.C.; Varadarajulu, S. Ultrathin endoscopes. Gastrointest. Endosc. 2010, 71, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.-C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef]
- Vertemati, M.; Cassin, S.; Rizzetto, F.; Vanzulli, A.; Elli, M.; Sampogna, G.; Gallieni, M. A Virtual Reality Environment to Visualize Three-Dimensional Patient-Specific Models by a Mobile Head-Mounted Display. Surg. Innov. 2019, 26, 359–370. [Google Scholar] [CrossRef] [PubMed]
- Vertemati, M.; Rizzetto, F.; Vezzulli, F.; Vanzulli, A.; Rantas, S.; Aseni, P.; Cassin, S. A mirroring virtual reality environment using mobile head mounted display for visualization of patient-specific anatomy. In Proceedings of the 2019 Inventions and Innovations: Medicine 2040, Tel Aviv-Yafo, Israel, 4–5 November 2019. [Google Scholar]
- Peden, R.G.; Mercer, R.; Tatham, A.J. The use of head-mounted display eyeglasses for teaching surgical skills: A prospective randomised study. Int. J. Surg. 2016, 34, 169–173. [Google Scholar] [CrossRef]
- Lerner, D.G.; Pall, H. Setting up the Pediatric Endoscopy Unit. Gastrointest. Endosc. Clin. N. Am. 2016, 26, 1–12. [Google Scholar] [CrossRef]
- Hayat, J.O.; Sirohi, R.; Gorard, D.A. Paediatric endoscopy performed by adult-service gastroenterologists. Eur. J. Gastroenterol. Hepatol. 2008, 20, 648–652. [Google Scholar] [CrossRef] [PubMed]
- Early, D.S.; Ben-Menachem, T.; Decker, G.A.; Evans, J.A.; Fanelli, R.D.; Fisher, D.A.; Fukami, N.; Hwang, J.H.; Jain, R.; Jue, T.L.; et al. Appropriate use of GI endoscopy. Gastrointest. Endosc. 2012, 75, 1127–1131. [Google Scholar] [CrossRef] [PubMed]
- Keil, R.; Drábek, J.; Lochmannová, J.; Šťovíček, J.; Koptová, P.; Wasserbauer, M.; Frýbová, B.; Šnajdauf, J.; Matouš, J.; Kotalová, R.; et al. ERCP in infants, children, and adolescents—Different roles of the methods in different age groups. PLoS ONE 2019, 14, e0210805. [Google Scholar] [CrossRef]
- Tagawa, M.; Morita, A.; Imagawa, K.; Mizokami, Y. Endoscopic retrograde cholangiopancreatography and endoscopic ultrasound in children. Dig. Endosc. 2021, 33, 1045–1058. [Google Scholar] [CrossRef]
- Liu, Q.Y.; Gugig, R.; Troendle, D.M.; Bitton, S.; Patel, N.; Vitale, D.; Abu-El-Haija, M.; Husain, S.Z.; Morinville, V.D. The Roles of Endoscopic Ultrasound and Endoscopic Retrograde Cholangiopancreatography in the Evaluation and Treatment of Chronic Pancreatitis in Children: A Position Paper from the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition Pancreas Committee. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 681–693. [Google Scholar] [CrossRef]
- Saito, T.; Terui, K.; Mitsunaga, T.; Nakata, M.; Kuriyama, Y.; Higashimoto, Y.; Kouchi, K.; Onuma, N.; Takahashi, H.; Yoshida, H. Role of Pediatric Endoscopic Retrograde Cholangiopancreatography in an Era Stressing Less-Invasive Imaging Modalities. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 204–209. [Google Scholar] [CrossRef]
- Negm, A.A.; Petersen, C.; Markowski, A.; Luettig, B.; Ringe, K.I.; Lankisch, T.O.; Manns, M.P.; Ure, B.; Schneider, A.S. The Role of Endoscopic Retrograde Cholangiopancreatography in the Diagnosis of Biliary Atresia: 14 Years’ Experience. Eur. J. Pediatr. Surg. 2018, 28, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Felux, J.; Sturm, E.; Busch, A.; Zerabruck, E.; Graepler, F.; Stüker, D.; Manger, A.; Kirschner, H.-J.; Blumenstock, G.; Malek, N.P.; et al. ERCP in infants, children and adolescents is feasible and safe: Results from a tertiary care center. United Eur. Gastroenterol. J. 2017, 5, 1024–1029. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.; Cohen, R.Z.; Mekaroonkamol, P.; Taylor, A.; Freeman, A.J.; Fritzen, C.; Sauer, C.; Chawla, S.; Keilin, S.; Cai, Q.; et al. Retrospective Multicenter Matched Controlled Comparison of Endoscopic Retrograde Cholangiopancreatography in Pediatric Patients: A 10-year Experience. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 568–573. [Google Scholar] [CrossRef]
- Cho, J.M.; Jeong, I.S.; Kim, H.J.; Oh, S.H.; Kim, K.M. Early adverse events and long-term outcomes of endoscopic sphincterotomy in a pediatric population: A single-center experience. Endoscopy 2017, 49, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Wandling, M.W.; Hungness, E.S.; Pavey, E.S.; Stulberg, J.J.; Schwab, B.; Yang, A.D.; Shapiro, M.B.; Bilimoria, K.Y.; Ko, C.Y.; Nathens, A.B. Nationwide Assessment of Trends in Choledocholithiasis Management in the United States from 1998 to 2013. JAMA Surg. 2016, 151, 1125–1130. [Google Scholar] [CrossRef] [PubMed]
- Doud, A.; Bond, L.; Downard, C.; Vitale, G.; Fallat, M.; Foley, D.; Wright, T.; Bond, S. Management of complicated biliary disease in the pediatric population. Surgery 2022, 171, 736–740. [Google Scholar] [CrossRef] [PubMed]
- Guda, N.M.; Reddy, D.N.; Kumar, A. Complications of ERCP. Indian J. Gastroenterol. 2013, 33, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lorio, E.; Moreau, C.; Michalek, J.E.; Patel, S. Expanding the Use of Endoscopic Retrograde Cholangiopancreatography in Pediatrics: A National Database Analysis of Demographics and Complication Rates. Gastroenterol. Res. 2022, 15, 314–324. [Google Scholar] [CrossRef]
- Troendle, D.M.; Ruan, W.; Fishman, D.S.; Barth, B.A.; Liu, Q.Y.; Giefer, M.; Kim, K.M.; Martinez, M.; Dall’oglio, L.; Torroni, F.; et al. Technical Outcomes in Pediatric Endoscopic Retrograde Cholangiopancreatography: Data from an International Collaborative. J. Pediatr. Gastroenterol. Nutr. 2022, 75, 755–760. [Google Scholar] [CrossRef]
- Lyu, Y.; Cheng, Y.; Li, T.; Cheng, B.; Jin, X. Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: A meta-analysis. Surg. Endosc. 2018, 33, 3275–3286. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Mirzaie, S.; Dunnsiri, T.; Chen, F.; Wilhalme, H.; MacQueen, I.T.; Cryer, H.; Eastoak-Siletz, A.; Guan, M.; Cuff, C.; et al. Systematic review and meta-analysis of the 2010 ASGE non-invasive predictors of choledocholithiasis and comparison to the 2019 ASGE predictors. Clin. J. Gastroenterol. 2022, 15, 286–300. [Google Scholar] [CrossRef] [PubMed]
- Asenov, Y.; Akin, M.; Cantez, S.; Soysal, F.G.; Tekant, Y.; Akın, M. Endoscopic retrograde cholangiopancreatography in children: Retrospective series with a long-term follow-up and literature review. Turk. J. Gastroenterol. 2019, 30, 192–197. [Google Scholar] [CrossRef]
- Keane, M.G.; Kumar, M.; Cieplik, N.; Thorburn, D.; Johnson, G.J.; Webster, G.J.; Chapman, M.H.; Lindley, K.J.; Pereira, S.P. Paediatric pancreaticobiliary endoscopy: A 21-year experience from a tertiary hepatobiliary centre and systematic literature review. BMC Pediatr. 2018, 18, 42. [Google Scholar] [CrossRef] [PubMed]
- Capparelli, M.A.; D’alessandro, P.D.; Questa, H.A.; Ayarzabal, V.H.; Bailez, M.M.; Barrenechea, M.E. Development of a risk score for choledocholithiasis in pediatric patients. Pediatr. Surg. Int. 2021, 37, 1393–1399. [Google Scholar] [CrossRef]
- Frybova, B.; Drabek, J.; Lochmannova, J.; Douda, L.; Hlava, S.; Zemkova, D.; Mixa, V.; Kyncl, M.; Zeman, L.; Rygl, M.; et al. Cholelithiasis and choledocholithiasis in children; risk factors for development. PLoS ONE 2018, 13, e0196475. [Google Scholar] [CrossRef] [PubMed]
- Fishman, D.S.; Chumpitazi, B.P.; Raijman, I.; Tsai, C.M.-W.; Smith, E.O.; Mazziotti, M.V.; Gilger, M.A. Endoscopic retrograde cholangiography for pediatric choledocholithiasis: Assessing the need for endoscopic intervention. World J. Gastrointest. Endosc. 2016, 8, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Pierce, R.A.; Jonnalagadda, S.; Spitler, J.A.; Tessier, D.J.; Liaw, J.M.; Lall, S.C.; Melman, L.M.; Frisella, M.M.; Todt, L.M.; Brunt, L.M.; et al. Incidence of residual choledocholithiasis detected by intraoperative cholangiography at the time of laparoscopic cholecystectomy in patients having undergone preoperative ERCP. Surg. Endosc. 2008, 22, 2365–2372. [Google Scholar] [CrossRef]
- Usatin, D.; Fernandes, M.; Allen, I.E.; Perito, E.R.; Ostroff, J.; Heyman, M.B. Complications of Endoscopic Retrograde Cholangiopancreatography in Pediatric Patients; A Systematic Literature Review and Meta-Analysis. J. Pediatr. 2016, 179, 160–165.e3. [Google Scholar] [CrossRef]
- Lightdale, C.J. Endoscopic Operations: Delivering a Powerful Method with Efficiency and Quality. Gastrointest. Endosc. Clin. N. Am. 2021, 31, xiii–xiv. [Google Scholar] [CrossRef]
- Lightdale, J.R.; Thomson, M.A.; Walsh, C.M. The Pediatric Endoscopy Quality Improvement Network Joint NASPGHAN/ESPGHAN Guidelines: A Global Path to Quality for Pediatric Endoscopy. J. Pediatr. Gastroenterol. Nutr. 2021, 74 (Suppl. 1), S1–S2. [Google Scholar] [CrossRef] [PubMed]
- Pall, H.; Lerner, D.; Khlevner, J.; Reynolds, C.; Kurowski, J.; Troendle, D.; Utterson, E.; Evans, P.M.; Brill, H.; Wilsey, M.; et al. Developing the Pediatric Gastrointestinal Endoscopy Unit: A Clinical Report by the Endoscopy and Procedures Committee. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 295–306. [Google Scholar] [CrossRef] [PubMed]

| Congenital Malformations (Duplication Cysts) | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Patients age, weight | Female 24 months 12 kg | Female 10 months 10 kg | Female 180 months 59 kg | |
| Symptoms | No | No | No | |
| Diagnosis (prenatal evaluation yes/no) | Multiple gastric duplication Cyst (yes) | Esophageal duplication cyst (yes) | Duodenal duplication cyst | |
| Radiological investigations | MR, US, EUS, X-ray | US, MR, CT-scan, barium swallow | US, MRI | |
| Endoscopic instrumentation | EBUS | EBUS | EG-3870UTK Linear-Array Ultrasound Gastroscope | |
| Management | MIS (laparoscopic resection of gastric duplication cysts) | MIS (thoracoscopic resection of esophageal duplication cyst) | Planned endoscopic removal by unroofing and mucosectomy | |
| Endoscopic Advantages/Limitations | Reduction in the diagnostic possibilities by identification of cysts surrounded by gastrointestinal wall layers | Definition of the relationships with surrounding tissues | Anatomical definition of surrounding structures (in particular, the biliary tree and pancreatic duct) | |
| Biliary Tree Abnormalities Malformative/Congenital | ||||
| 4 | 5 | 6 | 7 | |
| Patients age, weight | Female 192 months 60 kg | Male 55 months 14 kg | Male 120 months 27 kg | Male 8 months 9 kg |
| Symptoms | Acute pancreatitis, pain in right hypochondrium | Icterus, pancreatitis | Chronic pancreatitis with choletithiasis, genetic-based | No |
| Diagnosis (prenatal evaluation yes/no) | Cholelithiasis and choledocholithiasis in duodenal atresia (duodeno-jejuno anastomosis at birth) and pancreas divisum (yes) | Choledochal cyst (Todani I) and choledocholitiasis (no) | Mutation of the gene PRSS1, Cholelitiasis, pancreatic duct duplication (no) | Gallbladder duplication Annular pancreas Duodenal duplication (yes) |
| Radiological investigations | US, MR, CT Scan, VR HMD | US, Cholangio MR | US, X-ray, Cholangio MR, CT, VR HMD | US, Cholangio MR, CT |
| Endoscopic instrumentation | EG-3870UTK Linear-Array Ultrasound Gastroscope | EBUS + Duodenoscope | Duodenoscope, EG-3870UTK Linear-Array Ultrasound Gastroscope | EBUS |
| Management | MIS (laparoscopic cholecisectomy) with LCBDE | 1. ERCP + sphincterotomy + stone removal 2. Open surgery: choledochal cyst removal and Roux-en-Y bilio-digestive anastomosis | 1. EUS + ERCP + stent placement + sphincterotomy + DASE; MIS (laparoscopic cholecystectomy) with LCBDE 2. ERCP and pancreatic stent replacement | MIS (laparoscopic cholecystectomies) with attempted LCBDE (failure for fibrosis) |
| Endoscopic Advantages/Limitations | Anatomical definition ERCP technically impossible for difficulties in reaching the papilla | Diagnostic and therapeutic procedures | Effective biliopancreatic drainage permitted postponed cholecystectomy and pancreatic preservation | Anatomical definition |
| Biliary Tree Abnormalities Idiophatic Lithiasis | ||||
| 8 | 9 | 10 | ||
| Patients age, weight | Male 192 months 80 kg | Female 144 months 58 kg | Male 20 days 3.5 kg | |
| Symptoms | Acute pancreatitis | Abdominal pain | Cholestatic icterus | |
| Diagnosis (prenatal evaluation yes/no) | Cholelitiasis (no) | Cholelitiasis (no) | Non-syndromic paucity of interlobular bile ducts (no) | |
| Radiological investigations | US, cholangio-MR, CT Scan | US, cholangio-MRI | US | |
| Endoscopic instrumentation | EG-3870UTK Linear-Array Ultrasound Gastroscope | N/A | ||
| Management | MIS (laparoscopic cholecystectomy) with LCBDE | MIS (laparoscopic cholecystectomy) with LCBDE | Anterograde cholangiography, hepatic biopsy | |
| Endoscopic Advantages/Limitations | Size limitations; impossibility to perform ERCP | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Destro, F.; Salerno, R.; Calcaterra, V.; Ardizzone, S.; Meroni, M.; Roveri, M.; Pierucci, U.M.; Zaja, A.; Rizzetto, F.; Campari, A.; et al. Echo-Endoscopy Combined with Virtual Reality: A Whole Perspective of Laparoscopic Common Bile Duct Exploration in Children. Children 2023, 10, 760. https://doi.org/10.3390/children10040760
Destro F, Salerno R, Calcaterra V, Ardizzone S, Meroni M, Roveri M, Pierucci UM, Zaja A, Rizzetto F, Campari A, et al. Echo-Endoscopy Combined with Virtual Reality: A Whole Perspective of Laparoscopic Common Bile Duct Exploration in Children. Children. 2023; 10(4):760. https://doi.org/10.3390/children10040760
Chicago/Turabian StyleDestro, Francesca, Raffaele Salerno, Valeria Calcaterra, Sandro Ardizzone, Milena Meroni, Margherita Roveri, Ugo Maria Pierucci, Alberta Zaja, Francesco Rizzetto, Alessandro Campari, and et al. 2023. "Echo-Endoscopy Combined with Virtual Reality: A Whole Perspective of Laparoscopic Common Bile Duct Exploration in Children" Children 10, no. 4: 760. https://doi.org/10.3390/children10040760
APA StyleDestro, F., Salerno, R., Calcaterra, V., Ardizzone, S., Meroni, M., Roveri, M., Pierucci, U. M., Zaja, A., Rizzetto, F., Campari, A., Vertemati, M., Milani, P., & Pelizzo, G. (2023). Echo-Endoscopy Combined with Virtual Reality: A Whole Perspective of Laparoscopic Common Bile Duct Exploration in Children. Children, 10(4), 760. https://doi.org/10.3390/children10040760







