Suicidality Prevalence in a Pediatric Psychiatric Clinic: Relation to Social and Environmental Risk Factors
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. Ethical Approach
2.4. Patients
2.5. Suicidality
2.6. Recorded Psychometric Scales
2.7. Associated Predictors
2.8. Statistical Analysis
3. Results
3.1. Patients
3.2. Social and Family Characteristics
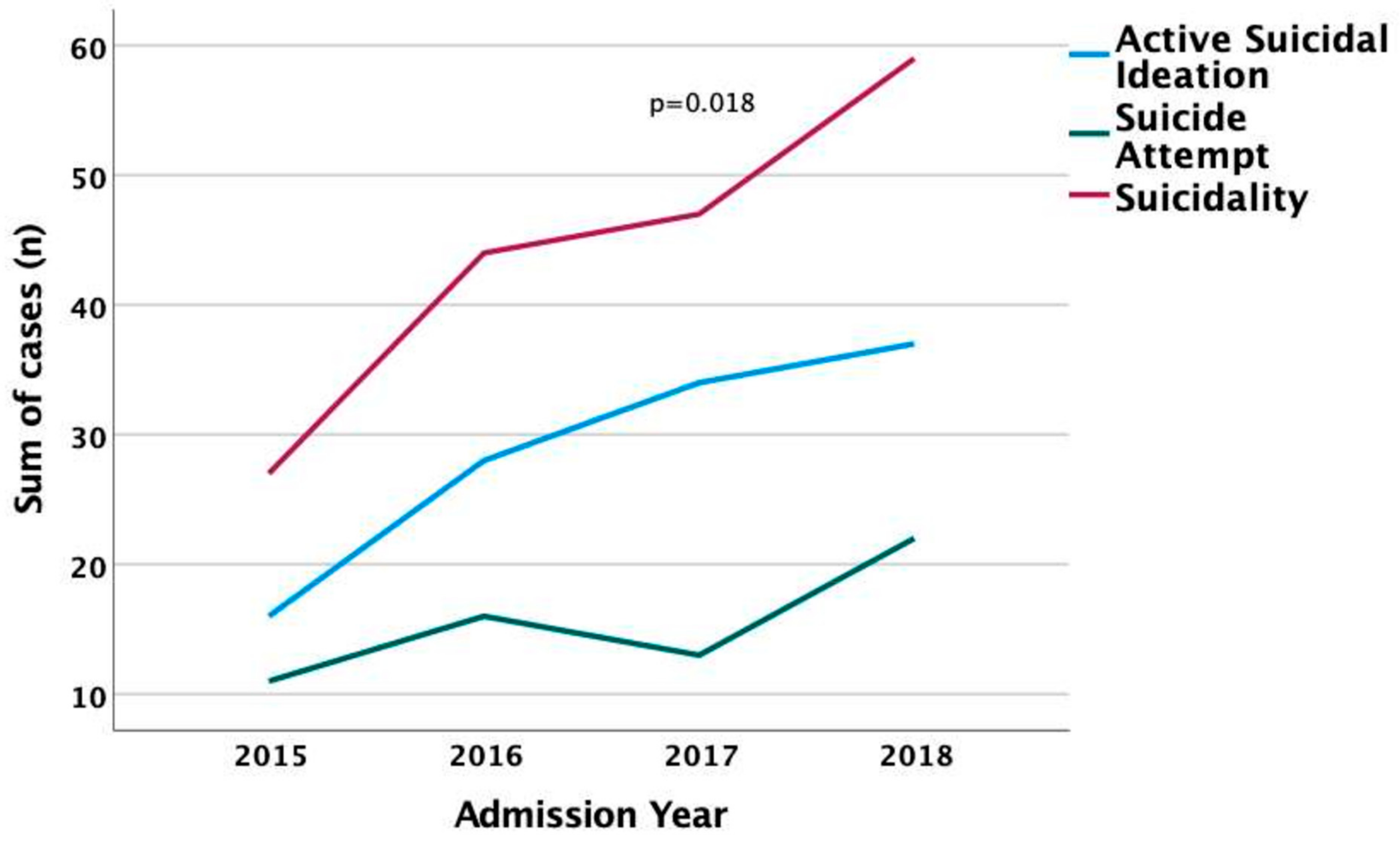
3.3. Suicidality
3.4. Risk Factors Associated with Suicidality
3.5. Suicide Attempt
3.6. Risk Factors for Suicide Attempts
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Suicidality: Risk Factors and What You Can Do|Thriveworks. Available online: https://thriveworks.com/help-with/suicide/suicidality/ (accessed on 8 March 2023).
- Suicidality—Anderson University. Available online: https://anderson.edu/student-life/counseling/suicidality/ (accessed on 8 March 2023).
- Di Lorenzo, R.; Cimino, N.; Di Pietro, E.; Pollutri, G.; Neviani, V.; Ferri, P. A 5-Year Retrospective Study of Demographic, Anamnestic, and Clinical Factors Related to Psychiatric Hospitalizations of Adolescent Patients. Neuropsychiatr. Dis. Treat. 2016, 12, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Taillieu, T.L.; Sareen, J.; Afifi, T.O. Associations among Child Abuse History, Deployment-Related Traumatic Events, Mental Disorders, and Suicidal Behaviors in Canadian Regular Force Personnel. J. Trauma. Stress 2022, 35, 1060–1071. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhan, N.; Zou, J.; Xie, D.; Liu, M.; Geng, F. The Transmission of Psychological Distress and Lifestyles from Parents to Children during COVID-19. J. Affect. Disord. 2022, 303, 74–81. [Google Scholar] [CrossRef]
- Bolt, J.; Patel, F.; Stone, L.; Pandian, D.; Manuel, M.M.; Gaines, N. Impact of COVID-19 on Pediatric Mental and Behavioral Health Visits to the Emergency Department. Pediatr. Emerg. Care 2022, 38, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Borschmann, R.; Stark, P.; Prakash, C.; Sawyer, S.M. Risk Profile of Young People Admitted to Hospital for Suicidal Behaviour in Melbourne, Australia. J. Paediatr. Child Health 2018, 54, 1213–1220. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and Mental Health: A Review of the Existing Literature. Asian J. Psychiatr. 2020, 52, 102066. [Google Scholar] [CrossRef]
- Shi, L.; Que, J.Y.; Lu, Z.A.; Gong, Y.M.; Liu, L.; Wang, Y.H.; Ran, M.S.; Ravindran, N.; Ravindran, A.V.; Fazel, S.; et al. Prevalence and Correlates of Suicidal Ideation among the General Population in China during the COVID-19 Pandemic. Eur. Psychiatry 2021, 64, e18. [Google Scholar] [CrossRef]
- Petruzzelli, M.G.; Furente, F.; Colacicco, G.; Annecchini, F.; Margari, A.; Gabellone, A.; Margari, L.; Matera, E. Implication of COVID-19 Pandemic on Adolescent Mental Health: An Analysis of the Psychiatric Counseling from the Emergency Room of an Italian University Hospital in the Years 2019–2021. J. Clin. Med. 2022, 11, 6177. [Google Scholar] [CrossRef]
- Van Hove, L.; Baetens, I.; Van Leeuwen, K.; Roelants, M.; Roeljan Wiersema, J.; Lewis, S.P.; Heath, N. Passive Suicidal Ideation in Childhood. Crisis 2021. online ahead of print. [Google Scholar] [CrossRef]
- DeVille, D.C.; Whalen, D.; Breslin, F.J.; Morris, A.S.; Khalsa, S.S.; Paulus, M.P.; Barch, D.M. Prevalence and Family-Related Factors Associated with Suicidal Ideation, Suicide Attempts, and Self-Injury in Children Aged 9 to 10 Years. JAMA Netw. Open 2020, 3, e1920956. [Google Scholar] [CrossRef]
- Newton, A.S.; Prisnie, K.; Macdonald, L.A.; Eltorki, M.; Finkelstein, Y.; Fitzpatrick, E.; Gagnon, I.; Greenfield, B.; Joubert, G.I.; Katz, L.Y.; et al. An Innovative Model of Pediatric Emergency Department Mental Health Care: Protocol for a Multicenter Type 1 Effectiveness-Implementation Cluster Randomized Trial. J. Am. Acad. Child Adolesc. Psychiatry 2022, 61, 946–948. [Google Scholar] [CrossRef] [PubMed]
- Gatta, M.; Raffagnato, A.; Iannattone, S.; Mistrorigo, C.; Fasolato, R.; Traverso, A.; Zanato, S.; Miscioscia, M. Hospitalisation in Child Neuropsychiatry: A Case Study Along a Five-Year Epidemiological-Clinical Trend. Clin. Neuropsychiatry 2022, 19, 72–83. [Google Scholar] [CrossRef] [PubMed]
- Economou, M.; Madianos, M.; Peppou, L.E.; Theleritis, C.; Patelakis, A.; Stefanis, C. Suicidal Ideation and Reported Suicide Attempts in Greece during the Economic Crisis. World Psychiatry 2013, 12, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Rachiotis, G.; Stuckler, D.; McKee, M.; Hadjichristodoulou, C. What Has Happened to Suicides during the Greek Economic Crisis? Findings from an Ecological Study of Suicides and Their Determinants (2003–2012). BMJ Open 2015, 5, e007295. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Holmberg, E.B.; Photos, V.I.; Michel, B.D. Self-Injurious Thoughts and Behaviors Interview: Development, Reliability, and Validity in an Adolescent Sample. Psychol. Assess. 2007, 19, 309–317. [Google Scholar] [CrossRef]
- Kokkevi, A.; Richardson, C.; Olszewski, D.; Matias, J.; Monshouwer, K.; Bjarnason, T. Multiple Substance Use and Self-Reported Suicide Attempts by Adolescents in 16 European Countries. Eur. Child Adolesc. Psychiatry 2012, 21, 443–450. [Google Scholar] [CrossRef]
- Kokkevi, A.; Rotsika, V.; Arapaki, A.; Richardson, C. Increasing Self-Reported Suicide Attempts by Adolescents in Greece between 1984 and 2007. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 231–237. [Google Scholar] [CrossRef]
- Yellowlees, P.M.; Marks, S. Problematic Internet Use or Internet Addiction? Comput. Hum. Behav. 2007, 23, 1447–1453. [Google Scholar] [CrossRef]
- Furman, W.; Buhrmester, D. The Network of Relationships Inventory: Behavioral Systems Version. Int. J. Behav. Dev. 2009, 33, 470–478. [Google Scholar] [CrossRef]
- Jetté, N.; Quan, H.; Hemmelgarn, B.; Drosler, S.; Maass, C.; Moskal, L.; Paoin, W.; Sundararajan, V.; Gao, S.; Jakob, R.; et al. The Development, Evolution, and Modifications of ICD-10: Challenges to the International Comparability of Morbidity Data. Med. Care 2010, 48, 1105–1110. [Google Scholar] [CrossRef]
- Dickstein, S. Family Routines and Rituals--the Importance of Family Functioning: Comment on the Special Section. J. Fam. Psychol. 2002, 16, 441–444. [Google Scholar] [CrossRef]
- Formoso, D.; Gonzales, N.A.; Aiken, L.S. Family Conflict and Children’s Internalizing and Externalizing Behavior: Protective Factors. Am. J. Community Psychol. 2000, 28, 175–199. [Google Scholar] [CrossRef] [PubMed]
- Abu-Rayya, H.M.; Yang, B. Unhealthy Family Functioning as a Psychological Context Underlying Australian Children’s Emotional and Behavioural Problems. Internet J. Ment. Health 2012, 1, 1–8. [Google Scholar]
- Guberman, C.; Manassis, K. Symptomatology and Family Functioning in Children and Adolescents with Comorbid Anxiety and Depression. J. Can. Acad. Child Adolesc. Psychiatry 2011, 20, 186–195. [Google Scholar]
- Biel, M.G. Parental Psychiatric Symptoms and Children’s Outcomes: Toward Understanding and Responding to Intergenerational Risk in Child Psychiatry. J. Am. Acad. Child Adolesc. Psychiatry 2018, 57, 632–633. [Google Scholar] [CrossRef]
- Reupert, A.E.; Maybery, D.J.; Kowalenko, N.M. Children Whose Parents Have a Mental Illness: Prevalence, Need and Treatment. Med. J. Aust. 2013, 199, S7–S9. [Google Scholar] [CrossRef]
- van Santvoort, F.; Hosman, C.M.H.; Janssens, J.M.A.M.; van Doesum, K.T.M.; Reupert, A.; van Loon, L.M.A. The Impact of Various Parental Mental Disorders on Children’s Diagnoses: A Systematic Review. Clin. Child Fam. Psychol. Rev. 2015, 18, 281–299. [Google Scholar] [CrossRef]
- Rasic, D.; Hajek, T.; Alda, M.; Uher, R. Risk of Mental Illness in Offspring of Parents with Schizophrenia, Bipolar Disorder, and Major Depressive Disorder: A Meta-Analysis of Family High-Risk Studies. Schizophr. Bull. 2014, 40, 28–38. [Google Scholar] [CrossRef]
- Mitchell, R.H.; Ani, C.; Cyr, C.; Irvine, J.; Joffe, A.R.; Skinner, R.; Wong, S.; Stang, A.S.; Laffin, M.; Korczak, D.J. Near-Fatal Self-Harm Among Canadian Adolescents. Can. J. Psychiatry 2021, 67, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Boyer, L.; Henry, J.M.; Samuelian, J.C.; Belzeaux, R.; Auquier, P.; Lancon, C.; Da Fonseca, D. Mental Disorders among Children and Adolescents Admitted to a French Psychiatric Emergency Service. Emerg. Med. Int. 2013, 2013, 651530. [Google Scholar] [CrossRef]
- Hanssen-Bauer, K.; Heyerdahl, S.; Hatling, T.; Jensen, G.; Olstad, P.M.; Stangeland, T.; Tinderholt, T. Admissions to Acute Adolescent Psychiatric Units: A Prospective Study of Clinical Severity and Outcome. Int. J. Ment. Health Syst. 2011, 5, 1. [Google Scholar] [CrossRef]
- Curtin, S.C.; Warner, M.; Hedegaard, H. Increase in Suicide in the United States, 1999–2014. NCHS Data Brief. 2016, 241, 1–8. [Google Scholar]
- Junuzovic, M.; Lind, K.M.T.; Jakobsson, U. Child Suicides in Sweden, 2000–2018. Eur. J. Pediatr. 2022, 181, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-S.; Lim, D.; Paik, J.-W.; Choi, Y.Y.; Jeon, J.; Sung, H.K. Suicide Attempt-Related Emergency Department Visits among Adolescents: A Nationwide Population-Based Study in Korea, 2016–2019. BMC Psychiatry 2022, 22, 418. [Google Scholar] [CrossRef] [PubMed]
- Ciccotti, H.R.; Spiller, H.A.; Casavant, M.J.; Kistamgari, S.; Funk, A.R.; Smith, G.A. Pediatric Suspected Suicides and Nonfatal Suicide Attempts Reported to United States Poison Control Centers Before and During the COVID-19 Pandemic. J. Med. Toxicol. 2023. epub ahead of print. [Google Scholar] [CrossRef]
- Beautrais, A.L.; Joyce, P.R.; Mulder, R.T. Precipitating Factors and Life Events in Serious Suicide Attempts among Youths Aged 13 through 24 Years. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 1543–1551. [Google Scholar] [CrossRef] [PubMed]
- Flores, J.P.; Stuart, E.A.; Swartz, K.L.; Jallah, N.A.; Wilcox, H.C. Risk and Protective Factors Associated with Suicidal Thoughts and Behaviors Among Maryland Middle School Students. School Ment. Health 2022, 14, 1024–1043. [Google Scholar] [CrossRef]
- Arnon, S.; Klomek, A.B.; Visoki, E.; Moore, T.M.; Argabright, S.T.; DiDomenico, G.E.; Benton, T.D.; Barzilay, R. Association of Cyberbullying Experiences and Perpetration with Suicidality in Early Adolescence. JAMA Netw. Open 2022, 5, e2218746. [Google Scholar] [CrossRef]
- Sedgwick, R.; Epstein, S.; Dutta, R.; Ougrin, D. Social Media, Internet Use and Suicide Attempts in Adolescents. Curr. Opin. Psychiatry 2019, 32, 534–541. [Google Scholar] [CrossRef]
- Niederkrotenthaler, T.; Stack, S.; Till, B.; Sinyor, M.; Pirkis, J.; Garcia, D.; Rockett, I.R.H.; Tran, U.S. Association of Increased Youth Suicides in the United States with the Release of 13 Reasons Why. JAMA Psychiatry 2019, 76, 933–940. [Google Scholar] [CrossRef]
- Bachmann, S. Epidemiology of Suicide and the Psychiatric Perspective. Int. J. Environ. Res. Public Health 2018, 15, 1425. [Google Scholar] [CrossRef] [PubMed]
- Fang, M. School Poverty and the Risk of Attempted Suicide among Adolescents. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 955–967. [Google Scholar] [CrossRef] [PubMed]



| Admission Characteristics | Age Group (Years) | * p | |||
|---|---|---|---|---|---|
| Total | 5–10 | 11–14 | 15–18 | ||
| Admission | n (%) | ||||
| First Admission | 152 (61) | 3 (2) | 50 (32.9) | 99 (65.1) | 0.242 |
| Readmission | 97 (39) | 0 (0.0) | 27 (27.8) | 70 (72.2) | |
| Origin | |||||
| From the Emergency Department | 162 (65.1) | 2 (1.2) | 49 (30.3) | 111 (68.5) | 0.403 |
| Another Clinic | 49 (19.7) | 1 (2) | 17 (34.7) | 31 (63.3) | |
| From Other Hospital | 27 (10.8) | 0 (0.0) | 5 (18.5) | 22 (81.5) | |
| From Outpatient Institutions | 11 (4.4) | 0 (0.0) | 6 (54.5) | 5 (45.5) | |
| Intra-Hospital Transport | |||||
| Pediatric Intensive Care Unit | 5 (10.2) | 0 (0.0) | 3 (60) | 2 (40) | 0.003 |
| Department of Pediatrics | 23 (46.9) | 1 (4.3) | 14 (60.9) | 8 (34.8) | |
| Department of Internal Medicine | 12 (24.5) | 0 (0.0) | 0 (0.0) | 12 (100) | |
| Department of Acute Psychiatry | 9 (18.4) | 0 (0.0) | 0 (0.0) | 9 (100) | |
| Admission Modality | |||||
| Voluntary | 205 (82.6) | 3 (1.5) | 67 (32.7) | 135 (65.9) | 0.322 |
| Public Prosecution Order | 44 (17.3) | 0 (0.0) | 11 (23.3) | 33 (76.7) | |
| Reason for Hospitalization | |||||
| Suicide Attempt | 62 (24.9) | 0 (0.0) | 22 (35.5) | 40 (64.5) | 0.002 |
| Suicidal Behavior # | 72 (28.9) | 0 (0) | 21 (29.2) | 51 (70.8) | |
| Emotional Disorder | 33 (13.3) | 1 (3.0) | 8 (24.2) | 24 (72.7) | |
| Behavioral Disorder | 33 (13.3) | 2 (6.1) | 9 (27.3) | 22 (66.7) | |
| Eating Disorder | 8 (3.2) | 0 (0.0) | 8 (100) | 0 (0.0) | |
| Social Reason | 11 (4.4) | 0 (0.0) | 4 (36.4) | 7 (63.6) | |
| Psychosis | 30 (12.0) | 0 (0.0) | 5 (16.7) | 25 (83.3) | |
| Age Group (Years) | * p | ||||
|---|---|---|---|---|---|
| Total | 5–10 | 11–14 | 15–18 | ||
| (First admission data, n = 152) | n (%) | ||||
| Characteristics of patients | |||||
| Total number of patients | 152 (100) | 3 (2) | 50 (32.9) | 99 (65.1) | |
| Females/males | 107/45 (70.4/29.6) | 1/2 (0.9/4.4) | 37/13 (34.6/28.9) | 69/30 (64.5/66.7) | 0.331 |
| School abandonment | 30 (21.5) | 1 (3.3) | 7 (23.3) | 22 (73.3) | 0.156 |
| Family Environment | |||||
| Divorced parents | 37 (30.6) | 1 (2.7) | 15 (40.5) | 21 (56.8) | 0.938 |
| Psychiatric diseases of father or suspicion | 52 (35.1) | 1 (1.9) | 20 (38.5) | 31 (59.6) | 0.423 |
| Psychiatric diseases of mother or suspicion | 98 (65.0) | 1 (1) | 41 (41.8) | 56 (57.1) | 0.018 |
| Father’s addictions | 23 (15.5) | 0 (0.0) | 10 (43.5) | 13 (56.5) | 0.423 |
| Institutions (orphanages) | 22 (14.6) | 0 (0.0) | 6 (27.3) | 16 (72.7) | 0.314 |
| (All admissions data, n = 249) | n (%) | ||||
| Recent Stressful Events | |||||
| Socio-economic status low | 109 (72.7) | 2 (1.8) | 41 (37.6) | 66 (60.6) | 0.193 |
| Problems with family relationships | 77 (30.9) | 1 (1.3) | 24 (31.2) | 52 (67.5) | 0.994 |
| Problems with school | 22 (13.2) | 0 (0.0) | 8 (36.4) | 14 (63.6) | 0.819 |
| Quarreling with friends | 57 (22.9) | 0 (0.0) | 19 (33.3) | 38 (66.7) | 0.593 |
| Bullying | 60 (24.1) | 0 (0.0) | 26 (43.3) | 34 (56.4) | 0.042 |
| Child abuse: physical | 25 (10.0) | 1 (4.0) | 7 (28.0) | 17 (68) | 0.557 |
| Child abuse: sexual | 15 (6.0) | 0 (0.0) | 5 (33.3) | 10 (66.7) | |
| Patient’s Conditions/Addictions | |||||
| Chronic disease | 68 (27.8) | 1 (1.5) | 20 (29.4) | 47 (69.1) | 0.927 |
| Psychotic episode | 50 (20.2) | 0 (0.0) | 12 (24) | 38 (76) | 0.303 |
| Aggressive behavior | 27 (10.9) | 0 (0.0) | 4 (14.8) | 23 (85.2) | 0.660 |
| Internet addicted (patient) | 91 (36.5) | 2 (2.2) | 28 (30.8) | 61 (67.0) | 0.552 |
| Substance abuse: alcohol | 6 (2.5) | 0 (0.0) | 1 (16.7) | 5 (83.3) | 0.338 |
| Substance abuse (patient): cannabinoids | 32 (13.1) | 0 (0.0) | 5 (15.6) | 27 (84.4) | |
| Substance abuse (patient): other and/or more substances | 6 (2.5) | 0 (0.0) | 1 (16.7) | 5 (83.3) | |
| Age Group (Years) | * p | ||||
|---|---|---|---|---|---|
| Total | 5–10 | 11–14 | 15–18 | ||
| n (%) | |||||
| Suicidality | |||||
| Suicide attempt | 62 (24.9) | 0 (0.0) | 22 (35.5) | 40 (64.5) | 0.430 |
| Active suicidal ideation | 115 (46.2) | 2 (1.7) | 34 (29.6) | 79 (68.7) | 0.721 |
| Suicidality (both) | 177 (71.1) | 2 (1.1) | 56 (31.6) | 119 (67.2) | 0.920 |
| Suicide attempt | |||||
| First attempt at admission | 43 (28.3) | 0 (0.0) | 16 (37.2) | 27 (62.8) | 0.450 |
| Violent | 23 (37.1) | 0 (0.0) | 12 (52.2) | 11 (47.8) | 0.034 |
| Not violent | 39 (62.9) | 0 (0.0) | 10 (25.6 | 29 (74.4) | |
| Attempt at readmission | 19 (19.6) | 0 (0.0) | 6 (31.6) | 13 (68.4) | 0.560 |
| Previous attempts ^ | 47 (31.3) | 0 (0.0) | 14 (29.8) | 33 (70.2) | 0.377 |
| Suicide attempt method | |||||
| Drug overdose | 35 (56.5) | 0 (0.0) | 9 (25.7) | 26 (74.3) | 0.134 |
| Jumping from height | 8 (12.9) | 0 (0.0) | 5 (62.5) | 3 (37.5) | |
| Poison | 4 (6.5) | 0 (0.0) | 1 (25) | 3 (75) | |
| Firearm | 2 (3.2) | 0 (0.0) | 1 (50) | 1 (50) | |
| Wrist-cutting | 3 (4.8) | 0 (0.0) | 3 (100) | 0 (0.0) | |
| Drowning | 2 (3.2) | 0 (0.0) | 0 (0.0) | 2 (100) | |
| Vehicular impact | 4 (6.5) | 0 (0.0) | 1 (25.0) | 3 (75) | |
| Hanging | 2 (3.2) | 0 (0.0) | 1 (50) | 1 (50) | |
| Self-strangulation | 1 (1.6) | 0 (0.0) | 1 (100) | 0 (0.0) | |
| Self-immolation | 1 (1.6) | 0 (0.0) | 0 (0.0) | 1 (100) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ilia, S.; Sakapeti, E.; Briassoulis, P.; Gerostergios, G.; Vgontzas, A.; Briassoulis, G. Suicidality Prevalence in a Pediatric Psychiatric Clinic: Relation to Social and Environmental Risk Factors. Children 2023, 10, 558. https://doi.org/10.3390/children10030558
Ilia S, Sakapeti E, Briassoulis P, Gerostergios G, Vgontzas A, Briassoulis G. Suicidality Prevalence in a Pediatric Psychiatric Clinic: Relation to Social and Environmental Risk Factors. Children. 2023; 10(3):558. https://doi.org/10.3390/children10030558
Chicago/Turabian StyleIlia, Stavroula, Evangelia Sakapeti, Panagiotis Briassoulis, George Gerostergios, Alexandros Vgontzas, and George Briassoulis. 2023. "Suicidality Prevalence in a Pediatric Psychiatric Clinic: Relation to Social and Environmental Risk Factors" Children 10, no. 3: 558. https://doi.org/10.3390/children10030558
APA StyleIlia, S., Sakapeti, E., Briassoulis, P., Gerostergios, G., Vgontzas, A., & Briassoulis, G. (2023). Suicidality Prevalence in a Pediatric Psychiatric Clinic: Relation to Social and Environmental Risk Factors. Children, 10(3), 558. https://doi.org/10.3390/children10030558






