Adverse Childhood Experience as a Risk Factor for Developing Type 2 Diabetes among the Jazan Population: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Tool and Data Collection
2.3. Sample Size Calculation
2.4. Participants’ Inclusion and Exclusion Criteria
2.5. Statistical Analysis
2.6. Ethical Approval
3. Results
3.1. General Characteristics of the Participants
3.2. Characteristics of the Participants with Type 2 Diabetes Mellitus Compared to Those without Type 2 Diabetes Mellitus
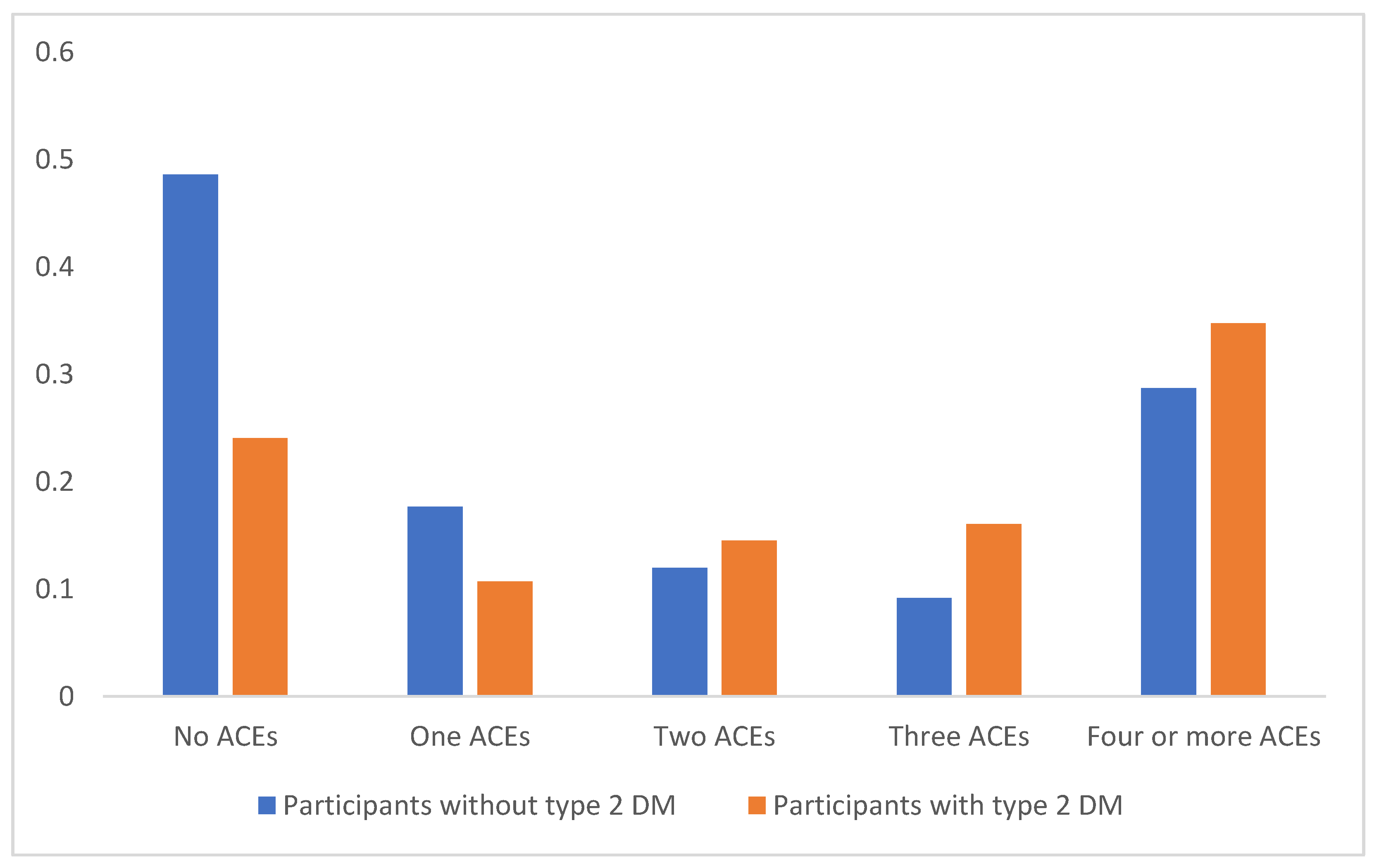
3.3. Adverse Childhood Events among Participants with Type 2 Diabetes Mellitus Compared to Those without Type 2 Diabetes Mellitus
3.4. Adverse Childhood Events of the Participants with Type 2 Diabetes Mellitus Compared to Those without Type 2 Diabetes Mellitus
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ahmed, A.S.; Alotaibi, W.S.; Aldubayan, M.A.; Alhowail, A.H.; Al-Najjar, A.H.; Chigurupati, S.; Elgharabawy, R.M. Factors Affecting the Incidence, Progression, and Severity of COVID-19 in Type 1 Diabetes Mellitus. BioMed Res. Int. 2021, 2021, 1676914. [Google Scholar] [CrossRef]
- Smushkin, G.; Vella, A. What is type 2 diabetes? Medicine 2010, 38, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Hughes, K.; Ford, K.; Bellis, M. Adverse Childhood Experiences (ACEs) and Diabetes|A Brief Review. Public Health Wales. Published Online First. 2020. Available online: https://research.bangor.ac.uk/portal/files/37959822/PHWBangor_ACEs_Diabetes_Factsheet_5_.pdf (accessed on 15 August 2022).
- Ayoub, C.C.; O’Connor, E.; Rappolt-Schlichtmann, G.; Fischer, K.W.; Rogosch, F.A.; Toth, S.L.; Cicchetti, D. Cognitive and emotional differences in young maltreated children: A translational application of dynamic skill theory. Dev. Psychopathol. 2006, 18, 679–706. [Google Scholar] [CrossRef] [PubMed]
- Kim-Spoon, J.; Cicchetti, D.; Rogosch, F.A. A Longitudinal Study of Emotion Regulation, Emotion Lability-Negativity, and Internalizing Symptomatology in Maltreated and Nonmaltreated Children. Child Dev. 2013, 84, 512–527. [Google Scholar] [CrossRef] [PubMed]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Marks, J.S. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Yan, P.; Shan, Z.; Chen, S.; Li, M.; Luo, C.; Gao, H.; Hao, L.; Liu, L. Adverse childhood experiences and risk of type 2 diabetes: A systematic review and meta-analysis. Metabolism 2015, 64, 1408–1418. [Google Scholar] [CrossRef]
- Almuneef, M.; Hollinshead, D.; Saleheen, H.; AlMadani, S.; Derkash, B.; AlBuhairan, F.; Al-Eissa, M.; Fluke, J. Adverse childhood experiences and association with health, mental health, and risky behavior in the kingdom of Saudi Arabia. Child Abuse Negl. 2016, 60, 10–17. [Google Scholar] [CrossRef]
- Campbell, J.A.; Mosley-Johnson, E.; Garacci, E.; Walker, R.J.; Egede, L.E. The co-occurrence of diabetes and adverse childhood experiences and its impact on mortality in US adults. J. Affect. Disord. 2019, 249, 20–25. [Google Scholar] [CrossRef]
- Lynch, L.; Waite, R.; Davey, M.P. Adverse Childhood Experiences and Diabetes in Adulthood: Support for a Collaborative Approach to Primary Care. Contemp. Fam. Ther. 2013, 35, 639–655. [Google Scholar] [CrossRef]
- Zhang, K.; Wu, B.; Zhang, W. Adverse childhood experiences in relation to comorbid cardiovascular diseases and diabetes among middle-aged and old adults in China. Geriatr. Gerontol. Int. 2022, 22, 12–18. [Google Scholar] [CrossRef]
- Subramaniam, M.; Abdin, E.; Vaingankar, J.A.; Chang, S.; Sambasivam, R.; Jeyagurunathan, A.; Seow, L.S.; Van Dam, R.; Chow, W.L.; Chong, S.A. Association of adverse childhood experiences with diabetes in adulthood: Results of a cross-sectional epidemiological survey in Singapore. BMJ Open 2021, 11, e045167. [Google Scholar] [CrossRef] [PubMed]
- Adverse Childhood Experiences International Questionnaire (ACE-IQ). Available online: https://cdn.who.int/media/docs/default-source/documents/child-maltreatment/ace-iq-guidance-for-analysing.pdf?sfvrsn=adfe12bb_2 (accessed on 13 January 2023).
- Alhowaymel, F.M.; Alenezi, A. Adverse Childhood Experiences and Health in Rural Areas of Riyadh Province in Saudi Arabia: A Cross-Sectional Study. Healthcare 2022, 10, 2502. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yin, Y.; Zhang, X.; Ye, J.; Zhang, J. Association of adverse childhood experiences with diabetes: A systematic review and meta-analysis. J. Diabetes Its Complicat. 2022, 36, 108289. [Google Scholar] [CrossRef]
- Zhu, S.; Shan, S.; Liu, W.; Li, S.; Hou, L.; Huang, X.; Liu, Y.; Yi, Q.; Sun, W.; Tang, K.; et al. Adverse childhood experiences and risk of diabetes: A systematic review and meta-analysis. J. Glob. Health 2022, 12, 04082. [Google Scholar] [CrossRef]
- Amemiya, A.; Fujiwara, T.; Shirai, K.; Kondo, K.; Oksanen, T.; Pentti, J.; Vahtera, J. Association between adverse childhood experiences and adult diseases in older adults: A comparative cross-sectional study in Japan and Finland. BMJ Open 2019, 9, e024609. [Google Scholar] [CrossRef] [PubMed]
- Widom, C.S.; Czaja, S.J.; Bentley, T.; Johnson, M.S. A prospective investigation of physical health outcomes in abused and neglected children: New findings from a 30-year follow-up. Am. J. Public Health 2012, 102, 1135–1144. [Google Scholar] [CrossRef]
- Monnat, S.M.; Chandler, R.F. Long Term Physical Health Consequences of Adverse Childhood Experiences. Sociol. Q. 2015, 56, 723–752. [Google Scholar] [CrossRef]
- Cavanaugh, C.E.; Petras, H.; Martins, S.S. Gender-specific profiles of adverse childhood experiences, past year mental and substance use disorders, and their associations among a national sample of adults in the United States. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 1257–1266. [Google Scholar] [CrossRef]
- Haahr-Pedersen, I.; Perera, C.; Hyland, P.; Vallières, F.; Murphy, D.; Hansen, M.; Spitz, P.; Hansen, P.; Cloitre, M. Females have more complex patterns of childhood adversity: Implications for mental, social, and emotional outcomes in adulthood. Eur. J. Psychotraumatol. 2020, 11, 1708618. [Google Scholar] [CrossRef]
- Lown, E.A.; Lui, C.K.; Karriker-Jaffe, K.; Mulia, N.; Williams, E.; Ye, Y.; Li, L.; Greenfield, T.K.; Kerr, W.C. Adverse childhood events and risk of diabetes onset in the 1979 National longitudinal survey of youth cohort. BMC Public Health 2019, 19, 1007. [Google Scholar] [CrossRef]
- Kalmakis, K.A.; Meyer, J.S.; Chiodo, L.; Leung, K. Adverse childhood experiences and chronic hypothalamic–pituitary–adrenal activity. Stress 2015, 18, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Mosili, P.; Mkhize, B.C.; Ngubane, P.; Sibiya, N.; Khathi, A. The dysregulation of the hypothalamic-pituitary-adrenal axis in diet-induced prediabetic male Sprague Dawley rats. Nutr. Metab. (Lond.) 2020, 17, 104. [Google Scholar] [CrossRef] [PubMed]
- Bădescu, S.V.; Tătaru, C.; Kobylinska, L.; Georgescu, E.L.; Zahiu, D.M.; Zăgrean, A.M.; Zăgrean, L. The association between Diabetes mellitus and depression. J. Med. Life 2016, 9, 120–125. [Google Scholar] [PubMed]
- Soares, S.; Rocha, V.; Kelly-Irving, M.; Stringhini, S.; Fraga, S. Adverse Childhood Events and Health Biomarkers: A Systematic Review. Front. Public Health 2021, 9, 649825. [Google Scholar] [CrossRef] [PubMed]
- Deschênes, S.S.; Graham, E.; Kivimäki, M.; Schmitz, N. Adverse Childhood Experiences and the Risk of Diabetes: Examining the Roles of Depressive Symptoms and Cardiometabolic Dysregulations in the Whitehall II Cohort Study. Diabetes Care 2018, 41, 2120–2126. [Google Scholar] [CrossRef]
- Al-Eissa, M.A.; AlBuhairan, F.S.; Qayad, M.; Saleheen, H.; Runyan, D.; Almuneef, M. Determining child maltreatment incidence in Saudi Arabia using the ICAST-CH: A pilot study. Child Abuse Neglect 2015, 42, 174–182. [Google Scholar] [CrossRef]
- AlHemyari, A.H.; Al-Zamil, N.A.; Shaikh, A.Y.; Al-Eidi, D.A.; Al-Dahlan, H.W.; Al-Shamekh, S.S. Prevalence of adverse childhood experiences and their relationship to mental and physical illnesses in the Eastern Region of Saudi Arabia. Brain Behav. 2022, 12, e2668. [Google Scholar] [CrossRef]
- Alhowaymel, F. Geographical Disparity of Adverse Childhood Experiences and Chronic Diseases in Saudi Arabia. Ph.D. Thesis, University of Massachusetts Amherst, Amherst, MA, USA, 2020. [Google Scholar] [CrossRef]
- Herzog, J.I.; Schmahl, C. Adverse Childhood Experiences and the Consequences on Neurobiological, Psychosocial, and Somatic Conditions Across the Lifespan. Front. Psychiatry 2018, 9, 420. [Google Scholar] [CrossRef]
- Robert, A.; Al Dawish, M.; Braham, R.; Musallam, M.; Al Hayek, A.; Al Kahtany, N. Type 2 Diabetes Mellitus in Saudi Arabia: Major Challenges and Possible Solutions. CDR 2016, 13, 59–64. [Google Scholar] [CrossRef]
- Itumalla, R.; Kumar, R.; Tharwat Elabbasy, M.; Perera, B.; Torabi, M.R. Structural Factors and Quality of Diabetes Health Services in Hail, Saudi Arabia: A Cross-Sectional Study. Healthcare 2021, 9, 1691. [Google Scholar] [CrossRef]
- Al-Quwaidhi, A.J.; Pearce, M.S.; Sobngwi, E.; Critchley, J.A.; O’Flaherty, M. Comparison of type 2 diabetes prevalence estimates in Saudi Arabia from a validated Markov model against the International Diabetes Federation and other modelling studies. Diabetes Res. Clin. Pract. 2014, 103, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Albeladi, F.I.; Alluli, M.M.; Daghriri, K.A.; Almalki, Y.H.; Wafi, M.Y.; Otaif, F.A.; Sulays, Z.Y.; Hakami, A.A.; Alharbi, A.A.; Alhazmi, A.H. Level of Adherence to COVID-19 Preventive Measures Among HealthCare Workers in Saudi Arabia. Cureus 2021, 13, e15969. [Google Scholar] [CrossRef] [PubMed]
- Aquilina, S.R.; Shrubsole, M.J.; Butt, J.; Sanderson, M.; Schlundt, D.G.; Cook, M.C.; Epplein, M. Adverse childhood experiences and adultdiet quality. J. Nutr. Sci. 2021, 10, e95. [Google Scholar] [CrossRef] [PubMed]
- Alhazmi, A.; Sane, F.; Lazrek, M.; Nekoua, M.P.; Badia-Boungou, F.; Engelmann, I.; Alidjinou, E.K.; Hober, D. Enteroviruses and Type 1 Diabetes Mellitus: An Overlooked Relationship in Some Regions. Microorganisms 2020, 8, 1458. [Google Scholar] [CrossRef]
- Hurissi, E.; Alameer, M.; Ageeli, F.; Allami, M.; Alharbi, M.; Suhail, H.; Albeishy, H.; Oraibi, O.; Somaili, M.; Hummadi, A.; et al. The Association between SARS-CoV-2 Infection and Diabetic Ketoacidosis in Patients with New-Onset Diabetes: A Retrospective Study from a Diabetic Center in Saudi Arabia. Pediatr. Rep. 2022, 14, 519–527. [Google Scholar] [CrossRef]
| Age in Years | Mean|SD | 40.45 | 12.93 |
|---|---|---|---|
| Sex | Female | 303 | 52.33% |
| Male | 276 | 47.67% | |
| Marital status | Single | 148 | 25.56% |
| Married | 378 | 65.28% | |
| Divorced | 37 | 6.39% | |
| Widow | 16 | 2.76% | |
| Job | Student | 95 | 16.41% |
| Employed | 314 | 54.23% | |
| Looking for job | 80 | 13.82% | |
| Retired | 90 | 15.54% | |
| Monthly income in SAR | Less than 5 k | 183 | 31.61% |
| from 5 k to 10 k | 153 | 26.42% | |
| From 10 k to 15 k | 152 | 26.25% | |
| More than 15 k | 91 | 15.72% | |
| Residence | City | 180 | 31.09% |
| Governate | 188 | 32.47% | |
| Village | 192 | 33.16% | |
| Mountain | 19 | 3.28% | |
| Educational level | Informal education | 10 | 1.73% |
| General education | 130 | 22.45% | |
| University level | 422 | 72.88% | |
| Postgraduate | 17 | 2.94% | |
| Father | Informal education | 138 | 23.83% |
| General education | 237 | 40.93% | |
| University level | 189 | 32.64% | |
| Postgraduate | 15 | 2.59% | |
| Mother | Informal education | 261 | 45.08% |
| General education | 177 | 30.57% | |
| University level | 138 | 23.83% | |
| Postgraduate | 4 | 0.69% | |
| BMI classification | Underweight | 32 | 5.53% |
| Normal | 195 | 33.68% | |
| Overweight | 201 | 34.72% | |
| Obese | 151 | 26.08% | |
| First degree relative | No | 313 | 54.06% |
| Yes | 266 | 45.94% | |
| Have you been diagnosed with type 2 DM | No | 317 | 54.75% |
| Yes | 262 | 45.25% | |
| BMI | Mean | SD | 26.97 | 5.54 |
| How was your diagnosis first confirmed | FBG | 63 | 24.05% |
| RBG | 30 | 11.45% | |
| HBa1c | 165 | 62.98% | |
| OGT | 4 | 1.53% |
| Variables | Participants without T2DM (n = 317, 54.75%) | Participants with T2DM (n = 262, 45.25%) | p-Value | |||
|---|---|---|---|---|---|---|
| Age in years (mean|SD) | 35.95 | 11.57 | 44.34 | 12.80 | 0.0001 * | |
| Sex | Female | 194 | 61.20% | 109 | 41.60% | 0.0001 * |
| Male | 123 | 38.80% | 153 | 58.40% | ||
| Marital status | Single | 117 | 36.91% | 31 | 11.83% | 0.0001 * |
| Married | 185 | 58.36% | 193 | 73.66% | ||
| Divorced | 11 | 3.47% | 26 | 9.92% | ||
| Widow | 4 | 1.26% | 12 | 4.58% | ||
| Job | Student | 79 | 24.92% | 16 | 6.11% | 0.0001 * |
| Employed | 160 | 50.47% | 154 | 58.78% | ||
| Looking for job | 57 | 17.98% | 23 | 8.78% | ||
| Retired | 21 | 6.62% | 69 | 26.34% | ||
| Monthly income in SAR | Less than 5 k | 117 | 36.91% | 66 | 25.19% | 0.007 * |
| from 5 k to 10 k | 69 | 21.77% | 84 | 32.06% | ||
| From 10 k to 15 k | 82 | 25.87% | 70 | 26.72% | ||
| More than 15 k | 49 | 15.46% | 42 | 16.03% | ||
| Residence | City | 101 | 31.86% | 79 | 30.15% | 0.703 |
| Governate | 104 | 32.81% | 84 | 32.06% | ||
| Village | 104 | 32.81% | 88 | 33.59% | ||
| Mountain | 8 | 2.52% | 11 | 4.20% | ||
| Educational level | Informal education | 2 | 0.63% | 8 | 3.05% | 0.0001 * |
| General education | 51 | 16.09% | 79 | 30.15% | ||
| University level | 248 | 78.23% | 174 | 66.41% | ||
| Postgraduate | 16 | 5.05% | 1 | 0.38% | ||
| Fathers’ educational level | Informal education | 54 | 17.03% | 84 | 32.06% | 0.0001 * |
| General education | 133 | 41.96% | 104 | 39.69% | ||
| University level | 116 | 36.59% | 73 | 27.86% | ||
| Postgraduate | 14 | 4.42% | 1 | 0.38% | ||
| Mother’s educational level | Informal education | 110 | 34.70% | 151 | 57.63% | 0.0001 * |
| General education | 107 | 33.75% | 70 | 26.72% | ||
| University level | 98 | 30.91% | 40 | 15.27% | ||
| Postgraduate | 2 | 0.63% | 1 | 0.38% | ||
| BMI classification | Underweight | 28 | 8.83% | 4 | 1.53% | 0.002 * |
| Normal | 107 | 33.75% | 88 | 33.59% | ||
| Overweight | 105 | 33.12% | 96 | 36.64% | ||
| Obese | 77 | 24.29% | 74 | 28.24% | ||
| First-degree relative relationship | No | 172 | 54.26% | 141 | 53.82% | 0.933 |
| Yes | 145 | 45.74% | 121 | 46.18% | ||
| Variables | Participants without Type 2 DM (n = 317, 54.75%) | Participants with Type 2 DM (n = 262, 45.25%) | p-Value | |||
|---|---|---|---|---|---|---|
| Did a parent or other adult in the household often swear at you, insult you, put you down, or humiliate you? | No | 226 | 71.29% | 124 | 47.33% | 0.0001 * |
| Yes | 91 | 28.71% | 138 | 52.67% | ||
| Did a parent or other person in the home often threaten you physically? | No | 266 | 83.91% | 183 | 69.85% | 0.0001 * |
| Yes | 51 | 16.09% | 79 | 30.15% | ||
| Have you often felt that no one in your family loves you? | No | 244 | 76.97% | 166 | 63.36% | 0.0001 * |
| Yes | 73 | 23.03% | 96 | 36.64% | ||
| Have you often felt that you have no one to protect you? | No | 277 | 87.38% | 198 | 75.57% | 0.0001 * |
| Yes | 40 | 12.62% | 64 | 24.43% | ||
| Have you often felt that you have no one to take you to the doctor even though you need to? | No | 289 | 91.17% | 186 | 70.99% | 0.0001 * |
| Yes | 28 | 8.83% | 76 | 29.01% | ||
| Has a parent or someone ever hit you often? | No | 219 | 69.09% | 123 | 46.95% | 0.0001 * |
| Yes | 98 | 30.91% | 139 | 53.05% | ||
| Have you lived with someone in your family who suffers from drinking or alcohol addiction? | No | 312 | 98.42% | 235 | 89.69% | 0.0001 * |
| Yes | 5 | 1.58% | 27 | 10.31% | ||
| Have you had a friend who suffers from drinking or alcohol addiction? | No | 310 | 97.79% | 233 | 88.93% | 0.0001 * |
| Yes | 7 | 2.21% | 29 | 11.07% | ||
| Was a household member depressed or mentally ill | No | 292 | 92.11% | 200 | 76.34% | 0.0001 * |
| Yes | 25 | 7.89% | 62 | 23.66% | ||
| Did a household member attempt suicide? | No | 309 | 97.48% | 230 | 87.79% | 0.0001 * |
| Yes | 8 | 2.52% | 32 | 12.21% | ||
| Did you live with your parents | No | 33 | 10.41% | 52 | 19.85% | 0.002 * |
| Yes | 284 | 89.59% | 210 | 80.15% | ||
| Did your family take care of each other? | No | 23 | 7.26% | 54 | 20.61% | 0.0001 * |
| Yes | 294 | 92.74% | 208 | 79.39% | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oraibi, O.; Ghalibi, A.T.; Shami, M.O.; Khawaji, M.J.; Madkhali, K.A.; Yaseen, A.M.; Hakami, S.M.; Alhazmi, N.H.; Mahla, K.H.; Qumayri, M.A.; et al. Adverse Childhood Experience as a Risk Factor for Developing Type 2 Diabetes among the Jazan Population: A Cross-Sectional Study. Children 2023, 10, 499. https://doi.org/10.3390/children10030499
Oraibi O, Ghalibi AT, Shami MO, Khawaji MJ, Madkhali KA, Yaseen AM, Hakami SM, Alhazmi NH, Mahla KH, Qumayri MA, et al. Adverse Childhood Experience as a Risk Factor for Developing Type 2 Diabetes among the Jazan Population: A Cross-Sectional Study. Children. 2023; 10(3):499. https://doi.org/10.3390/children10030499
Chicago/Turabian StyleOraibi, Omar, Ali T. Ghalibi, Mohammed O. Shami, Meshal J. Khawaji, Khalid A. Madkhali, Abdulrahman M. Yaseen, Sultan M. Hakami, Nirmin H. Alhazmi, Khulud H. Mahla, Marwah A. Qumayri, and et al. 2023. "Adverse Childhood Experience as a Risk Factor for Developing Type 2 Diabetes among the Jazan Population: A Cross-Sectional Study" Children 10, no. 3: 499. https://doi.org/10.3390/children10030499
APA StyleOraibi, O., Ghalibi, A. T., Shami, M. O., Khawaji, M. J., Madkhali, K. A., Yaseen, A. M., Hakami, S. M., Alhazmi, N. H., Mahla, K. H., Qumayri, M. A., Majrashi, K. A., Hummadi, A., Madkhali, M. A., & Alhazmi, A. H. (2023). Adverse Childhood Experience as a Risk Factor for Developing Type 2 Diabetes among the Jazan Population: A Cross-Sectional Study. Children, 10(3), 499. https://doi.org/10.3390/children10030499






