The Role of SNPs in the Pathogenesis of Idiopathic Central Precocious Puberty in Girls
Abstract
1. Introduction
Aim
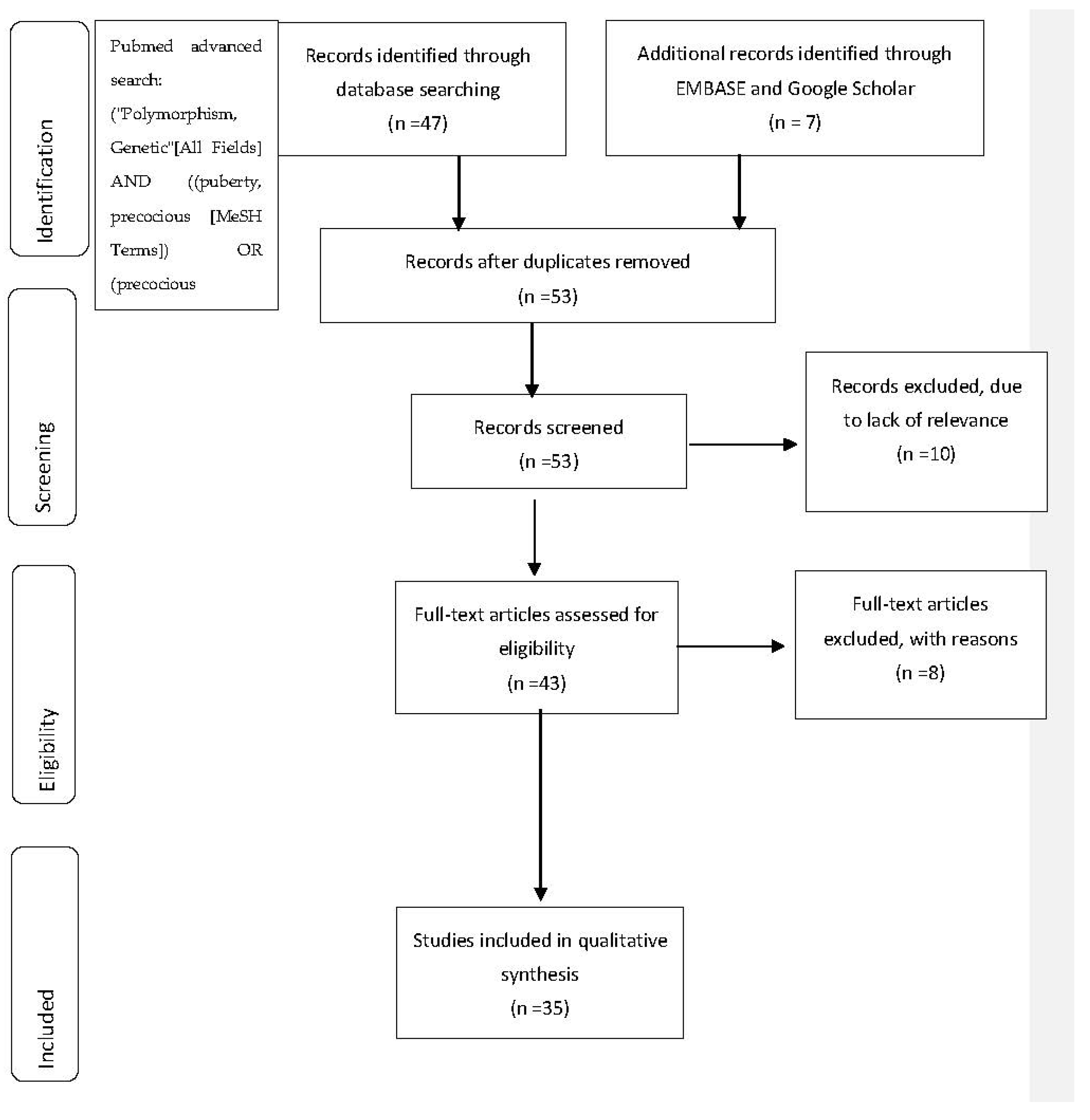
2. Materials and Methods
3. Results
Most Important Polymorphisms
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Latronico, A.C.; Brito, V.N.; Carel, J.-C. Causes, Diagnosis, and Treatment of Central Precocious Puberty. Lancet Diabetes Endocrinol. 2016, 4, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Berberoğlu, M. Precocious Puberty and Normal Variant Puberty: Definition, Etiology, Diagnosis and Current Management—Review. J. Clin. Res. Pediatr. Endocrinol. 2009, 1, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Alotaibi, M.F. Physiology of Puberty in Boys and Girls and Pathological Disorders Affecting Its Onset. J. Adolesc. 2019, 71, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Soriano-Guillén, L.; Argente, J. Central Precocious Puberty, Functional and Tumor-Related. Best Pract. Res. Clin. Endocrinol. Metab. 2019, 33, 101262. [Google Scholar] [CrossRef]
- Carel, J.-C.; Léger, J. Precocious Puberty. N. Engl. J. Med. 2008, 358, 2366–2377. [Google Scholar] [CrossRef]
- Youn, H.J.; Han, W. A Review of the Epidemiology of Breast Cancer in Asia: Focus on Risk Factors. Asian Pac. J. Cancer Prev. 2020, 21, 867–880. [Google Scholar] [CrossRef]
- Okoth, K.; Chandan, J.S.; Marshall, T.; Thangaratinam, S.; Thomas, G.N.; Nirantharakumar, K.; Adderley, N.J. Association between the Reproductive Health of Young Women and Cardiovascular Disease in Later Life: Umbrella Review. BMJ 2020, 371, m3502. [Google Scholar] [CrossRef]
- Belbasis, L.; Bellou, V.; Tzoulaki, I.; Evangelou, E. Early-Life Factors and Risk of Multiple Sclerosis: An MR-EWAS. Neuroepidemiology 2020, 54, 433–445. [Google Scholar] [CrossRef]
- Sultan, C.; Gaspari, L.; Maimoun, L.; Kalfa, N.; Paris, F. Disorders of Puberty. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 48, 62–89. [Google Scholar] [CrossRef]
- Chen, M.; Eugster, E.A. Central Precocious Puberty: Update on Diagnosis and Treatment. Pediatr Drugs 2015, 17, 273–281. [Google Scholar] [CrossRef]
- Robert, F.; Pelletier, J. Exploring the Impact of Single-Nucleotide Polymorphisms on Translation. Front. Genet. 2018, 9, 507. [Google Scholar] [CrossRef] [PubMed]
- Walter, N.A.R.; McWeeney, S.K.; Peters, S.T.; Belknap, J.K.; Hitzemann, R.; Buck, K.J. Single-Nucleotide Polymorphism Masking. Alcohol Res. Health 2008, 31, 270–271. [Google Scholar] [PubMed]
- Altshuler, D.; Daly, M.J.; Lander, E.S. Genetic Mapping in Human Disease. Science 2008, 322, 881–888. [Google Scholar] [CrossRef] [PubMed]
- Visscher, P.M.; Yengo, L.; Cox, N.J.; Wray, N.R. Discovery and Implications of Polygenicity of Common Diseases. Science 2021, 373, 1468–1473. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Chen, T.; Zhou, Y.; Li, K.; Xiao, J. An Association Study between the Genetic Polymorphisms within GnRHI, LHβ and FSHβ Genes and Central Precocious Puberty in Chinese Girls. Neurosci. Lett. 2010, 486, 188–192. [Google Scholar] [CrossRef]
- Ko, J.M.; Lee, H.S.; Hwang, J.S. KISS1 Gene Analysis in Korean Girls with Central Precocious Puberty: A Polymorphism, p.P110T, Suggested to Exert a Protective Effect. Endocr. J. 2010, 57, 701–709. [Google Scholar] [CrossRef]
- Li, D.; Wu, Y.; Cheng, J.; Liu, L.; Li, X.; Chen, D.; Huang, S.; Wen, Y.; Ke, Y.; Yao, Y.; et al. Association of Polymorphisms in the Kisspeptin/GPR54 Pathway Genes with Risk of Early Puberty in Chinese Girls. J. Clin. Endocrinol. Metab. 2020, 105, e1458–e1467. [Google Scholar] [CrossRef]
- Rhie, Y.-J.; Lee, K.-H.; Ko, J.M.; Lee, W.J.; Kim, J.H.; Kim, H.-S. KISS1 Gene Polymorphisms in Korean Girls with Central Precocious Puberty. J. Korean Med. Sci. 2014, 29, 1120. [Google Scholar] [CrossRef]
- Shahab, M.; Mastronardi, C.; Seminara, S.B.; Crowley, W.F.; Ojeda, S.R.; Plant, T.M. Increased Hypothalamic GPR54 Signaling: A Potential Mechanism for Initiation of Puberty in Primates. Proc. Natl. Acad. Sci. USA 2005, 102, 2129–2134. [Google Scholar] [CrossRef]
- Luan, X.; Zhou, Y.; Wang, W.; Yu, H.; Li, P.; Gan, X.; Wei, D.; Xiao, J. Association Study of the Polymorphisms in the KISS1 Gene with Central Precocious Puberty in Chinese Girls. Eur. J. Endocrinol. 2007, 157, 113–118. [Google Scholar] [CrossRef]
- Luan, X.; Yu, H.; Wei, X.; Zhou, Y.; Wang, W.; Li, P.; Gan, X.; Wei, D.; Xiao, J. GPR54 Polymorphisms in Chinese Girls with Central Precocious Puberty. Neuroendocrinology 2007, 86, 77–83. [Google Scholar] [CrossRef]
- Ghaemi, N.; Ghahraman, M.; Noroozi Asl, S.; Vakili, R.; Fardi Golyan, F.; Moghbeli, M.; Abbaszadegan, M.R. Novel DNA Variation of GPR54 Gene in Familial Central Precocious Puberty. Ital. J. Pediatr. 2019, 45, 10. [Google Scholar] [CrossRef] [PubMed]
- Oh, Y.J.; Rhie, Y.-J.; Nam, H.-K.; Kim, H.R.; Lee, K.-H. Genetic Variations of the KISS1R Gene in Korean Girls with Central Precocious Puberty. J. Korean Med. Sci. 2017, 32, 108. [Google Scholar] [CrossRef] [PubMed]
- Abreu, A.P.; Dauber, A.; Macedo, D.B.; Noel, S.D.; Brito, V.N.; Gill, J.C.; Cukier, P.; Thompson, I.R.; Navarro, V.M.; Gagliardi, P.C.; et al. Central Precocious Puberty Caused by Mutations in the Imprinted Gene MKRN3. N. Engl. J. Med. 2013, 368, 2467–2475. [Google Scholar] [CrossRef] [PubMed]
- Butler, M.G. Genomic Imprinting Disorders in Humans: A Mini-Review. J. Assist. Reprod. Genet. 2009, 26, 477–486. [Google Scholar] [CrossRef]
- Grandone, A.; Capristo, C.; Cirillo, G.; Sasso, M.; Umano, G.R.; Mariani, M.; Miraglia Del Giudice, E.; Perrone, L. Molecular Screening of MKRN3, DLK1, and KCNK9 Genes in Girls with Idiopathic Central Precocious Puberty. Horm. Res. Paediatr. 2017, 88, 194–200. [Google Scholar] [CrossRef]
- Meader, B.N.; Albano, A.; Sekizkardes, H.; Delaney, A. Heterozygous Deletions in MKRN3 Cause Central Precocious Puberty Without Prader-Willi Syndrome. J. Clin. Endocrinol. Metab. 2020, 105, 2732–2739. [Google Scholar] [CrossRef]
- Settas, N.; Dacou-Voutetakis, C.; Karantza, M.; Kanaka-Gantenbein, C.; Chrousos, G.P.; Voutetakis, A. Central Precocious Puberty in a Girl and Early Puberty in Her Brother Caused by a Novel Mutation in the MKRN3 Gene. J. Clin. Endocrinol. Metab. 2014, 99, E647–E651. [Google Scholar] [CrossRef]
- Jeong, H.R.; Lee, H.S.; Hwang, J.S. Makorin Ring Finger 3 Gene Analysis in Koreans with Familial Precocious Puberty. J. Clin. Endocrinol. Metab. 2017, 30, 1197–1201. [Google Scholar] [CrossRef]
- Yi, B.R.; Kim, H.J.; Park, H.S.; Cho, Y.J.; Kim, J.Y.; Yee, J.; Chung, J.E.; Kim, J.H.; Lee, K.E.; Gwak, H.S. Association between MKRN3 and LIN28B Polymorphisms and Precocious Puberty. BMC Genet. 2018, 19, 47. [Google Scholar] [CrossRef] [PubMed]
- Pagani, S.; Calcaterra, V.; Acquafredda, G.; Montalbano, C.; Bozzola, E.; Ferrara, P.; Gasparri, M.; Villani, A.; Bozzola, M. MKRN3 and KISS1R Mutations in Precocious and Early Puberty. Ital. J. Pediatr. 2020, 46, 39. [Google Scholar] [CrossRef] [PubMed]
- Bessa, D.S.; Maschietto, M.; Aylwin, C.F.; Canton, A.P.M.; Brito, V.N.; Macedo, D.B.; Cunha-Silva, M.; Palhares, H.M.C.; de Resende, E.A.M.R.; Borges, M.D.F.; et al. Methylome Profiling of Healthy and Central Precocious Puberty Girls. Clin. Epigenet. 2018, 10, 146. [Google Scholar] [CrossRef] [PubMed]
- Dauber, A.; Cunha-Silva, M.; Macedo, D.B.; Brito, V.N.; Abreu, A.P.; Roberts, S.A.; Montenegro, L.R.; Andrew, M.; Kirby, A.; Weirauch, M.T.; et al. Paternally Inherited DLK1 Deletion Associated with Familial Central Precocious Puberty. J. Clin. Endocrinol. Metab. 2017, 102, 1557–1567. [Google Scholar] [CrossRef] [PubMed]
- Macedo, D.B.; Kaiser, U.B. DLK1, Notch Signaling and the Timing of Puberty. Semin. Reprod. Med. 2019, 37, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Gomes, L.G.; Cunha-Silva, M.; Crespo, R.P.; Ramos, C.O.; Montenegro, L.R.; Canton, A.; Lees, M.; Spoudeas, H.; Dauber, A.; Macedo, D.B.; et al. DLK1 Is a Novel Link Between Reproduction and Metabolism. J. Clin. Endocrinol. Metab. 2019, 104, 2112–2120. [Google Scholar] [CrossRef]
- Topaloglu, A.K.; Reimann, F.; Guclu, M.; Yalin, A.S.; Kotan, L.D.; Porter, K.M.; Serin, A.; Mungan, N.O.; Cook, J.R.; Ozbek, M.N.; et al. TAC3 and TACR3 Mutations in Familial Hypogonadotropic Hypogonadism Reveal a Key Role for Neurokinin B in the Central Control of Reproduction. Nat. Genet. 2009, 41, 354–358. [Google Scholar] [CrossRef]
- Brauner, R.; Bignon-Topalovic, J.; Bashamboo, A.; McElreavey, K. Peripheral Precocious Puberty of Ovarian Origin in a Series of 18 Girls: Exome Study Finds Variants in Genes Responsible for Hypogonadotropic Hypogonadism. Front. Pediatr. 2021, 9, 641397. [Google Scholar] [CrossRef]
- Nakayama, Y.; Wondisford, F.E.; Lash, R.W.; Bale, A.E.; Weintraub, B.D.; Cutler, G.B.; Radovick, S. Analysis of Gonadotropin-Releasing Hormone Gene Structure in Families with Familial Central Precocious Puberty and Idiopathic Hypogonadotropic Hypogonadism. J. Clin. Endocrinol. Metab. 1990, 70, 1233–1238. [Google Scholar] [CrossRef]
- Ubuka, T.; Inoue, K.; Fukuda, Y.; Mizuno, T.; Ukena, K.; Kriegsfeld, L.J.; Tsutsui, K. Identification, Expression, and Physiological Functions of Siberian Hamster Gonadotropin-Inhibitory Hormone. Endocrinology 2012, 153, 373–385. [Google Scholar] [CrossRef]
- Bentley, G.E.; Tsutsui, K.; Kriegsfeld, L.J. Recent Studies of Gonadotropin-Inhibitory Hormone (GnIH) in the Mammalian Hypothalamus, Pituitary and Gonads. Brain Res. 2010, 1364, 62–71. [Google Scholar] [CrossRef]
- Hinuma, S.; Shintani, Y.; Fukusumi, S.; Iijima, N.; Matsumoto, Y.; Hosoya, M.; Fujii, R.; Watanabe, T.; Kikuchi, K.; Terao, Y.; et al. New Neuropeptides Containing Carboxy-Terminal RFamide and Their Receptor in Mammals. Nat. Cell Biol. 2000, 2, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Lima, C.J.G.; Cardoso, S.C.; Lemos, E.F.L.; Zingler, E.; Capanema, C.; Menezes, L.D.; Vogado, G.; dos Santos, B.T.A.; de Moraes, O.L.; Duarte, E.F.; et al. Mutational Analysis of the Genes Encoding RFAmide-Related Peptide-3, the Human Orthologue of Gonadotrophin-Inhibitory Hormone, and Its Receptor (GPR147) in Patients with Gonadotrophin-Releasing Hormone-Dependent Pubertal Disorders. J. Neuroendocrinol. 2014, 26, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Aiello, F.; Cirillo, G.; Cassio, A.; Di Mase, R.; Tornese, G.; Umano, G.R.; Miraglia del Giudice, E.; Grandone, A. Molecular Screening of PROKR2 Gene in Girls with Idiopathic Central Precocious Puberty. Ital. J. Pediatr. 2021, 47, 5. [Google Scholar] [CrossRef] [PubMed]
- He, C.; Kraft, P.; Chen, C.; Buring, J.E.; Paré, G.; Hankinson, S.E.; Chanock, S.J.; Ridker, P.M.; Hunter, D.J.; Chasman, D.I. Genome-Wide Association Studies Identify Loci Associated with Age at Menarche and Age at Natural Menopause. Nat. Genet. 2009, 41, 724–728. [Google Scholar] [CrossRef] [PubMed]
- Park, S.W.; Lee, S.-T.; Sohn, Y.B.; Cho, S.Y.; Kim, S.-H.; Kim, S.J.; Kim, C.H.; Ko, A.-R.; Paik, K.-H.; Kim, J.-W.; et al. LIN28B Polymorphisms Are Associated with Central Precocious Puberty and Early Puberty in Girls. Korean J. Pediatr. 2012, 55, 388. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.K.; Elks, C.E.; Li, S.; Zhao, J.H.; Luan, J.; Andersen, L.B.; Bingham, S.A.; Brage, S.; Smith, G.D.; Ekelund, U.; et al. Genetic Variation in LIN28B Is Associated with the Timing of Puberty. Nat. Genet. 2009, 41, 729–733. [Google Scholar] [CrossRef]
- Chen, Y.-C.; Chen, L.-M.; Lin, H.-H.; Chen, B.-H.; Chao, M.-C.; Hsiao, H.-P. Association Study of LIN28B in Girls with Precocious Puberty. J. Pediatr. Endocrinol. Metab. 2017, 30, 663–667. [Google Scholar] [CrossRef]
- Hu, Z.; Chen, R.; Cai, C. Association of Genetic Polymorphisms around the LIN28B Gene and Idiopathic Central Precocious Puberty Risks among Chinese Girls. Pediatr. Res. 2016, 80, 521–525. [Google Scholar] [CrossRef]
- Chou, I.-C.; Wang, C.-H.; Lin, W.-D.; Tsai, C.-H.; Tsai, F.-J. Association Study in Taiwanese Girls with Precocious Puberty. J. Clin. Endocrinol. Metab. 2011, 24, 103–104. [Google Scholar] [CrossRef]
- Ranke, M.B. Insulin-like Growth Factor Binding-Protein-3 (IGFBP–3). Best Pract. Res. Clin. Endocrinol. Metab. 2015, 29, 701–711. [Google Scholar] [CrossRef]
- Dai, Z.; Wu, F.; Yeung, E.W.; Li, Y. IGF-IEc Expression, Regulation and Biological Function in Different Tissues. Growth Horm. IGF Res. 2010, 20, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.-P.; Yang, S.-F.; Wang, S.-L.; Su, P.-H. Associations among IGF-1, IGF2, IGF-1R, IGF-2R, IGFBP-3, Insulin Genetic Polymorphisms and Central Precocious Puberty in Girls. BMC Endocr. Disord. 2018, 18, 66. [Google Scholar] [CrossRef] [PubMed]
- Schmitz-Peiffer, C.; Whitehead, J. IRS-1 Regulation in Health and Disease. IUBMB Life 2003, 55, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Xin, X.; Xiao, J.; Luan, X.; Zhou, Y.; Lu, D.; Wei, D.; Yang, S. Association Study of Six Activity SNPS in Adrenal Steroid Hormone Metabolism and IBM Related Genes with Precocious Puberty in Chinese Girls. Neuro. Endocrinol. Lett. 2006, 27, 219–224. [Google Scholar] [PubMed]
- Laakso, S.; Utriainen, P.; Laakso, M.; Voutilainen, R.; Jääskeläinen, J. Polymorphism Pro12Ala of PPARG in Prepubertal Children with Premature Adrenarche and Its Association with Growth in Healthy Children. Horm. Res. Paediatr. 2010, 74, 365–371. [Google Scholar] [CrossRef]
- Tusset, C.; Noel, S.D.; Trarbach, E.B.; Silveira, L.F.G.; Jorge, A.A.L.; Brito, V.N.; Cukier, P.; Seminara, S.B.; Mendonça, B.B.D.; Kaiser, U.B.; et al. Mutational Analysis of TAC3 and TACR3 Genes in Patients with Idiopathic Central Pubertal Disorders. Arq. Bras. Endocrinol. Metabol. 2012, 56, 646–652. [Google Scholar] [CrossRef]
- Xin, X.; Zhang, J.; Chang, Y.; Wu, Y. Association Study of TAC3 and TACR3 Gene Polymorphisms with Idiopathic Precocious Puberty in Chinese Girls. J. Pediatr. Endocrinol. Metab. 2015, 28, 65–71. [Google Scholar] [CrossRef]
- Lee, H.S.; Park, H.K.; Kim, K.H.; Ko, J.H.; Kim, Y.J.; Yi, K.H.; Hwang, J.S. Estrogen Receptor α Gene Analysis in Girls with Central Precocious Puberty. J. Pediatr. Endocrinol. Metab. 2013, 26, 645–649. [Google Scholar] [CrossRef]
- Lee, H.; Kim, Y.; Hwang, J. No Effect of the Estrogen Receptor α Gene Polymorphisms in the Etiology of Precocious Puberty in Girls. Exp. Clin. Endocrinol. Diabetes 2013, 121, 206–209. [Google Scholar] [CrossRef]
- Stavrou, I. Association of Polymorphisms of the Oestrogen Receptoralpha Gene with the Age of Menarche. Hum. Reprod. 2002, 17, 1101–1105. [Google Scholar] [CrossRef]
- Soares, J.M., Jr.; de Holanda, F.S.; Matsuzaki, C.N.; Sorpreso, I.C.E.; de Arruda Veiga, E.C.; de Abreu, L.C.; Carvalho, K.C.; Baracat, E.C. Analysis of the PvuII and XbaI Polymorphisms in the Estrogen Receptor Alpha Gene in Girls with Central Precocious Puberty: A Pilot Study. BMC Med. Genet. 2018, 19, 84. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Yoon, J.S.; So, C.H.; Kim, K.H.; Hwang, J.S. No Association between Estrogen Receptor Gene Polymorphisms and Premature Thelarche in Girls. Gynecol. Endocrinol. 2017, 33, 816–818. [Google Scholar] [CrossRef] [PubMed]
- Waxman, D.J.; Attisano, C.; Guengerich, F.P.; Lapenson, D.P. Human Liver Microsomal Steroid Metabolism: Identification of the Major Microsomal Steroid Hormone 6β-Hydroxylase Cytochrome P-450 Enzyme. Arch. Biochem. Biophys. 1988, 263, 424–436. [Google Scholar] [CrossRef] [PubMed]
- Daly, A.K. Significance of the Minor Cytochrome P450 3A Isoforms. Clin. Pharm. 2006, 45, 13–31. [Google Scholar] [CrossRef]
- Kadlubar, F.F.; Berkowitz, G.S.; Delongchamp, R.R.; Wang, C.; Green, B.L.; Tang, G.; Lamba, J.; Schuetz, E.; Wolff, M.S. The CYP3A4*1B Variant Is Related to the Onset of Puberty, a Known Risk Factor for the Development of Breast Cancer. Cancer Epidemiol. Biomark. Prev. 2003, 12, 327–331. [Google Scholar]
- Xin, X.; Luan, X.; Xiao, J.; Wei, D.; Wang, J.; Lu, D.; Yang, S. Association Study of Four Activity SNPs of CYP3A4 with the Precocious Puberty in Chinese Girls. Neurosci. Lett. 2005, 381, 284–288. [Google Scholar] [CrossRef]
- Lee, H.S.; Kim, K.H.; Hwang, J.S. Association of Aromatase (TTTA)n Repeat Polymorphisms with Central Precocious Puberty in Girls. Clin. Endocrinol. 2014, 81, 395–400. [Google Scholar] [CrossRef]
- Su, P.-H.; Yang, S.-F.; Yu, J.-S.; Chen, S.-J.; Chen, J.-Y. Study of Leptin Levels and Gene Polymorphisms in Patients with Central Precocious Puberty. Pediatr. Res. 2012, 71, 361–367. [Google Scholar] [CrossRef]
- Zhang, Y.; Chua, S. Leptin Function and Regulation. In Comprehensive Physiology; Terjung, R., Ed.; Wiley: Hoboken, NJ, USA, 2017; pp. 351–369. ISBN 978-0-470-65071-4. [Google Scholar]
- Münzberg, H.; Morrison, C.D. Structure, Production and Signaling of Leptin. Metabolism 2015, 64, 13–23. [Google Scholar] [CrossRef]
- Gueorguiev, M.; Góth, M.I.; Korbonits, M. Leptin and Puberty: A Review. Pituitary 2001, 4, 79–86. [Google Scholar] [CrossRef]
- Moore, L.D.; Le, T.; Fan, G. DNA Methylation and Its Basic Function. Neuropsychopharmacology 2013, 38, 23–38. [Google Scholar] [CrossRef] [PubMed]
- Mattei, A.L.; Bailly, N.; Meissner, A. DNA Methylation: A Historical Perspective. Trends Genet. 2022, 38, 676–707. [Google Scholar] [CrossRef] [PubMed]
- Meng, H.; Cao, Y.; Qin, J.; Song, X.; Zhang, Q.; Shi, Y.; Cao, L. DNA Methylation, Its Mediators and Genome Integrity. Int. J. Biol. Sci. 2015, 11, 604–617. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.A.; Kaiser, U.B. Genetics in Endocrinology: Genetic Etiologies of Central Precocious Puberty and the Role of Imprinted Genes. Eur. J. Endocrinol. 2020, 183, R107–R117. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Lupski, J.R. Non-Coding Genetic Variants in Human Disease. Hum. Mol. Genet. 2015, 24, R102–R110. [Google Scholar] [CrossRef]
- Klein, D.A.; Emerick, J.E.; Sylvester, J.E.; Vogt, K.S. Disorders of Puberty: An Approach to Diagnosis and Management. Am. Fam. Physician 2017, 96, 590–599. [Google Scholar]
- Leka-Emiri, S.; Chrousos, G.P.; Kanaka-Gantenbein, C. The Mystery of Puberty Initiation: Genetics and Epigenetics of Idiopathic Central Precocious Puberty (ICPP). J. Endocrinol. Investig. 2017, 40, 789–802. [Google Scholar] [CrossRef]
- Léger, J. Assistance Publique-Hôpitaux de Paris, Hôpital Robert Debré, Service d’Endocrinologie Diabétologie Pédiatrique, Centre de Référence des Maladies Endocriniennes Rares de la Croissance, F-75019 Paris, France; Université Paris Diderot, Sorbonne Paris Cité, F-75019 Paris, France; Institut National de la Santé et de la Recherche Médicale (Inserm), Unité 1141, DHU Protect, F-75019 Paris, France Central Precocious Puberty-Management and Long-Term Outcomes. Eur. Endocrinol. 2015, 11, 45. [Google Scholar] [CrossRef]
- Bianco, S.D.C. A Potential Mechanism for the Sexual Dimorphism in the Onset of Puberty and Incidence of Idiopathic Central Precocious Puberty in Children: Sex-Specific Kisspeptin as an Integrator of Puberty Signals. Front. Endocrin. 2012, 3, 149. [Google Scholar] [CrossRef]
- Pita, J.; Barrios, V.; Gavela-Pérez, T.; Martos-Moreno, G.Á.; Muñoz-Calvo, M.T.; Pozo, J.; Rovira, A.; Argente, J.; Soriano-Guillén, L. Circulating Kisspeptin Levels Exhibit Sexual Dimorphism in Adults, Are Increased in Obese Prepubertal Girls and Do Not Suffer Modifications in Girls with Idiopathic Central Precocious Puberty. Peptides 2011, 32, 1781–1786. [Google Scholar] [CrossRef]
- Matsuzaki, C.N.; Júnior, J.M.S.; Damiani, D.; de Azevedo Neto, R.S.; Carvalho, K.C.; de Holanda, F.S.; Stafuzza, E.M.; Almeida, J.A.M.; Baracat, E.C. Are CYP1A1, CYP17 and CYP1B1 Mutation Genes Involved on Girls with Precocious Puberty? A Pilot Study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 181, 140–144. [Google Scholar] [CrossRef] [PubMed]
| Gene | Polymorphism Position | Major/Minor Allele | DbSNP ID | Location | Expression | Study | Country | Comments |
|---|---|---|---|---|---|---|---|---|
| KISS1 | 54650055 * | G/T | - | Exon 3 | 110th aminoacid p.P110T | Luan et al. [20] Ko et al. [16] | China (Han) Korea | Statistical correlation with CPP (p-value = 0.025) Significantly protective role (p-value = 0.022) |
| 55648184 | C/G | rs1132506 | Exon 3 | 3′-UTR | Li et al. [17] Rhie et al. [18] | China (Han) Korea | Significant association with early puberty in A, D a More common among patients than controls (p-value = 0.017) | |
| 204196482 | A/- | rs5780218 | 5′-UTR | Li et al. [17] | China (Han) | Significant association with early puberty in A, D, and R a | ||
| 55648186 | -/T | rs35128240 | Exon 3 | 3′-UTR | Rhie et al. [18] | Korea | More common among patients than controls (p-value = 0.044) | |
| KISS1R | 855765 | A/G | - | Promoter region | 5′-UTR | Luan et al. [21] | China (Han) | Statistical correlation with CPP (p-value = 0.037) |
| c.1091 | T/A | rs3050132 | Exon 5 | Codon 364 p.Leu364His | Ghaemi et al. [22] Oh Y.J. et al. [23] | Iran Korea | p.Leu364His (no statistical research) was present in 64% of all cases Significantly more common in D a Significantly more frequent among CPP patients (p = 0.031) | |
| c.738 + 64 | G/T | rs350131 | Intron 4 | Oh Y.J. et al. [23] | Korea | CPP more common in R a (p = 0.006). Significantly higher allele frequencies in CPP patients than in controls (p-value = 0.023) | ||
| PLCB1 | 8883556 | A/G | rs708910 | 3′ UTR | Li et al. [17] | China (Han) | Significantly associated with early puberty in R a | |
| MKRN3 | c.1018 | T/G | - | C3HC4 Ring motif | p.C340G | Settas et al. [28] | Greece | The missense variant, a probable damaging mutation, was present in both siblings affected by CPP, following an imprinted mode of inheritance. |
| FSHβ | 30230078 | T/C | rs639403 | Untranslated region, not regulatory | Zhao et al. [15] | China | Weak correlation with CPP (p-value = 0.025) | |
| LIN28B | chr6:105080213 | A/T | rs221634 | 3′ UTR | Chen et al. [47] | Taiwan | Significant correlation with CPP in D a | |
| 6:104960124 | A/C | rs314276 | 3′ UTR | Chen et al. [47] Hu et al. [48] Ong et al. [46] | Taiwan United Kingdom | Significant correlation with CPP in D, R a No statistical significance after adjusting for multiple testing Association with earlier breast development, 0.12-years-earlier menarche and shorter final height. | ||
| A/C | rs4946651/rs369065 | 5′ region to intron 2 | Park et al. [45] | Korea | ||||
| TAC3 | G/C | A63P mutant | Xin et al. [57] | China | Significantly more common among patients compared with controls (p = 0.024) |
| Gene | Polymorphism Position | Major/Minor Allele | DbSNP ID | Location | Expression | Study | Country | Comments |
|---|---|---|---|---|---|---|---|---|
| KISS1 | 54650055 * | G/T | - | Exon 3 | 110th aminoacid p.P110T | Ko et al. [16] Luan et al. [20] | China (Han) Korea | Significantly protective role (p-value = 0.022) Statistical correlation with CPP (p-value = 0.025) |
| 55648176 | T/G | - | Exon 3 | Rhie et al. [18] | Korea | Significantly protective role (p-value= 0.030) | ||
| NPVF | 7:25226954 (GRCh38) 7:25266573 (GRCh37) | TAA>- | rs3216928 | Exon 2 | c.212_214del | Lima et al. [42] | Brazil | Significanly lower probability of CPP (OR = 0.33; 95% CI = 0.08–0.88) |
| LIN28B | 104931079 | T/C | rs7759938 * | 3′ UTR | Hu et al. [48] | China (Han) | Decreased risk of CPP with the CC genotype. Significant association to CPP in both A a and R a (after adjusting for multiple testing) | |
| 104952962 | G/A C/T | rs314280 * | Intron | Hu et al. [48] Chou et al. [49] | China (Han) Taiwan | Significant association to CPP in both A, R a. (after adjusting for multiple testing). Minor allele phenotype (AA) was protective from CPP Not statistically significant correlation (p-value = 0.1045) | ||
| A/C | rs4946651/rs369065 | Intron 2 | 5′ region to intron 2 | Park et al. [45] | Korea | Significantly less common among CPP patients. Non-A/C haplotypes associated with CPP. | ||
| IRS-1 | IRS-1 R972 | Xin et al. [54] | China | Significantly more common among controls (2.6%) compared with patients (0.6%) (p-value = 0.043) |
| Gene | Haplotype | Study | p-Value |
|---|---|---|---|
| KISS1 | GGA * | Li et al. [17] | 0.005 |
| GGGC–ACCC * | Rhie et al. [18] | 0.024 | |
| KISS1R | CAGTGTC | Oh YJ et al. [23] | 0.042 |
| LHβ | GCAAA | Zhao et al. [15] | 7.77 × 10−4 |
| GCGGT * | Zhao et al. [15] | 4.67 × 10−6 | |
| CCAAA * | Zhao et al. [15] | 1.21 × 10−4 | |
| CYP19A1 | (TTTA)13 | Lee et al. [67] | 0.033 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toutoudaki, K.; Paltoglou, G.; Papadimitriou, D.T.; Eleftheriades, A.; Tsarna, E.; Christopoulos, P. The Role of SNPs in the Pathogenesis of Idiopathic Central Precocious Puberty in Girls. Children 2023, 10, 450. https://doi.org/10.3390/children10030450
Toutoudaki K, Paltoglou G, Papadimitriou DT, Eleftheriades A, Tsarna E, Christopoulos P. The Role of SNPs in the Pathogenesis of Idiopathic Central Precocious Puberty in Girls. Children. 2023; 10(3):450. https://doi.org/10.3390/children10030450
Chicago/Turabian StyleToutoudaki, Konstantina, George Paltoglou, Dimitrios T. Papadimitriou, Anna Eleftheriades, Ermioni Tsarna, and Panagiotis Christopoulos. 2023. "The Role of SNPs in the Pathogenesis of Idiopathic Central Precocious Puberty in Girls" Children 10, no. 3: 450. https://doi.org/10.3390/children10030450
APA StyleToutoudaki, K., Paltoglou, G., Papadimitriou, D. T., Eleftheriades, A., Tsarna, E., & Christopoulos, P. (2023). The Role of SNPs in the Pathogenesis of Idiopathic Central Precocious Puberty in Girls. Children, 10(3), 450. https://doi.org/10.3390/children10030450








