The Mother-Baby Bond: Role of Past and Current Relationships
Abstract
1. Introduction
2. Materials and Methods
2.1. Structured Clinical Interview
2.2. Edinburgh Postnatal Depression Scale
2.3. Parental Bonding Instrument
2.4. Relationship Questionnaire
2.5. State-Trait Anxiety Inventory (STAI)
2.6. Dyadic Adjustment Scale (DAS)
2.7. Maternal Foetal Attachment Scale (MFAS)
2.8. Mother-to-Infant Bonding Scale (MIBS)
2.9. Statistical Analyses
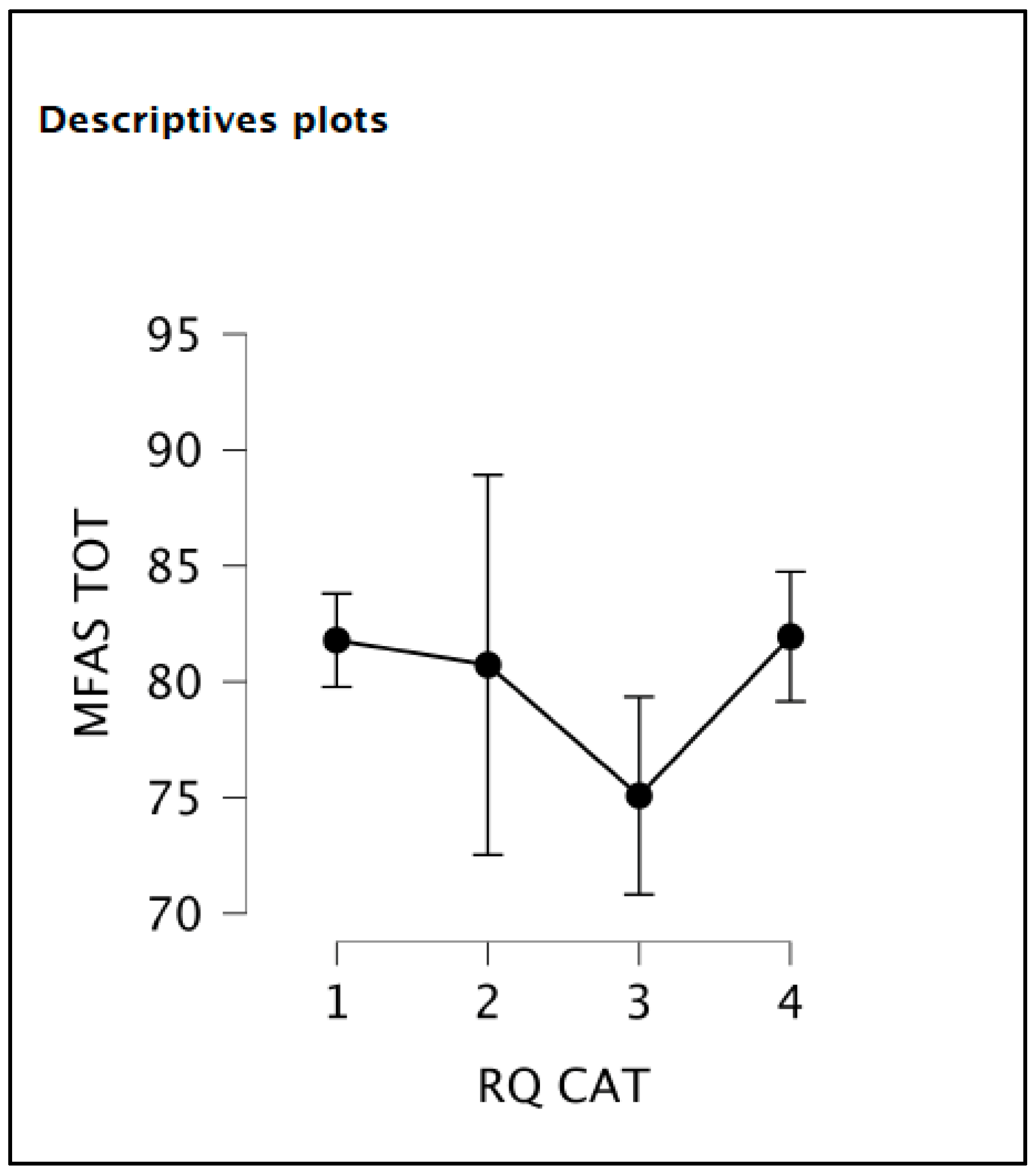
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fernandez Arias, P.; Yoshida, K.; Brockington, I.F.; Kernreiter, J.; Klier, C.M. Foetal abuse. Arch. Womens Ment. Health 2019, 22, 569–573. [Google Scholar] [CrossRef]
- Maguire, J.; McCormack, C.; Mitchell, A.; Monk, C. Neurobiology of maternal mental illness. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Kohlhoff, J.; Barnett, B. Parenting self-efficacy: Links with maternal depression, infant behaviour and adult attachment. Early Hum. Dev. 2013, 89, 249–256. [Google Scholar] [CrossRef]
- Brandon, A.R.; Pitts, S.; Denton, W.H.; Stringer, C.A.; Evans, H.M. History of the Theory of Prenatal Attachment. J. Prenat. Perinat. Psychol. Health 2009, 23, 201–222. [Google Scholar]
- Bianciardi, E.; Barone, Y.; Lo Serro, V.; De Stefano, A.; Giacchetti, N.; Aceti, F.; Niolu, C. Inflammatory markers of perinatal depression in women with and without history of trauma. Riv. Psichiatr. 2021, 56, 237–245. [Google Scholar]
- Niarchou, M.; Zammit, S.; Lewis, G. The Avon Longitudinal Study of Parents and Children (ALSPAC) birth cohort as a resource for studying psychopathology in childhood and adolescence: A summary of findings for depression and psychosis. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 1017–1027. [Google Scholar] [CrossRef]
- Kuboshita, R.; Fujisawa, T.X.; Makita, K.; Kasaba, R.; Okazawa, H.; Tomoda, A. Intrinsic brain activity associated with eye gaze during mother–child interaction. Sci. Rep. 2020, 10, 18903. [Google Scholar] [CrossRef]
- Crowell, J. Editorial: Maternal Bonding: How and Why Does It Matter? J. Am. Acad. Child Adolesc. Psychiatry 2022, 61, 751–753. [Google Scholar] [CrossRef]
- Hillerer, K.M.; Jacobs, V.R.; Fischer, T.; Aigner, L. The maternal brain: An organ with peripartal plasticity. Neural Plast. 2014, 2014, 574159. [Google Scholar] [CrossRef]
- Bartels, A.; Zeki, S. The neural correlates of maternal and romantic love. Neuroimage 2004, 21, 1155–1166. [Google Scholar] [CrossRef]
- Zhang, L.; Wang, L.; Yuan, Q.; Huang, C.; Cui, S.; Zhang, K.; Zhou, X. The mediating role of prenatal depression in adult attachment and maternal-fetal attachment in primigravida in the third trimester. BMC Pregnancy Childbirth 2021, 21, 307. [Google Scholar] [CrossRef]
- Petri, E.; Palagini, L.; Bacci, O.; Borri, C.; Teristi, V.; Corezzi, C.; Faraoni, S.; Antonelli, P.; Cargioli, C.; Banti, S.; et al. Maternal–foetal attachment independently predicts the quality of maternal–infant bonding and post-partum psychopathology. J. Matern. Neonatal Med. 2018, 31, 3153–3159. [Google Scholar] [CrossRef]
- O’Donnell, K.J.; Meaney, M.J. Fetal origins of mental health: The developmental origins of health and disease hypothesis. Am. J. Psychiatry 2017, 174, 319–328. [Google Scholar] [CrossRef]
- Briana, D.D.; Malamitsi-Puchner, A. Developmental origins of adult health and disease: The metabolic role of BDNF from early life to adulthood. Metabolism 2018, 81, 45–51. [Google Scholar] [CrossRef]
- Brummelte, S. Introduction: Early adversity and brain development. Neuroscience 2017, 342, 1–3. [Google Scholar] [CrossRef]
- McMahon, C.; Trapolini, T.; Barnett, B. Maternal state of mind regarding attachment predicts persistence of postnatal depression in the preschool years. J. Affect. Disord. 2008, 107, 199–203. [Google Scholar] [CrossRef]
- Branchi, I.; Cirulli, F. Early experiences: Building up the tools to face the challenges of adult life. Dev. Psychobiol. 2014, 56, 1661–1674. [Google Scholar] [CrossRef]
- Bergman, K.; Sarkar, P.; Glover, V.; O’Connor, T.G. Maternal Prenatal Cortisol and Infant Cognitive Development: Moderation by Infant-Mother Attachment. Biol. Psychiatry 2010, 67, 1026–1032. [Google Scholar] [CrossRef]
- Seedat, S. Paternal perinatal mental disorders are inextricably linked to maternal and child morbidity. World Psychiatry 2020, 19, 337–338. [Google Scholar] [CrossRef]
- Alderdice, F. Supporting psychological well-being around the time of birth: What can we learn from maternity care? World Psychiatry 2020, 19, 332–333. [Google Scholar] [CrossRef]
- Benvenuti, P.; Ferrara, M.; Niccolai, C.; Valoriani, V.; Cox, J.L. The Edinburgh Postnatal Depression Scale: Validation for an Italian sample. J. Affect. Disord. 1999, 53, 137–141. [Google Scholar] [CrossRef]
- Parker, G.; Tupling, H.; Brown, L. A parental bonding instrument. Br. J. Med. Psychol. 1979, 52, 1–10. [Google Scholar] [CrossRef]
- Niolu, C.; Bianciardi, E.; Di Lorenzo, G.; Nicolai, S.; Celi, M.; Ribolsi, M.; Pietropolli, A.; Ticconi, C.; Tarantino, U.; Siracusano, A. Insecure attachment style predicts low bone mineral density in postmenopausal women. A pilot study. Riv. Psichiatr 2016, 51, 143–148. [Google Scholar]
- D’Argenio, A.; Mazzi, C.; Pecchioli, L.; Di Lorenzo, G.; Siracusano, A.; Troisi, A. Early trauma and adult obesity: Is psychological dysfunction the mediating mechanism? Physiol. Behav. 2009, 98, 543–546. [Google Scholar] [CrossRef]
- Ramanaiah, N.V.; Franzen, M.; Schill, T. A Psychometric Study of the State-Trait Anxiety inventory. J. Personal. Assess. 1983, 47, 531–535. [Google Scholar] [CrossRef]
- Spanier, G.B. Measuring Dyadic Adjustment: New Scales for Assessing the Quality of Marriage and Similar Dyads. J. Marriage Fam. 1976, 38, 15. [Google Scholar] [CrossRef]
- Busonera, A.; Cataudella, S.; Lampis, J.; Tommasi, M.; Zavattini, G.C. Psychometric properties of a 20-item version of the Maternal-Fetal Attachment Scale in a sample of Italian expectant women. Midwifery 2016, 34, 79–87. [Google Scholar] [CrossRef]
- Taylor, A.; Atkins, R.; Kumar, R.; Adams, D.; Glover, V. A new mother-to-infant bonding scale: Links with early maternal mood. Arch. Womens Ment. Health 2005, 8, 45–51. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioural Science, 2nd ed.; Taylor Francis: Abingdon, UK, 1988. [Google Scholar]
- Craig, M.; Howard, L. Postnatal depression. BMJ Clin. Evid. 2009, 2009, 1407. [Google Scholar]
- Khanlari, S.; Barnett Am, B.; Ogbo, F.A.; Eastwood, J. Re-examination of perinatal mental health policy frameworks for women signalling distress on the Edinburgh Postnatal Depression Scale (EPDS) completed during their antenatal booking-in consultation: A call for population health intervention. BMC Pregnancy Childbirth 2019, 19, 221. [Google Scholar] [CrossRef]
- Smythe, K.L.; Petersen, I.; Schartau, P. Prevalence of Perinatal Depression and Anxiety in Both Parents. JAMA Netw. Open 2002, 5, e2218969. [Google Scholar] [CrossRef]
- Fredriksen, E.; von Soest, T.; Smith, L.; Moe, V. Depressive symptom contagion in the transition to parenthood: Interparental processes and the role of partner-related attachment. J. Abnorm. Psychol. 2019, 128, 397–403. [Google Scholar] [CrossRef]
- Robakis, T.K.; Zhang, S.; Rasgon, N.L.; Li, T.; Wang, T.; Roth, M.C.; Humphreys, K.L.; Gotlib, I.H.; Ho, M.; Khechaduri, A.; et al. Epigenetic signatures of attachment insecurity and childhood adversity provide evidence for role transition in the pathogenesis of perinatal depression. Transl. Psychiatry 2020, 10, 48. [Google Scholar] [CrossRef]
- Zaki, N.; Ruiz-Ruano García, A.M.; López Puga, J. Attachment style and prenatal expectations from a Bayesian perspective. Psicothema 2019, 32, 138–144. [Google Scholar]
- Røhder, K.; Væver, M.S.; Aarestrup, A.K.; Jacobsen, R.K.; Smith-Nielsen, J.; Schiøtz, M.L. Maternal-fetal bonding among pregnant women at psychosocial risk: The roles of adult attachment style, prenatal parental reflective functioning, and depressive symptoms. PLoS ONE 2020, 15, e0239208. [Google Scholar] [CrossRef]
- Rollè, L.; Giordano, M.; Santoniccolo, F.; Trombetta, T. Prenatal attachment and perinatal depression: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 2644. [Google Scholar] [CrossRef]
- Papapetrou, C.; Panoulis, K.; Mourouzis, I.; Kouzoupis., A. Pregnancy and the perinatal period: The impact of attachment theory. Psychiatriki. 2020, 31, 257–270. [Google Scholar] [CrossRef]
- Kossakowska, K.; Bielawska-Batorowicz, E. Postpartum Depressive Symptoms and Their Selected Psychological Predictors in Breast-, Mixed and Formula-Feeding Mothers. Front. Psychiatry 2022, 13, 20. [Google Scholar] [CrossRef]
- Dubber, S.; Reck, C.; Müller, M.; Gawlik, S. Postpartum bonding: The role of perinatal depression, anxiety and maternal–fetal bonding during pregnancy. Arch. Womens Ment. Health 2015, 18, 187–195. [Google Scholar] [CrossRef]
- Reissland, N.; Froggatt, S.; Reames, E.; Girkin, J. Effects of maternal anxiety and depression on fetal neuro-development. J. Affect. Disord. 2018, 241, 469–474. [Google Scholar] [CrossRef]
- Webb, A.R.; Heller, H.T.; Benson, C.B.; Lahav, A. Mother’s voice and heartbeat sounds elicit auditory plasticity in the human brain before full gestation. Proc. Natl. Acad. Sci. USA 2015, 112, 3152–3157. [Google Scholar] [CrossRef]
- Bianciardi, E.; Vito, C.; Betrò, S.; De Stefano, A.; Siracusano, A.; Niolu, C. The anxious aspects of insecure attachment styles are associated with depression either in pregnancy or in the postpartum period. Ann. Gen. Psychiatry 2020, 19, 51. [Google Scholar] [CrossRef]
- Karbowa-Płowens, M. John Bowlby and Attachment Theory. In Encyclopedia of Evolutionary Psychological Science; Springer: Berlin/Heidelberg, Germany, 2019. [Google Scholar]
- Wilhelm, K. Parental Bonding and Adult Attachment Style: The Relationship between Four Category Models. Int. J. Women’s Heal. Wellness 2016, 2. [Google Scholar] [CrossRef]
- Niolu, C.; Bianciardi, E.; Di Lorenzo, G.; Marchetta, C.; Barone, Y.; Sterbini, N.; Ribolsi, M.; Reggiardo, G.; Siracusano, A. Enhancing adherence, subjective well-being and quality of life in patients with schizophrenia: Which role for long-acting risperidone? Ther. Adv. Psychopharmacol. 2015, 5, 278–288. [Google Scholar] [CrossRef]
- Niolu, C.; Barone, Y.; Bianciardi, E.; Ribolsi, M.; Marchetta, C.; Robone, C.; Ambrosio, A.; Sarchiola, L.; Reggiardo, G.; Di Lorenzo, G.; et al. Predictors of poor adherence to treatment in inpatients with bipolar and psychotic spectrum disorders. Riv. Psichiatr 2015, 50, 285–294. [Google Scholar]
- Gentile, S.; Fusco, M.L. Untreated perinatal paternal depression: Effects on offspring. Psychiatry Res. 2017, 252, 325–332. [Google Scholar] [CrossRef]
- Jannini, T.B.; Lorenzo, G.D.; Bianciardi, E.; Niolu, C.; Toscano, M.; Ciocca, G.; Jannini, E.A.; Siracusano, A. Off-label Uses of Selective Serotonin Reuptake Inhibitors (SSRIs). Curr. Neuropharmacol. 2021, 20, 693–712. [Google Scholar] [CrossRef]
- Stephenson, L.A.; Macdonald, A.J.D.; Seneviratne, G.; Waites, F.; Pawlby, S. Mother and Baby Units matter: Improved outcomes for both. BJPsych Open 2018, 4, 119–125. [Google Scholar] [CrossRef]
- NICE. Antenatal and postnatal mental health: Clinical management and service guidance. Essent. MIDIRS 2015, 6, 14. [Google Scholar]
| Variable | Value | N | % |
|---|---|---|---|
| Mean age yrs (range) SD | 32.0 (18–46) SD = 5.30 | ||
| Education | |||
| Primary school | 1 | 0.8 | |
| Junior high school | 22 | 18.5 | |
| High school | 58 | 48.8 | |
| Bachelors degree/Post graduate | 38 | 31.9 | |
| Couple relationship | |||
| Single/separated/divorced | 3 | 2.5 | |
| Married/cohabiting | 116 | 97.5 | |
| Occupation | |||
| Unemployed | 41 | 34.5 | |
| Employed full/part time | 78 | 65.5 |
| Variable | Value | N | % |
|---|---|---|---|
| EPDS | |||
| <12 | 103 | 86.7 | |
| ≥12 | 16 | 13.3 | |
| RQ | |||
| Secure | 65 | 54.6 | |
| Preoccupied | 7 | 5.9 | |
| Fearful-Avoidant | 14 | 11.8 | |
| Dismissing-Avoidant | 33 | 27.7 | |
| PBI Mother Care | |||
| >27 | 45 | 37.8 | |
| <26 | 74 | 62.2 | |
| PBI Mother Protection | |||
| <13 | 64 | 53.7 | |
| >13 | 55 | 46.2 | |
| PBI Father Care | |||
| <23 | 44 | 37.0 | |
| >24 | 75 | 63.0 | |
| PBI Father Protection | |||
| <12 | 53 | 44.5 | |
| >12.5 | 66 | 55.5 | |
| PBI Mother | |||
| Affectionate constraint | 27 | 22.7 | |
| Affectionate control | 29 | 24.4 | |
| Optimal parenting | 48 | 40.3 | |
| Neglectful parenting | 15 | 12.6 | |
| PBI Father | |||
| Affectionate constraint | 34 | 28.6 | |
| Affectionate control | 32 | 26.9 | |
| Optimal parenting | 41 | 34.4 | |
| Neglectful parenting | 12 | 10.1 | |
| Breastfeeding at 1st month (N = 118) | No 49 | ||
| Yes 69 | 3 | 2.5 | |
| Breastfeeding at 3rd month (N = 117) | No 70 | ||
| Yes 47 | 4 | 3.3 | |
| Breastfeeding at 6th month (N = 116) | No 83 | ||
| Yes 33 |
| Cases | Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| RQ CAT Residuals | 560.691 7277.173 | 3 114 | 186.897 63.835 | 2.928 | 0.037 |
| N | r | p | ||
|---|---|---|---|---|
| MFAS TOT |
| 118 | −0.150 | 0.106 |
| MFAS TOT |
| 117 | 0.182 * | 0.049 |
| MFAS TOT |
| 118 | 0.069 | 0.458 |
| MFAS TOT |
| 118 | 0.011 | 0.903 |
| MFAS TOT |
| 118 | 0.044 | 0.633 |
| MFAS TOT |
| 118 | −0.088 | 0.345 |
| MFAS TOT |
| 118 | −0.253 ** | 0.006 |
| MFAS TOT |
| 118 | 0.038 | 0.682 |
| MFAS TOT |
| 118 | 0.053 | 0.572 |
| MFAS TOT |
| 118 | −0.071 | 0.443 |
| MFAS TOT |
| 112 | 0.051 | 0.596 |
| MFAS TOT |
| 112 | −0.128 | 0.180 |
| Test | Statistic | df | p | |
|---|---|---|---|---|
| MFAS TOT | Student | −0.108 | 114.000 | 0.914 |
| Welch | −0.108 | 109.709 | 0.914 | |
| Mann-Whitney | 1707.500 | 0.811 | ||
| AGE | Student | −0.205 | 115.000 | 0.838 |
| Welch | −0.205 | 109.548 | 0.838 | |
| Mann-Whitney | 1662.500 | 0.882 | ||
| DAS TOT | Student | −1.808 | 114.000 | 0.073 |
| Welch | −1.814 | 108.992 | 0.072 | |
| Mann-Whitney | 1320.500 | 0.061 | ||
| EPDS (TOT) | Student | 2.839 | 115.000 | 0.005 |
| Welch | 2.955 | 112.624 | 0.004 | |
| Mann-Whitney | 2133.000 | 0.015 | ||
| STAI Y-1 TOT | Student | 1.442 | 115.000 | 0.152 |
| Welch | 1.474 | 114.919 | 0.143 | |
| Mann-Whitney | 1887.000 | 0.281 | ||
| STAI Y-2 TOT | Student | 1.927 | 115.000 | 0.056 |
| Welch | 1.960 | 114.361 | 0.052 | |
| Mann-Whitney | 1977.500 | 0.115 | ||
| RQ 1 | Student | −0.771 | 115.000 | 0.442 |
| Welch | −0.772 | 109.544 | 0.442 | |
| Mann-Whitney | 1522.500 | 0.352 | ||
| RQ 2 | Student | 1.936 | 115.000 | 0.055 |
| Welch | 1.965 | 113.967 | 0.052 | |
| Mann-Whitney | 2016.500 | 0.064 | ||
| RQ 3 | Student | 0.508 | 115.000 | 0.613 |
| Welch | 0.506 | 107.812 | 0.614 | |
| Mann-Whitney | 1809.000 | 0.504 | ||
| RQ 4 | Student | 1.224 | 115.000 | 0.223 |
| Welch | 1.213 | 105.170 | 0.228 | |
| Mann-Whitney | 1946.000 | 0.156 | ||
| PBI MOTHER CARE | Student | −1.518 | 115.000 | 0.132 |
| Welch | −1.561 | 114.886 | 0.121 | |
| Mann-Whitney | 1473.000 | 0.234 | ||
| PBI MOTHER OVER PROTECTION | Student | 0.616 | 115.000 | 0.539 |
| Welch | 0.624 | 113.839 | 0.534 | |
| Mann-Whitney | 1712.000 | 0.906 | ||
| PBI FATHER CARE | Student | −1.317 | 109.000 | 0.191 |
| Welch | −1.296 | 96.013 | 0.198 | |
| Mann-Whitney | 1230.000 | 0.086 | ||
| PBI FATHER OVERPROTECTION | Student | 1.014 | 109.000 | 0.313 |
| Welch | 1.037 | 108.759 | 0.302 | |
| Mann-Whitney | 1616.000 | 0.566 |
| Test | Statistic | df | p | |
|---|---|---|---|---|
| MFAS TOT | Student | −1.096 | 113.000 | 0.275 |
| Welch | −1.089 | 94.472 | 0.279 | |
| Mann-Whitney | 1430.500 | 0.373 | ||
| AGE | Student | −0.218 | 114.000 | 0.828 |
| Welch | −0.210 | 85.271 | 0.834 | |
| Mann-Whitney | 1609.000 | 0.946 | ||
| DAS TOT | Student | −1.572 | 113.000 | 0.119 |
| Welch | −1.593 | 103.537 | 0.114 | |
| Mann-Whitney | 1363.500 | 0.182 | ||
| EPDS (TOT) | Student | 3.977 | 114.000 | <0.001 |
| Welch | 3.627 | 68.009 | <0.001 | |
| Mann-Whitney | 2199.000 | 0.001 | ||
| STAI Y-1 TOT | Student | 1.544 | 114.000 | 0.125 |
| Welch | 1.434 | 73.570 | 0.156 | |
| Mann-Whitney | 1795.500 | 0.329 | ||
| STAI Y-2 TOT | Student | 1.085 | 114.000 | 0.280 |
| Welch | 1.034 | 81.880 | 0.304 | |
| Mann-Whitney | 1733.500 | 0.530 | ||
| RQ 1 | Student | −0.880 | 114.000 | 0.381 |
| Welch | −0.848 | 85.612 | 0.399 | |
| Mann-Whitney | 1495.500 | 0.473 | ||
| RQ 2 | Student | 1.374 | 114.000 | 0.172 |
| Welch | 1.333 | 88.004 | 0.186 | |
| Mann-Whitney | 1825.000 | 0.237 | ||
| RQ 3 | Student | 1.730 | 114.000 | 0.086 |
| Welch | 1.724 | 97.709 | 0.088 | |
| Mann-Whitney | 1946.000 | 0.061 | ||
| RQ 4 | Student | 1.552 | 114.000 | 0.124 |
| Welch | 1.564 | 101.627 | 0.121 | |
| Mann-Whitney | 1910.500 | 0.100 | ||
| PBI MOTHER CARE | Student | −2.460 | 114.000 | 0.015 |
| Welch | −2.341 | 81.376 | 0.022 | |
| Mann-Whitney | 1234.500 | 0.029 | ||
| PBI MOTHER OVER PROTECTION | Student | 2.076 | 114.000 | 0.040 |
| Welch | 1.974 | 81.256 | 0.052 | |
| Mann-Whitney | 1907.500 | 0.108 | ||
| PBI FATHER CARE | Student | −0.370 | 108.000 | 0.712 |
| Welch | −0.370 | 92.573 | 0.712 | |
| Mann-Whitney | 1402.500 | 0.764 | ||
| PBI FATHER OVERPROTECTION | Student | 1.326 | 108.000 | 0.188 |
| Welch | 1.284 | 81.920 | 0.203 | |
| Mann-Whitney | 1636.000 | 0.262 |
| Test | Statistic | df | p | |
|---|---|---|---|---|
| MFAS TOT | Student | −1.375 | 113.000 | 0.172 |
| Welch | −1.373 | 109.545 | 0.173 | |
| Mann-Whitney | 1404.500 | 0.181 | ||
| AGE | Student | 0.104 | 114.000 | 0.917 |
| Welch | 0.105 | 113.665 | 0.916 | |
| Mann-Whitney | 1720.500 | 0.779 | ||
| DAS TOT | Student | −2.245 | 113.000 | 0.027 |
| Welch | −2.208 | 99.714 | 0.030 | |
| Mann-Whitney | 1237.000 | 0.024 | ||
| EPDS (TOT) | Student | 4.205 | 114.000 | <0.001 |
| Welch | 4.430 | 94.450 | <0.001 | |
| Mann-Whitney | 2306.500 | <0.001 | ||
| STAI Y-1 TOT | Student | 1.826 | 114.000 | 0.070 |
| Welch | 1.881 | 110.655 | 0.063 | |
| Mann-Whitney | 1940.000 | 0.134 | ||
| STAI Y-2 TOT | Student | 1.346 | 114.000 | 0.181 |
| Welch | 1.372 | 113.788 | 0.173 | |
| Mann-Whitney | 1885.000 | 0.233 | ||
| RQ 1 | Student | −0.828 | 114.000 | 0.409 |
| Welch | −0.839 | 113.899 | 0.403 | |
| Mann-Whitney | 1532.500 | 0.442 | ||
| RQ 2 | Student | 1.326 | 114.000 | 0.187 |
| Welch | 1.330 | 111.621 | 0.186 | |
| Mann-Whitney | 1933.000 | 0.131 | ||
| RQ 3 | Student | 2.809 | 114.000 | 0.006 |
| Welch | 2.845 | 113.912 | 0.005 | |
| Mann-Whitney | 2176.000 | 0.004 | ||
| RQ 4 | Student | 0.743 | 114.000 | 0.459 |
| Welch | 0.740 | 109.022 | 0.461 | |
| Mann-Whitney | 1817.500 | 0.408 | ||
| PBI MOTHER CARE | Student | −2.506 | 114.000 | 0.014 |
| Welch | −2.569 | 112.460 | 0.012 | |
| Mann-Whitney | 1270.000 | 0.027 | ||
| PBI MOTHER OVER PROTECTION | Student | 1.627 | 114.000 | 0.107 |
| Welch | 1.659 | 113.657 | 0.100 | |
| Mann-Whitney | 1907.500 | 0.187 | ||
| PBI FATHER CARE | Student | −1.440 | 108.000 | 0.153 |
| Welch | −1.460 | 107.873 | 0.147 | |
| Mann-Whitney | 1288.000 | 0.203 | ||
| PBI FATHER OVERPROTECTION | Student | 0.926 | 108.000 | 0.357 |
| Welch | 0.928 | 105.358 | 0.356 | |
| Mann-Whitney | 1645.500 | 0.383 |
| Model Summary–MFAS TOT. | |||||||||
| Model | R | R² | Adjusted R² | RMSE | R² Change | F Change | df1 | df2 | p |
| 1 | 0.000 | 0.000 | 0.000 | 8.139 | 0.000 | 0 | 110 | ||
| 2 | 0.214 | 0.046 | 0.037 | 7.987 | 0.046 | 5.220 | 1 | 109 | 0.024 |
| ANOVA | |||||||||
| Model | Sum of Squares | df | Mean Square | F | p | ||||
| 2 | Regression | 332.991 | 1 | 332.991 | 5.220 | 0.024 | |||
| Residual | 6952.919 | 109 | 63.788 | ||||||
| Total | 7285.910 | 110 | |||||||
| Coefficients | |||||||||
| Model | Unstandardized | Standard Error | Standardized | t | p | ||||
| 1 | (Intercept) | 81.234 | 0.772 | 105.161 | <0.001 | ||||
| 2 | (Intercept) | 83.971 | 1.418 | 59.234 | <0.001 | ||||
| RQ 3 | −0.999 | 0.437 | −0.214 | −2.285 | 0.024 | ||||
| Variable | Beta (a) | 95%CI | SE | p |
|---|---|---|---|---|
| EPDS TOT | 0.243 | (0.003–0.022) | 0.005 | 0.008 |
| STAI Y-1 | 0.185 | (0.002–0.009) | 0.002 | 0.046 |
| STAI Y-2 | 0.304 | (0.004–0.014) | 0.003 | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bianciardi, E.; Ongaretto, F.; De Stefano, A.; Siracusano, A.; Niolu, C. The Mother-Baby Bond: Role of Past and Current Relationships. Children 2023, 10, 421. https://doi.org/10.3390/children10030421
Bianciardi E, Ongaretto F, De Stefano A, Siracusano A, Niolu C. The Mother-Baby Bond: Role of Past and Current Relationships. Children. 2023; 10(3):421. https://doi.org/10.3390/children10030421
Chicago/Turabian StyleBianciardi, Emanuela, Francesca Ongaretto, Alberto De Stefano, Alberto Siracusano, and Cinzia Niolu. 2023. "The Mother-Baby Bond: Role of Past and Current Relationships" Children 10, no. 3: 421. https://doi.org/10.3390/children10030421
APA StyleBianciardi, E., Ongaretto, F., De Stefano, A., Siracusano, A., & Niolu, C. (2023). The Mother-Baby Bond: Role of Past and Current Relationships. Children, 10(3), 421. https://doi.org/10.3390/children10030421






