Diametaphyseal Distal Forearm Fractures in Children: A STROBE Compliant Comparison of Outcomes of Different Stabilization Techniques Regarding Complications
Abstract
1. Introduction
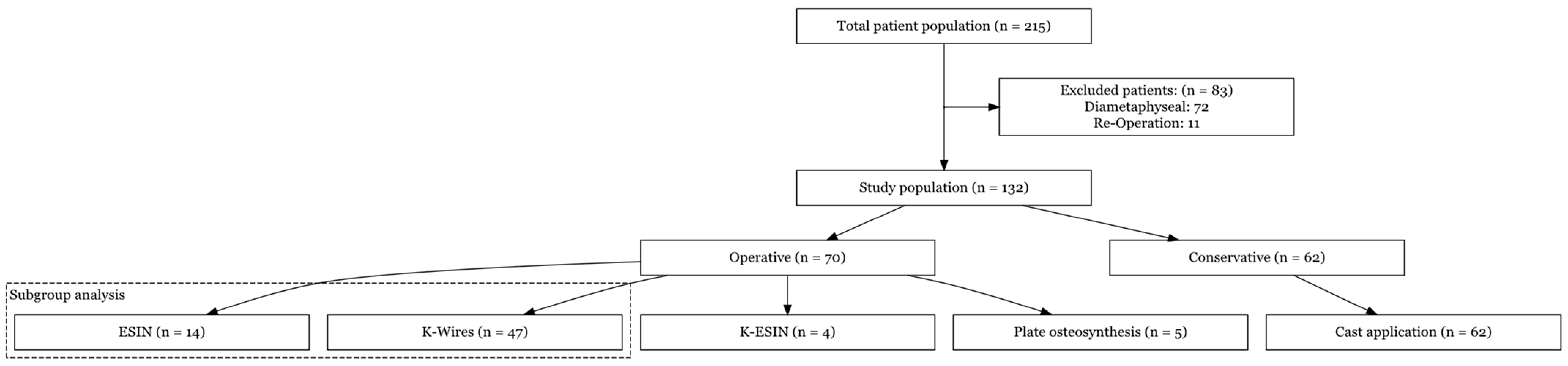
2. Materials and Methods
2.1. Study Design
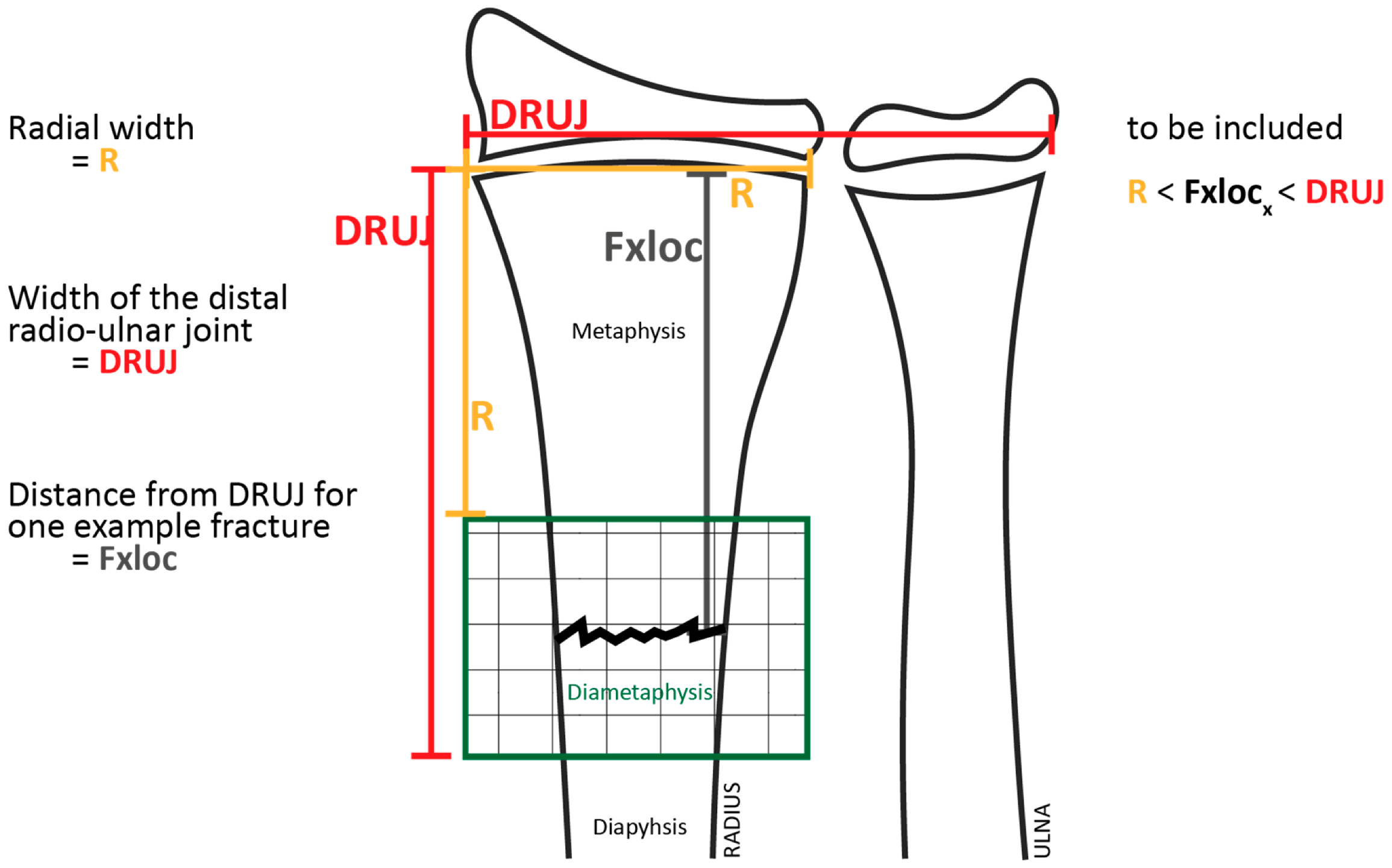
2.2. Measurements
2.3. Additional Analyses
2.4. Statistical Methods
3. Results
3.1. Patient Characteristics
3.2. Fracture Mechanism/Type
3.3. Type of Stabilization
3.4. Primary Analysis (Surgical vs. Conservative Treatment)
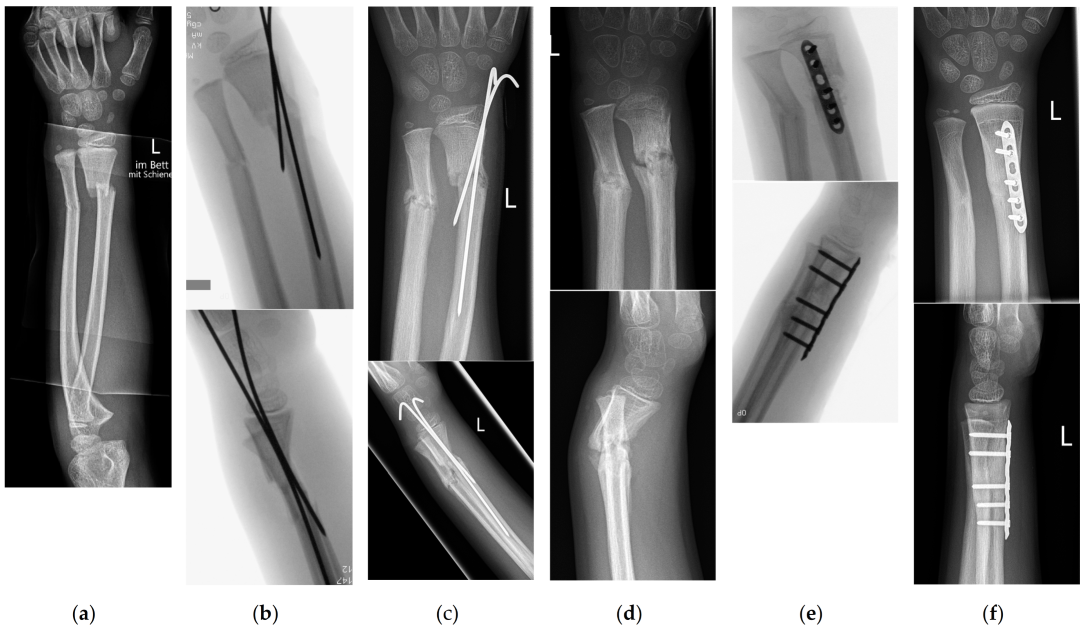
3.5. Subgroup Analysis (Conservative vs. ESIN vs. K-Wire Fixation)
3.5.1. Complications
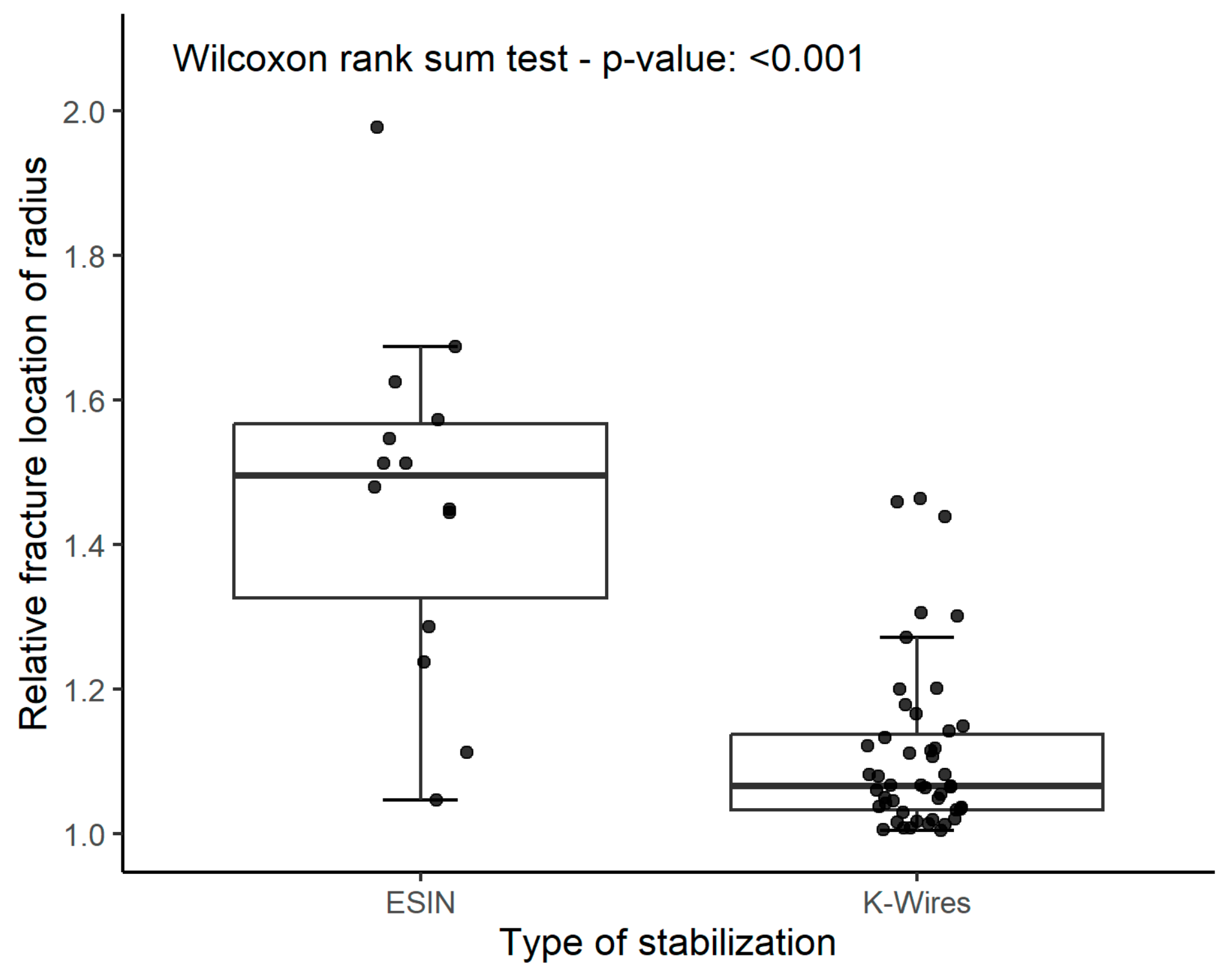
3.5.2. Secondary Radiologic Parameters/Parameters Potentially Influencing Stability after Reduction of Fracture
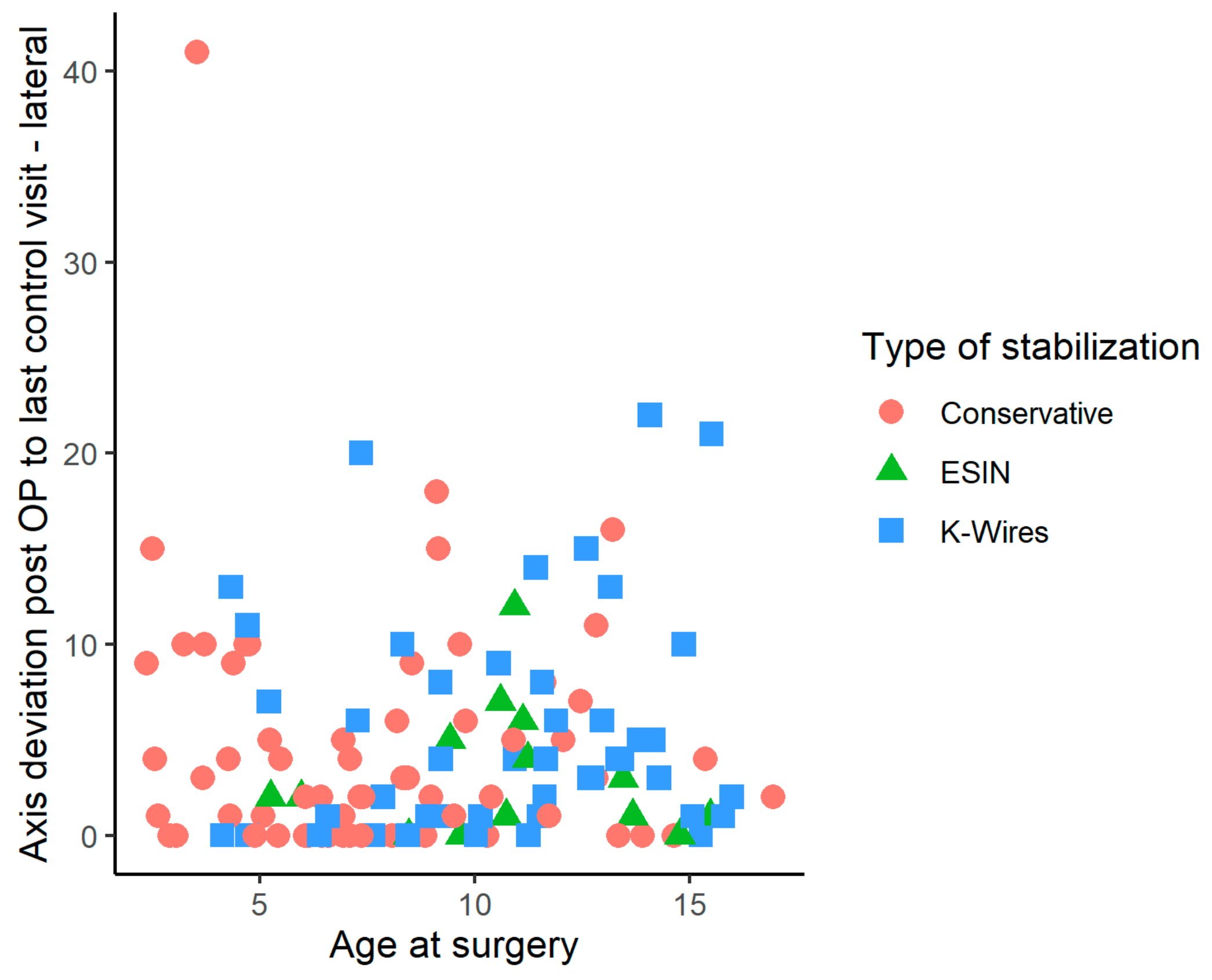
3.5.3. Residual Axis Malalignment
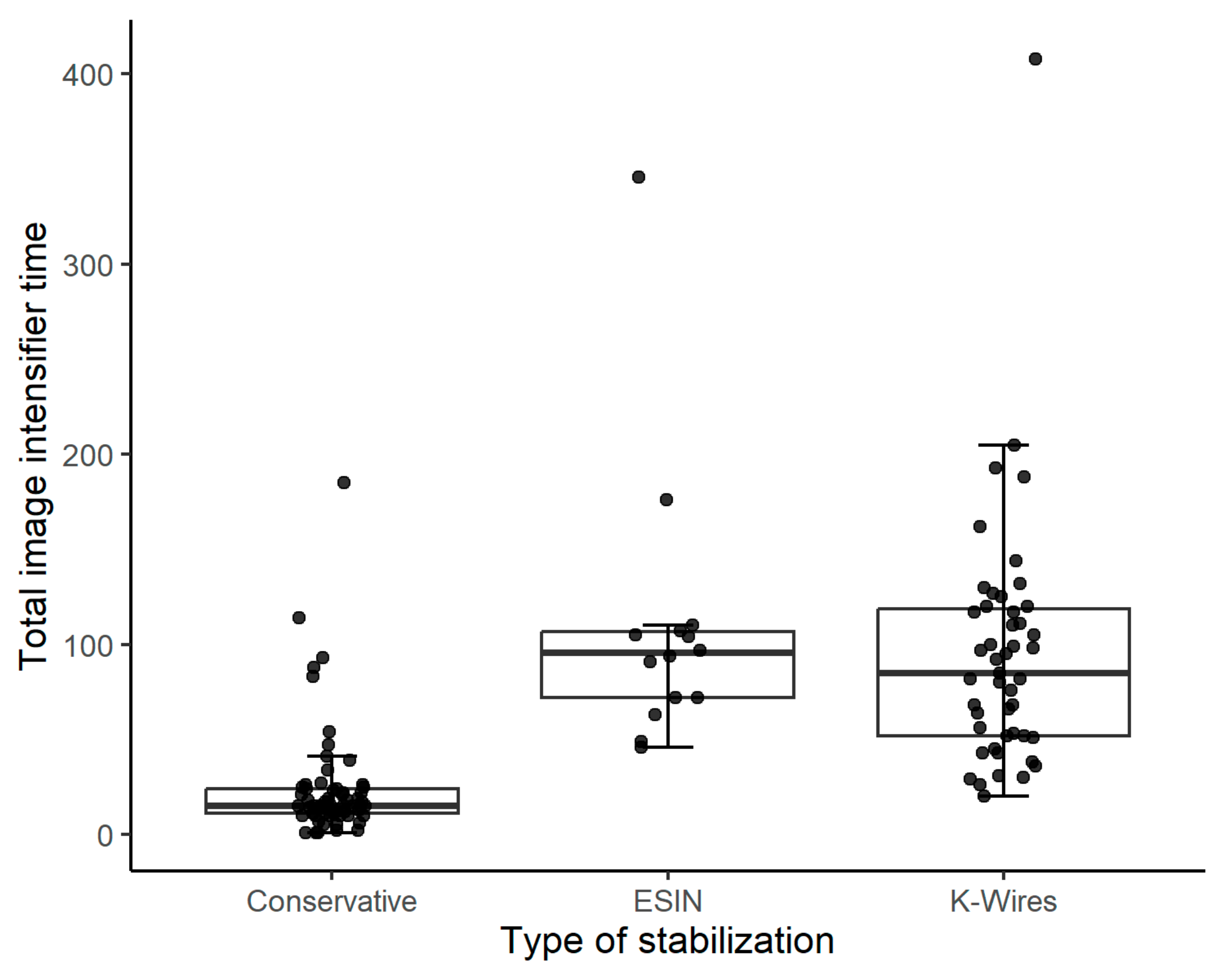
3.5.4. Total Time of Exposure to Image Intensifier Radiation
3.5.5. Choice of Treatment Relative to Fracture Location
3.6. Revision Interventions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AP/PA | Anterior-posterior/posterior-anterior |
| CR | Closed reduction |
| DESIN | Dorsally inserted elastic stable intramedullary nail |
| ESIN | Elastic-stable intramedullary nailing |
| IQR | Interquartile range |
| K-ESIN | Intramedullary K-wires in ESIN technique |
| K-wire(s) | Kirschner wire(s) |
| LOS | Length of stay |
| RFL | Relative fracture location |
| ROM | Range of motion |
| SESIN | Short elastic stable intramedullary nail |
| SD | Standard deviation |
| STROBE | Acronym for “Strengthening the reporting of observational studies in epidemiology” (STROBE) statement |
| UKBB | University Children’s Hospital Basel (Universitäts-Kinderspital beider Basel), Basel, Switzerland |
References
- Joeris, A.; Lutz, N.; Wicki, B.; Slongo, T.; Audigé, L. An epidemiological evaluation of pediatric long bone fractures—A retrospective cohort study of 2716 patients from two Swiss tertiary pediatric hospitals. BMC Pediatr. 2014, 14, 314. [Google Scholar] [CrossRef] [PubMed]
- Lempesis, V.; Jerrhag, D.; Rosengren, B.E.; Landin, L.; Tiderius, C.J.; Karlsson, M.K. Pediatric Distal Forearm Fracture Epidemiology in Malmö, Sweden—Time Trends During Six Decades. J. Wrist Surg. 2019, 8, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Jerrhag, D.; Englund, M.; Karlsson, M.K.; Rosengren, B.E. Epidemiology and time trends of distal forearm fractures in adults—A study of 11.2 million person-years in Sweden. BMC Musculoskelet. Disord. 2017, 18, 240. [Google Scholar] [CrossRef] [PubMed]
- Marzi, I. Kindertraumatologie, 3rd ed.; Springer: Berlin/Heidelberg, Germany, 2016; p. 570. [Google Scholar]
- Sinikumpu, J.J.; Nietosvaara, Y. Treatment of Distal Forearm Fractures in Children. Scand. J. Surg. 2021, 110, 276–280. [Google Scholar] [CrossRef]
- Pavone, V.; Vescio, A.; Lucenti, L.; Chisari, E.; Canavese, F.; Testa, G. Analysis of loss of reduction as risk factor for additional secondary displacement in children with displaced distal radius fractures treated conservatively. Orthop. Traumatol. Surg. Res. 2020, 106, 193–198. [Google Scholar] [CrossRef]
- Persiani, P.; Martini, L.; Calogero, V.; Giannini, E.; Speziale Varsamis, T.; Mazza, O.; Crostelli, M.; Mascello, D.; De Meo, D.; Villani, C. Analysis of the risk of a secondary displacement in conservatively treated paediatric distal radius metaphyseal fractures. A multicentric study. Clin. Ther. 2022, 173, 84–87. [Google Scholar] [CrossRef]
- Marson, B.A.; Ng, J.W.G.; Craxford, S.; Chell, J.; Lawniczak, D.; Price, K.R.; Ollivere, B.J.; Hunter, J.B. Treatment of completely displaced distal radial fractures with a straight plaster or manipulation under anaesthesia. Bone Jt. J. 2021, 103, 902–907. [Google Scholar] [CrossRef]
- Graham, H.K. Fractures of the Distal Radial Metaphysis in Children: Which Ones Need Reduction?: Commentary on an article by Topi Laaksonen, MD; et al.: “Epidemiology, Treatment, and Treatment Quality of Overriding Distal Metaphyseal Radial Fractures in Children and Adolescents”. J. Bone Jt. Surg. 2022, 104, 297. [Google Scholar] [CrossRef]
- Truong, W.H.; Howard, A.; Georgiadis, A. Displaced Distal Radius Fractures in Children: To Reduce or Not to Reduce? To Pin or Not to Pin? JPOSNA® 2020, 2. [Google Scholar] [CrossRef]
- Laaksonen, T.; Kosola, J.; Nietosvaara, N.; Puhakka, J.; Nietosvaara, Y.; Stenroos, A. Epidemiology, Treatment, and Treatment Quality of Overriding Distal Metaphyseal Radial Fractures in Children and Adolescents. J. Bone Jt. Surg. 2022, 104, 207–214. [Google Scholar] [CrossRef]
- Vescio, A.; Testa, G.; Sapienza, M.; Caldaci, A.; Montemagno, M.; Andreacchio, A.; Canavese, F.; Pavone, V. Is Obesity a Risk Factor for Loss of Reduction in Children with Distal Radius Fractures Treated Conservatively? Children 2022, 9, 425. [Google Scholar] [CrossRef]
- Kruppa, C.; Bunge, P.; Schildhauer, T.A.; Dudda, M. Low complication rate of elastic stable intramedullary nailing (ESIN) of pediatric forearm fractures: A retrospective study of 202 cases. Medicine 2017, 96, e6669. [Google Scholar] [CrossRef]
- Kraus, R. Distale Radiusfraktur im Wachstumsalter. Trauma Und Berufskrankh. 2014, 16, 53–60. [Google Scholar] [CrossRef]
- Weinberg, A.M.; Castellani, C.; Amerstorfer, F. Elastisch-stabile intramedulläre Marknagelung (ESIN) von Unterarmfrakturen. Oper. Orthop. Und Traumatol. 2008, 20, 285–296. [Google Scholar] [CrossRef]
- Slongo, T. Technique and biomechanics of Kirschner wire osteosynthesis in children. Oper. Orthop. Und Traumatol. 2020, 32, 509–529. [Google Scholar] [CrossRef]
- Kubiak, R.; Aksakal, D.; Weiss, C.; Wessel, L.M.; Lange, B. Is there a standard treatment for displaced pediatric diametaphyseal forearm fractures?: A STROBE-compliant retrospective study. Medicine 2019, 98, e16353. [Google Scholar] [CrossRef]
- Lieber, J.; Sommerfeldt, D.W. Diametaphyseal forearm fracture in childhood: Pitfalls and recommendations for treatment. Unfallchirurg 2011, 114, 292–299. [Google Scholar] [CrossRef]
- Slongo, T. Was tun, wenn die elastisch-stabile intramedulläre Nagelung (ESIN) an ihre Grenzen stößt? Trauma Und Berufskrankh. 2015, 17, 216–228. [Google Scholar] [CrossRef]
- Józsa, G.; Devecseri, G.; Vajda, P.; Juhasz, Z.; Varga, M.; Juhasz, T. Distance of the fracture from the radiocarpal surface in childhood: Does it determine surgical technique? A retrospective clinical study: A STROBE compliant observational study. Medicine 2020, 99, e17763. [Google Scholar] [CrossRef]
- Sato, K.; Mimata, Y.; Takahashi, G.; Murakami, K.; Numata, N.; Doita, M. Fractures of the proximal segments of the pediatric distal radial metaphysis exhibit less angular stability than fractures of the distal segments. J. Pediatr. Orthop. B 2022, 31, 471–478. [Google Scholar] [CrossRef]
- Du, M.; Han, J. Antegrade elastic stable intramedullary nail fixation for paediatric distal radius diaphyseal metaphyseal junction fractures: A new operative approach. Injury 2019, 50, 598–601. [Google Scholar] [CrossRef] [PubMed]
- Lieber, J.; Schmid, E.; Schmittenbecher, P.P. Unstable diametaphyseal forearm fractures: Transepiphyseal intramedullary Kirschner-wire fixation as a treatment option in children. Eur. J. Pediatr. Surg. 2010, 20, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Ebert, L.C. Die Distale Diametaphysäre Radiusfraktur im Kindesalter—Ein Vergleich Verschiedener Therapieverfahren. Ph.D. Thesis, University of Regensburg, Regensburg, Germany, 2019. [Google Scholar]
- Kim, B.S.; Lee, Y.S.; Park, S.Y.; Nho, J.H.; Lee, S.G.; Kim, Y.H. Flexible Intramedullary Nailing of Forearm Fractures at the Distal Metadiaphyseal Junction in Adolescents. Clin. Orthop. Surg. 2017, 9, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Meinberg, E.G.; Agel, J.; Roberts, C.S.; Karam, M.D.; Kellam, J.F. Fracture and Dislocation Classification Compendium-2018. J. Orthop. Trauma 2018, 32 (Suppl. S1), S1–S170. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibanes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Varga, M.; Jozsa, G.; Hanna, D.; Toth, M.; Hajnal, B.; Krupa, Z.; Kassai, T. Bioresorbable implants vs. Kirschner-wires in the treatment of severely displaced distal paediatric radius and forearm fractures—A retrospective multicentre study. BMC Musculoskelet. Disord. 2022, 23, 362. [Google Scholar] [CrossRef]
- LaValva, S.M.; Rogers, B.H.; Arkader, A.; Shah, A.S. Risk Factors for Failed Closed Reduction of Pediatric Distal Radius Fractures. J. Hand Surg. Glob. Online 2020, 2, 196–202. [Google Scholar] [CrossRef]
- Miller, B.S.; Taylor, B.; Widmann, R.F.; Bae, D.S.; Snyder, B.D.; Waters, P.M. Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: A prospective, randomized study. J. Pediatr. Orthop. 2005, 25, 490–494. [Google Scholar] [CrossRef]
- Caruso, G.; Caldari, E.; Sturla, F.D.; Caldaria, A.; Re, D.L.; Pagetti, P.; Palummieri, F.; Massari, L. Management of pediatric forearm fractures: What is the best therapeutic choice? A narrative review of the literature. Musculoskelet. Surg. 2020, 105, 225–234. [Google Scholar] [CrossRef]
- Jordan, R.W.; Westacott, D.; Srinivas, K.; Shyamalan, G. Predicting redisplacement after manipulation of paediatric distal radius fractures: The importance of cast moulding. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 841–845. [Google Scholar] [CrossRef]
- Constantino, D.M.; Machado, L.; Carvalho, M.; Cabral, J.; Cardoso, P.S.; Balacó, I.; Ling, T.P.; Alves, C. Redisplacement of paediatric distal radius fractures: What is the problem? J. Child. Orthop. 2021, 15, 532–539. [Google Scholar] [CrossRef]
- Crawford, S.N.; Lee, L.S.; Izuka, B.H. Closed treatment of overriding distal radial fractures without reduction in children. J. Bone Jt. Surg. 2012, 94, 246–252. [Google Scholar] [CrossRef]
- Barvelink, B.; Ploegmakers, J.J.W.; Harsevoort, A.G.J.; Stevens, M.; Verheyen, C.C.; Hepping, A.M.; Bulstra, S.K. The evolution of hand function during remodelling in nonreduced angulated paediatric forearm fractures: A prospective cohort study. J. Pediatr. Orthop. B 2020, 29, 172–178. [Google Scholar] [CrossRef]
- Gendelberg, D.; Hennrikus, W.; Slough, J.; Armstrong, D.; King, S. A Radiation Safety Training Program Results in Reduced Radiation Exposure for Orthopaedic Residents Using the Mini C-arm. Clin. Orthop. Relat. Res. 2016, 474, 580–584. [Google Scholar] [CrossRef]
- Varga, M.; Józsa, G.; Fadgyas, B.; Kassai, T.; Renner, A. Short, double elastic nailing of severely displaced distal pediatric radial fractures. Medicine 2017, 96, e6532. [Google Scholar] [CrossRef]
- Wang, R.; Wu, L.; Wang, Y.; Fan, M.; Wang, Y.; Ning, B.; Zheng, P. Limited Open Reduction and Transepiphyseal Intramedullary Kirschner Wire Fixation for Treatment of Irreducible Distal Radius Diaphyseal Metaphyseal Junction Fracture in Older Children. Front. Pediatr. 2022, 10, 871044. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gotzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; Initiative, S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef]
|
| N Total | Spiral (%) | Oblique (%) | Transverse (%) | Multifragmentary/ Comminuted (%) | |
|---|---|---|---|---|---|
| Fall | 44 | 1 (2.3%) | 18 (40.9%) | 24 (54.5%) | 1 (2.3%) |
| Sport | 44 | 1 (2.3%) | 16 (36.4%) | 25 (56.8%) | 2 (4.6%) |
| Fall from a height | 24 | 3 (12.5%) | 9 (37.5%) | 12 (50%) | 0 |
| Bicycle accident | 15 | 4 (26.7%) | 3 (20%) | 8 (53.3% | 0 |
| Traffic accident | 3 | 0 | 0 | 2 (66.7%) | 1 (33.3%) |
| Other/Unknown | 2 | 0 | 1 (50%) | 1 (50%) | 0 |
| Characteristics | N (%) |
|---|---|
| Type of stabilization | |
| -Cast application | 62 (47%) |
| -ESIN | 14 (10.6%) |
| -K-wires | 47 (35.6%) |
| -K-ESIN | 4 (3.0%) |
| -Plate osteosynthesis | 5 (3.8%) |
| Unplanned reoperation | |
| -Yes | 11 (8.3%) |
| -No | 121 (91.7%) |
| N Total | Conservative (%) n = 62 | Operative (%) n = 70 | p-Value 1 | ||
|---|---|---|---|---|---|
| Reoperation | Yes | 11 | 7 (11.3%) | 4 (5.7%) | 0.347 |
| (Clavien-Dindo IIIb) | No | 121 | 55 (88.7%) | 66 (94.3%) | |
| Other complications | Yes | 19 | 6 (9.7%) | 13 (18.6%) | 0.214 |
| No | 113 | 56 (90.3%) | 57 (81.4%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wollkopf, A.D.P.; Halbeisen, F.S.; Holland-Cunz, S.G.; Mayr, J. Diametaphyseal Distal Forearm Fractures in Children: A STROBE Compliant Comparison of Outcomes of Different Stabilization Techniques Regarding Complications. Children 2023, 10, 374. https://doi.org/10.3390/children10020374
Wollkopf ADP, Halbeisen FS, Holland-Cunz SG, Mayr J. Diametaphyseal Distal Forearm Fractures in Children: A STROBE Compliant Comparison of Outcomes of Different Stabilization Techniques Regarding Complications. Children. 2023; 10(2):374. https://doi.org/10.3390/children10020374
Chicago/Turabian StyleWollkopf, Andreas D. P., Florian S. Halbeisen, Stefan G. Holland-Cunz, and Johannes Mayr. 2023. "Diametaphyseal Distal Forearm Fractures in Children: A STROBE Compliant Comparison of Outcomes of Different Stabilization Techniques Regarding Complications" Children 10, no. 2: 374. https://doi.org/10.3390/children10020374
APA StyleWollkopf, A. D. P., Halbeisen, F. S., Holland-Cunz, S. G., & Mayr, J. (2023). Diametaphyseal Distal Forearm Fractures in Children: A STROBE Compliant Comparison of Outcomes of Different Stabilization Techniques Regarding Complications. Children, 10(2), 374. https://doi.org/10.3390/children10020374






