A Cross-Sectional Investigation of Preadolescent Cardiometabolic Health: Associations with Fitness, Physical Activity, Sedentary Behavior, Nutrition, and Sleep
Abstract
1. Introduction
2. Materials and Methods
2.1. Recruitment and Participants
2.2. Study Design
2.3. Primary Outcome: Cardiometabolic Disease Risk
2.3.1. Adiposity
2.3.2. Pulse Wave Analysis
2.3.3. Blood Biomarkers
2.4. Exposure Variables
2.4.1. Cardiorespiratory Fitness
2.4.2. Muscular Fitness
2.4.3. Physical Activity and Sedentary Behavior
2.4.4. Sleep
2.4.5. Nutrition
2.5. Covariates
2.6. Statistical Analysis
3. Results
3.1. Cardiometabolic Factor Correlations and Analysis
3.2. Univariate Models
3.3. Multivariable Models
4. Discussion
4.1. Comparison with Other Studies
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 12 October 2022).
- Jankowska, A.; Brzezí Nski, M.; Romanowicz-Sołtyszewska, A.; Szlagatys-Sidorkiewicz, A. Metabolic Syndrome in Obese Children-Clinical Prevalence and Risk Factors. Int. J. Environ. Res. Public Health Artic. Public Health 2021, 18, 1060. [Google Scholar] [CrossRef]
- Stoner, L.; Pontzer, H.; Barone Gibbs, B.; Moore, J.B.; Castro, N.; Skidmore, P.; Lark, S.; Williams, M.A.; Hamlin, M.J.; Faulkner, J. Fitness and Fatness Are Both Associated with Cardiometabolic Risk in Preadolescents. J. Pediatr. 2020, 217, 39–45.e1. [Google Scholar]
- Stoner, L.; Castro, N.; Signal, L.; Skidmore, P.; Faulkner, J.; Lark, S.; Williams, M.A.; Muller, D.; Harrex, H. Sleep and Adiposity in Preadolescent Children: The Importance of Social Jetlag. Child. Obes. 2018, 14, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Stoner, L.; Weatherall, M.; Skidmore, P.; Castro, N.; Lark, S.; Faulkner, J.; Williams, M.A. Cardiometabolic risk variables in preadolescent children: A factor analysis. J. Am. Heart Assoc. 2017, 6, e007071. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.B.; Riddoch, C.; Kriemler, S.; Hills, A.P. Physical activity and cardiovascular risk factors in children. Br. J. Sports Med. 2011, 45, 871–876. [Google Scholar] [CrossRef] [PubMed]
- Gillman, M.W.; Pinto, B.M.; Tennstedt, S.; Glanz, K.; Marcus, B.; Friedman, R.H. Relationships of physical activity with dietary behaviors among adults. Prev. Med. 2001, 32, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Bai, W.; Zhu, B.; Duan, R.; Yu, X.; Xu, W.; Wang, M.; Hua, W.; Yu, W.; Li, W.; et al. Prevalence and correlates of poor sleep quality among college students: A cross-sectional survey. Health Qual. Life Outcomes 2020, 18, 1–11. [Google Scholar] [CrossRef]
- Rabel, M.; Laxy, M.; Thorand, B.; Peters, A.; Schwettmann, L.; Mess, F. Clustering of Health-Related Behavior Patterns and Demographics. Results From the Population-Based KORA S4/F4 Cohort Study. Front. Public Health. 2019, 6, 387. [Google Scholar] [CrossRef]
- Whitaker, K.M.; Gabriel, K.P.; Buman, M.P.; Pereira, M.A.; Jacobs, D.R.; Reis, J.P.; Gibbs, B.B.; Carnethon, M.R.; Staudenmayer, J.; Sidney, S.; et al. Associations of accelerometer-measured sedentary time and physical activity with prospectively assessed cardiometabolic risk factors: The CARDIA study. J. Am. Heart Assoc. 2019, 8, e010212. [Google Scholar] [CrossRef]
- Dolezal, B.A.; Neufeld, E.V.; Boland DMMartin, J.L.; Cooper, C.B. Interrelationship between Sleep and Exercise: A Systematic Review. Adv. Prev. Med. 2017, 2017, 1–14. [Google Scholar] [CrossRef]
- Fletcher, E.A.; McNaughton, S.A.; Crawford, D.; Cleland, V.; Della Gatta, J.; Hatt, J.; Dollman, J.; Timperio, A. Associations between sedentary behaviours and dietary intakes among adolescents. Public Health Nutr. 2018, 21, 1115. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults a report of the American College of Cardiology/American Heart Association Task Force on Clinical practice guidelines. Hypertension 2018, 71, E13–E115. [Google Scholar] [CrossRef] [PubMed]
- Abbate, M.; Gallardo-Alfaro, L.; Del Mar Bibiloni, M.; Tur, J.A. Efficacy of dietary intervention or in combination with exercise on primary prevention of cardiovascular disease: A systematic review. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1080–1093. [Google Scholar] [CrossRef] [PubMed]
- Ventura, E.; Davis, J.; Byrd-Williams, C.; Alexander, K.; McClain, A.; Lane, C.J.; Spruijt-Metz, D.; Weigensberg, M.; Goran, M. Reduction in risk factors for type 2 diabetes mellitus in response to a low-sugar, high-fiber dietary intervention in overweight Latino adolescents. Arch. Pediatr. Adolesc. Med. 2009, 163, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Van Buren, D.J.; Tibbs, T.L. Lifestyle Interventions to Reduce Diabetes and Cardiovascular Disease Risk Among Children. Curr. Diab. Rep. 2014, 14, 1–11. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Castro, N.; Faulkner, J.; Skidmore, P.; Williams, M.; Lambrick, D.M.; Signal, L.; Thunders, M.; Muller, D.; Lark, S.; Hamlin, M.; et al. Pre-Adolescent Cardio-Metabolic Associations and Correlates: PACMAC methodology and study protocol. BMJ Open 2014, 4, e005815. [Google Scholar] [CrossRef]
- Noradilah, M.J.; Ang, Y.N.; Kamaruddin, N.A.; Deurenberg, P.; Ismail, M.N.; Poh, B.K. Assessing Body Fat of Children by Skinfold Thickness, Bioelectrical Impedance Analysis, and Dual-Energy X-Ray Absorptiometry: A Validation Study among Malay Children Aged 7 to 11 Years. Asia-Pacific J. Public Health 2016, 28, 74S–84S. [Google Scholar] [CrossRef]
- Saikia, B.; Derrick, G.; Fordham, T.; Brierley, J. Validation of uscom bp+ in children and adolescents a preliminary report. Crit. Care Med. 2015, 43, 30–31. [Google Scholar] [CrossRef]
- Stoner, L.; Lambrick, D.M.; Faulkner, J.; Young, J. Guidelines for the use of pulse wave analysis in adults and children. J. Atheroscler. Thromb. 2013, 20, 404–406. Available online: http://www.ncbi.nlm.nih.gov/pubmed/23358124 (accessed on 11 June 2018). [CrossRef]
- Butlin, M.; Qasem, A.; Avolio, A.P. Estimation of central aortic pressure waveform features derived from the brachial cuff volume displacement waveform. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS, San Diego, CA, USA, 28 August–1 September 2012. [Google Scholar]
- Wilkinson, D.M.; Fallowfield, J.L.; Myers, S.D. A modified incremental shuttle run test for the determination of peak shuttle running speed and the prediction of maximal oxygen uptake. J. Sport. Sci. 2010, 17, 413–419. [Google Scholar] [CrossRef]
- Boreham, C.; Paliczka, V.J.; Nichols, A. A comparison of the PWC170 and 20-MST tests of aerobic fitness in adolescent schoolchildren. J. Sport. Med. Phys. Fit. 1990, 30, 19–23. [Google Scholar]
- Hamlin, M.J.; Fraser, M.; Lizamore, C.A.; Draper, N.; Shearman, J.P.; Kimber, N.E. Measurement of Cardiorespiratory Fitness in Children from Two Commonly Used Field Tests After Accounting for Body Fatness and Maturity. J. Hum. Kinet. 2014, 40, 83. [Google Scholar] [CrossRef] [PubMed]
- Melo, X.; Santa-Clara, H.; Almeida, J.P.; Carnero, E.A.; Sardinha, L.B.; Bruno, P.M.; Fernhall, B. Comparing several equations that predict peak VO2 using the 20-m multistage-shuttle run-test in 8–10-year-old children. Eur. J. Appl. Physiol. 2010, 111, 839–849. [Google Scholar] [CrossRef] [PubMed]
- Leger, L.A.; Lambert, J. A maximal multistage 20-m shuttle run test to predict VO2 max. Eur. J. Appl. Physiol. Occup. Physiol. 1982, 49, 1–12. [Google Scholar] [CrossRef] [PubMed]
- MIirwald, R.L.; GBaxter-Jones, A.D.; Bailey, D.A.; Beunen, G.P. An assessment of maturity from anthropometric measurements. Med. Sci. Sports Exerc. 2002, 34, 689–694. [Google Scholar] [CrossRef]
- Fitness Assessment—FitnessGram by The Cooper Institute. Available online: https://fitnessgram.net/assessment/ (accessed on 27 October 2021).
- Innes, E. Handgrip strength testing: A review of the literature. Aust. Occup. Ther. J. 1999, 46, 120–140. [Google Scholar] [CrossRef]
- Hashmi, S. Validation of Youth Physical Activity Questionnaire (YPAQ) against Actigraph GT3X Accelerometer among Preadolescents and Adolescents in Urban Setting of Karachi, Pakistan. Theses Diss. January 2012. Available online: https://ecommons.aku.edu/theses_dissertations/1214 (accessed on 3 February 2023).
- Brooke, H.L.; Corder, K.; Griffin, S.J.; Ekelund, U.; van Sluijs, E.M. More of the same or a change of scenery: An observational study of variety and frequency of physical activity in British children. BMC Public Health 2013, 13, 1–9. [Google Scholar] [CrossRef]
- Corder, K.; van SLuijs, E.M.; Wright, A.; Whincup, P.; Wareham, N.J.; Ekelund, U. Is it possible to assess free-living physical activity and energy expenditure in young people by self-report? Am. J. Clin. Nutr. 2009, 89, 862–870. [Google Scholar] [CrossRef]
- Roenneberg, T.; Allebrandt, K.V.; Merrow, M.; Vette. Social jetlag and obesity. Curr. Biol. 2012, 22, 939–943. [Google Scholar] [CrossRef]
- Wolfson, A.R.; Carskadon, M.A.; Acebo, C.; Seifer, R.; Fallone, G.; Labyak, S.E.; Marin, J.L. Evidence for the validity of a sleep habits survey for adolescents. Sleep 2003, 26, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Owens, J.A.; Spirito, A.; McGuinn, M.; Nobile, C. Sleep habits and sleep disturbance in elementary school-aged children. J. Dev. Behav. Pediatr. 2000, 21, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, P.; Sjeaff, S.A.; Wong, J.E.; Skidmore, P.M. Reproducibility and Relative Validity of a Short Food Frequency Questionnaire in 9-10 Year-Old Children. Nutrients 2016, 8, 271. [Google Scholar] [CrossRef] [PubMed]
- Schulze, M.B.; Hoffman, K.; Kroke, A.; Boeing, H. An approach to construct simplified measures of dietary patterns from exploratory factor analysis. Br. J. Nutr. 2003, 89, 409–418. [Google Scholar] [CrossRef] [PubMed]
- New Zealand in Profile 2015: An Overview of New Zealand’s People, Economy, and Environment; Statistics New Zealand: Wellington, New Zealand, 2015.
- Goldstein, H. Multilevel Statistical Models, 4th ed.; Wiley: Hoboken, NJ, USA, 2010. [Google Scholar]
- Higgins, S.; Pomeroy, A.; Bates, L.C.; Paterson, C.; Barone Gibbs, B.; Pontzer, H.; Stoner, L. Sedentary behavior and cardiovascular disease risk: An evolutionary perspective. Front. Physiol. 2022, 13, 962791. [Google Scholar] [CrossRef] [PubMed]
- Veronesi, G.; Powell-Wiley, T.M.; Degano, I.R.; Stoner, L.; Gibbs, B.B.; Barone Gibbs, B.; Meyer, M.L.; Fryer, S.; Credeur, D.; Paterson, C.; et al. A Primer on Repeated Sitting Exposure and the Cardiovascular System: Considerations for Study Design, Analysis, Interpretation, and Translation. Front. Cardiovasc. Med. 2021, 1, 716938. [Google Scholar] [CrossRef]
- Ross, R.; Blair, S.N.; Arena, R.; Church, T.S.; Despres, J.P.; Franklin, B.A.; Haskell, W.L.; Kaminsky, L.A.; Levine, B.D.; Lavie, C.J.; et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e653–e699. [Google Scholar] [CrossRef]
- Patel, M. Normative Data of VO2 max Using 20 Meter Shuttle Run Test in Normal Healthy Urban Children Between the Age Group of 7 to 19 Years. Int. J. Innov. Sci. Res. Technol. 2020, 5, 1161–1166. [Google Scholar]
- Heyward, V.H. The Physical Fitness Specialist Certification Manual; The Cooper Institute for Aerobics Research: Dallas, TX, USA, 1998; Volume 48. [Google Scholar]
- Carnethon, M.R.; Gidding, S.S.; Nehgme, R.; Sidney, S.; Jacobs, D.R.; Liu, K. Cardiorespiratory Fitness in Young Adulthood and the Development of Cardiovascular Disease Risk Factors. J. Am. Med. Assoc. 2003, 290, 3092–3100. [Google Scholar] [CrossRef]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA J. Am. Med. Assoc. 2009, 301, 2024–2035. [Google Scholar] [CrossRef]
- Stevens, J.; Cai, J.; Evenson, K.R.; Thomas, R. Fitness and Fatness as Predictors of Mortality from All Causes and from Cardiovascular Disease in Men and Women in the Lipid Research Clinics Study. Am. J. Epidemiol. 2002, 156, 832–841. [Google Scholar] [CrossRef] [PubMed]
- We Must Identify and Treat Obese Kids. Available online: https://www.newsweek.com/we-must-identify-and-treat-obese-kids-628625 (accessed on 30 November 2022).
- Ruiz, J.R.; Cavero-Redondo, I.; Ortega, F.B.; Welk, G.J.; Andersen, L.B.; Martinez-Vizcaino, V. Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br. J. Sports Med. 2016, 50, 1451 LP–1458 LP. [Google Scholar] [CrossRef] [PubMed]
- Mota, J.; Guerra, S.; Leandro, C.; Pinto, A.; Ribeiro, J.C.; Duarte, J.A. Association of maturation, sex, and body fat in cardiorespiratory fitness. Am. J. Hum. Biol. 2002, 14, 707–712. [Google Scholar] [CrossRef] [PubMed]
- O’Keeffe, L.M.; Frysz, M.; Bell, J.A.; Howe, L.D.; Fraser, A. Puberty timing and adiposity change across childhood and adolescence: Disentangling cause and consequence. Hum. Reprod. 2020, 35, 2784–2792. [Google Scholar] [CrossRef]
- Albert, P.R. Why is depression more prevalent in women? J. Psychiatry Neurosci. 2015, 40, 219–221. [Google Scholar] [CrossRef]
- de Heer, H.D.; Wilkinson, A.V.; Strong, L.L.; Bondy, M.L.; Koehly, L.M. Sitting time and health outcomes among Mexican origin adults: Obesity as a mediator. BMC Public Heal. 2012, 12, 1–9. [Google Scholar] [CrossRef]
- Frydenlund, G.; Jørgensen, T.; Toft, U.; Pisinger, C.; Aadahl, M. Sedentary leisure time behavior, snacking habits and cardiovascular biomarkers: The Inter99 Study. Eur. J. Prev. Cardiol. 2012, 19, 1111–1119. [Google Scholar] [CrossRef]
- Pereira, S.M.P.; Ki, M.; Power, C. Sedentary Behaviour and Biomarkers for Cardiovascular Disease and Diabetes in Mid-Life: The Role of Television-Viewing and Sitting at Work. PLoS ONE 2012, 7, e31132. [Google Scholar] [CrossRef]
- Pulsford, R.M.; Stamatakis, E.; Britton, A.R.; Brunner, E.J.; Hillsdon, M.M. Sitting Behavior and Obesity: Evidence from the Whitehall II Study. Am. J. Prev. Med. 2013, 44, 132. [Google Scholar] [CrossRef]
- van der Ploeg, H.P.; Chey, T.; Korda, R.J.; Banks, E.; Bauman, A. Sitting Time and All-Cause Mortality Risk in 222 497 Australian Adults. Arch. Intern. Med. 2012, 172, 494–500. [Google Scholar] [CrossRef]
- Yates, T.; Khunti, K.; Wilmot, E.G.; Brady, E.; Webb, D.; Srinivasan, B.; Henson, J.; Talbot, D.; Davies, M.J. Self-Reported Sitting Time and Markers of Inflammation, Insulin Resistance, and Adiposity. Am. J. Prev. Med. 2012, 42, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, B.; Baur, L.A.; Hardy, L.L.; Kifley, A.; Rose, K.A.; Wong, T.Y.; Mitchell, P. Relationship between a range of sedentary behaviours and blood pressure during early adolescence. J. Hum. Hypertens. 2011, 26, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Grøntved, A.; Ried-Larsen, M.; Møller, N.C.; Kristensen, P.L.; Wedderkopp, N.; Froberg, K.; Hu, F.B.; Ekelund, U.; Andersen, L.B. Youth screen-time behaviour is associated with cardiovascular risk in young adulthood: The European Youth Heart Study. Eur. J. Prev. Cardiol. 2014, 21, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.R.; Ortega, F.B.; Castillo, R.; Martin-Matillas, M.; Kwak, L.; Vicente-Rodriguez, G.; Noriega, J.; Tercedor, P.; Sjostrom, M.; Moreno, L.A.; et al. Physical activity, fitness, weight status, and cognitive performance in adolescents. J. Pediatr. 2010, 157, 917–922.E5. [Google Scholar] [CrossRef]
- Grontved, A.; Ried-Larsen, M.; Froberg, K.; Wedderkopp, N.; Brage, S.; Kristensen, P.L.; Andersen, L.B.; Møller, N.C. Screen time viewing behaviors and isometric trunk muscle strength in youth. Med. Sci. Sports Exerc. 2013, 45, 1975–1980. [Google Scholar] [CrossRef]
- Bates, L.; Zieff, G.; Stanford, K.; Moore, J.; Kerr, Z.; Hanson, E.; Barone Gibbs, B.; Kline, C.; Stoner, L. COVID-19 Impact on Behaviors across the 24-Hour Day in Children and Adolescents: Physical Activity, Sedentary Behavior, and Sleep. Children 2020, 7, 138. [Google Scholar] [CrossRef]
- Gortmaker, S.L.; Cheung, L.W.Y.; Peterson, K.E.; Chomitz, G.; Cradle, J.H.; Dart, H.; Fox, M.K.; Bullock, R.B.; Sobol, A.M.; Colditz, G.; et al. Impact of a School-Based Interdisciplinary Intervention on Diet and Physical Activity Among Urban Primary School Children: Eat Well and Keep Moving. Arch. Pediatr. Adolesc. Med. 1999, 153, 975–983. [Google Scholar] [CrossRef]

| (a) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Stratified by CMD Risk Score | ||||||||
| Total | Low | Normal | High | |||||
| n | % | n | % | n | % | n | % | |
| Categorical Variables | ||||||||
| Ethnicity | ||||||||
| European | 257 | 82 | 35 | 14 | 191 | 74 | 31 | 12 |
| Māori-Pacific Islander | 56 | 18 | 6 | 11 | 34 | 61 | 16 | 29 |
| School Year | ||||||||
| 4 | 69 | 22 | 13 | 18 | 52 | 75 | 4 | 6 |
| 5 | 88 | 28 | 9 | 10 | 71 | 81 | 8 | 9 |
| 6 | 96 | 30 | 15 | 16 | 60 | 63 | 21 | 22 |
| 7 | 63 | 20 | 4 | 6 | 44 | 70 | 15 | 24 |
| Decile | ||||||||
| Low (≤5) | 162 | 51 | 23 | 14 | 109 | 67 | 30 | 19 |
| High (>5) | 154 | 49 | 18 | 12 | 118 | 77 | 18 | 12 |
| Weight Status | ||||||||
| Overweight | 89 | 28 | 1 | 1 | 59 | 66 | 29 | 33 |
| Non-Overweight | 227 | 72 | 40 | 18 | 168 | 74 | 19 | 8 |
| Fitness level | ||||||||
| VO2 max (mL/kg/min) | 42.9 | 4.4 | 45.1 | 4 | 43.3 | 4 | 39.4 | 5 |
| VO2 max Low | 232 | 73 | 38 | 16 | 178 | 77 | 16 | 7 |
| VO2 max High | 84 | 27 | 3 | 4 | 49 | 58 | 32 | 38 |
| (b) | ||||||||
| Stratified by CMD Risk Score | ||||||||
| Total | Low | Normal | Low | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Continuous Variables | ||||||||
| Age (years) | 9.6 | 1.1 | 9.2 | 1.1 | 9.5 | 1.2 | 10.0 | 0.9 |
| Body Fatness | ||||||||
| Weight (kg) | 34.4 | 9.2 | 30.7 | 5.6 | 33.1 | 7.3 | 43.9 | 13.0 |
| Body Fat (%) | 19.7 | 9.4 | 13.1 | 5.3 | 18.7 | 7.5 | 29.9 | 12.2 |
| Fat Mass Index (fat mass/m2) | 3.65 | 2.4 | 2.1 | 0.9 | 3.3 | 1.6 | 6.7 | 3.7 |
| Waist-to-Hip Ratio | 0.8 | 0.1 | 0.8 | 0.1 | 0.8 | 0.0 | 0.9 | 0.1 |
| Physical Activity & Sedentary Behavior | ||||||||
| Physical Activity (min) | 166.0 | 137.0 | 190.2 | 151.3 | 162.8 | 131.4 | 162.2 | 151.9 |
| Sedentary Behavior (min) | 282.0 | 208.0 | 230.5 | 158.1 | 286.4 | 214.1 | 308.3 | 212.5 |
| Sleep | ||||||||
| Average Sleep Duration (h) | 10.1 | 0.8 | 10.4 | 0.7 | 10.1 | 0.8 | 10.1 | 0.9 |
| Social Jetlag (h) | 0.7 | 0.5 | 0.6 | 0.4 | 0.7 | 0.5 | 0.9 | 0.6 |
| Sleep Disturbances | 40.2 | 5.9 | 39.5 | 5.5 | 40.2 | 6.0 | 41.0 | 6.0 |
| Dietary Habits | ||||||||
| Processed Food | 0.0 | 1.9 | 0.4 | 2.3 | −0.1 | 1.4 | 0.5 | 3.1 |
| Fruit and Vegetable Pattern | 0.1 | 1.6 | 0.5 | 1.8 | 0.1 | 1.5 | −0.5 | 1.5 |
| Breakfast Food | 0.0 | 1.3 | 0.2 | 1.3 | 0.0 | 1.3 | −0.1 | 1.2 |
| Cardiometabolic Risk | ||||||||
| Systolic Blood Pressure (mmHg) | 100.8 | 7.7 | 94.7 | 5.0 | 100.4 | 6.9 | 108.4 | 7.5 |
| Diastolic Blood Pressure (mmHg) | 61.6 | 6.2 | 55.8 | 5.0 | 61.6 | 5.4 | 66.9 | 6.0 |
| Central Blood Pressure (mmHg) | 93.3 | 7.7 | 86.9 | 6.3 | 93.1 | 6.9 | 99.9 | 7.5 |
| Augmentation Index (%) | 55.8 | 15.3 | 57.1 | 13.6 | 56.5 | 15.3 | 51.3 | 16.1 |
| Heart Rate (bpm) | 74.8 | 11.7 | 67.9 | 10.4 | 75.1 | 11.2 | 79.3 | 12.8 |
| Fasting Blood Glucose (mmol/L) | 5.0 | 0.4 | 5.0 | 0.4 | 5.0 | 0.4 | 5.1 | 0.4 |
| Glycosylated Hemoglobin (%) | 5.1 | 0.3 | 5.0 | 0.3 | 5.1 | 0.3 | 5.3 | 0.4 |
| Total Cholesterol (mmol/L) | 3.6 | 0.6 | 3.1 | 0.4 | 3.6 | 0.5 | 4.0 | 0.8 |
| HDL Cholesterol (mmol/L) | 1.5 | 0.4 | 1.4 | 0.3 | 1.5 | 0.4 | 1.5 | 0.4 |
| LDL Cholesterol (mmol/L) | 1.9 | 0.5 | 1.6 | 0.4 | 1.8 | 0.5 | 2.2 | 0.6 |
| Triglycerides (mmol/L) | 0.9 | 0.4 | 0.8 | 0.2 | 0.8 | 0.4 | 1.1 | 0.6 |
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Comm. | |
|---|---|---|---|---|---|
| BP | CHO | Adiposity | Carb-Met | ||
| SBP | 0.92 | 0.04 | 0.16 | −0.03 | 0.128 |
| DBP | 0.88 | −0.01 | 0.05 | 0.03 | 0.218 |
| cSBP | 0.94 | 0.04 | −0.01 | 0.02 | 0.122 |
| CHO | 0.04 | 0.92 | 0.00 | 0.00 | 0.148 |
| LDL-C | 0.00 | 0.73 | −0.02 | 0.07 | 0.460 |
| HDL-C | −0.04 | −0.50 | 0.03 | 0.50 | 0.493 |
| AIx | 0.25 | −0.03 | −0.68 | 0.13 | 0.458 |
| FMI | 0.25 | −0.09 | 0.56 | 0.46 | 0.410 |
| WHR | 0.06 | 0.03 | 0.50 | 0.29 | 0.663 |
| HR | 0.27 | 0.07 | 0.48 | −0.19 | 0.652 |
| Glucose | 0.07 | −0.10 | 0.48 | −0.14 | 0.739 |
| Triglycerides | 0.14 | −0.05 | −0.13 | 0.65 | 0.536 |
| HbA1c | −0.17 | 0.12 | −0.05 | 0.61 | 0.587 |
| Eigenvalue | 2.8 | 1.7 | 1.5 | 1.4 | |
| % Variance Explained | 21.2 | 12.9 | 11.8 | 10.9 | |
| Cumulative Variance | 21.2 | 34.1 | 45.9 | 56.8 | |
| KMO | 0.56 | ||||
| Bartlett’s Test | <0.001 | ||||
| Bold numbers represent variables with a factor loading > |0.4|. | |||||
| components retained based on an eigenvalue of 1 | |||||
| β | LCI | UCI | p-Value | |
|---|---|---|---|---|
| Univariable | ||||
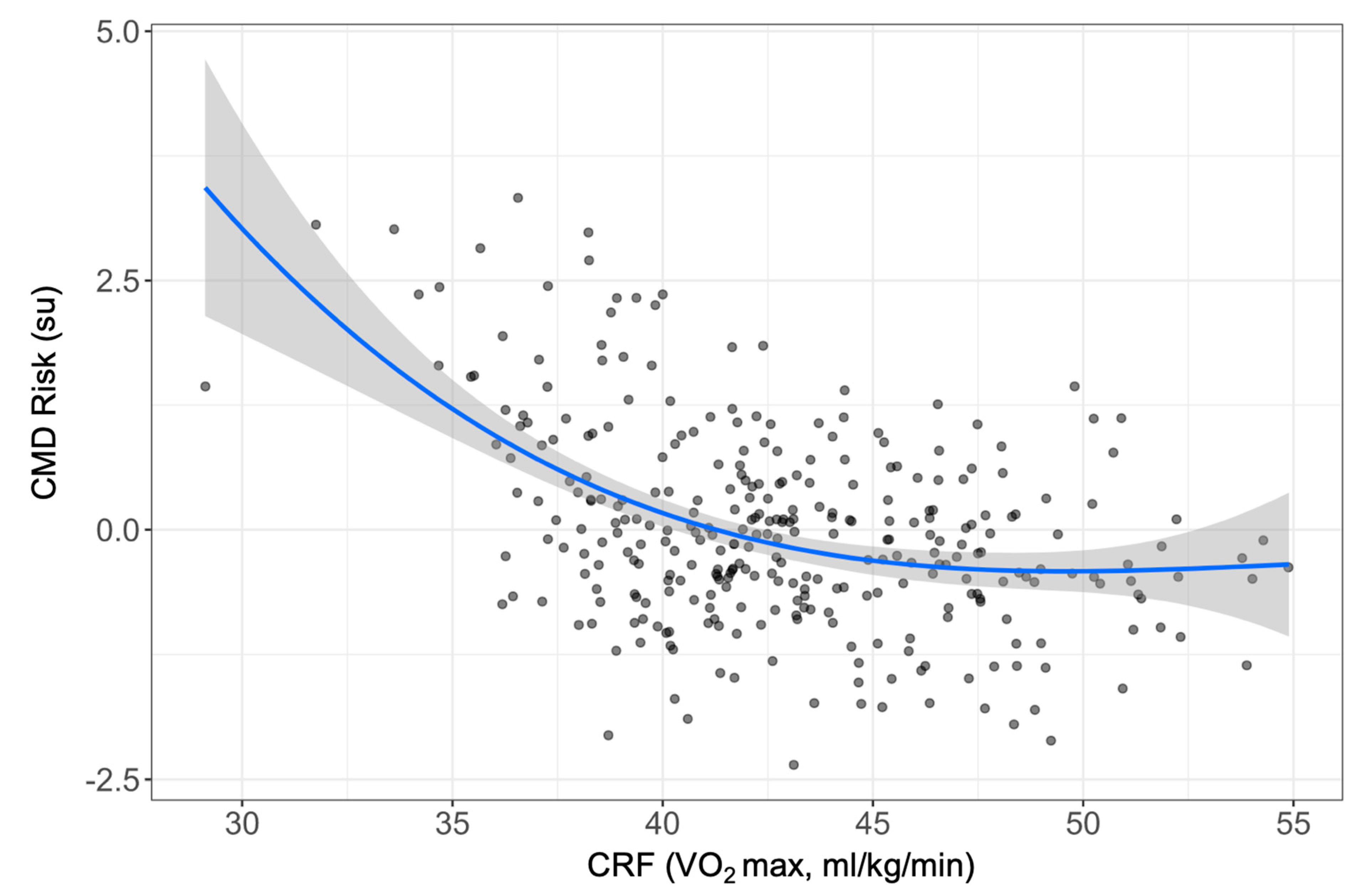
| VO2 max | −0.44 | −0.54 | −0.34 | < 0.001 |
| VO2 maxPoly | 0.17 | 0.10 | 0.25 | <0.001 |
| Strength | 0.15 | 0.04 | 0.26 | 0.007 |
| Physical Activity | 0.00 | −0.11 | 0.11 | 0.974 |
| Sedentary | 0.15 | 0.04 | 0.26 | 0.006 |
| Sleep Duration | −0.11 | −0.22 | 0.00 | 0.052 |
| Social Jetlag | 0.13 | 0.02 | 0.24 | 0.019 |
| Sleep Disturbance | 0.09 | −0.02 | 0.20 | 0.112 |
| Processed Foods | 0.04 | −0.08 | 0.15 | 0.528 |
| Fruit/Veg | −0.17 | −0.28 | −0.06 | 0.003 |
| Breakfast | −0.07 | −0.18 | 0.04 | 0.239 |
| Multivariable Model 1 | ||||
| VO2 max | −0.42 | −0.52 | −0.32 | <0.001 |
| VO2 maxPoly | 0.15 | 0.08 | 0.22 | <0.001 |
| Strength | 0.18 | 0.08 | 0.28 | <0.001 |
| Sedentary | 0.12 | 0.03 | 0.22 | 0.013 |
| Sleep Duration | −0.05 | −0.15 | 0.05 | 0.328 |
| Social Jetlag | −0.01 | −0.11 | 0.09 | 0.832 |
| Fruit/Veg | −0.02 | −0.12 | 0.08 | 0.717 |
| Multivariable Model 2 | ||||
| VO2 max | −0.45 | −0.56 | −0.34 | <0.001 |
| VO2 maxPoly | 0.19 | 0.11 | 0.27 | <0.001 |
| Strength | 0.09 | −0.02 | 0.21 | 0.113 |
| Sedentary | 0.12 | 0.02 | 0.21 | 0.019 |
| Sleep Duration | −0.01 | −0.11 | 0.08 | 0.766 |
| Social Jetlag | −0.02 | −0.12 | 0.08 | 0.662 |
| Fruit/Veg | −0.03 | −0.13 | 0.07 | 0.520 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castro, N.; Zieff, G.; Bates, L.C.; Pagan Lassalle, P.; Higgins, S.; Faulkner, J.; Lark, S.; Skidmore, P.; Hamlin, M.J.; Signal, T.L.; et al. A Cross-Sectional Investigation of Preadolescent Cardiometabolic Health: Associations with Fitness, Physical Activity, Sedentary Behavior, Nutrition, and Sleep. Children 2023, 10, 336. https://doi.org/10.3390/children10020336
Castro N, Zieff G, Bates LC, Pagan Lassalle P, Higgins S, Faulkner J, Lark S, Skidmore P, Hamlin MJ, Signal TL, et al. A Cross-Sectional Investigation of Preadolescent Cardiometabolic Health: Associations with Fitness, Physical Activity, Sedentary Behavior, Nutrition, and Sleep. Children. 2023; 10(2):336. https://doi.org/10.3390/children10020336
Chicago/Turabian StyleCastro, Nicholas, Gabriel Zieff, Lauren C. Bates, Patricia Pagan Lassalle, Simon Higgins, James Faulkner, Sally Lark, Paula Skidmore, Michael J. Hamlin, T. Leigh Signal, and et al. 2023. "A Cross-Sectional Investigation of Preadolescent Cardiometabolic Health: Associations with Fitness, Physical Activity, Sedentary Behavior, Nutrition, and Sleep" Children 10, no. 2: 336. https://doi.org/10.3390/children10020336
APA StyleCastro, N., Zieff, G., Bates, L. C., Pagan Lassalle, P., Higgins, S., Faulkner, J., Lark, S., Skidmore, P., Hamlin, M. J., Signal, T. L., Williams, M. A., & Stoner, L. (2023). A Cross-Sectional Investigation of Preadolescent Cardiometabolic Health: Associations with Fitness, Physical Activity, Sedentary Behavior, Nutrition, and Sleep. Children, 10(2), 336. https://doi.org/10.3390/children10020336








