The Family Caregiving Environment Associates with Adolescent Patients’ Severity of Eating Disorder and Interpersonal Problems: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
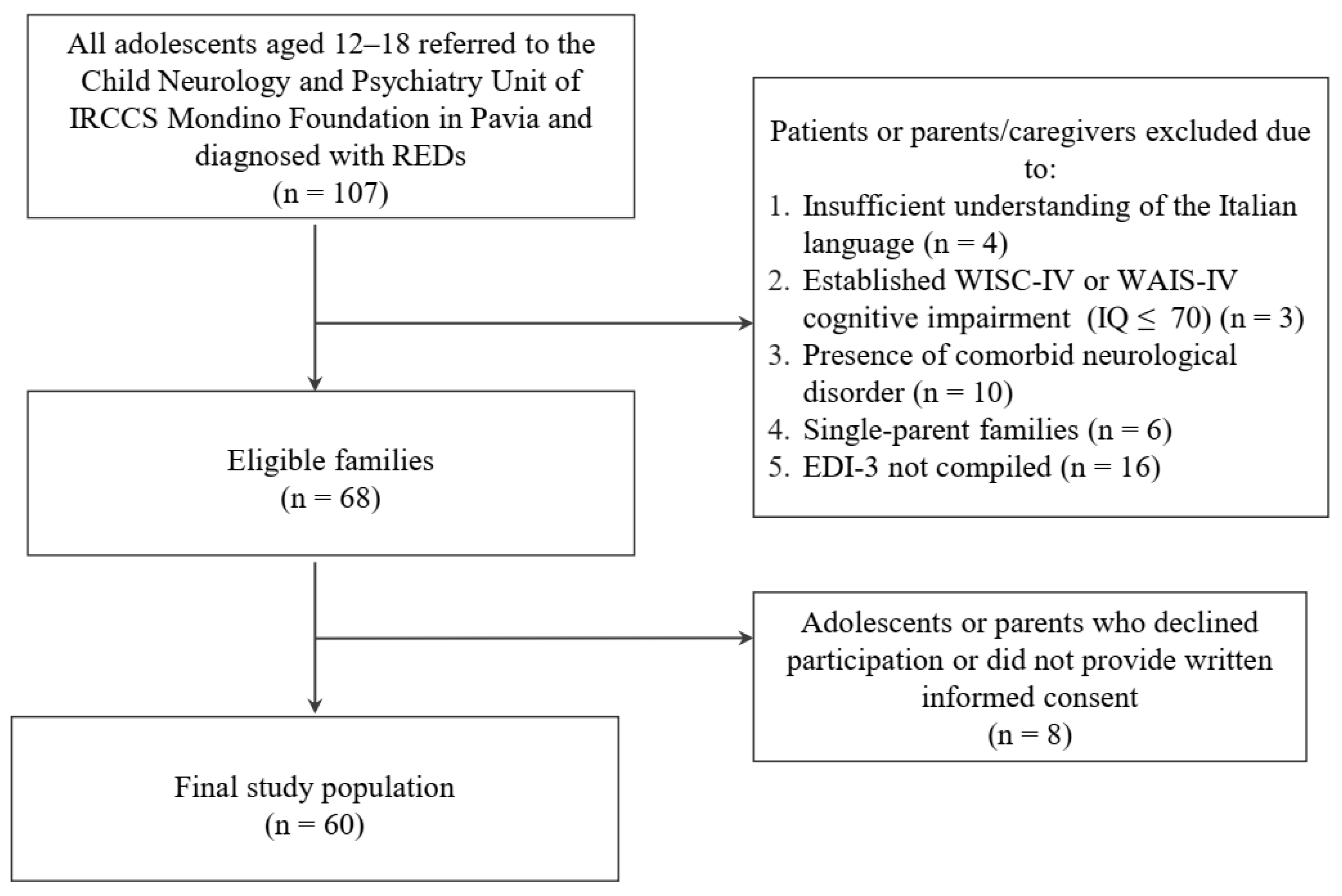
2.1. Participants
2.2. Procedures and Measures
2.3. Plan of Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| A-AN | atypical anorexia nervosa |
| AC | affective contact |
| AN | anorexia nervosa |
| B | bulimia |
| BD | body dissatisfaction |
| BMI | body mass index |
| DT | drive for thinness |
| EDI-3 | Eating Disorder Inventory-3 |
| EDRC | Eating Disorder Risk Composite |
| FA | focal attention |
| IPC | Interpersonal Problems Composite |
| K-SADS-PL | Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime |
| LTPc | Lausanne Trilogue Play—clinical version |
| OR | organization |
| PA | participation |
| REDs | restrictive eating disorders |
| SCID-5-PD | Structured Clinical Interview for DSM-5—Personality Disorders |
References
- Mensi, M.M.; Orlandi, M.; Rogantini, C.; Provenzi, L.; Chiappedi, M.; Criscuolo, M.; Castiglioni, M.C.; Zanna, V.; Borgatti, R. Assessing Family Functioning Before and After an Integrated Multidisciplinary Family Treatment for Adolescents With Restrictive Eating Disorders. Front. Psychiatry 2021, 12, 653047. [Google Scholar] [CrossRef] [PubMed]
- Keski-Rahkonen, A.; Mustelin, L. Epidemiology of Eating Disorders in Europe: Prevalence, Incidence, Comorbidity, Course, Consequences, and Risk Factors. Curr. Opin. Psychiatry 2016, 29, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Smink, F.R.E.; Van Hoeken, D.; Hoek, H.W. Epidemiology of Eating Disorders: Incidence, Prevalence and Mortality Rates. Curr. Psychiatry Rep. 2012, 14, 406–414. [Google Scholar] [CrossRef]
- Treasure, J.; Claudino, A.M.; Zucker, N. Eating Disorders. Lancet 2010, 375, 583–593. [Google Scholar] [CrossRef]
- Krug, I.; Binh Dang, A.; Granero, R.; Agüera, Z.; Sánchez, I.; Riesco, N.; Jimenez-Murcia, S.; Menchón, J.M.; Fernandez-Aranda, F. Drive for Thinness Provides an Alternative, More Meaningful, Severity Indicator than the DSM-5 Severity Indices for Eating Disorders. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2021, 29, 482–498. [Google Scholar] [CrossRef]
- Balottin, L.; Mannarini, S.; Mensi, M.M.; Chiappedi, M.; Gatta, M. Triadic Interactions in Families of Adolescents with Anorexia Nervosa and Families of Adolescents with Internalizing Disorders. Front. Psychol. 2017, 7, 1–13. [Google Scholar] [CrossRef]
- Holtom-Viesel, A.; Allan, S. A Systematic Review of the Literature on Family Functioning across All Eating Disorder Diagnoses in Comparison to Control Families. Clin. Psychol. Rev. 2014, 34, 29–43. [Google Scholar] [CrossRef]
- Balottin, L.; Mannarini, S.; Mensi, M.M.; Chiappedi, M.; Balottin, U. Are Family Relations Connected to the Quality of the Outcome in Adolescent Anorexia Nervosa? An Observational Study with the Lausanne Trilogue Play. Clin. Psychol. Psychother. 2018, 25, 785–796. [Google Scholar] [CrossRef] [PubMed]
- Batista, M.; Žigić Antić, L.; Žaja, O.; Jakovina, T.; Begovac, I. Predictors of Eating Disorder Risk In Anorexia Nervosa Adolescents. Acta Clin. Croat. 2018, 57, 399–410. [Google Scholar] [CrossRef]
- Arcelus, J.; Haslam, M.; Farrow, C.; Meyer, C. The Role of Interpersonal Functioning in the Maintenance of Eating Psychopathology: A Systematic Review and Testable Model. Clin. Psychol. Rev. 2013, 33, 156–167. [Google Scholar] [CrossRef]
- Hoffman, E.R.; Gagne, D.A.; Thornton, L.M.; Klump, K.L.; Brandt, H.; Crawford, S.; Fichter, M.M.; Halmi, K.A.; Johnson, C.; Jones, I.; et al. Understanding the Association of Impulsivity, Obsessions, and Compulsions with Binge Eating and Purging Behaviours in Anorexia Nervosa. Eur. Eat. Disord. Rev. 2012, 20, e129–e136. [Google Scholar] [CrossRef] [PubMed]
- Connan, F.; Troop, N.; Landau, S.; Campbell, I.C.; Treasure, J. Poor Social Comparison and the Tendency to Submissive Behavior in Anorexia Nervosa. Int. J. Eat. Disord. 2007, 40, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Martín, A.; Novalbos Ruiz, J.P.; Martínez Nieto, J.M.; Escobar Jiménez, L.; Castro de Haro, A.L. Epidemiological Study of the Influence of Family and Socioeconomic Status in Disorders of Eating Behaviour. Eur. J. Clin. Nutr. 2004, 58, 846–852. [Google Scholar] [CrossRef]
- Fivaz-Depeursinge, E.; Corboz-Warnery, A. The Primary Triangle: A Developmental Systems View of Mothers, Fathers and Infants; Basic Books: New York, NY, USA, 1999. [Google Scholar]
- Muratore, A.F.; Attia, E. Current Therapeutic Approaches to Anorexia Nervosa: State of the Art. Clin. Ther. 2021, 43, 85–94. [Google Scholar] [CrossRef]
- Springall, G.; Caughey, M.; Zannino, D.; Cheung, M.; Burton, C.; Kyprianou, K.; Yeo, M. Family-Based Treatment for Adolescents with Anorexia Nervosa: A Long-Term Psychological Follow-Up. J. Paediatr. Child Health 2022, 58, 1642–1647. [Google Scholar] [CrossRef]
- Liu, J.; Rockwell, R.E.; Kaye, W.H.; Wierenga, C.E.; Brown, T.A. Family Functioning and Eating Disorders Treatment in a Partial Hospitalization Program in Adolescent Females with Eating Disorders. Int. J. Eat. Disord. 2022, 55, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Harris, B.A.; Scharff, A.; Smith, M.; Brooks, G.; Thompson-Brenner, H.; Boswell, J.F. Trajectories of Interpersonal Problems in Residential Eating Disorder Treatment: Exploring the Influence of Primary Diagnosis. Clin. Psychol. Psychother. 2022, 29. [Google Scholar] [CrossRef]
- Malagoli Togliatti, M.; Mazzoni, S. Osservare, Valutare, e Sostenere La Relazione Genitori-Figli. Il Lausanne Trilogue Play Clinico [Observe, Evaluate, and Support the Parent-Child Relationship. The Clinical Lausanne Trilogue Play]; Raffaello Cortina Editore: Milan, Italy, 2006. [Google Scholar]
- Mensi, M.M.; Balottin, L.; Rogantini, C.; Orlandi, M.; Galvani, M.; Figini, S.; Chiappedi, M.; Balottin, U. Focus on Family Functioning in Anorexia Nervosa: New Perspectives Using the Lausanne Trilogue Play. Psychiatry Res. 2020, 288, 112968. [Google Scholar] [CrossRef]
- Taylor, G.J.; Parker, J.D.; Bagby, R.M.; Bourke, M.P. Relationships between Alexithymia and Psychological Characteristics Associated with Eating Disorders. J. Psychosom. Res. 1996, 41, 561–568. [Google Scholar] [CrossRef]
- Bomba, M.; Corbetta, F.; Gambera, A.; Nicosia, F.; Bonini, L.; Neri, F.; Tremolizzo, L.; Nacinovich, R. Heart Rate Variability in Adolescents with Functional Hypothalamic Amenorrhea and Anorexia Nervosa. Psychiatry Res. 2014, 215, 406–409. [Google Scholar] [CrossRef]
- Duclos, J.; Dorard, G.; Berthoz, S.; Curt, F.; Faucher, S.; Falissard, B.; Godart, N. Expressed Emotion in Anorexia Nervosa: What Is inside the “Black Box”? Compr. Psychiatry 2014, 55, 71–79. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Kaufman, J.; Birmaher, B.; Axelson, D.; Pereplitchikova, F.; Brent, D.; Ryan, N. Schedule for Affective Disorders and Schizophrenia for School-Aged Children: Present and Lifetime Version (K-SADS-PL) DSM-5; Child and Adolescent Research and Education: New Heaven, CT, USA, 2016. [Google Scholar]
- Kaufman, J.; Birmaher, B.; Rao, U.; Ryan, N.; di Sogos, C.; Di Noia, S.P.; Fioriello, F.; Picchiotti, G. K-SADS-PL DSM-5. Intervista Diagnostica per La Valutazione Dei Disturbi Psicopatologici in Bambini e Adolescenti. [Schedule for Affective Disorders and Schizophrenia for School-Aged Children: Present and Lifetime Version (K-SADS-PL) DSM-5]; Erickson: Trento, Italy, 2019. [Google Scholar]
- Wechsler, D. Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV); Giunti Organizzazioni Speciali: Florence, Italy, 2003. [Google Scholar]
- Wechsler, D. Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV); Giunti Organizzazioni Speciali: Florence, Italy, 2008. [Google Scholar]
- First, M.B.; Williams, J.B.W.; Janet, S.B.; Spitzer, R.L. Structured Clinical Interview for DSM-5. Personality Disorders (SCID-5-PD); American Psychiatric Association: Washington, DC, USA, 2017. [Google Scholar]
- Mensi, M.M. Available online: http://doi.org/20211006_REDs_LTP-EDI_MMM_01 (accessed on 22 December 2022).
- Garner, D. Eating Disorder Inventory-3 (EDI-3). Int. J. Eat. Disord. 2004, 35, 478–479. [Google Scholar]
- Giannini, M.; Pannocchia, L.; Dalle Grave, R.; Muratori, F.; Viglione, V. EDI-3 Eating Disorder Inventory-3. Manuale. Adattamento Italiano; Giunti OS—Organizzazioni Speciali: Florence, Italy, 2008. [Google Scholar]
- Vansteelandt, K.; Pieters, G.; Vanderlinden, J.; Probst, M. Body Dissatisfaction Moderates Weight Curves in the Inpatient Treatment of Anorexia Nervosa. Int. J. Eat. Disord. 2010, 43, 694–700. [Google Scholar] [CrossRef]
- Garner, D.M.; Garner, M.V.; Rosen, L.W. Anorexia Nervosa “Restricters” Who Purge: Implications for Subtyping Anorexia Nervosa. Int. J. Eat. Disord. 1993, 13, 171–185. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows; IBM: Armonk, NY, USA, 2020. [Google Scholar]
- R Core. Team R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022. [Google Scholar]
- Lyke, J.; Matsen, J. Family Functioning and Risk Factors for Disordered Eating. Eat. Behav. 2013, 14, 497–499. [Google Scholar] [CrossRef]
- Anastasiadou, D.; Medina-Pradas, C.; Sepulveda, A.R.; Treasure, J. A Systematic Review of Family Caregiving in Eating Disorders. Eat. Behav. 2014, 15, 464–477. [Google Scholar] [CrossRef] [PubMed]
- Felker, K.R.; Stivers, C. The Relationship of Gender and Family Environment to Eating Disorder Risk in Adolescents. Adolescence 1994, 29, 821–834. [Google Scholar] [PubMed]
- Mensi, M.M.; Criscuolo, M.; Vai, E.; Rogantini, C.; Orlandi, M.; Ballante, E.; Zanna, V.; Mazzoni, S.; Balottin, U.; Borgatti, R. Perceived and Observed Family Functioning in Adolescents Affected by Restrictive Eating Disorders. Fam. Relat. 2022, 71, 724–736. [Google Scholar] [CrossRef]
- Balottin, L.; Nacinovich, R.; Bomba, M.; Mannarini, S. Alexithymia in Parents and Adolescent Anorexic Daughters: Comparing the Responses to TSIA and TAS-20 Scales. Neuropsychiatr. Dis. Treat. 2014, 10, 1941–1951. [Google Scholar] [CrossRef]
- Gatta, M.; Balottin, L.; Mannarini, S.; Chesani, G.; Del Col, L.; Spoto, A.; Battistella, P.A. Familial Factors Relating to Alexithymic Traits in Adolescents with Psychiatric Disorders. Clin. Psychol. 2017, 21, 252–262. [Google Scholar] [CrossRef]
- Kooiman, C.G.; van Rees Vellinga, S.; Spinhoven, P.; Draijer, N.; Trijsburg, R.W.; Rooijmans, H.G.M. Childhood Adversities as Risk Factors for Alexithymia and Other Aspects of Affect Dysregulation in Adulthood. Psychother. Psychosom. 2004, 73, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Lock, J.; La Via, M.C. Practice Parameter for the Assessment and Treatment of Children and Adolescents with Eating Disorders. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 412–425. [Google Scholar] [CrossRef] [PubMed]
| Phase | Description |
|---|---|
| 1 | Mother/father interacts with son/daughter, while the other parent is simply present. |
| 2 | Father/mother interacts with son/daughter, while the other parent is simply present. |
| 3 | The parents interact together with their son/daughter. |
| 4 | The parents continue to interact with each other without involving the son/daughter. |
| Functional Level | Description | How to Measure |
|---|---|---|
| Participation (PA) | Ability to get involved in the same interactive space, getting in touch with the other family members. It indicates the inclusion or the exclusion of a member of the triad. | Note how the participant places his body in the inter-active field, if he/she sits correctly, and if he/she orients his/her body to other family members and the task. |
| Organization (OR) | The capacity of each participant to play a role coherent with the different parts of the play: the roles played by each parent and the son/daughter have to be different according to the different phases | Note if each participant plays her/his role. |
| Focal Attention (FA) | Ability to reach and maintain a joint attentive focus shared by the triad during the play. | Note whether each of the participants (regardless of their role in a specific phase) pays attention to the interactive elements, ongoing activities, and actions of the other participants, sharing meanings with each other through glances, gestures, and words. |
| Affective Contact (AC) | Emotional sharing and the reciprocity and communion of affections. | Note ways of looking, physical contact, verbal communication of affections, and reinforcements within the triad |
| Complete Data | |||
|---|---|---|---|
| (n = 60) | |||
| Mean | SD | ||
| Age (months) | 180.12 | 111.480 | |
| Weight, kg | 40.773 | 9.8736 | |
| Height, cm | 158.133 | 7.1247 | |
| BMI kg/m2 | 16.26 | 3.5995 | |
| Weight loss, kg | 95.958 | 274.7674 | |
| N | % | ||
| Sex | Female | 59 | 98% |
| Male | 1 | 2% | |
| N | % | ||
| Patient’s social withdrawal | Yes | 5 | 8% |
| No | 55 | 92% | |
| Patient’s school withdrawal | Yes | 6 | 10% |
| No | 54 | 90% | |
| Menarche | Yes | 46 | 77% |
| No | 14 | 23% | |
| Period | Primary amenorrhea | 9 | 20% |
| Secondary amenorrhea | 29 | 63% | |
| Irregular period | 8 | 17% | |
| Binge eating | Yes | 17 | 28% |
| No | 43 | 72% | |
| Dysmorphophobia | Yes | 52 | 87% |
| No | 8 | 13% | |
| Obsessive-compulsive behaviours | Yes | 25 | 42% |
| No | 35 | 58% | |
| Hyperactivity | Yes | 31 | 52% |
| No | 29 | 48% | |
| Elimination conducts | Yes | 15 | 25% |
| No | 45 | 75% | |
| Family history of psychiatric disorders | Yes | 37 | 62% |
| No | 23 | 38% | |
| Family history of eating disorders | Yes | 4 | 7% |
| No | 56 | 93% | |
| Treatment | Day hospital | 7 | 14% |
| Diet | 21 | 42% | |
| Psychiatric | 22 | 44% | |
| Mean | SD | ||
| Paternal educational level | 61.97 | 216.813 | |
| Maternal educational level | 62.82 | 216.607 | |
| Family socioeconomic status | 103.500 | 241.6933 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baradel, G.; Provenzi, L.; Chiappedi, M.; Orlandi, M.; Vecchio, A.; Borgatti, R.; Mensi, M.M., on behalf of the Mondino Foundation Eating Disorders Clinical and Research Group. The Family Caregiving Environment Associates with Adolescent Patients’ Severity of Eating Disorder and Interpersonal Problems: A Cross-Sectional Study. Children 2023, 10, 237. https://doi.org/10.3390/children10020237
Baradel G, Provenzi L, Chiappedi M, Orlandi M, Vecchio A, Borgatti R, Mensi MM on behalf of the Mondino Foundation Eating Disorders Clinical and Research Group. The Family Caregiving Environment Associates with Adolescent Patients’ Severity of Eating Disorder and Interpersonal Problems: A Cross-Sectional Study. Children. 2023; 10(2):237. https://doi.org/10.3390/children10020237
Chicago/Turabian StyleBaradel, Giorgia, Livio Provenzi, Matteo Chiappedi, Marika Orlandi, Arianna Vecchio, Renato Borgatti, and Martina Maria Mensi on behalf of the Mondino Foundation Eating Disorders Clinical and Research Group. 2023. "The Family Caregiving Environment Associates with Adolescent Patients’ Severity of Eating Disorder and Interpersonal Problems: A Cross-Sectional Study" Children 10, no. 2: 237. https://doi.org/10.3390/children10020237
APA StyleBaradel, G., Provenzi, L., Chiappedi, M., Orlandi, M., Vecchio, A., Borgatti, R., & Mensi, M. M., on behalf of the Mondino Foundation Eating Disorders Clinical and Research Group. (2023). The Family Caregiving Environment Associates with Adolescent Patients’ Severity of Eating Disorder and Interpersonal Problems: A Cross-Sectional Study. Children, 10(2), 237. https://doi.org/10.3390/children10020237








