A Creative and Movement-Based Blended Intervention for Children in Outpatient Residential Care: A Mixed-Method, Multi-Center, Single-Arm Feasibility Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Design
2.3. Participants
2.4. Measures
2.4.1. Measures for Children and Adolescents
- (1)
- Baseline sociodemographic variables and media usage. Besides demographic variables, child hobbies, and interests, media usage and changes in media consumption as a result of the pandemic were assessed at baseline T0. The items regarding media usage were: (1) Media/device usage (“Which of the following devices do you use most often? Rate the frequency from 1 (most often) to 4 (least often) for each of the following devices: cell phone—computer/laptop—tablet/game console”); (2) Daily smartphone usage (“On average, how much time do you spend on your smartphone per day? (<30 min—30–60 min—1–2 h—3–4 h—>5 h”)); (3) Change in media consumption since the pandemic (“How has your media consumption (= time spent on laptop, smartphone, or tablet) changed since the pandemic? (five-step response format: significantly more—significantly less”)); (4) Subjective feeling about own media consumption (“How do you feel about your amount of media consumption? (five-step response format: very good—very bad”)). The questionnaire is available in the Supplementary Materials S1.
- (2)
- Child psychological symptoms. We used the Beck’s Youth Inventory (BYI-2) [26], a validated and manualized German version of the BYI-2 [27]. This questionnaire includes five scales, 20 items each: Depression (BDI-Y), Anxiety (BAI-Y), Anger (BANI-Y), Disruptive Behavior (BDBI-Y), and Self-worth (BSCI-Y). Participants rated the total of 100 items on a four-point Likert scale as to how often this applied to them in the last 2 weeks (“never—always”). The Cronbach Alpha of the various scales can be rated as good to very good for the baseline measurement (0.87–0.94) as well as for the post-measurement (0.86–0.94) within the current sample.
- (3)
- Intrapersonal and social resources. We used six subscales of the Resource Questionnaire for Children and Adolescents (FRKJ 8–16) [28], a validated and manualized German questionnaire, which is designed to assess the intrapersonal and social resources of children and adolescents. The six subscales capture intrapersonal resources (empathy and perspective-taking, self-efficacy, self-esteem, sense of coherence, optimism, and self-control) with a total of 36 items. Cronbach alpha reliabilities were adequate to good (0.67–0.80) in the baseline-survey as well as in the post-measurement (0.66–0.84) in the current sample.
- (4)
- Structured interview. The structured interview collects feedback on the app, on the face-to-face activities, and on the blended care intervention in general. For the app-related information, the children provided their current well-being after using the app, their liking of the design, as well as a possible recommendation to others. They also rate the activities (theater, nature, art, yoga) by favorability and give a preference between app or face-to-face activity. Finally, we asked the children if they would have preferred a longer project duration and what they like best about the project. The interview was only implemented in the T1 post measurement and can be found in the Supplementary Materials S2.
2.4.2. Instruments for Residential Staff
- (1)
- Child and parent-related risk factors. Using a self-generated questionnaire with 9 items, we obtained information regarding preexisting factors affecting the intervention execution, child-centered and parental risk factors regarding mental health distress during the COVID-19 pandemic, and participants’ residential care histories: (1) Child’s dyslexia (“Does the child or adolescent have a reading disability?”); (2) Child’s current crises or problems (“Are there currently problems/crises with the child/adolescent? (If yes, please state briefly)”); (3) Parental contact (“Does the child or adolescent have regular contact with parents?”); (4) Frequency of contact (“How often has the child/adolescent contact with at least one parent?”); as well as (5) History of connection to the facility (“How long does the child/adolescent attend the facility?”) and (6) History of connection to the youth welfare office (“How long has the child been involved with the youth welfare office?”) were obtained. Parent-centered information, such as (7) Migration background (“Do the parents have a migration background?”) and (8) Mental illness (“Does at least one parent or guardian of the child/adolescent have a mental illness?”) were also collected. Information to a respective DSM-5 diagnosis for the mentally ill person could be given if present (9). The questionnaire can be found in the Supplementary Materials S3.
- (2)
- Structured Interview for the feasibility and acceptance of the blended care intervention. The 15 item-structured interview was conducted at T1 within the facility by a trained research assistant. Particularly, perceived strengths and suggestions for improvement of the intervention were explored, the app was evaluated by the staff, and feedback on the impression of children’s and adolescent´s acceptance of the intervention regarding usage and app design was collected. The interview of the residential staff is available in the Supplementary Materials S4.
2.5. Blended Creative and Movement-Oriented Intervention
2.5.1. Procedure
2.5.2. Mondori App
2.5.3. Creative and Movement Based Face-to-Face Group Intervention
2.6. Data Analysis
2.6.1. Drop Out Analyses
2.6.2. Missing Data
3. Results
3.1. Baseline Data
3.1.1. Sample Characteristics
3.1.2. Media Usage and Prior Experiences with Creative and Movement-based Activities
3.1.3. Baseline Data on Child Psychological Symptoms and Resources
3.1.4. Risk Factors
3.2. Acceptance and Feasibility Results
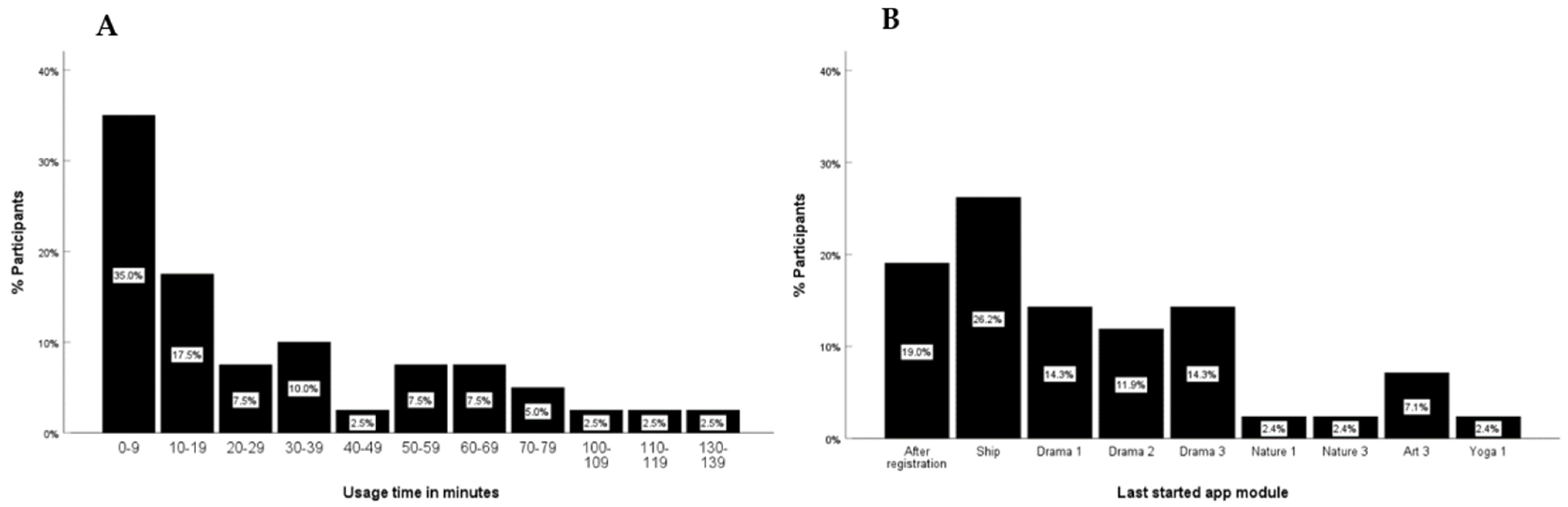
Acceptance and Feasibility of the Mondori App
3.3. Qualitative Interviews Regarding Mondori App
Acceptance and Feasibility of the Face-to-Face Activities
3.4. Qualitative Data Regarding Face-to-Face Activities
Acceptance and Feasibility of a Blended Intervention
3.5. Quantitative Effectiveness Outcomes
3.5.1. Intervention Effectiveness Data on Child Psychological Symptoms and Resources
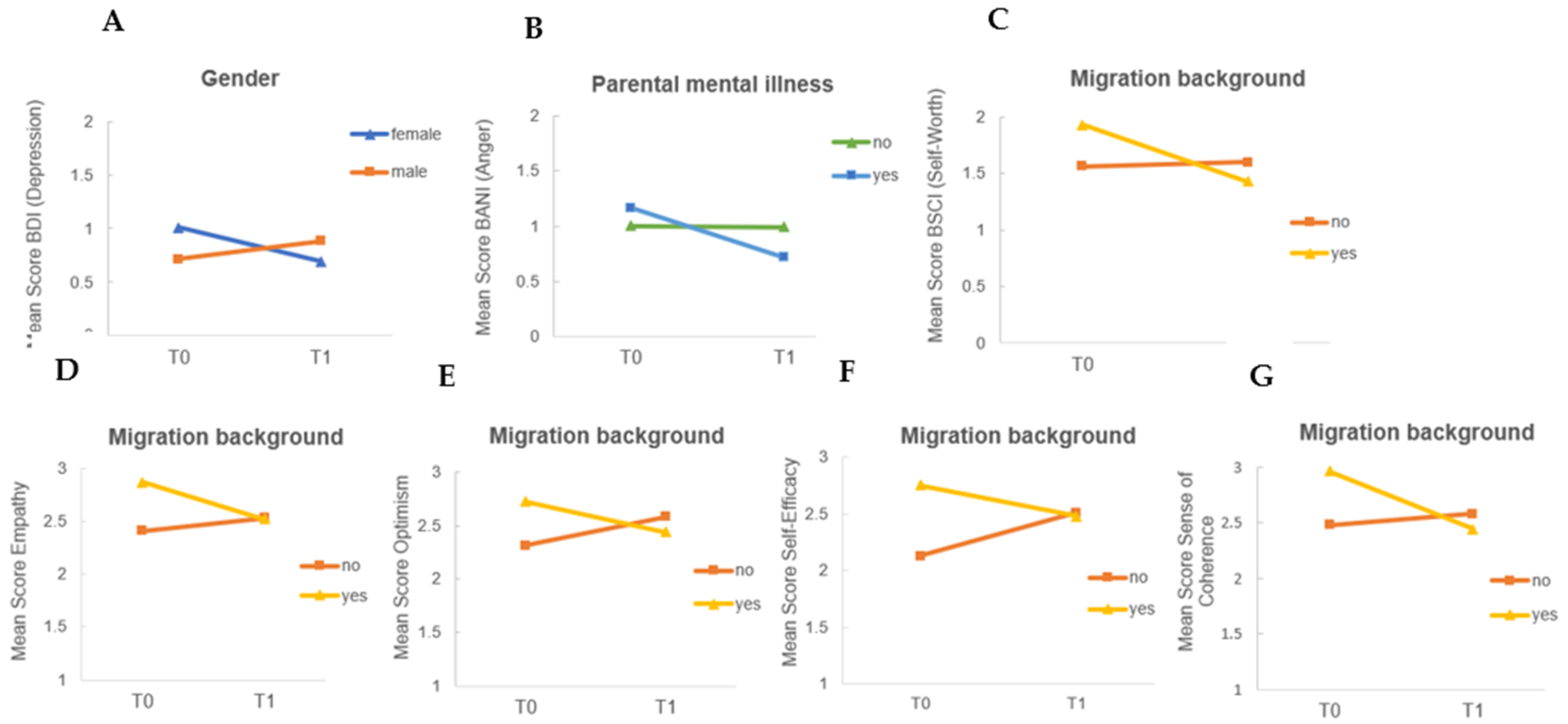
3.5.2. Effects of Risk Factors on Outcome Change Score
4. Discussion
5. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Calvano, C.; Engelke, L.; Di Bella, J.; Kindermann, J.; Renneberg, B.; Winter, S. Families in the COVID-19 pandemic: Parental stress, parent mental health and the occurrence of adverse childhood experiences—Results of a representative survey in Germany. Eur. Child Adolesc. Psychiatry 2022, 31, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Patrick, S.W.; Henkhaus, L.E.; Zickafoose, J.S.; Lovell, K.; Halvorson, A.; Loch, S.; Letterie, M.; Davis, M.M. Well-being of parents and children during the COVID-19 pandemic: A national survey. Pediatrics 2020, 146, e2020016824. [Google Scholar] [CrossRef] [PubMed]
- Al Gharaibeh, F.; Gibson, L. The impact of COVID-19 quarantine measures on the mental health of families. J. Soc. Work 2022, 22, 655–673. [Google Scholar] [CrossRef] [PubMed]
- Luijten, M.A.J.; van Muilekom, M.M.; Teela, L.; Polderman, T.J.C.; Terwee, C.B.; Zijlmans, J.; Klaufus, L.; Popma, A.; Oostrom, K.J.; van Oers, H.A.; et al. The impact of lockdown during the COVID-19 pandemic on mental and social health of children and adolescents. Qual. Life Res. 2021, 30, 2795–2804. [Google Scholar] [CrossRef]
- Reiss, F.; Meyrose, A.K.; Otto, C.; Lampert, T.; Klasen, F.; Ravens-Sieberer, U. Socioeconomic status, stressful life situations and mental health problems in children and adolescents: Results of the German BELLA cohort-study. PLoS ONE 2019, 14, e0213700. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Kaman, A.; Otto, C.; Adedeji, A.; Napp, A.-K.; Becker, M.; Blanck-Stellmacher, U.; Löffler, C.; Schlack, R.; Hölling, H.; et al. Mental health and psychological burden of children and adolescents during the first wave of the COVID-19 pandemic-results of the COPSY study. Bundesgesundheitsblatt Gesundh. Gesundh. 2021, 64, 1512–1521. [Google Scholar] [CrossRef]
- Costa, M.; Matos, P.M.; Santos, B.; Carvalho, H.; Ferreira, T.; Mota, C.P. We stick together! COVID-19 and psychological adjustment in youth residential car. Child Abus. Negl. 2022, 130, 105370. [Google Scholar] [CrossRef]
- Jones, B.; Woolfenden, S.; Pengilly, S.; Breen, C.; Cohn, R.; Biviano, L.; Johns, A.; Worth, A.; Lamb, R.; Lingam, R.; et al. COVID-19 pandemic: The impact on vulnerable children and young people in Australia. J. Paediatr. Child Health 2020, 56, 1851–1855. [Google Scholar] [CrossRef]
- Montserrat, C.; Garcia-Molsosa, M.; Llosada-Gistau, J.; Sitjes-Figueras, R. The views of children in residential care on the COVID-19 lockdown: Implications for and their well-being and psychosocial intervention. Child Abus. Negl. 2021, 120, 105182. [Google Scholar] [CrossRef]
- Rosenberg, J.; McDonough Ryan, P.; O’Brien, C.; Ganjavi, F.; Sharifi, M. Pilot Wellness Program with Adapted Social–Emotional Learning and COVID-19 Curriculum for Refugee Youth. Health Educ. Behav. 2022, 49, 17–25. [Google Scholar] [CrossRef]
- Cusinato, M.; Iannattone, S.; Spoto, A.; Poli, M.; Moretti, C.; Gatta, M.; Miscioscia, M. Stress, resilience, and well-being in Italian children and their parents during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 8297. [Google Scholar] [CrossRef]
- Cui, Y.; Li, Y.; Zheng, Y. Mental health services for children in China during the COVID-19 pandemic: Results of an expert-based national survey among child and adolescent psychiatric hospitals. Eur. Child Adolesc. Psychiatry 2020, 29, 743–748. [Google Scholar] [CrossRef]
- Xue, Q.; Xie, X.; Liu, Q.; Zhou, Y.; Zhu, K.; Wu, H.; Wan, Z.; Feng, Y.; Meng, H.; Zhang, J.; et al. Knowledge, attitudes, and practices towards COVID-19 among primary school students in Hubei Province, China. Child. Youth Serv. Rev. 2021, 120, 105735. [Google Scholar] [CrossRef]
- Shoshani, A.; Kor, A. The mental health effects of the COVID-19 pandemic on children and adolescents: Risk and protective factors. Psychol. Trauma Theory Res. Pract. Policy 2022, 14, 1365–1373. [Google Scholar] [CrossRef]
- Alves, J.; Yunker, A.G.; DeFendis, A.; Xiang, A.H.; Page, K.A. BMI status and associations between affect, physical activity and anxiety among US children during COVID-19. Pediatr. Obes. 2021, 16, e12786. [Google Scholar] [CrossRef]
- Decosimo, A.; Hanson, J.; Quinn, M.; Badu, P.; Smith, E.G. Playing to live: Outcome evaluation of a community-based psychosocial expressive arts program for children during the Liberian Ebola epidemic. Glob. Ment. Health 2019, 6, e3. [Google Scholar] [CrossRef]
- Cahill, S.; Egan, B.E.; Seber, J. Activity-and occupation-based interventions to support mental health, positive behavior, and social participation for children and youth: A systematic review. Am. J. Occup. Ther. 2020, 74, 17402180020p1–7402180020p28. [Google Scholar] [CrossRef]
- Malboeuf-Hurtubise, C.; Léger-Goodes, T.; Mageau, G.A.; Joussemet, M.; Herba, C.; Chadi, N.; Lefrançois, D.; Camden, C.; Bussières, È.-L.; Taylor, G.; et al. Philosophy for children and mindfulness during COVID-19: Results from a randomized cluster trial and impact on mental health in elementary school students. Prog. Neuro Psychopharmacol. Biol. Psychiatry 2021, 107, 110260. [Google Scholar] [CrossRef]
- Boldt, K.; Coenen, M.; Movsisyan, A.; Voss, S.; Rehfuess, E.; Kunzler, A.; Lieb, K.; Jung-Sievers, C. Interventions to ameliorate the psychosocial effects of the COVID-19 pandemic on children—A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 2361. [Google Scholar] [CrossRef]
- Tymofiyeva, O.; Hu, M.Y.; Sipes, B.S.; Jakary, A.; Glidden, D.V.; Jariwala, N.; Bhandari, S.; Parks, K.C.; Nguyen, C.; Henje, E.; et al. A Feasibility Study of a Remotely-Delivered Mindfulness-Based Training for Adolescents During the COVID-19 Pandemic. Front. Psychiatry 2022, 13, 645. [Google Scholar] [CrossRef]
- Pavarini, G.; Reardon, T.; Hollowell, A.; Bennett, V.; Lawrance, E.; Pinfold, V.; Singh, I. Online peer support training to promote adolescents’ emotional support skills, mental health and agency during COVID-19: Randomised controlled trial and qualitative evaluation. Eur. Child Adolesc. Psychiatry 2022. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Wang, W.; Zhong, Y.; Wu, F.; Zhu, Z.; Tham, Y.C.; Lamoureux, E.; Xiao, L.; Zhu, E.; Liu, H.; et al. A peer-to-peer live-streaming intervention for children during COVID-19 homeschooling to promote physical activity and reduce anxiety and eye strain: Cluster randomized controlled trial. J. Med. Internet Res. 2021, 23, e24316. [Google Scholar] [CrossRef] [PubMed]
- Zepeda, M.S.; Deighton, S.; Markova, V.; Madsen, J.W.; Racine, N. iCOPE with COVID-19: A Brief Telemental Health Intervention for Children and Adolescents during the COVID-19 Pandemic. Cogn. Behav. Pract. 2021. [Google Scholar] [CrossRef] [PubMed]
- Clarke, A.M.; Kuosmanen, T.; Barry, M.M. A systematic review of online youth mental health promotion and prevention interventions. J. Youth Adolesc. 2021, 44, 90–113. [Google Scholar] [CrossRef] [PubMed]
- Eldridge, S.M.; on behalf of the PAFS consensus group; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016, 2, 64. [Google Scholar] [CrossRef]
- Beck, J.S. Beck Youth Inventories: Manual, 2nd ed.; Pearson: San Antonio, TX, USA, 2005. [Google Scholar]
- Siefen, G.; Busch, J. German Adaptation and Standardization of the Beck Youth Inventories, 2nd ed.; Pearson Clinical Assessment: Frankfurt, Germany, 2018. [Google Scholar]
- Lohaus, A.; Nussbeck, F.W. FRKJ 8-16 Fragebogen zu Ressourcen im Kindes-und Jugendalter, 1st ed.; Hogrefe: Göttingen, Germany, 2016. [Google Scholar]
- Schlarb, A. Praxisbuch KVT mit Kindern und Jugendlichen. Störungsspezifische Strategien und Leitfäden; Beltz-Verlag: Weinheim, Germany, 2012. [Google Scholar]
- Schulze, U.M.; Kliegl, K.; Mauser, C.; Rapp, M.; Allroggen, M.; Fegert, J.M. ECHT STARK! Ein Manual für die Arbeit mit Kindern Psychisch Kranker und Suchtkranker Eltern; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Michalak, J.; Heidenreich, T.; Williams, J.G.; Meibert, P. Achtsamkeitsübungen für die Klinische Praxis und den Klinischen Alltag; Hogref: Boston, MA, USA, 2012. [Google Scholar]
- Rashid, T.; Seligman, M.P. Positive Psychotherapy: Clinician Manual; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- Serra, G.; Scalzo, L.L.; Giuffrè, M.; Ferrara, P.; Corsello, G. Smartphone use and addiction during the coronavirus disease 2019 (COVID-19) pandemic: Cohort study on 184 Italian children and adolescents. Ital. J. Pediatr. 2021, 47, 150. [Google Scholar] [CrossRef]
- Donovan, E.; Rodgers, F.; Cousineau, T.; McGowan, K.; Luk, S.; Yates, K.; Franko, D.L. Brief report: Feasibility of a mindfulness and self-compassion based mobile intervention for adolescents. J. Adolesc. 2016, 53, 217–221. [Google Scholar] [CrossRef]
- Pramana, G.; Parmanto, B.; Kendall, P.C.; Silk, J.S. The SmartCAT: An m-health platform for ecological momentary intervention in child anxiety treatment. Telemed. e-Health 2014, 20, 419–427. [Google Scholar] [CrossRef]
- Fleming, T.M.; de Beurs, D.; Khazaal, Y.; Gaggioli, A.; Riva, G.; Botella, C.; Baños, R.M.; Aschieri, F.; Bavin, L.M.; Kleiboer, A.; et al. Maximizing the impact of e-therapy and serious gaming: Time for a paradigm shift. Front. Psychiatry 2016, 7, 65. [Google Scholar] [CrossRef]
- National Collaborating Centre for Mental Health. E-Therapies systematic Review for Children and Young People with Mental Health Problems; NCCMH: Essex, UK, 2014. [Google Scholar]
- Grist, R.; Porter, J.; Stallard, P. Mental health mobile apps for preadolescents and adolescents: A systematic review. J. Med. Internet Res. 2017, 19, e7332. [Google Scholar] [CrossRef]
- Van Lieshout, S.; Mevissen, F.E.F.; Van Breukelen, G.; Jonker, M.; Ruiter, R.A.C. Make a move: A comprehensive effect evaluation of a sexual harassment prevention program in Dutch residential youth car. J. Interpers. Violence 2019, 34, 1772–1800. [Google Scholar] [CrossRef]
- Damnjanovic, M.; Lakic, A.; Stevanovic, D.; Jovanovic, A. Effects of mental health on quality of life in children and adolescents living in residential and foster care: A cross-sectional study. Epidemiol. Psychiatr. Sci. 2011, 20, 257–262. [Google Scholar] [CrossRef]
- Minnis, H.; Everett, K.; Pelosi, A.; Dunn, J.; Knapp, M. Children in foster care: Mental health, service use and costs. Eur. Child Adolesc. Psychiatry 2006, 15, 63–70. [Google Scholar] [CrossRef]
- De Swart, J.; Broek, H.V.D.; Stams, G.; Asscher, J.; Van der Laan, P.; Holsbrink-Engels, G.; Van der Helm, G. The effectiveness of institutional youth care over the past three decades: A meta-analysis. Child. Youth Serv. Rev. 2012, 34, 1818–1824. [Google Scholar] [CrossRef]
- Araban, M.; Montazeri, A.; Stein, L.A.R.; Karimy, M.; Mehrizi, A.A.H. Prevalence and factors associated with disruptive behavior among Iranian students during 2015: A cross-sectional study. Ital. J. Pediatr. 2020, 46, 85. [Google Scholar] [CrossRef]
- Vinayak, S.; Judge, J. Resilience and empathy as predictors of psychological wellbeing among adolescents. Int. J. Health Sci. Res. 2018, 8, 192–200. [Google Scholar]
- Pössel, P.; Adelson, J.L.; Hautzinger, M. A randomized trial to evaluate the course of effects of a program to prevent adolescent depressive symptoms over 12 months. Behav. Res. Ther. 2011, 49, 838–851. [Google Scholar] [CrossRef]
- Wiegand-Grefe, S.; Sell, M.; Filter, B.; Plass-Christl, A. Family functioning and psychological health of children with mentally ill parents. Int. J. Environ. Res. Public Health 2019, 16, 1278. [Google Scholar] [CrossRef]
- Leijdesdorff, S.; van Doesum, K.; Popma, A.; Klaassen, R.; van Amelsvoort, T. Prevalence of psychopathology in children of parents with mental illness and/or addiction: An up to date narrative review. Curr. Opin. Psychiatry 2017, 30, 312–317. [Google Scholar] [CrossRef]
- Wolke, D.; Waylen, A.; Samara, M.; Steer, C.; Goodman, R.; Ford, T.; Lamberts, K. Selective drop-out in longitudinal studies and non-biased prediction of behaviour disorders. Br. J. Psychiatry 2009, 195, 249–256. [Google Scholar] [CrossRef]
- Granero Pérez, R.; Ezpeleta, L.; Domenech, J.M. Features associated with the non-participation and drop out by socially-at-risk children and adolescents in mental-health epidemiological studies. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Dülsen, P.; Barck, K.; Daubmann, A.; Höller, A.; Zeidler, J.; Kilian, R.; Wiegand-Grefe, S.; Baumeister, H. Clinical-and Cost Effectiveness of a Guided Internet-Based Intervention for Children (12–18 Years) of Parents with Mental Disorders (iCHIMPS): Study Protocol of a Multicentered Cluster-Randomized Controlled Trial. Front. Digit. Health 2022, 4, 816412. [Google Scholar] [CrossRef] [PubMed]
- Reupert, A.; Maybery, D.; Bartholomew, C.; Cuff, R.; Foster, K.; Matar, J.; Pettenuzzo, L. The acceptability and effectiveness of an online intervention for youth with parents with a mental illness and/or substance use issue. J. Adolesc. Health 2020, 66, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Mood, C.; Jonsson, J.O.; Låftman, S.B. Immigrant integration and youth mental health in four European countries. Eur. Sociol. Rev. 2016, 32, 716–729. [Google Scholar] [CrossRef]
- Harker, K. Immigrant generation, assimilation and adolescent psychological well-being. Soc. Forces 2001, 79, 969–1004. [Google Scholar] [CrossRef]
- Motti-Stefanidi, F.; Masten, A.S. A resilience perspective on immigrant youth adaptation and development. In Handbook on Positive Development of Minority Children and Youth; Cabrera, N.J., Leyendecker, B., Eds.; Springer Science + Business Media: Berlin/Heidelberg, Germany, 2017; pp. 19–34. [Google Scholar]
- Yakeley, J. Shame, culture and mental health. Nord. J. Psychiatry 2018, 72 (Suppl. 1), S20–S22. [Google Scholar] [CrossRef]
- Bergin, A.D.; Vallejos, E.P.; Davies, E.B.; Daley, D.; Ford, T.; Harold, G.; Hetrick, S.; Kidner, M.; Long, Y.; Merry, S.; et al. Preventive digital mental health interventions for children and young people: A review of the design and reporting of research. NPJ Digit. Med. 2020, 3, 133. [Google Scholar] [CrossRef]


| Week | Island | Objective | Therapy Type | App Content | Face-to-Face Content |
|---|---|---|---|---|---|
| 1 | Ship | Setting goals, motivation | - | Defining own goals, creating own motivation sentences | T0 |
| 2 | Jungle | Emotion recognition and acceptance | Drama | Paraphrase emotions with body and face, writing a role play-script | Figure play with jungle animals, bodily and improvisational expression of emotions |
| 3 | Valley | Self-esteem | Nature | Encouraging braveness, meditation, seeing individual beauty of nature in oneself | Experience uniqueness of nature and create analogies with the self |
| 4 | Underwater | Activating resources | Art | Meditation, drawing internal and external resources | Meditation and creative creation of personal and external strengths |
| 5 | Ice | Setting boundaries | Yoga | Yoga-video, recognizing own boundaries, establishing rituals | Breathing exercises and asanas |
| 6 | - | Feedback and reflection | - | - | T1 |
| Variables | n (%) |
|---|---|
| Sociodemographic characteristics | |
| Mean age ± SD, years | 10.6 ± 1.7 |
| Male gender | 26 (57.8) |
| Cultural characteristics 1 | |
| German native language | 26 (53.1) |
| Parental migration background | 21 (42.9) |
| Psychological characteristics 1 | |
| Presence of current crisis 2 (=yes) | 25 (51.0) |
| Presence of reading disability (=yes) | 14 (28.6) |
| Mentally ill parent(s) 3 (=yes) | 21 (47.7) |
| Affiliation to residential care 1 | |
| Duration of the previous residence | |
| in respective facility | |
| <1 year | 14 (28.6) |
| 1–2 years | 13 (26.5) |
| 2–6 years | 14 (28.5) |
| >6 years | 1 (2.0) |
| Other previous youth welfare facility | |
| <1 year | 4 (8.2) |
| 1–2 years | 7 (14.3) |
| 2–6 years | 20 (40.8) |
| >6 years | 9 (18.4) |
| Contact with parent(s) 1 | |
| Yes | 39 (79.6) |
| Frequency | |
| daily | 18 (36.7) |
| weekly | 6 (12.3) |
| monthly | 10 (20.4) |
| annual | 1 (2.0) |
| Media Use and Media Consumption | n (%) |
|---|---|
| Most frequent device utilization | |
| Smartphone | 31 (68.9) |
| Laptop | 4 (8.9) |
| Tablet | 5 (11.1) |
| Game console | 2 (4.4) |
| Average time on smartphone/day | |
| <1 h | 8 (22.2) |
| 1–2 h | 14 (38.9) |
| 3–4 h | 2 (5.6) |
| >5 h | 12 (33.3) |
| Subjective app using confidence | |
| not confident (not, not at all confident) | 6 (15.0) |
| partly confident | 9 (22.5) |
| confident (confident, very confident) | 25 (62.5) |
| App preferences (3 most mentioned) | |
| TikTok | 14 (36.8) |
| YouTube | 14 (36.8) |
| Roblox | 12 (31.6) |
| Media consumption change 1 | |
| a lot more | 15 (37.5) |
| more | 5 (12.5) |
| same | 14 (35.0) |
| less | 6 (15.0) |
| Consumption evaluation | |
| positive (good, very good) | 27 (65.9)) |
| neutral | 10 (24.4) |
| poor (bad, very bad) | 4 (9.7) |
| Gender | Current Crisis | Parental Mental Illness | Migration Background | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | |||||||||||||
| Outcome | f (n = 16) | m (n = 24) | p-value | d [95% CI] | y (n = 22) | n (n = 17) | p-value | d [95% CI] | y (n = 20) | n (n = 19) | p-value | d [95% CI] | y (n = 17) | n (n = 20) | p-value | d [95% CI] |
| Self-worth | 1.83 (0.15) | 1.69 (0.11) | 0.429 | 0.258 [−0.38–0.89] | 1.70 (0.14) | 1.78 (0.11) | 0.689 | −0.130 [0.76–0.50] | 1.79 (0.13) | 1.68 (0.14) | 0.557 | −0.190 [−0.82–0.44] | 1.90 (0.14) | 1.60 (0.12) | 0.117 | 0.530 [−0.13–1.18] |
| Anxiety | 1.08 (0.18) | 0.875 (0.14) | 0.357 | 0.301 [−0.34–0.93] | 1.16 (0.17) | 0.80 (0.14) | 0.118 | 0.517 [−0.13–1.12] | 1.13 (0.18) | 0.87 (0.14) | 0.252 | −0.373 [−1.00–0.26] | 0.85 (0.15) | 1.12 (0.15) | 0.253 | −0.383 [−1.03–0.27] |
| Depression | 1.02 (0.21) | 0.72 (0.09) | 0.207 | 0.472 [−0.17–1.11] | 1.07 (0.16) | 0.65 (0.11) | 0.045 * | 0.669 [0.01–1.31] | 0.99 (0.43) | 0.77 (0.10) | 0.282 | −0.35 [−0.98–0.29] | 0.65 (0.14) | 1.07 (0.15) | 0.024 * | r = −0.37 |
| Anger | 1.08 (0.16) | 1.06 (0.10) | 0.940 | 0.024 [−0.61–0.66] | 1.22 (0.13) | 1.00 (0.13) | 0.253 | 0.375 [−0.26–1.01] | 1.27 (0.37) | 0.98 (0.08) | 0.117 | −0.510 [−1.1–0.13] | 0.95 (0.12) | 1.25 (0.13) | 0.097 | −0.562 [−1.28–0.07] |
| Disruptive behavior | 0.494 (0.11) | 0.704 (0.07) | 0.011 * | r = −0.40 | 0.74 (0.09) | 0.48 (0.09) | 0.031 * | r = −0.35 | 0.63 (0.10) | 0.62 (0.09) | 0.947 | −0.021 [−0.65–0.61] | 0.57 (0.09) | 0.70 (0.10) | 0.326 | −0.329 [−0.98–0.32] |
| Empathy | 2.91 (0.16) | 2.45 (0.12) | 0.028 * | 0.712 [0.08–1.34] | 2.61 (0.14) | 2.60 (0.15) | 0.965 | 0.014 [−0.60–0.62] | 2.59 (0.65) | 2.62 (0.14) | 0.908 | 0.036 [−0.57–0.64] | 2.89 (0.14) | 2.35 (0.13) | 0.008 * | 0.886 [0.23–1.53] |
| Self-efficacy | 2.57 (0.16) | 2.48 (0.12) | 0.658 | 0.139 [−0.47–0.75] | 2.40 (0.14) | 2.56 (0.14) | 0.459 | −0.233 [−0.84–0.38] | 2.51 (0.13) | 2.43 (0.15) | 0.686 | −0.126 [−0.73–0.48] | 2.81 (0.16) | 2.18 (0.09) | 0.002 * | 1.13 [0.46–1.80] |
| Self-worth | 2.78 (0.16) | 2.61 (0.14) | 0.474 | 0.225 [−0.39–0.84] | 2.37 (0.14) | 2.97 (0.12) | 0.007 * | −0.881 [−1.52–−0.23] | 2.62 (0.15) | 2.64 (0.17) | 0.934 | 0.026 [−0.58 −0.63] | 2.84 (0.17) | 2.50 (0.15) | 0.142 | 0.474 [−0.16–1.10] |
| Sense of coherence | 2.76 (0.16) | 2.64 (0.12) | 0.537 | 0.194 [−0.42–0.81] | 2.54 (0.12) | 2.83 (0.13) | 0.145 | −0.463 [−1.08–0.16] | 2.67 (0.13) | 2.66 (0.15) | 0.937 | −0.025 [−0.63–0.58] | 2.91 (0.15) | 2.47 (0.13) | 0.028 * | 0.724 [0.08–1.36] |
| Optimism | 2.68 (0.14) | 2.41 (0.10) | 0.123 | 0.491 [−0.13–1.1] | 2.42 (0.12) | 2.53 (0.13) | 0.576 | −0.176 [−0.79–0.44] | 2.53 (0.13) | 2.40 (0.12) | 0.491 | −0.215 [0.82–0.39] | 2.68 (0.15) | 2.33 (0.10) | 0.052 | 0.635 [−0.01–1.27] |
| Self-control | 2.82 (0.14) | 2.60 (0.12) | 0.254 | 0.361 [−0.26–0.97] | 2.56 (0.13) | 2.84 (0.13) | 0.154 | −0.453 [−1.07–0.17] | 2.71 (0.12) | 2.66 (0.16) | 0.809 | −0.075 [−0.68–0.53] | 2.73 (0.17) | 2.63 (0.11) | 0.641 | 0.149 [−0.47–0.77] |
| Supportive Feedback | Feedback Suggesting Improvement |
|---|---|
| Interaction with Avatar “chatting/interacting with Fauli” | Text length “too much texts/questions” |
| Aesthetics “graphics, design, islands, different worlds” | Presentation time “talked too fast” |
| App-features “rewards, diary, SOS-button” | Technical errors “pixelated animals”, “didn´t work” |
| Game character “different levels, content of challenges” | Content/Challenges “too easy, number of challenges” |
| Other | Presentation style |
| “nothing, app was not used” | “weird/not many answers” |
| Therapy Type/Aim | General Findings | Quotes |
|---|---|---|
| Drama therapy/ Perception and regulation of emotions | Positive perception of expressing feelings nonverbally | “I discovered my body all new today—like a newborn! I am proud and happy” (10-year-old girl) “I can represent something with my body, too!” (11-year-old-boy) “I am happy right now but sad that the program is over.” (13-year-old non-binary participant) “I take with me today that role-playing is fun!” (9-year-old girl) |
| Nature therapy/ Enhancing self-esteem | By creating analogies to the animal world, participants were able to name their strengths in a simplified way: | “The bee is very diligent because it makes honey for people. And I’m very diligent because I did a lot of homework today.” (8-year-old girl) “A male and female unicorn met and fell in love with each other. So my strength is love.” (11-year-old boy) “That was pretty great, I don’t want it to end. And I really want to do this tree exercise again!” (9-year-old girl) “I like everything that has to do with nature.” (12-year-old boy) |
| Art therapy/ Activating resources | Participants especially seemed to enjoy the free and unassessed process of creating a painting and creating a strength animal or object to provide them with support: | “I am completely free!” (12-year-old girl) “This circle was particularly beautiful to me. I don’t know why, but when I look at it, I think of the future.” (13-year-old boy) “My magical creature, the unicorn, wants everyone to have happiness except the bad people.” (9-year-old girl) “I painted a very special panda.” (8-year-old girl) “These are lotus flowers with wings. They have a colorful power. If you put something in there, it becomes very small or very big.” (13-year-old girl) |
| Yoga therapy/Setting boundaries | Changing opinion during the session: At first, the participants were skeptical but then embraced the yoga session | “I want to remember everything I learned in yoga today and incorporate it into my life.” (11-year-old boy) “I’ve never seen the kids so happy. You really could hook them.” (Pedagogical specialist to yoga therapist) |
| Intervention Part | General Findings | Quotes |
|---|---|---|
| Face-to-face activities | Movement (yoga) Freedom to create (art) Being outside (nature) Sympathy of the therapists | “The physical activity and releasing the energy in yoga was my highlight.” (11-year-old boy) “I liked that we were allowed to just paint away in art and didn’t have an objective.” (11-year-old boy) “I especially liked the fact that we were outdoors as well.” (10-year-old boy) “That the nature therapist was here.” (11-year-old girl) “The yoga teacher was very sympathetic to me.” (11-year-old boy) |
| Mondori app | Digital companionship of the avatar “Fauli” | “That Fauli was always with me.” (12-year-old boy) |
| Blended intervention | Voluntary character Multidimensional examination of topics | “That we could freely choose whether we wanted to attend.” (10-year-old girl) “The different approaches to the topic of emotions.” (Primary educator of a participating facility) “Creative and diversified change from everyday life.” (Pedagogical specialist of a facility) “Tasks were processed differently.” (Pedagogical director of a facility) |
| Measure | Pre | Post | p-Value | 95% CI for MD | η | ||
|---|---|---|---|---|---|---|---|
| n | Mean (SE) | n | Mean (SE) | ||||
| Mental health | |||||||
| Anxiety | 42 | 0.99 (0.69) | 34 | 0.97 (0.61) | 0.776 | [−0.24–0.19] | 0.62 |
| Depression | 42 | 0.87 (0.64) | 35 | 0.89 (0.63) | 0.978 | [−0.20–0.21] | 0.64 |
| Anger | 42 | 1.10 (0.57) | 34 | 0.93 (0.48) | 0.071 | [0.00–0.039] | 0.56 |
| Disruptive behavior | 42 | 0.63 (0.42) | 34 | 0.55 (0.32) | 0.207 | [−0.05–0.27] | 0.46 |
| Self-worth | 42 | 1.71 (0.57) | 35 | 1.49 (0.55) | 0.060 | [0.00−0.39] | 0.54 |
| Resources | |||||||
| Empathy | 45 | 2.60 (0.68) | 35 | 2.54 (0.55) | 0.191 | [−0.04–0.30] | 0.57 |
| Self-efficacy | 45 | 2.48 (0.64) | 35 | 2.47 (0.48) | 0.768 | [−0.24–0.17] | 0.66 |
| Self-esteem | 45 | 2.64 (0.72) | 35 | 2.47 (0.74) | 0.124 | [−0.04–0.40] | 0.70 |
| Sense of coherence | 45 | 2.66 (0.63) | 35 | 2.50 (0.67) | 0.077 | [−0.03–0.45] | 0.73 |
| Optimism | 45 | 2.48 (0.57) | 35 | 2.51 (0.49) | 0.931 | [−0.21–0.19] | 0.61 |
| Self-control | 45 | 2.66 (0.61) | 35 | 2.39 (0.60) | 0.061 | [0.00–0.47] | 0.71 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Birnkammer, S.; Calvano, C. A Creative and Movement-Based Blended Intervention for Children in Outpatient Residential Care: A Mixed-Method, Multi-Center, Single-Arm Feasibility Trial. Children 2023, 10, 207. https://doi.org/10.3390/children10020207
Birnkammer S, Calvano C. A Creative and Movement-Based Blended Intervention for Children in Outpatient Residential Care: A Mixed-Method, Multi-Center, Single-Arm Feasibility Trial. Children. 2023; 10(2):207. https://doi.org/10.3390/children10020207
Chicago/Turabian StyleBirnkammer, Susanne, and Claudia Calvano. 2023. "A Creative and Movement-Based Blended Intervention for Children in Outpatient Residential Care: A Mixed-Method, Multi-Center, Single-Arm Feasibility Trial" Children 10, no. 2: 207. https://doi.org/10.3390/children10020207
APA StyleBirnkammer, S., & Calvano, C. (2023). A Creative and Movement-Based Blended Intervention for Children in Outpatient Residential Care: A Mixed-Method, Multi-Center, Single-Arm Feasibility Trial. Children, 10(2), 207. https://doi.org/10.3390/children10020207






