External Esophageal Stenting Technique in Palliation for Tracheal Agenesis in a Case of Esophageal Lung: A Lesson Learned from the Experience for Tracheomalacia
Abstract
:1. Introduction
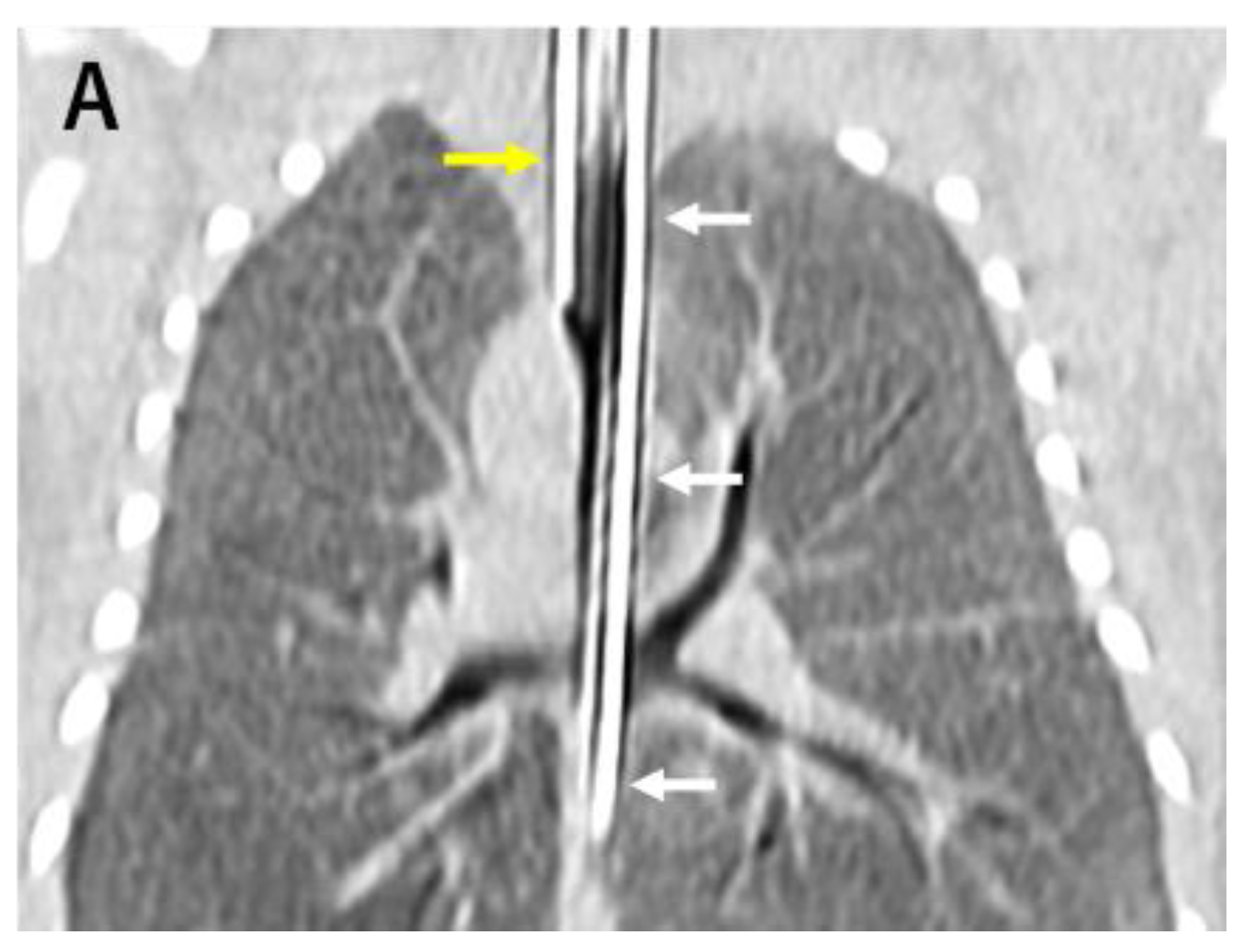
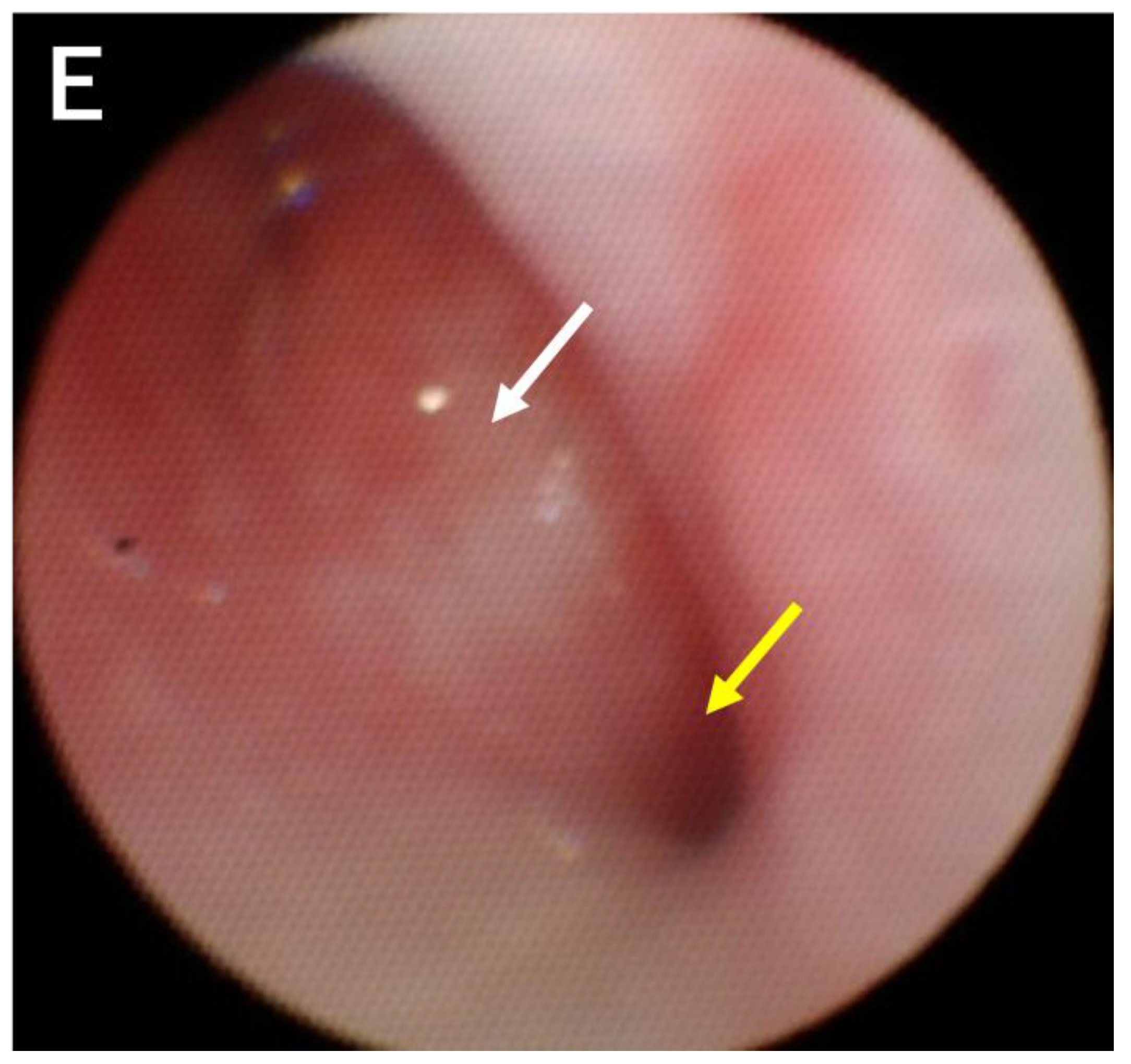
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Payne, W. Congenital absence of the trachea. Brooklyn Med. J. 1900, 14, 568–570. [Google Scholar]
- de Groot-van der Mooren, M.; Haak, M.C.; Lakeman, P.; Cohen-Overbeek, T.E.; van der Voorn, J.P.; Bretschneider, J.H. Tracheal agenesis: Approach towards this severe diagnosis. Case report and review of the literature. Eur. J. Pediatr. 2012, 171, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Floyd, J.; Campbell, D.C.; Dominy, D. Agenesis of the trachea. Am. Rev. Respir. Dis. 1962, 86, 557–560. [Google Scholar] [PubMed]
- Watanabe, T.; Okuyama, H.; Kubota, A.; Kawahara, H.; Hasegawa, T.; Ueno, T. A case of tracheal agenesis surviving without mechanical ventilation after external esophageal stenting. J. Pediatr. Surg. 2008, 43, 1906–1908. [Google Scholar] [CrossRef]
- Usui, N.; Kamiyama, M.; Tani, G.; Takama, Y.; Soh, H.; Uehara, S. Three-stage reconstruction of the airway and alimentary tract in a case of tracheal agenesis. Ann. Thorac. Surg. 2010, 89, 2019–2022. [Google Scholar] [CrossRef] [PubMed]
- Park, B.J.; Kim, M.S.; Yang, J.H.; Jun, T.G. Tracheal agenesis reconstruction with external esophageal stenting: Postoperative results and complications. Korean J. Thorac. Cardiovasc. Surg. 2015, 48, 439–442. [Google Scholar] [CrossRef]
- Densmore, J.C.; Oldham, K.T.; Dominguez, K.M.; Berdan, E.R.; McCormick, M.E.; Beste, D.J. Neonatal esophageal trachealization and esophagocarinoplasty in the treatment of flow-limited Floyd II tracheal agenesis. J. Thorac. Cardiovasc. Surg. 2017, 153, e121–e125. [Google Scholar] [CrossRef]
- Nakamoto, Y.; Ando, M.; Hasegawa, H. External Stenting for Tracheobronchomalacia Associated with Congenital Heart Disease. Circulation 2014, 130, A12872. [Google Scholar] [CrossRef]
- Ando, M.; Nagase, Y.; Hasegawa, H.; Takahashi, Y. External stenting: A reliable technique to relieve airway obstruction in small children. J. Thorac. Cardiovasc. Surg. 2017, 153, 1167–1177. [Google Scholar] [CrossRef]
- Sugandhi, N.; Sharma, P.; Agarwala, S.; Kabra, S.K.; Gupta, A.K.; Gupta, D.K. Esophageal lung: Presentation, management, and review of literature. J. Pediatr. Surg. 2011, 46, 1634–1637. [Google Scholar] [CrossRef]
- Straughan, A.J.; Mulcahy, C.F.; Sandler, A.D.; Bauman, N.M.; Steinhorn, D.; Gitman, L. Tracheal Agenesis: Vertical Division of the Native Esophagus—A Novel Surgical Approach and Review of the Literature. Ann. Otol. Rhinol. Laryngol. 2021, 130, 547–562. [Google Scholar] [CrossRef]
- Hiyama, E.; Yokoyama, T.; Ichikawa, T.; Matsuura, Y. Surgical management of tracheal agenesis. J. Thorac. Cardiovasc. Surg. 1994, 108, 830–833. [Google Scholar] [CrossRef]
- Soh, H.; Kawahawa, H.; Imura, K.; Yagi, M.; Yoneda, A.; Kubota, A. Tracheal agenesis in a child who survived for 6 years. J. Pediatr. Surg. 1999, 34, 1541–1543. [Google Scholar] [CrossRef]
- Fuchimoto, Y.; Mori, M.; Takasato, F.; Tomita, H.; Yamamoto, Y.; Shimojima, N. A long-term survival case of tracheal agenesis: Management for tracheoesophageal fistula and esophageal reconstruction. Pediatr. Surg. Int. 2011, 27, 103–106. [Google Scholar] [CrossRef] [PubMed]
- Tazuke, Y.; Okuyama, H.; Uehara, S.; Ueno, T.; Nara, K.; Yamanaka, H. Long-term outcomes of four patients with tracheal agenesis who underwent airway and esophageal reconstruction. J. Pediatr. Surg. 2015, 50, 2009–2011. [Google Scholar] [CrossRef]
- Varela, P.; Torre, M.; Schweiger, C.; Nakamura, H. Congenital tracheal malformations. Pediatr. Surg. Int. 2018, 34, 701–713. [Google Scholar] [CrossRef]
- Hagl, S.; Jakob, H.; Sebening, C.; van Bodegom, P.; Schmidt, K.; Zilow, E. External stabilization of long-segment tracheobronchomalacia guided by intraoperative bronchoscopy. Ann. Thorac. Surg. 1997, 64, 1412–1421. [Google Scholar] [CrossRef] [PubMed]
- Fabre, D.; Kolb, F.; Fadel, E.; Mercier, O.; Mussot, S.; Chevalier, T.L.; Dartevelle, P. Successful tracheal replacement in humans using autologous tissues: An 8-year experience. Ann. Thorac. Surg. 2013, 96, 1146–1155. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Liu, Z. Airway reconstruction with autologous pulmonary tissue flap and an elastic metallic stent. World J. Surg. 2015, 39, 1981–1985. [Google Scholar] [CrossRef]
- Delaere, P.R.; Vranckx, J.J.; Verleden, G.; Leyn, P.D.; Raemdonck, D.V. Tracheal allotransplantation after withdrawal of immunosuppressive therapy. N. Engl. J. Med. 2014, 370, 1568–1570. [Google Scholar] [CrossRef]
- Elliott, M.J.; Butler, C.R.; Varanou-Jenkins, A.; Partington, L.; Carvalho, C.; Samuel, E.; Crowley, C.; Lange, P.; Hamilton, N.J.; Hynds, R.E.; et al. Tracheal replacement therapy with a stem cell-seeded graft: Lessons from compassionate use application of a GMP-compliant tissue-engineered medicine. Stem Cells Transl. Med. 2017, 6, 1458–1464. [Google Scholar] [CrossRef] [PubMed]



| Case | Publication | Floyd’s Type | Age of External Stenting (Months) | Surgical Approach | PTFE Graft Size and Form | Reported Age of Survival (Months) |
|---|---|---|---|---|---|---|
| 1 | 2008 [4] | I | 2 | Median sternotomy | 16 mm, full circle | 109 |
| 2 | 2010 [5] | I | 8 | Right thoracotomy | 20 mm, semicircle | 98 |
| 3 | 2015 [6] | II | 3 | Median sternotomy | 8 mm, 3/4 circle | 11 |
| 4 | 2017 [7] | II | 3 | Median sternotomy | 20 mm, full circle | 36 |
| 5 | 2023 * | III | 7 | Median sternotomy | 16 mm, semicircle | 12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirotani, T.; Tamura, R.; Ando, M.; Okajima, H. External Esophageal Stenting Technique in Palliation for Tracheal Agenesis in a Case of Esophageal Lung: A Lesson Learned from the Experience for Tracheomalacia. Children 2023, 10, 1907. https://doi.org/10.3390/children10121907
Hirotani T, Tamura R, Ando M, Okajima H. External Esophageal Stenting Technique in Palliation for Tracheal Agenesis in a Case of Esophageal Lung: A Lesson Learned from the Experience for Tracheomalacia. Children. 2023; 10(12):1907. https://doi.org/10.3390/children10121907
Chicago/Turabian StyleHirotani, Taichi, Ryo Tamura, Makoto Ando, and Hideaki Okajima. 2023. "External Esophageal Stenting Technique in Palliation for Tracheal Agenesis in a Case of Esophageal Lung: A Lesson Learned from the Experience for Tracheomalacia" Children 10, no. 12: 1907. https://doi.org/10.3390/children10121907
APA StyleHirotani, T., Tamura, R., Ando, M., & Okajima, H. (2023). External Esophageal Stenting Technique in Palliation for Tracheal Agenesis in a Case of Esophageal Lung: A Lesson Learned from the Experience for Tracheomalacia. Children, 10(12), 1907. https://doi.org/10.3390/children10121907







