Parents’ Perceptions Regarding Their Children’s Medications and Expert-Assessed Drug-Related Problems in Pediatric Patients with Inborn Errors of Metabolism
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Participants, and Setting
2.2. Telephone Interview
- Parental perceptions regarding their children’s IEM medication; only for parents of children taking IEM medication;
- The patient’s complete medication, prescribed by physicians or bought by themselves: IEM medication, medication for other chronic conditions, if applicable, and other as-needed medication (e.g., for colds);
- Sociodemographic data of parents and patients.
2.3. Expert-Assessed Drug-Related Problems
- Medication appropriate: The medication can be safely used in the patient, according to the literature;
- Medication problematic without clinical relevance: According to the literature, the medication should not be used in the patient. However, the identified problems were negligible in the affected patients in our study. Yet, it cannot be ruled out that problems might occur in other patients;
- Necessary medication with clinically relevant problems because no safe alternatives are available: According to the literature, the medication should not be used in the patient due to potential clinically relevant problems. However, the medication is necessary for the patient, and there is no safe alternative;
- Non-necessary medication with clinically relevant problems because safe alternatives are available: According to the literature, the medication should not be used in the patient due to potential clinically relevant problems. Safe alternatives exist, or the medication is not necessary for the patient and can be omitted. Thus, those medications are avoidable;
- Not assessable due to lack of specifications: The manufacturer or the parents did not provide sufficient information on the medication, so it could not be included in the analysis.
2.4. Analysis and Statistics
3. Results
3.1. Characteristics of Patients and Their Parents
3.2. Parental Perceptions Regarding Their Children’s IEM Medication
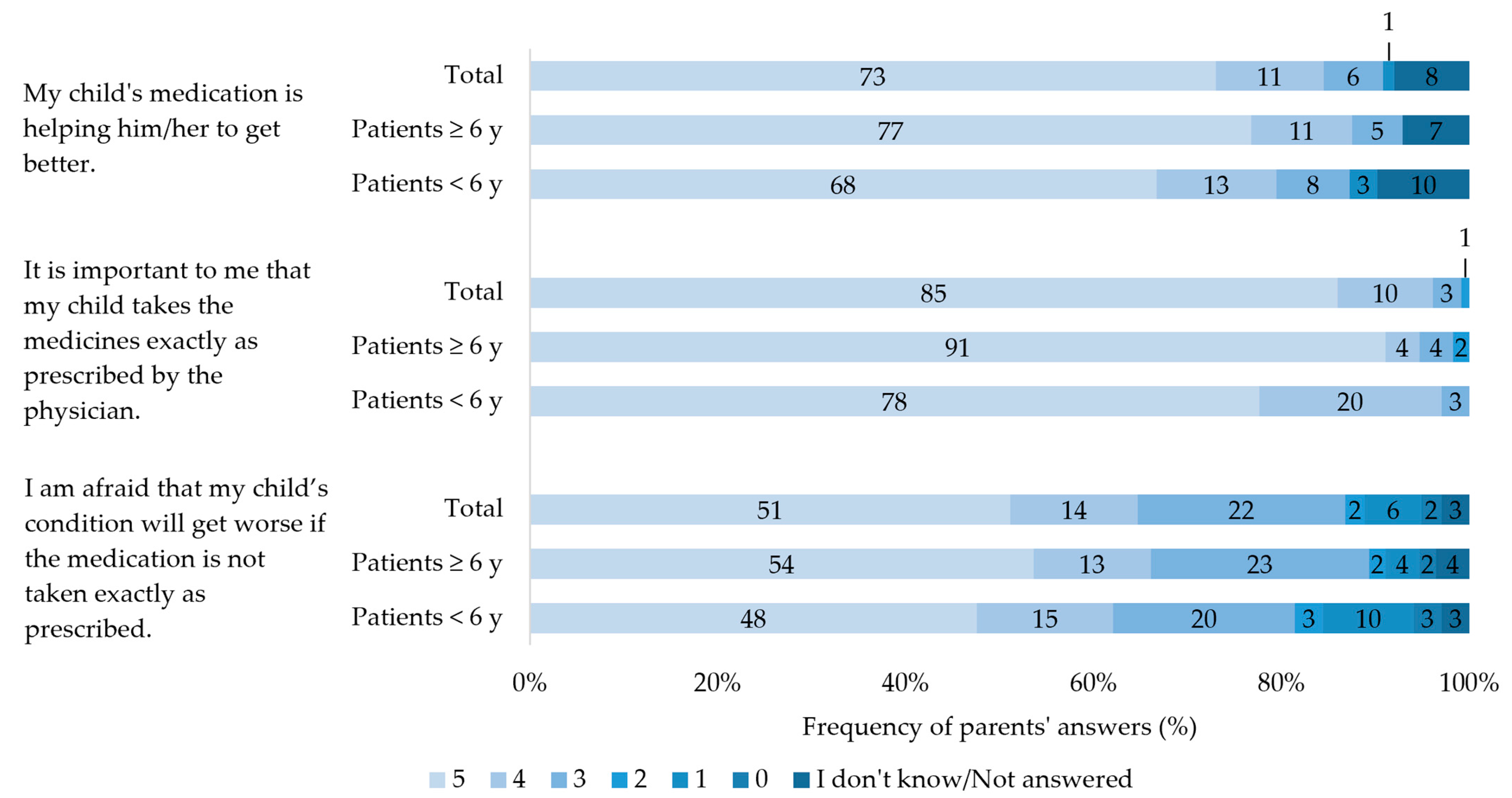
3.2.1. Importance of IEM Medication Intake
3.2.2. Perceived Complications with IEM Medication
3.2.3. ADR of IEM Medication as Perceived by the Parents
3.3. Expert-Assessed Drug-Related Problems
4. Discussion
4.1. Parental Perceptions Regarding Their Children’s IEM Medication
4.1.1. Importance of IEM Medication Intake
4.1.2. Perceived Complications with the IEM Medication
4.1.3. ADR of IEM Medication as Perceived by the Parents
4.2. Expert-Assessed Drug-Related Problems
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zschocke, J.; Hoffmann, G.F. Vademecum Metabolicum. Diagnosis and Treatment of Inherited Metabolic Disorders, 5th ed.; Thieme: Stuttgart, Germany, 2020; pp. 1–29. [Google Scholar]
- Virtual Metabolic Human Database. Available online: https://www.vmh.life/#diseases (accessed on 16 November 2023).
- Sahoo, S.; Franzson, L.; Jonsson, J.J.; Thiele, I. A compendium of inborn errors of metabolism mapped onto the human metabolic network. Mol. Biosyst. 2012, 10, 2545–2558. [Google Scholar] [CrossRef] [PubMed]
- Inborn Errors of Metabolism Knowledgebase. Available online: http://iembase.org/index.asp (accessed on 16 November 2023).
- Ferreira, C.R.; Rahman, S.; Keller, M.; Zschocke, J.; ICIMD Advisory Group. An international classification of inherited metabolic disorders (ICIMD). J. Inherit. Metab. Dis. 2021, 44, 164–177. [Google Scholar] [CrossRef] [PubMed]
- Gesellschaft für Neonatologie und pädiatrische Intensivmedizin e.V. Neugeborenen-Screening auf Angeborene Stoffwechselstörungen, Endokrinopathien, Schwere Kombinierte Immundefekte (SCID), Sichelzellkrankheit, 5q-Assoziierte Spinale Muskelatrophie (SMA) und Mukoviszidose. 2022. Available online: https://www.awmf.org/uploads/tx_szleitlinien/024-012l_S2k_Neugeborenenscreening_2022-02_01.pdf (accessed on 30 August 2023).
- Gramer, G.; Hauck, F.; Lobitz, S.; Sommerburg, O.; Speckmann, C.; Hoffmann, G.F. Neugeborenenscreening 2020. Monatsschrift Kinderheilkd. 2017, 165, 216–225. [Google Scholar] [CrossRef]
- Siddiq, S.; Wilson, B.J.; Graham, I.D.; Lamoureux, M.; Khangura, S.D.; Tingley, K.; Tessier, L.; Chakraborty, P.; Coyle, D.; Dyack, S.; et al. Experiences of caregivers of children with inherited metabolic diseases: A qualitative study. Orphanet J. Rare Dis. 2016, 11, 168. [Google Scholar] [CrossRef] [PubMed]
- German Society for Neonatal Screening, e.V. National Screening Report Germany 2017. Available online: https://www.screening-dgns.de/Pdf/Screeningreports/DGNS-Screeningreport-e_2017.pdf (accessed on 30 August 2023).
- Feldmann, R.; Osterloh, J.; Onon, S.; Fromm, J.; Rutsch, F.; Weglage, J. Neurocognitive functioning in adults with phenylketonuria: Report of a 10-year follow-up. Mol. Genet. Metab. 2019, 126, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Bickel, H.; Gerrard, J.; Hickmans, E.M. Influence of phenylalanine intake on phenylketonuria. Lancet 1953, 265, 812–813. [Google Scholar] [CrossRef]
- Karall, D.; Scholl-Bürgi, S. Seltene Krankheiten: Angeborene Stoffwechselstörungen im Kinder- und Jugendalter. Pädiatrie Pädologie 2017, 52, 194–198. [Google Scholar] [CrossRef][Green Version]
- Yue, W.W.; Mackinnon, S.; Bezerra, G.A. Substrate reduction therapy for inborn errors of metabolism. Emerg. Top. Life Sci. 2019, 3, 63–73. [Google Scholar] [CrossRef]
- Das, A.M.; Illsinger, S. Pharmacological Therapy in Inborn Errors of Metabolism. In Drug Discovery and Evaluation: Methods in Clinical Pharmacology; Hock, F.J., Gralinski, M.R., Eds.; Springer: Cham, Switzerland, 2019; pp. 1–16. [Google Scholar]
- Mütze, U.; Roth, A.; Weigel, J.F.W.; Beblo, S.; Baerwald, C.G.; Bührdel, P.; Kiess, W. Transition of young adults with phenylketonuria from pediatric to adult care. J. Inherit. Metab. Dis. 2011, 34, 701–709. [Google Scholar] [CrossRef]
- Ziesch, B.; Weigel, J.; Thiele, A.; Mütze, U.; Rohde, C.; Ceglarek, U.; Thiery, J.; Kiess, W.; Beblo, S. Tetrahydrobiopterin (BH4) in PKU: Effect on dietary treatment, metabolic control, and quality of life. J. Inherit. Metab. Dis. 2012, 35, 983–992. [Google Scholar] [CrossRef]
- Bosch, A.M.; Burlina, A.; Cunningham, A.; Bettiol, E.; Moreau-Stucker, F.; Koledova, E.; Benmedjahed, K.; Regnault, A. Assessment of the impact of phenylketonuria and its treatment on quality of life of patients and parents from seven European countries. Orphanet J. Rare Dis. 2015, 10, 80. [Google Scholar] [CrossRef] [PubMed]
- Anderson, V.A.; Anderson, P.; Northam, E.; Jacobs, R.; Mikiewicz, O. Relationships between cognitive and behavioral measures of executive function in children with brain disease. Child Neuropsychol. 2002, 8, 231–240. [Google Scholar] [CrossRef]
- Alptekin, I.M.; Koc, N.; Gunduz, M.; Cakiroglu, F.P. The impact of phenylketonuria on PKU patients’ quality of life: Using of the phenylketonuria-quality of life (PKU-QOL) questionnaires. Clin. Nutr. ESPEN 2018, 27, 79–85. [Google Scholar] [CrossRef]
- Channon, S.; Goodman, G.; Zlotowitz, S.; Mockler, C.; Lee, P.J. Effects of dietary management of phenylketonuria on long-term cognitive outcome. Arch. Dis. Child. 2007, 92, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Pascoal, C.; Brasil, S.; Francisco, R.; Marques-da-Silva, D.; Rafalko, A.; Jaeken, J.; Videira, P.A.; Barros, L.; dos Reis Ferreira, V. Patient and observer reported outcome measures to evaluate health-related quality of life in inherited metabolic diseases: A scoping review. Orphanet J. Rare Dis. 2018, 13, 215. [Google Scholar] [CrossRef] [PubMed]
- Bach, V.A.; Neininger, M.P.; Spindler, U.P.; Hotopp, L.C.; Hornemann, F.; Syrbe, S.; Merkenschlager, A.; Kiess, W.; Bernhard, M.K.; Bertsche, T.; et al. How do parents perceive adverse drug events of their children’s anticonvulsant medication? Eur. J. Paediatr. Neurol. 2018, 22, 427–433. [Google Scholar] [CrossRef]
- Agana, M.; Frueh, J.; Kamboj, M.; Patel, D.R.; Kanungo, S. Common metabolic disorder (inborn errors of metabolism) concerns in primary care practice. Ann. Transl. Med. 2018, 6, 469. [Google Scholar] [CrossRef]
- Pharmaceutical Care Network Europe Association. The PCNE Classification for Drug Related Problem V9.1. 2020. Available online: https://www.pcne.org/upload/files/417_PCNE_classification_V9-1_final.pdf (accessed on 30 August 2023).
- MacDonald, A. Diet and compliance in phenylketonuria. Eur. J. Pediatr. 2000, 159 (Suppl. S2), S136–S141. [Google Scholar] [CrossRef]
- Zimmermann, M.; Jacobs, P.; Fingerhut, R.; Torresani, T.; Thöny, B.; Blau, N.; Baumgartner, M.R.; Rohrbach, M. Positive effect of a simplified diet on blood phenylalanine control in different phenylketonuria variants, characterized by newborn BH4 loading test and PAH analysis. Mol. Genet. Metab. 2012, 106, 264–268. [Google Scholar] [CrossRef]
- Rohde, C.; Thiele, A.G.; Och, U.; Schönherr, K.; Meyer, U.; Rosenbaum-Fabian, S.; Maddalon, C.; Matzken, S.; Blessing, H.; Lang, F.; et al. Effect of dietary regime on metabolic control in phenylketonuria: Is exact calculation of phenylalanine intake really necessary? Mol. Genet. Metab. Rep. 2015, 5, 36–41. [Google Scholar] [CrossRef]
- Bombard, Y.; Baker, G.R.; Orlando, E.; Fancott, C.; Bhatia, P.; Casalino, S.; Onate, K.; Denis, J.L.; Pomey, M.P. Engaging patients to improve quality of care: A systematic review. Implement. Sci. 2018, 13, 98. [Google Scholar] [CrossRef]
- Zeltner, N.A.; Welsink-Karssies, M.M.; Landolt, M.A.; Bosshard-Bullinger, D.; Keller, F.; Bosch, A.M.; Groenendijk, M.; Grünert, S.C.; Karall, D.; Rettenbacher, B.; et al. Reducing complexity: Explaining inborn errors of metabolism and their treatment to children and adolescents. Orphanet J. Rare Dis. 2019, 14, 248. [Google Scholar] [CrossRef]
- Herziger, B.; Jeschke, S.; Müller, R.M.; Neininger, M.P.; Bertsche, T.; Bertsche, A. Drug-handling problems and expectations of the ideal pediatric drug-reported by children and their parents. Eur. J. Pediatr. 2022, 181, 2161–2171. [Google Scholar] [CrossRef]
- Connan, V.; Marcon, M.A.; Mahmud, F.H.; Assor, E.; Martincevic, I.; Bandsma, R.H.; Vresk, L.; Walsh, C.M. Online education for gluten-free diet teaching: Development and usability testing of an e-learning module for children with concurrent celiac disease and type 1 diabetes. Pediatr. Diabetes 2019, 20, 293–303. [Google Scholar] [CrossRef]
- Chawla, S.P.S.; Kaur, S.; Bharti, A.; Garg, R.; Kaur, M.; Soin, D.; Ghosh, A.; Pal, R. Impact of health education on knowledge, attitude, practices and glycemic control in type 2 diabetes mellitus. J. Family Med. Prim. Care 2019, 8, 261–268. [Google Scholar] [CrossRef]
- Harthan, A.A. An Introduction to Pharmacotherapy for Inborn Errors of Metabolism. J. Pediatr. Pharmacol. Ther. 2018, 23, 432–446. [Google Scholar] [CrossRef]
- Breitkreutz, J.; Boos, J. Paediatric and geriatric drug delivery. Expert. Opin. Drug Deliv. 2007, 4, 37–45. [Google Scholar] [CrossRef]
- Committee for Medicinal Products for Human Use (CHMP)/International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH). E 11 Clinical Investigation of Medicinal Products in the Paediatric Population. 2001. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/e-11-clinical-investigation-medicinal-products-paediatric-population-step-5_en.pdf (accessed on 30 August 2023).
- Mistry, P.; Batchelor, H. Evidence of acceptability of oral paediatric medicines: A review. J. Pharm. Pharmacol. 2017, 69, 361–376. [Google Scholar] [CrossRef]
- Zajicek, A.; Fossler, M.J.; Barrett, J.S.; Worthington, J.H.; Ternik, R.; Charkoftaki, G.; Lum, S.; Breitkreutz, J.; Baltezor, M.; Macheras, P.; et al. A report from the pediatric formulations task force: Perspectives on the state of child-friendly oral dosage forms. AAPS J. 2013, 15, 1072–1081. [Google Scholar] [CrossRef] [PubMed]
- Leitzen, S.; Kayser, C.; Weißmann, K.; Sachs, B. Arzneimittelnebenwirkungen und Medikationsfehler bei Kindern. Monatsschr. Kinderheilkd. 2022, 170, 217–227. [Google Scholar] [CrossRef]
- Neuspiel, D.R.; Taylor, M.M. Reducing the risk of harm from medication errors in children. Health Serv. Insights 2013, 6, 47–59. [Google Scholar] [CrossRef]
| Characteristics | Patients Aged < 6 Years | Patients Aged ≥ 6 Years | Total |
|---|---|---|---|
| Number of parents [N] | 44 * | 66 * | 108 * |
| Median age of parents (Q25/Q75; min/max) [years] | 35 (32/37; 24/45) | 41 (38/45.5; 30/54) | 38 (34/44; 24/54) |
| Sex of respondent [N (%)] | |||
| Male | 5 (11) | 11 (17) | 16 (15) |
| Female | 37 (84) | 55 (83) | 92 (85) |
| Number of children [N] | 47 | 72 | 119 |
| Median age of child (Q25/Q75; min/max) [years] | 3 (1/5; 0/5) | 12 (9/15; 6/17) | 8 (3.5/13); 0/17) |
| Sex of child [N (%)] | |||
| Male | 29 (62) | 43 (60) | 72 (61) |
| Female | 18 (38) | 29 (40) | 47 (39) |
| Diagnosis [N] | |||
| Phenylketonuria | 14 | 12 | 26 |
| Familial hypercholesterolemia | 0 | 18 | 18 |
| Medium-chain-acyl-CoA-dehydrogenase deficiency | 9 | 7 | 16 |
| Carnitine transporter deficiency | 0 | 6 | 6 |
| Unexplained hypoglycemia | 3 | 3 | 6 |
| Biotinidase deficiency | 2 | 3 | 5 |
| Hyperphenylalaninemia | 2 | 2 | 4 |
| Isovalerianacidemia | 3 | 1 | 4 |
| Glycogenosis type I | 1 | 2 | 3 |
| Long-chain-acyl-CoA-dehydrogenase deficiency | 1 | 2 | 3 |
| Smith–Lemli–Opitz syndrome | 2 | 1 | 3 |
| Congenital hyperinsulism | 0 | 2 | 2 |
| Methylenetetrahydrofolate-reductase deficiency | 0 | 2 | 2 |
| Very-long-chain-acyl-CoA-dehydrogenase deficiency | 0 | 2 | 2 |
| Vitamins B12 deficiency | 2 | 0 | 2 |
| 3-Methylcrotonyl-CoA-carboxylase deficiency | 0 | 1 | 1 |
| α-Mannosidose | 1 | 0 | 1 |
| Atypical phenylketonuria | 1 | 0 | 1 |
| Beckwith-Wiedemann syndrome | 0 | 1 | 1 |
| Galactosemia | 1 | 0 | 1 |
| Glutaraciduria type I | 0 | 1 | 1 |
| Glycogenosis type IX | 1 | 0 | 1 |
| Morbus Niemann–Pick type A | 1 | 0 | 1 |
| Non-ketotic hyperglycinemia | 1 | 0 | 1 |
| Ornithine-transcarbamylase deficiency | 0 | 1 | 1 |
| Pyruvate dehydrogenase deficiency | 1 | 0 | 1 |
| Tyrosinemia | 0 | 1 | 1 |
| X-Adrenoleukodystrophy | 0 | 1 | 1 |
| No diagnosis yet at the time of the interview. | 1 | 4 | 5 |
| Median number of medicinal products/nutritional supplements for the IEM (Q25/Q75; min/max) [N] | 1 (1/2; 0/10) | 1 (1/2; 0/7) | 1 (1/2; 0/10) |
| Median number of medicinal products/nutritional supplements for other chronic conditions or as-needed medication (Q25/Q75; min/max) [N] | 6 (4/8; 1/19) | 5 (3/7; 1/14) | 6 (3.5/8; 1/19) |
| Patients | Patients Aged < 6 Years (N = 40) | Patients Aged ≥ 6 Years (N = 56) | ||||
|---|---|---|---|---|---|---|
| Problems with Medication Intake | Problems [N] | Affected Patients [%] | Affected Patients [% (/13 Who Had Problems with Medication Intake)] | Problems [N] | Affected Patients [%] | Affected Patients [% (/26 Who Had Problems with Medication Intake)] |
| It is difficult to integrate intake into everyday life. | 3 | 8 | 27 | 1 | 2 | 4 |
| The intake is forgotten every now and then. | 0 | 0 | 0 | 20 | 36 | 77 |
| My child does not want to take the medication. | 9 | 23 | 81 | 11 | 20 | 42 |
| My child cannot take the medication without problems. | 2 | 5 | 18 | 1 | 2 | 4 |
| Total | 14 | 33 | 100 | 33 | 46 | 100 |
| Patients | Patients Aged < 6 Years (N = 40) | Patients Aged ≥ 6 Years (N = 56) | ||
|---|---|---|---|---|
| ADR | Feared ADR [N] (%) | Experienced ADR [N] (%) | Feared ADR [N] (%) | Experienced ADR [N] (%) |
| Non-specific ADR | 7 (18) | 0 (0) | 8 (14) | 0 (0) |
| Gastroenterological ADR | 5 (13) | 7 (18) | 3 (5) | 7 (13) |
| Neurological/psychiatric ADR | 3 (8) | 3 (8) | 5 (9) | 1 (2) |
| Long-term side effects (with unlicensed medicinal products) | 3 (8) | 0 (0) | 3 (5) | 0 (0) |
| Organ damage | 3 (8) | 1 (3) | 4 (7) | 0 (0) |
| Cancer | 1 (3) | 0 (0) | 1 (2) | 0 (0) |
| Weight gain | 1 (3) | 0 (0) | 1 (2) | 2 (4) |
| Developmental disorders | 1 (3) | 0 (0) | 1 (2) | 0 (0) |
| Dental problems | 1 (3) | 1 (3) | 0 (0) | 0 (0) |
| Diabetes | 0 (0) | 0 (0) | 1 (2) | 0 (0) |
| Effects on skin, hair, nails | 0 (0) | 0 (0) | 0 (0) | 3 (5) |
| Fish odor | 1 (3) | 1 (3) | 0 (0) | 3 (5) |
| Feeling of satiety | 0 (0) | 1 (3) | 0 (0) | 0 (0) |
| Increased urge to urinate | 0 (0) | 0 (0) | 0 (0) | 1 (2) |
| Expert Assessment | Number of Affected Preparations [N] (%) | Number of Affected Patients Aged < 6 Years [N] (%) | Number of Affected Patients Aged ≥ 6 Years [N] (%) |
|---|---|---|---|
| Medication appropriate | 711 (80) | 28 (62) | 36 (52) |
| Medication problematic without clinical relevance | 37 (4) | 2 (4) | 24 (35) |
| The oral dosage form was too large for the patient’s age, according to the literature; the affected patients were able to swallow the dosage form a | 18 (2) | 1 (2) | 8 (12) |
| Age (patient too old) a | 16 (2) | 2 (4) | 13 (19) |
| Inappropriate excipient according to literature in phenylketonuria, unproblematic due to phenylalanine tolerance at occasional use b | 3 (0.3) | 0 (0.0) | 3 (4) |
| Necessary medication with clinically relevant problems because no safe alternatives are available | 26 (3) | 8 (18) | 7 (10) |
| Age (patient too young) a | 4 (0.4) | 1 (2) | 0 (0.0) |
| Off-label (used for IEM *) b | 12 (1) | 5 (11) | 5 (7) |
| Off-label (used for other chronic indications) a | 8 (0.9) | 3 (7) | 2 (3) |
| Non-necessary medication with clinically relevant problems because safe alternatives are available | 20 (2) | 12 (27) | 12 (17) |
| Age (patient too young) a | 10 (1) | 8 (18) | 6 (9) |
| Inappropriate excipient for patient’s age a | 4 (0.4) | 4 (9) | 1 (1) |
| Use for the wrong indication a | 3 (0.3) | 1 (2) | 3 (4) |
| Use despite contraindications due to comorbidities a | 2 (0.2) | 0 (0.0) | 2 (3) |
| Medication is not probe-compatible in patients with a probe b | 1 (0.1) | 1 (2) | 0 (0.0) |
| Not assessable due to lack of specifications | 90 (10) | 27 (60) | 28 (41) |
| Medication for IEM * | 44 (5) | 16 (36) | 17 (25) |
| Medication for other conditions | 46 (5) | 14 (20) | 16 (23) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harings, T.; Neininger, M.P.; Eisenhofer, S.; Thiele, A.G.; Kiess, W.; Bertsche, A.; Beblo, S.; Bertsche, T. Parents’ Perceptions Regarding Their Children’s Medications and Expert-Assessed Drug-Related Problems in Pediatric Patients with Inborn Errors of Metabolism. Children 2023, 10, 1873. https://doi.org/10.3390/children10121873
Harings T, Neininger MP, Eisenhofer S, Thiele AG, Kiess W, Bertsche A, Beblo S, Bertsche T. Parents’ Perceptions Regarding Their Children’s Medications and Expert-Assessed Drug-Related Problems in Pediatric Patients with Inborn Errors of Metabolism. Children. 2023; 10(12):1873. https://doi.org/10.3390/children10121873
Chicago/Turabian StyleHarings, Tanjana, Martina Patrizia Neininger, Simone Eisenhofer, Alena Gerlinde Thiele, Wieland Kiess, Astrid Bertsche, Skadi Beblo, and Thilo Bertsche. 2023. "Parents’ Perceptions Regarding Their Children’s Medications and Expert-Assessed Drug-Related Problems in Pediatric Patients with Inborn Errors of Metabolism" Children 10, no. 12: 1873. https://doi.org/10.3390/children10121873
APA StyleHarings, T., Neininger, M. P., Eisenhofer, S., Thiele, A. G., Kiess, W., Bertsche, A., Beblo, S., & Bertsche, T. (2023). Parents’ Perceptions Regarding Their Children’s Medications and Expert-Assessed Drug-Related Problems in Pediatric Patients with Inborn Errors of Metabolism. Children, 10(12), 1873. https://doi.org/10.3390/children10121873








