Anterior Uveitis and Coats Disease in a 16-Year-Old Girl with Noonan Syndrome—A Case Report
Abstract
:1. Introduction
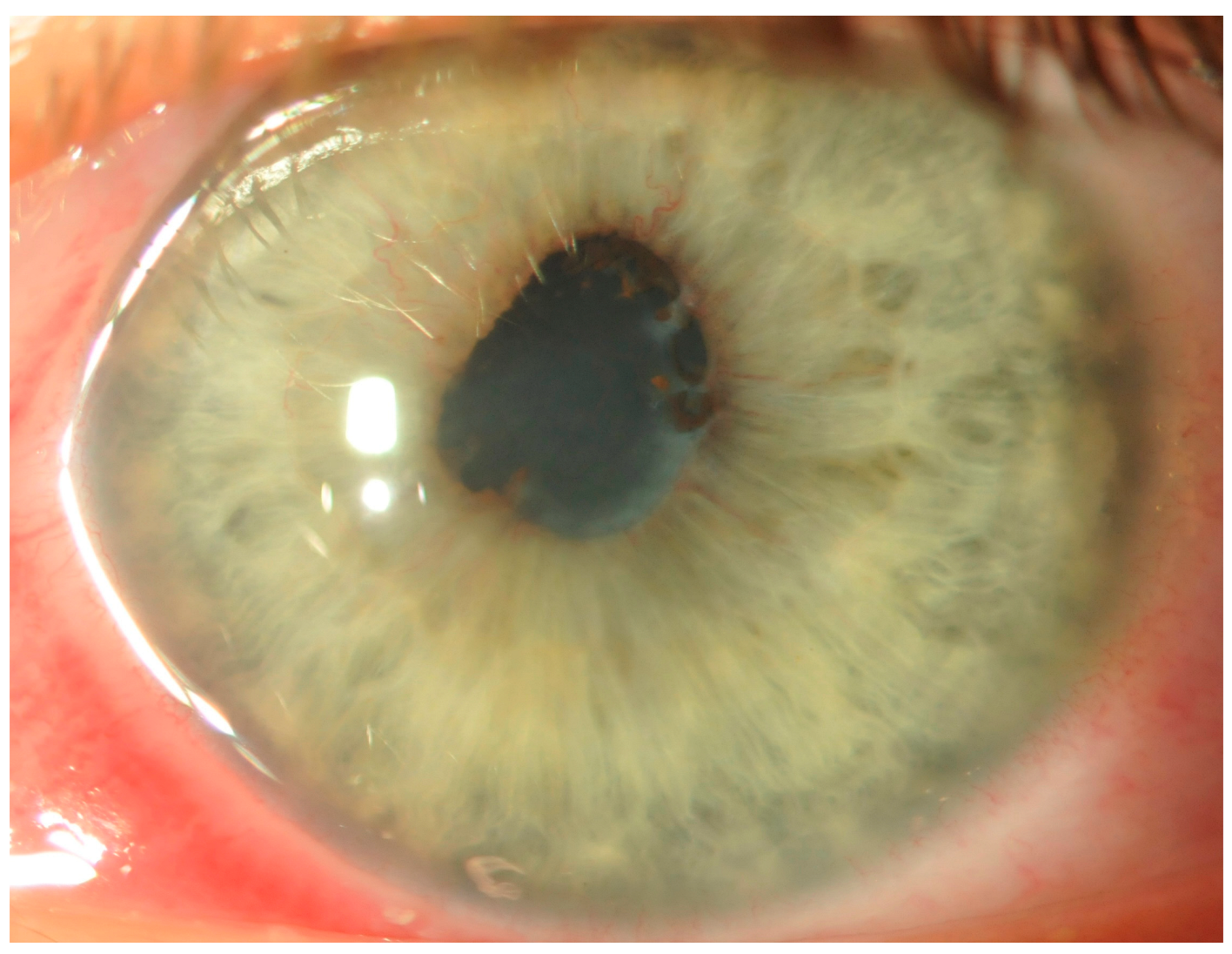
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roberts, A.E.; Allanson, J.E.; Tartaglia, M.; Gelb, B.D. Noonan syndrome. Lancet 2013, 381, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Carcavilla, A.; Suárez-Ortega, L.; Rodríguez Sánchez, A.; Gonzalez-Casado, I.; Ramón-Krauel, M.; Labarta, J.I.; Quinteiro Gonzalez, S.; Riaño Galán, I.; Ezquieta Zubicaray, B.; López-Siguero, J.P. Noonan syndrome: Genetic and clinical update and treatment options. An. Pediatr. (Engl. Ed.) 2020, 93, 61.e1–61.e14. [Google Scholar] [CrossRef]
- Zenker, M.; Edouard, T.; Blair, J.C.; Cappa, M. Noonan syndrome: Improving recognition and diagnosis. Arch. Dis. Child. 2022, 12, 1073–1078. [Google Scholar] [CrossRef] [PubMed]
- Mendez, H.M.; Opitz, J.M. Noonan syndrome: A review. Am. J. Med. Genet. 1985, 3, 493–506. [Google Scholar] [CrossRef] [PubMed]
- van Der Burgt, I.; Brunner, H. Genetic heterogeneity in Noonan syndrome: Evidence for an autosomal recessive form. Am. J. Med. Genet. 2000, 94, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Rauen, K.A. The RASopathies. Annu. Rev. Genomics Hum. Genet. 2013, 14, 355–369. [Google Scholar] [CrossRef]
- Christou, E.E.; Zafeiropoulos, P.; Rallis, D.; Baltogianni, M.; Asproudis, C.; Stefaniotou, M.; Giapros, V.; Asproudis, I. A Narrative Review of the Ocular Manifestations in Noonan Syndrome. Semin. Ophthalmol. 2022, 37, 215–221. [Google Scholar] [CrossRef]
- Lee, N.B.; Kelly, L.; Sharland, M. Ocular manifestations of Noonan syndrome. Eye 1992, 3, 328–334. [Google Scholar] [CrossRef]
- da Rocha Marin, L.; da Silva, F.T.; de Sá, L.C.; Brasil, A.S.; Pereira, A.; Furquim, I.M.; Kim, C.A.; Bertola, D.R. Ocular manifestations of Noonan syndrome. Ophthalmic Genet. 2012, 1, 1–5. [Google Scholar] [CrossRef]
- van Trier, D.C.; van der Burgt, I.; Draaijer, R.W.; Cruysberg, J.R.M.; Noordam, C.; Draaisma, J.M. Ocular findings in Noonan syndrome: A retrospective cohort study of 105 patients. Eur. J. Pediatr. 2018, 177, 1293–1298. [Google Scholar] [CrossRef]
- Quaio, C.R.; Carvalho, J.F.; da Silva, C.A.; Bueno, C.; Brasil, A.S.; Pereira, A.C.; Jorge, A.A.; Malaquias, A.C.; Kim, C.A.; Bertola, D.R. Autoimmune disease and multiple autoantibodies in 42 patients with RASopathies. Am. J. Med. Genet. A 2012, 158, 1077–1082. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, J.B.; Bidère, N.; Niemela, J.E.; Zheng, L.; Sakai, K.; Nix, C.P.; Danner, R.L.; Barb, J.; Munson, P.J.; Puck, J.M.; et al. NRAS mutation causes a human autoimmune lymphoproliferative syndrome. Proc. Natl. Acad. Sci. USA 2007, 104, 8953–8958. [Google Scholar] [CrossRef] [PubMed]
- Amoroso, A.; Garzia, P.; Vadacca, M.; Galluzzo, S.; Del Porto, F.; Mitterhofer, A.P.; Afeltra, A. The unusual association of three autoimmune diseases in a patient with Noonan syndrome. J. Adolesc. Health 2003, 1, 94–97. [Google Scholar] [CrossRef] [PubMed]
- van der Burgt, I. Noonan syndrome. Orphanet. J. Rare Dis. 2007, 2, 4. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Nadler, M.J.; Brennan, L.A.; Gish, G.D.; Timms, J.F.; Fusaki, N.; Jongstra-Bilen, J.; Tada, N.; Pawson, T.; Wither, J.; et al. The B-cell transmembrane protein CD72 binds to and is an in vivo substrate of the protein tyrosine phosphatase SHP-1. Curr. Biol. 1998, 18, 1009–1017. [Google Scholar] [CrossRef] [PubMed]
- Mustelin, T.; Vang, T.; Bottini, N. Protein tyrosine phosphatases and the immune response. Nat. Rev. Immunol. 2005, 5, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Stone, J.C. Regulation of Ras in lymphocytes: Get a GRP. Biochem. Soc. Trans. 2006, 5, 858–861. [Google Scholar] [CrossRef] [PubMed]
- Mor, A.; Philips, M.R.; Pillinger, M.H. The role of Ras signaling in lupus T lymphocytes: Biology and pathogenesis. Clin. Immunol. 2007, 3, 215–223. [Google Scholar] [CrossRef]
- Shields, J.A.; Shields, C.L.; Honavar, S.G.; Demirci, H.; Cater, J. Classification and management of Coats disease: The 2000 Proctor Lecture. Am. J. Ophthalmol. 2001, 5, 572–583. [Google Scholar] [CrossRef]
- Daruich, A.L.; Moulin, A.P.; Tran, H.V.; Matet, A.; Munier, F.L. Subfoveal nodule in Coats’ disease: Toward an Updated Classification Predicting Visual Prognosis. Retina 2017, 8, 1591–1598. [Google Scholar] [CrossRef]
- Sen, M.; Shields, C.L.; Honavar, S.G.; Shields, J.A. Coats disease: An overview of classification, management and outcomes. Indian J. Ophthalmol. 2019, 67, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Dalvin, L.A.; Udyaver, S.; Lim, L.S.; Mazloumi, M.; Atalay, H.T.; Khoo, C.T.L.; Shields, C.L. Coats Disease: Clinical Features and Outcomes by Age Category in 351 Cases. J. Pediatr. Ophthalmol. Strabismus 2019, 5, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Al-Qahtani, A.A.; Almasaud, J.M.; Ghazi, N.G. Clinical characteristics and treatment outcomes of Coats disease in a Saudi Arabian population. Retina 2015, 10, 2091–2099. [Google Scholar] [CrossRef] [PubMed]
- Rabiolo, A.; Marchese, A.; Sacconi, R.; Cicinelli, M.V.; Grosso, A.; Querques, L.; Querques, G.; Bandello, F. Refining Coats’ disease by ultra-widefield imaging and optical coherence tomography angiography. Graefes Arch. Clin. Exp. Ophthalmol. 2017, 10, 1881–1890. [Google Scholar] [CrossRef] [PubMed]
- Egbert, P.R.; Chan, C.C.; Winter, F.C. Flat preparations of the retinal vessels in Coats’ disease. J. Pediatr. Ophthalmol. 1976, 6, 336–339. [Google Scholar] [CrossRef]
- Fernandes, B.F.; Odashiro, A.N.; Maloney, S.; Zajdenweber, M.E.; Lopes, A.G.; Burnier, M.N., Jr. Clinical- histopathological correlation in a case of Coats’ disease. Diagn. Pathol. 2006, 1, 24. [Google Scholar] [CrossRef] [PubMed]
- Ridley, M.E.; Shields, J.A.; Brown, G.C.; Tasman, W. Coats’ disease. Evaluation of management. Ophthalmology 1982, 12, 1381–1387. [Google Scholar] [CrossRef] [PubMed]
- Ghorbanian, S.; Jaulim, A.; Chatziralli, I.P. Diagnosis and treatment of coats’ disease: A review of the literature. Ophthalmologica 2012, 4, 175–182. [Google Scholar] [CrossRef]
- Mannell, H.; Krotz, F. SHP-2 regulates growth factor dependent vascular signalling and function. Mini Rev. Med. Chem. 2014, 14, 471–483. [Google Scholar] [CrossRef]
- Schon, F.; Bowler, J.; Baraitser, M. Cerebral arteriovenous malformation in Noonan’s syndrome. Postgrad. Med. J. 1992, 795, 37–40. [Google Scholar] [CrossRef]
- Ganesan, V.; Kirkham, F.J. Noonan syndrome and moyamoya. Pediatr. Neurol. 1997, 3, 256–258. [Google Scholar] [CrossRef]
- Wang, S.; Yu, W.M.; Zhang, W.; McCrae, K.R.; Neel, B.G.; Qu, C.K. Noonan syndrome/leukemia-associated gain-of-function mutations in SHP-2 phosphatase (PTPN11) enhance cell migration and angiogenesis. J. Biol. Chem. 2009, 284, 913–920. [Google Scholar] [CrossRef]
- Loh, M.L.; Vattikuti, S.; Schubbert, S.; Reynolds, M.G.; Carlson, E.; Lieuw, K.H.; Cheng, J.W.; Lee, C.M.; Stokoe, D.; Bonifas, J.M.; et al. Mutations in PTPN11 implicate the SHP-2 phosphatase in leukemogenesis. Blood 2004, 6, 2325–2331. [Google Scholar] [CrossRef]
- Bentires-Alj, M.; Paez, J.G.; David, F.S.; Keilhack, H.; Halmos, B.; Naoki, K.; Maris, J.M.; Richardson, A.; Bardelli, A.; Sugarbaker, D.J.; et al. Activating mutations of the noonan syndrome-associated SHP2/PTPN11 gene in human solid tumors and adult acute myelogenous leukemia. Cancer Res. 2004, 24, 8816–8820. [Google Scholar] [CrossRef]
- Hirawat, R.; Sawal, R.; Vaidya, H. Atypical rubella retinopathy in a child with Noonan syndrome. Indian J. Ophthalmol. 2022, 70, 2769. [Google Scholar] [CrossRef] [PubMed]





| Stage | Fundus Features |
|---|---|
| 1 | Retinal telangiectasia only |
| 2 | Teleangiectasia and exudation A. extrafoveal exudation B. foveal exudation 1. without subfoveal nodule 2. with subfoveal nodule |
| 3 | Exudative retinal detachment A. subtotal detachment 1. extrafoveal 2. foveal B. total retinal detachment |
| 4 | Total retinal detachment and glaucoma |
| 5 | Advanced end-stage disease |
| Stage | Treatment | |
|---|---|---|
| 1 | Laser photocoagulation or cryotherapy | |
| 2 | ||
| 3 | Laser photocoagulation or cryotherapy; external drainage of total retinal detachment can be beneficial | |
| 4 | External drainage of total retinal detachment; vitreoretinal surgery; glaucoma surgery may be necessary; occasionally, observation is advised | |
| 5 | asymptomatic | Observation |
| with painful eye | Enucleation | |
| Adjuvant therapy: intravitreal or periocular triamcinolone, anti-VEGF | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Świerczyńska, M.; Tronina, A.; Lorenc, A.; Filipek, E. Anterior Uveitis and Coats Disease in a 16-Year-Old Girl with Noonan Syndrome—A Case Report. Children 2023, 10, 1643. https://doi.org/10.3390/children10101643
Świerczyńska M, Tronina A, Lorenc A, Filipek E. Anterior Uveitis and Coats Disease in a 16-Year-Old Girl with Noonan Syndrome—A Case Report. Children. 2023; 10(10):1643. https://doi.org/10.3390/children10101643
Chicago/Turabian StyleŚwierczyńska, Marta, Agnieszka Tronina, Anna Lorenc, and Erita Filipek. 2023. "Anterior Uveitis and Coats Disease in a 16-Year-Old Girl with Noonan Syndrome—A Case Report" Children 10, no. 10: 1643. https://doi.org/10.3390/children10101643
APA StyleŚwierczyńska, M., Tronina, A., Lorenc, A., & Filipek, E. (2023). Anterior Uveitis and Coats Disease in a 16-Year-Old Girl with Noonan Syndrome—A Case Report. Children, 10(10), 1643. https://doi.org/10.3390/children10101643






