Comparison of Characteristics and Survival Rates of Resectable Pancreatic Ductal Adenocarcinoma according to Tumor Location
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Preoperative Evaluation and Surgical Procedure
2.3. Data Collection
2.4. Outcome
2.5. Statistical Analysis
3. Results
3.1. Comparison of Patient Characteristics in PHC and PBTC Group
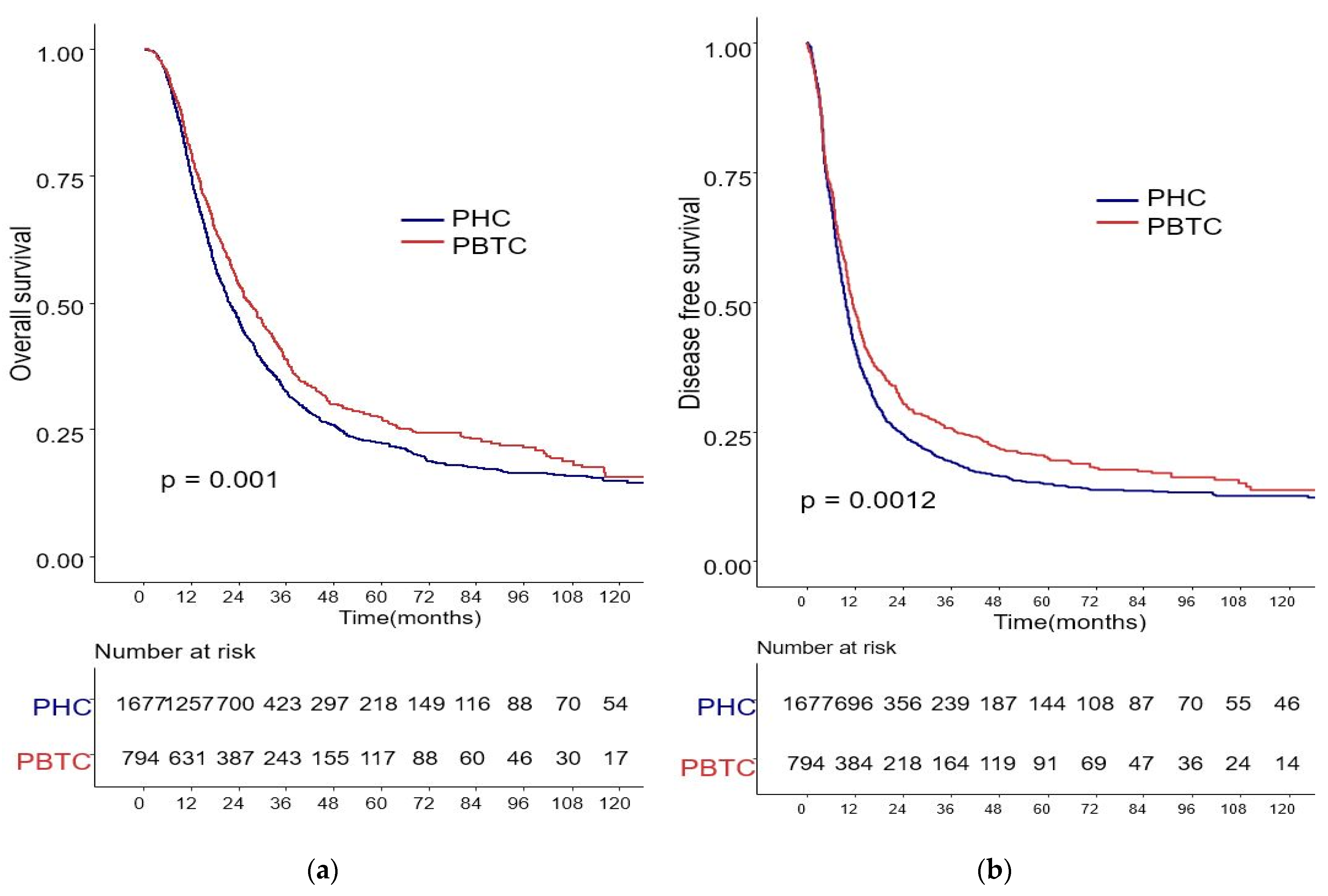
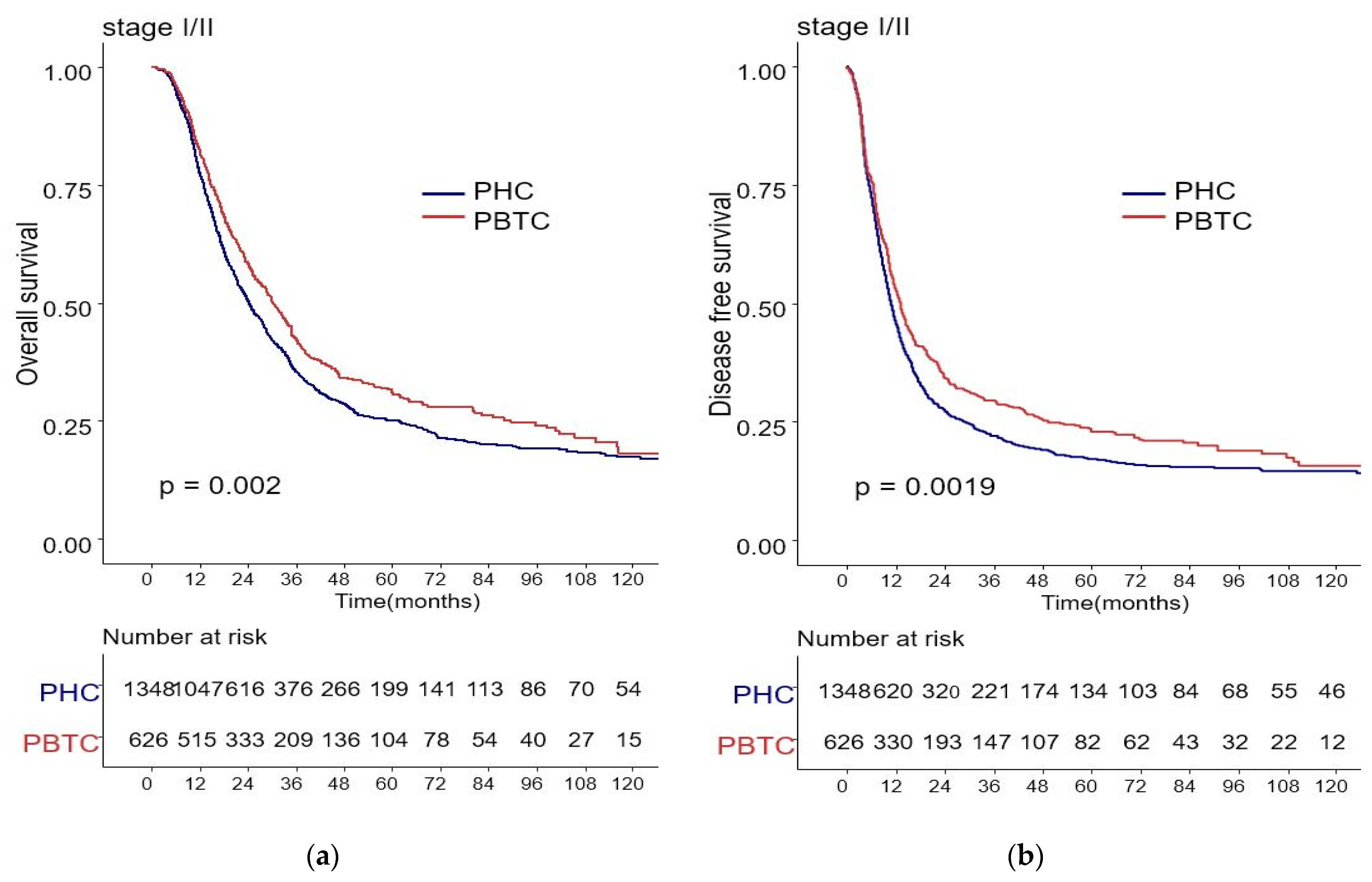
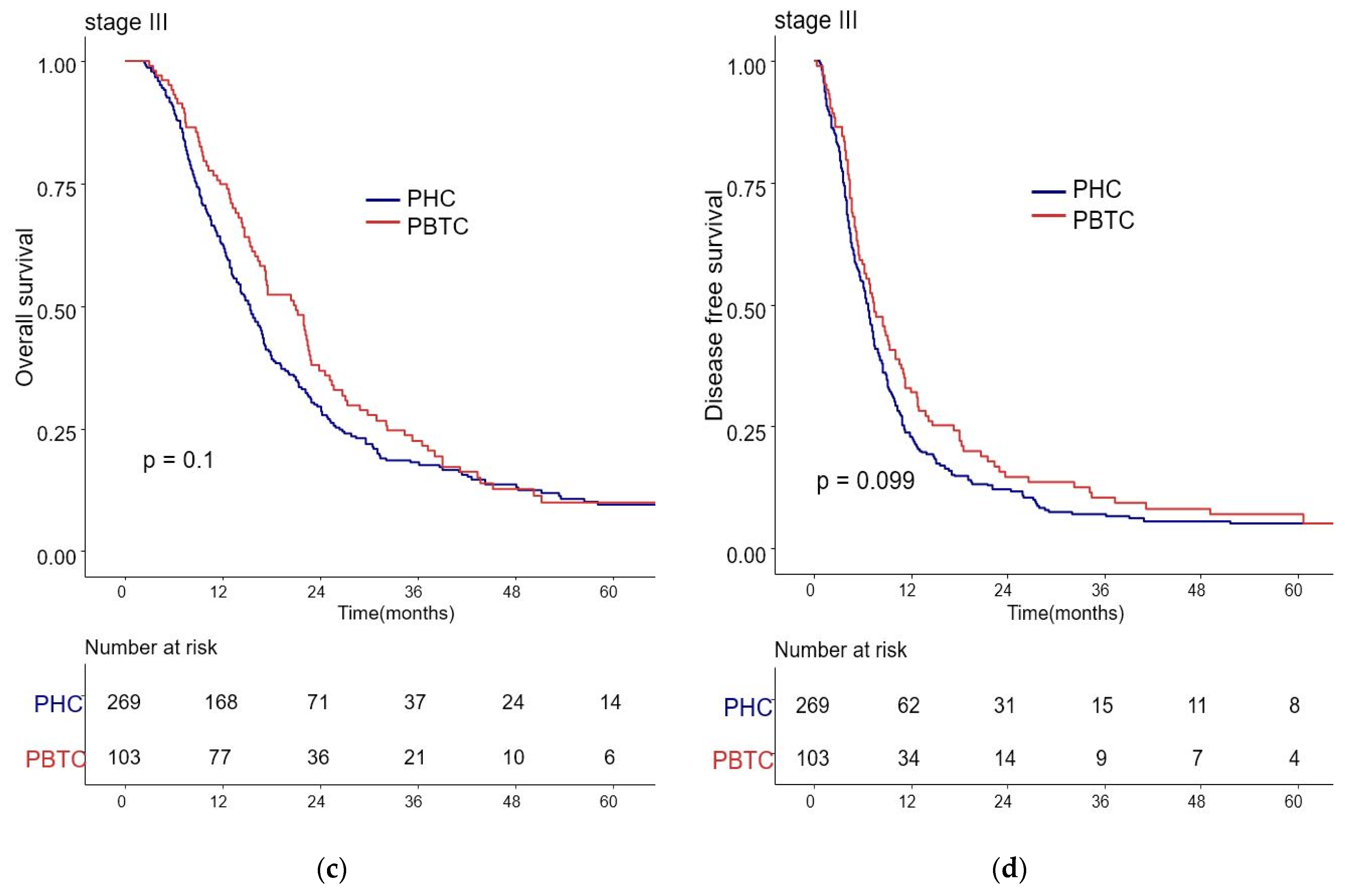
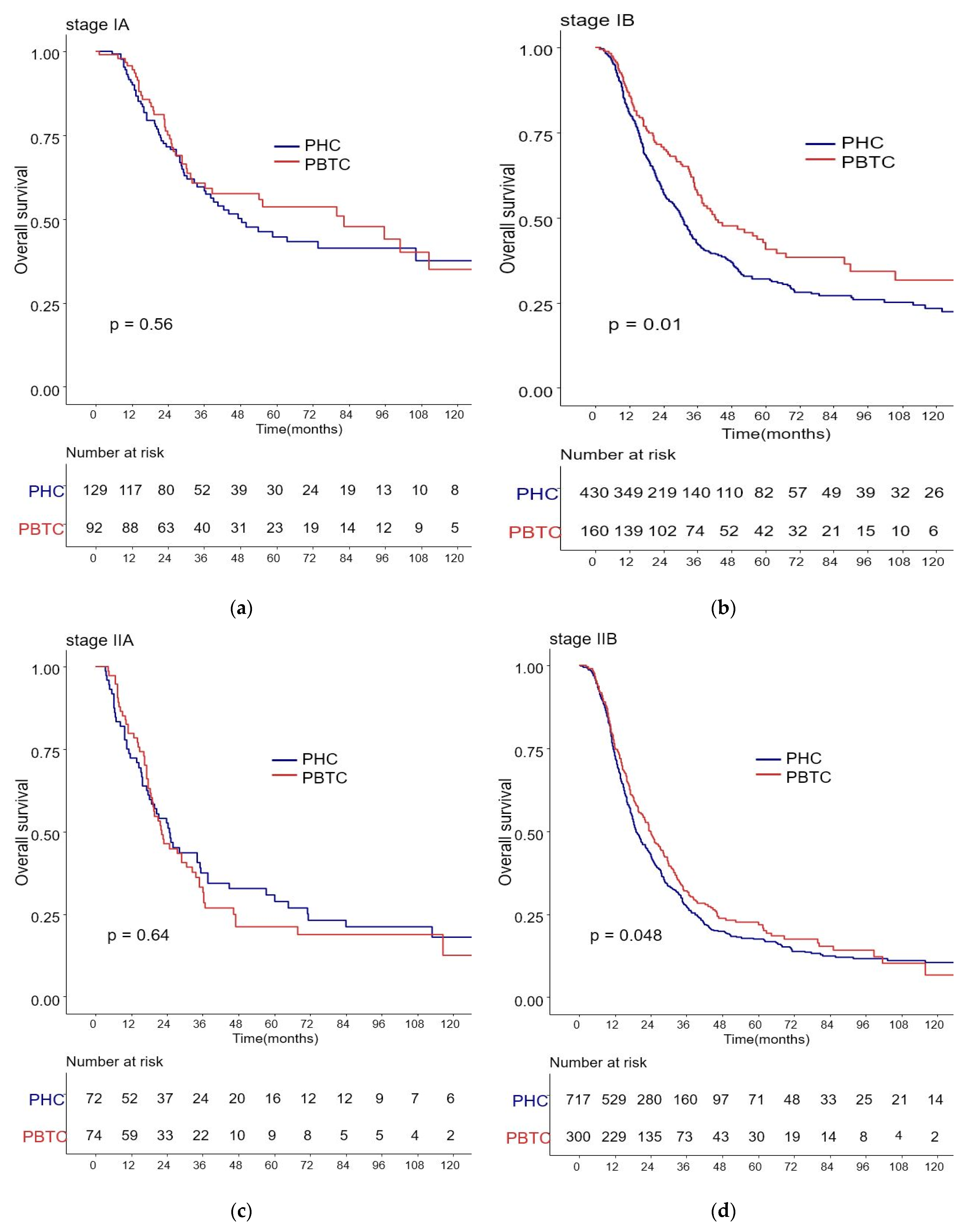
3.2. Comparison of Survival Rates for PHC and PBTC Patients
3.3. Potential Predictors for Overall Survival of PDAC Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pourshams, A.; Sepanlou, S.G.; Ikuta, K.S.; Bisignano, C.; Safiri, S.; Roshandel, G.; Sharif, M.; Khatibian, M.; Fitzmaurice, C.; Nixon, M.R.; et al. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. Gastroenterol. Hepatol. 2019, 4, 934–947. [Google Scholar] [CrossRef]
- Rawla, P.; Sunkara, T.; Gaduputi, V. Epidemiology of Pancreatic Cancer: Global Trends, Etiology and Risk Factors. World J. Oncol. 2019, 10, 10–27. [Google Scholar] [CrossRef]
- McGuigan, A.; Kelly, P.; Turkington, R.C.; Jones, C.; Coleman, H.G.; McCain, R.S. Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J. Gastroenterol. 2018, 24, 4846–4861. [Google Scholar] [CrossRef]
- Artinyan, A.; Soriano, P.A.; Prendergast, C.; Low, T.; Ellenhorn, J.D.; Kim, J. The anatomic location of pancreatic cancer is a prognostic factor for survival. HPB Off. J. Int. Hepato Pancreato Biliary Assoc. 2008, 10, 371–376. [Google Scholar] [CrossRef] [PubMed]
- van Erning, F.N.; Mackay, T.M.; van der Geest, L.G.M.; Groot Koerkamp, B.; van Laarhoven, H.W.M.; Bonsing, B.A.; Wilmink, J.W.; van Santvoort, H.C.; de Vos-Geelen, J.; van Eijck, C.H.J.; et al. Association of the location of pancreatic ductal adenocarcinoma (head, body, tail) with tumor stage, treatment, and survival: A population-based analysis. Acta Oncol. 2018, 57, 1655–1662. [Google Scholar] [CrossRef] [PubMed]
- Tomasello, G.; Ghidini, M.; Costanzo, A.; Ghidini, A.; Russo, A.; Barni, S.; Passalacqua, R.; Petrelli, F. Outcome of head compared to body and tail pancreatic cancer: A systematic review and meta-analysis of 93 studies. J. Gastrointest. Oncol. 2019, 10, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Ruess, D.A.; Makowiec, F.; Chikhladze, S.; Sick, O.; Riediger, H.; Hopt, U.T.; Wittel, U.A. The prognostic influence of intrapancreatic tumor location on survival after resection of pancreatic ductal adenocarcinoma. BMC Surg. 2015, 15, 123. [Google Scholar] [CrossRef] [PubMed]
- Meng, Z.; Cao, M.; Zhang, Y.; Liu, Z.; Wu, S.; Wu, H. Tumor location as an indicator of survival in T1 resectable pancreatic ductal adenocarcinoma: A propensity score-matched analysis. BMC Gastroenterol. 2019, 19, 59. [Google Scholar] [CrossRef]
- Lau, M.K.; Davila, J.A.; Shaib, Y.H. Incidence and survival of pancreatic head and body and tail cancers: A population-based study in the United States. Pancreas 2010, 39, 458–462. [Google Scholar] [CrossRef]
- Brennan, M.F.; Moccia, R.D.; Klimstra, D. Management of adenocarcinoma of the body and tail of the pancreas. Ann. Surg. 1996, 223, 506–511; discussion 511–512. [Google Scholar] [CrossRef]
- Sheng, W.; Dong, M.; Wang, G.; Shi, X.; Gao, W.; Wang, K.; Song, H.; Shi, G.; Tan, X. The diversity between curatively resected pancreatic head and body-tail cancers based on the 8th edition of AJCC staging system: A multicenter cohort study. BMC Cancer 2019, 19, 981. [Google Scholar] [CrossRef] [PubMed]
- Malleo, G.; Maggino, L.; Ferrone, C.R.; Marchegiani, G.; Luchini, C.; Mino-Kenudson, M.; Paiella, S.; Qadan, M.; Scarpa, A.; Lillemoe, K.D.; et al. Does Site Matter? Impact of Tumor Location on Pathologic Characteristics, Recurrence, and Survival of Resected Pancreatic Ductal Adenocarcinoma. Ann. Surg. Oncol. 2020, 27, 3898–3912. [Google Scholar] [CrossRef] [PubMed]
- Birnbaum, D.J.; Bertucci, F.; Finetti, P.; Birnbaum, D.; Mamessier, E. Head and Body/Tail Pancreatic Carcinomas Are Not the Same Tumors. Cancers 2019, 11, 497. [Google Scholar] [CrossRef]
- Yin, L.; Xiao, L.; Gao, Y.; Wang, G.; Gao, H.; Peng, Y.; Zhu, X.; Wei, J.; Miao, Y.; Jiang, K.; et al. Comparative bioinformatical analysis of pancreatic head cancer and pancreatic body/tail cancer. Med. Oncol. 2020, 37, 46. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, J.; Saiura, A.; Koga, R.; Seki, M.; Katori, M.; Kato, Y.; Sakamoto, Y.; Kokudo, N.; Yamaguchi, T. Improved survival of left-sided pancreas cancer after surgery. Jpn. J. Clin. Oncol. 2010, 40, 530–536. [Google Scholar] [CrossRef]
- Watanabe, I.; Sasaki, S.; Konishi, M.; Nakagohri, T.; Inoue, K.; Oda, T.; Kinoshita, T. Onset symptoms and tumor locations as prognostic factors of pancreatic cancer. Pancreas 2004, 28, 160–165. [Google Scholar] [CrossRef]
- Sohn, T.A.; Yeo, C.J.; Cameron, J.L.; Koniaris, L.; Kaushal, S.; Abrams, R.A.; Sauter, P.K.; Coleman, J.; Hruban, R.H.; Lillemoe, K.D. Resected adenocarcinoma of the pancreas-616 patients: Results, outcomes, and prognostic indicators. J. Gastrointest. Surg. 2000, 4, 567–579. [Google Scholar] [CrossRef]
- Wade, T.P.; Virgo, K.S.; Johnson, F.E. Distal pancreatectomy for cancer: Results in U.S. Department of Veterans Affairs hospitals, 1987–1991. Pancreas 1995, 11, 341–344. [Google Scholar] [CrossRef]
- Toomey, P.; Hernandez, J.; Golkar, F.; Ross, S.; Luberice, K.; Rosemurgy, A. Pancreatic adenocarcinoma: Complete tumor extirpation improves survival benefit despite larger tumors for patients who undergo distal pancreatectomy and splenectomy. J. Gastrointest. Surg. 2012, 16, 376–381. [Google Scholar] [CrossRef]
- Winer, L.K.; Dhar, V.K.; Wima, K.; Morris, M.C.; Lee, T.C.; Shah, S.A.; Ahmad, S.A.; Patel, S.H. The Impact of Tumor Location on Resection and Survival for Pancreatic Ductal Adenocarcinoma. J. Surg. Res. 2019, 239, 60–66. [Google Scholar] [CrossRef]
- Zheng, Z.; Wang, M.; Tan, C.; Chen, Y.; Ping, J.; Wang, R.; Liu, X. Disparities in survival by stage after surgery between pancreatic head and body/tail in patients with nonmetastatic pancreatic cancer. PLoS ONE 2019, 14, e0226726. [Google Scholar] [CrossRef]
- Imaoka, H.; Mizuno, N.; Hara, K.; Hijioka, S.; Tajika, M.; Tanaka, T.; Ishihara, M.; Yogi, T.; Tsutsumi, H.; Fujiyoshi, T.; et al. Evaluation of Modified Glasgow Prognostic Score for Pancreatic Cancer: A Retrospective Cohort Study. Pancreas 2016, 45, 211–217. [Google Scholar] [CrossRef]
- Distler, M.; Pilarsky, E.; Kersting, S.; Grützmann, R. Preoperative CEA and CA 19-9 are prognostic markers for survival after curative resection for ductal adenocarcinoma of the pancreas—A retrospective tumor marker prognostic study. Int. J. Surg. 2013, 11, 1067–1072. [Google Scholar] [CrossRef] [PubMed]
- Pulvirenti, A.; Ramera, M.; Bassi, C. Modifications in the International Study Group for Pancreatic Surgery (ISGPS) definition of postoperative pancreatic fistula. Transl. Gastroenterol. Hepatol. 2017, 2, 107. [Google Scholar] [CrossRef] [PubMed]
- Téoule, P.; Bartel, F.; Birgin, E.; Rückert, F.; Wilhelm, T.J. The Clavien-Dindo Classification in Pancreatic Surgery: A Clinical and Economic Validation. J. Investig. Surg. Off. J. Acad. Surg. Res. 2019, 32, 314–320. [Google Scholar] [CrossRef]
- Chun, Y.S.; Pawlik, T.M.; Vauthey, J.N. 8th Edition of the AJCC Cancer Staging Manual: Pancreas and Hepatobiliary Cancers. Ann. Surg. Oncol. 2018, 25, 845–847. [Google Scholar] [CrossRef]
- Chatterjee, D.; Katz, M.H.; Rashid, A.; Wang, H.; Iuga, A.C.; Varadhachary, G.R.; Wolff, R.A.; Lee, J.E.; Pisters, P.W.; Crane, C.H.; et al. Perineural and intraneural invasion in posttherapy pancreaticoduodenectomy specimens predicts poor prognosis in patients with pancreatic ductal adenocarcinoma. Am. J. Surg. Pathol. 2012, 36, 409–417. [Google Scholar] [CrossRef]
- Fernández-Cruz, L.; Johnson, C.; Dervenis, C. Locoregional dissemination and extended lymphadenectomy in pancreatic cancer. Dig. Surg. 1999, 16, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Malleo, G.; Maggino, L.; Ferrone, C.R.; Marchegiani, G.; Mino-Kenudson, M.; Capelli, P.; Rusev, B.; Lillemoe, K.D.; Bassi, C.; Fernàndez-Del Castillo, C.; et al. Number of Examined Lymph Nodes and Nodal Status Assessment in Distal Pancreatectomy for Body/Tail Ductal Adenocarcinoma. Ann. Surg. 2019, 270, 1138–1146. [Google Scholar] [CrossRef]
- Moon, H.J.; An, J.Y.; Heo, J.S.; Choi, S.H.; Joh, J.W.; Kim, Y.I. Predicting survival after surgical resection for pancreatic ductal adenocarcinoma. Pancreas 2006, 32, 37–43. [Google Scholar] [CrossRef]
- Sivasanker, M.; Desouza, A.; Bhandare, M.; Chaudhari, V.; Goel, M.; Shrikhande, S.V. Radical antegrade modular pancreatosplenectomy for all pancreatic body and tail tumors: Rationale and results. Langenbeck’s Arch. Surg. 2019, 404, 183–190. [Google Scholar] [CrossRef]
- Mehrabi, A.; Hafezi, M.; Arvin, J.; Esmaeilzadeh, M.; Garoussi, C.; Emami, G.; Kössler-Ebs, J.; Müller-Stich, B.P.; Büchler, M.W.; Hackert, T.; et al. A systematic review and meta-analysis of laparoscopic versus open distal pancreatectomy for benign and malignant lesions of the pancreas: It’s time to randomize. Surgery 2015, 157, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Ricci, C.; Casadei, R.; Taffurelli, G.; Pacilio, C.A.; Minni, F. Laparoscopic distal pancreatectomy: Many meta-analyses, few certainties. Updates Surg. 2016, 68, 225–234. [Google Scholar] [CrossRef] [PubMed]
- de Rooij, T.; van Hilst, J.; Busch, O.R.; Dijkgraaf, M.G.; Kooby, D.A.; Abu Hilal, M.; Besselink, M.G. Laparoscopic Distal Pancreatectomy for Pancreatic Ductal Adenocarcinoma: Time for a Randomized Controlled Trial? Results of an All-inclusive National Observational Study. Ann. Surg. 2017, 266, e84. [Google Scholar] [CrossRef]
- Moole, H.; Bechtold, M.; Puli, S.R. Efficacy of preoperative biliary drainage in malignant obstructive jaundice: A meta-analysis and systematic review. World J. Surg. Oncol. 2016, 14, 182. [Google Scholar] [CrossRef] [PubMed]
- Li, A.; Yu, J.; Kim, H.; Wolfgang, C.L.; Canto, M.I.; Hruban, R.H.; Goggins, M. MicroRNA array analysis finds elevated serum miR-1290 accurately distinguishes patients with low-stage pancreatic cancer from healthy and disease controls. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2013, 19, 3600–3610. [Google Scholar] [CrossRef]
- Ling, Q.; Xu, X.; Ye, P.; Xie, H.; Gao, F.; Hu, Q.; Liu, Z.; Wei, X.; Röder, C.; Trauzold, A.; et al. The prognostic relevance of primary tumor location in patients undergoing resection for pancreatic ductal adenocarcinoma. Oncotarget 2017, 8, 15159–15167. [Google Scholar] [CrossRef] [PubMed]
- Morales-Oyarvide, V.; Rubinson, D.A.; Dunne, R.F.; Kozak, M.M.; Bui, J.L.; Yuan, C.; Qian, Z.R.; Babic, A.; Da Silva, A.; Nowak, J.A.; et al. Lymph node metastases in resected pancreatic ductal adenocarcinoma: Predictors of disease recurrence and survival. Br. J. Cancer 2017, 117, 1874–1882. [Google Scholar] [CrossRef]
- Comito, T.; Cozzi, L.; Zerbi, A.; Franzese, C.; Clerici, E.; Tozzi, A.; Iftode, C.; Navarria, P.; D’Agostino, G.; Fogliata, A.; et al. Clinical results of stereotactic body radiotherapy (SBRT) in the treatment of isolated local recurrence of pancreatic cancer after R0 surgery: A retrospective study. Eur. J. Surg. Oncol. 2017, 43, 735–742. [Google Scholar] [CrossRef]
- Groot, V.P.; van Santvoort, H.C.; Rombouts, S.J.; Hagendoorn, J.; Borel Rinkes, I.H.; van Vulpen, M.; Herman, J.M.; Wolfgang, C.L.; Besselink, M.G.; Molenaar, I.Q. Systematic review on the treatment of isolated local recurrence of pancreatic cancer after surgery; re-resection, chemoradiotherapy and SBRT. HPB Off. J. Int. Hepato Pancreato Biliary Assoc. 2017, 19, 83–92. [Google Scholar] [CrossRef]
- Wang, L.; Cheng, C.S.; Chen, L.; Chen, Z. Benefit from the inclusion of surgery in the treatment of patients with stage III pancreatic cancer: A propensity-adjusted, population-based SEER analysis. Cancer Manag. Res. 2018, 10, 1907–1918. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dreyer, S.B.; Jamieson, N.B.; Upstill-Goddard, R.; Bailey, P.J.; McKay, C.J.; Biankin, A.V.; Chang, D.K. Defining the molecular pathology of pancreatic body and tail adenocarcinoma. Br. J. Surg. 2018, 105, e183–e191. [Google Scholar] [CrossRef] [PubMed]
| Total | PHC Patients | PBTC Patients | p-Value | ||
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | |||
| Age (year) | <65 | 1424 (57.6) | 981 (58.5) | 443 (55.8) | 0.204 |
| ≥65 | 1047 (42.4) | 696 (41.5) | 351 (44.2) | ||
| Sex | Male | 1465 (59.3) | 675 (40.3) | 331 (41.7) | 0.407 |
| Female | 1006 (40.7) | 1002 (59.7) | 463 (58.3) | ||
| BMI (kg/m2) | <25 | 1912 (77.4) | 1335 (79.6) | 577 (72.7) | <0.001 |
| ≥25 | 599 (22.6) | 342 (20.4) | 217 (27.3) | ||
| ASA scores | 1 | 54 (2.6) | 33 (2.5) | 21 (2.9) | 0.090 |
| 2 | 1881 (92.0) | 1245 (93.4) | 636 (89.1) | ||
| 3 | 108 (5.3) | 54 (4.1) | 54 (7.6) | ||
| 4 | 3 (0.1) | 0 (0.0) | 3 (0.4) | ||
| CA 19-9 | Normal | 811 (32.8) | 516 (31.6) | 295 (38.0) | 0.002 |
| Increased | 1599 (64.7) | 1118 (68.4) | 481 (62.0) | ||
| CEA | Normal | 1879 (76.0) | 1263 (81.6) | 616 (83.0) | 0.421 |
| Increased | 410 (16.6) | 284 (18.4) | 126 (17.0) | ||
| mGPS | 0 | 2103 (85.1) | 1386 (82.6) | 717 (90.3) | <0.001 |
| 1 | 128 (5.2) | 94 (5.6) | 34 (4.3) | ||
| 2 | 240 (9.7) | 197 (11.8) | 43 (5.4) | ||
| Period | 2000–2009 | 722 (29.2) | 514 (30.0) | 208 (25.4) | 0.023 |
| 2010–2018 | 1749 (70.8) | 1163 (69.3) | 586 (73.8) | ||
| Length of hospital stay | ≤15 | 1287 (52.1) | 767 (45.7) | 520 (65.5) | <0.001 |
| >15 | 1184 (47.9) | 1481 (54.3) | 274 (34.5) | ||
| POPF | No | 2047 (82.8) | 1484 (88.5) | 563 (70.9) | <0.001 |
| Grade A | 298 (12.1) | 133 (7.9) | 165 (20.8) | ||
| Grade B or C | 126 (5.1) | 60 (3.6) | 66 (8.3) | ||
| Complications | No | 1595 (64.7) | 1085 (64.9) | 510 (64.4) | 0.059 |
| Grade I–II | 683 (27.7) | 475 (28.4) | 208 (26.3) | ||
| Grade III–IV | 187 (7.6) | 113 (6.8) | 74 (9.3) | ||
| Adjuvant therapy | No | 707 (29.2) | 492 (29.9) | 215 (27.5) | 0.289 |
| CTx | 1321 (54.5) | 894 (54.4) | 427 (54.7) | ||
| CCRTx | 397 (16.3) | 258 (15.7) | 139 (17.8) |
| Total | PHC Patients | PBTC Patients | p-Value | ||
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | |||
| Operation method | Open | 2065 (83.6) | 1602(95.5) | 463 (58.3) | <0.001 |
| Lap/Robot | 406 (16.4) | 75 (4.5) | 331 (41.7) | ||
| Vein resection | No | 1828 (74.0) | 1122 (66.9) | 706 (88.9) | <0.001 |
| Yes | 643 (26.0) | 555 (33.1) | 88 (11.1) | ||
| Artery resection | No | 2344 (94.9) | 1597 (95.2) | 747 (94.1) | 0.227 |
| Yes | 127 (5.1) | 80 (4.8) | 47 (5.9) | ||
| Organ combined resection | No | 2347 (95.0) | 1643 (98.0) | 704 (88.7) | <0.001 |
| Yes | 124 (5.0) | 34 (2.0) | 90 (11.3) | ||
| Tumor size (cm) | Mean (sd) | 3.3 (1.7) | 3.2 (1.3) | 3.6 (1.9) | <0.001 |
| Differentiation | Well | 270 (10.9) | 169 (10.3) | 101 (13.0) | 0.138 |
| Moderate | 1832 (74.1) | 1257 (76.6) | 575 (74.2) | ||
| Poor | 314 (12.7) | 215 (13.1) | 99 (12.8) | ||
| T stage | T1 | 362 (14.7) | 218 (13.0) | 144 (18.1) | <0.001 |
| T2 | 1603 (64.9) | 1193 (71.2) | 410 (51.7) | ||
| T3 | 467 (18.9) | 246 (14.7) | 221 (27.9) | ||
| T4 | 37 (1.5) | 19 (1.1) | 18 (2.3) | ||
| N stage | N0 | 996 (40.3) | 642 (38.5) | 354 (45.3) | 0.002 |
| N1 | 1072 (43.4) | 745 (44.6) | 327 (41.8) | ||
| N2 | 383 (15.5) | 282 (16.9) | 101 (12.9) | ||
| M stage | M0 | 2368 (95.8) | 1626 (97.0) | 742 (93.5) | <0.001 |
| M1 | 103 (4.2) | 51 (3.0) | 52 (6.5) | ||
| Staging | IA | 221 (9.0) | 129 (7.7) | 92 (11.8) | <0.001 |
| IB | 590 (24.1) | 430 (25.8) | 160 (20.5) | ||
| IIA | 146 (6.0) | 72 (4.3) | 74 (9.5) | ||
| IIB | 1017 (41.5) | 717 (43.0) | 300 (38.4) | ||
| III | 372 (15.2) | 269 (16.1) | 103 (13.2) | ||
| IV | 103 (4.2) | 51 (3.1) | 52 (6.6) | ||
| LVI | No | 1163 (47.1) | 718 (42.8) | 445 (56.0) | <0.001 |
| Yes | 1308 (52.9) | 959 (57.2) | 349 (44.0) | ||
| PNI | No | 466 (18.9) | 271 (16.2) | 195 (24.6) | <0.001 |
| Yes | 2005 (81.1) | 1406 (83.8) | 599 (75.4) | ||
| RM | R0 | 1896 (75.6) | 1284 (76.6) | 585 (73.7) | 0.118 |
| R1 | 602 (24.4) | 393 (23.4) | 209 (26.3) |
| Univariate | Multivariate | ||||
|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | ||||
| Location | Head | 1.000 | 1.000 | ||
| Body/tail | 0.846 (0.766–0.935) | 0.001 | 1.041 (0.923–1.173) | 0.513 | |
| Age (yrs) | <65 | 1.000 | |||
| ≥65 | 1.086 (0.989–1.192) | 0.084 | |||
| Sex | Male | 1.000 | |||
| Female | 1.126 (1.025–1.237) | 0.014 | |||
| BMI (kg/m2) | <25 | 1.000 | 1.000 | ||
| ≥25 | 0.799 (0.712–0.896) | 0.001 | 0.862 (0.767–0.968) | 0.012 | |
| CA 19-9 | Normal | 1.000 | 1.000 | ||
| Increased | 1.377 (1.245–1.524) | 0.001 | 1.197 (1.080–1.325) | 0.001 | |
| CEA | Normal | 1.000 | |||
| Increased | 1.201 (1.061–1.359) | 0.004 | |||
| mGPS | 0 | 1.000 | 1.000 | ||
| 1 | 1.252 (1.029–1.523) | 0.025 | 1.265 (1.038–1.541) | 0.020 | |
| 2 | 1.290 (1.112–1.495) | 0.001 | 1.080 (0.929–1.257) | 0.315 | |
| Period | 2000–2009 | 1.000 | |||
| 2010–2018 | 0.663 (0.601–0.730) | 0.001 | |||
| Length of hospital stay | ≤15 | 1.000 | 1.000 | ||
| >15 | 1.457 (1.328–1.598) | 0.001 | 1.266 (1.144–1.401) | 0.001 | |
| POPF | No | 1.000 | |||
| Grade A | 0.882 (0.766–1.017) | 0.084 | |||
| Grade B or C | 0.976 (0.793–1.203) | 0.823 | |||
| Complications | No | 1.000 | 1.000 | ||
| Grade I–II | 1.179 (1.065–1.307) | 0.002 | 1.134 (1.020–1.262) | 0.021 | |
| Grade III–IV | 1.115 (0.929–1.337) | 0.243 | 1.041 (0.863–1.256) | 0.672 | |
| Adjuvant therapy | No | 1.000 | 1.000 | ||
| CTx | 0.737 (0.664–0.819) | 0.001 | 0.703 (0.632–0.782) | 0.001 | |
| CCRTx | 0.807 (0.702–0.928) | 0.003 | 0.633 (0.547–0.733) | 0.001 | |
| Operation method | Open | 1.000 | 1.000 | ||
| Lap/robot | 0.601 (0.522–0.692) | 0.001 | 0.749 (0.638–0.879) | 0.001 | |
| Vein resection | No | 1.000 | 1.000 | ||
| Yes | 1.557 (1.407–1.724) | 0.001 | 1.222 (1.096–1.363) | 0.001 | |
| Artery resection | No | 1.000 | |||
| Yes | 1.587 (1.315–1.916) | 0.001 | |||
| Combined resection | No | 1.000 | |||
| Yes | 1.138 (0.928–1.397) | 0.214 | |||
| Tumor size (cm) | 1.174 (1.145–1.205) | 0.001 | 1.114 (1.078–1.151) | 0.001 | |
| Differentiation | Well | 1.000 | 1.000 | ||
| Moderate | 1.689 (1.430–1.994) | 0.001 | 1.457 (1.236–1.718) | 0.001 | |
| Poor | 2.858 (2.342–3.486) | 0.001 | 2.393 (1.965–2.915) | 0.001 | |
| T stage | T1 | 1.000 | |||
| T2 | 1.640 (1.416–1.901) | 0.001 | |||
| T3 | 2.257 (1.907–2.670) | 0.001 | |||
| T4 | 3.052 (2.112–4.409) | 0.001 | |||
| N stage | N0 | 1.000 | |||
| N1 | 1.681 (1.514–1.866) | 0.001 | |||
| N2 | 2.346 (2.050–2.684) | 0.001 | |||
| M stage | M0 | 1.000 | |||
| M1 | 1.961 (1.591–2.417) | 0.001 | |||
| TNM stage | IA | 1.000 | 1.000 | ||
| IB | 1.460 (1.177–1.813) | 0.001 | 1.104 (0.885–1.378) | 0.381 | |
| IIA | 1.968 (1.508–2.568) | 0.001 | 1.142 (0.850–1.534) | 0.380 | |
| IIB | 2.424 (1.978–2.969) | 0.001 | 1.673 (1.350–2.073) | 0.001 | |
| III | 3.372 (2.705–4.204) | 0.001 | 2.182 (1.722–2.764) | 0.001 | |
| IV | 4.024 (3.043–5.321) | 0.001 | 2.530 (1.880–3.406) | 0.001 | |
| LVI | No | 1.000 | 1.000 | ||
| Yes | 1.521 (1.386–1.670) | 0.001 | 1.266 (1.147–1.398) | 0.001 | |
| PNI | No | 1.000 | |||
| Yes | 1.468 (1.295–1.664) | 0.001 | |||
| RM | R0 | 1.00 | 1.000 | ||
| R1 | 1.393 (1.256–1.546) | 0.001 | 1.194 (1.066–1.337) | 0.002 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sung, M.K.; Park, Y.; Kwak, B.J.; Jun, E.; Lee, W.; Song, K.B.; Lee, J.H.; Hwang, D.W.; Kim, S.C. Comparison of Characteristics and Survival Rates of Resectable Pancreatic Ductal Adenocarcinoma according to Tumor Location. Biomedicines 2021, 9, 1706. https://doi.org/10.3390/biomedicines9111706
Sung MK, Park Y, Kwak BJ, Jun E, Lee W, Song KB, Lee JH, Hwang DW, Kim SC. Comparison of Characteristics and Survival Rates of Resectable Pancreatic Ductal Adenocarcinoma according to Tumor Location. Biomedicines. 2021; 9(11):1706. https://doi.org/10.3390/biomedicines9111706
Chicago/Turabian StyleSung, Min Kyu, Yejong Park, Bong Jun Kwak, Eunsung Jun, Woohyung Lee, Ki Byung Song, Jae Hoon Lee, Dae Wook Hwang, and Song Cheol Kim. 2021. "Comparison of Characteristics and Survival Rates of Resectable Pancreatic Ductal Adenocarcinoma according to Tumor Location" Biomedicines 9, no. 11: 1706. https://doi.org/10.3390/biomedicines9111706
APA StyleSung, M. K., Park, Y., Kwak, B. J., Jun, E., Lee, W., Song, K. B., Lee, J. H., Hwang, D. W., & Kim, S. C. (2021). Comparison of Characteristics and Survival Rates of Resectable Pancreatic Ductal Adenocarcinoma according to Tumor Location. Biomedicines, 9(11), 1706. https://doi.org/10.3390/biomedicines9111706







