Abstract
Objective: This study aimed to investigate the application value of voxel-mirrored homotopic connectivity (VMHC) and regional homogeneity (ReHo) in evaluating cognitive impairment after heart transplantation. Methods: A total of 68 heart transplant patients and 56 healthy controls were included. ReHo and VMHC were calculated using DPARSF software. A two-sample t-test was applied to compare the differences in ReHo and VMHC between the two groups, and a Pearson correlation analysis was performed by extracting the VMHC and ReHo values of different brain regions and correlating them with cognitive scale scores of the patient groups. Results: Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA) scores were lower in the heart transplant group than in the control group (MMSE: t = 4.028, p < 0.001; MoCA: t = 4.914, p < 0.001). Compared with the control group, the ReHo values of Frontal_Sup_R (t = −4.422, p < 0.001), Thalamus_L (t = −3.911, p < 0.001), and Calcarine_L (t = −3.640, p < 0.001) were lower in the heart transplantation group, while the ReHo of Temporal_Sup_L was higher (t = 4.609, p < 0.001). VMHC was elevated for bilateral Cerebellum_Crus1 (t = 3.803, p < 0.001) and decreased for bilateral calcarine (t = −3.424, p < 0.001). The ReHo of Frontal_Sup_R was positively correlated with MMSE (r = 0.345, p = 0.004) and MoCA (r = 0.376, p = 0.002). The ReHo of Temporal_Sup_L was also positively correlated with MMSE (r = 0.397, p < 0.001) and MoCA (r = 0.542, p < 0.001). The VMHC of bilateral calcarine showed a positive correlation with MMSE (r = 0.513, p < 0.001) and MoCA (r = 0.398, p < 0.001). Other differential brain regions showed no significant correlation with the MMSE and MoCA scale scores. Conclusions: Cognitive decline was observed in heart transplant patients. Heart transplant patients exhibited altered ReHo and VMHC in several brain regions compared with healthy controls. These changes may underlie impaired cognitive function in heart transplant patients. These findings may contribute to understanding the neural mechanisms of cognitive changes in heart transplant patients and could inform future research on potential intervention strategies.
1. Introduction
Heart transplantation is a surgical procedure primarily for advanced congestive heart failure and severe coronary artery disease and is the primary treatment for end-stage heart disease [1]. According to statistics, the 1-year survival rate after heart transplantation is 87%, the 5-year survival rate is 72%, and the 10-year survival rate is expected to be 55% to 60% [2]. While heart transplantation improves overall patient function and quality of life, patients still face many challenges. Postoperative cognitive dysfunction (POCD) is a common postoperative reversible acute psychiatric disorder in heart transplant patients [3]. POCD refers to the state of cognitive impairment that develops in patients after surgical procedures, and the incidence of this condition varies (15% to 50%) depending on the risk and type of surgery [4]. The clinical features of the patients include attention deficits, impaired consciousness, changes in cognitive abilities, and disruption of sleep–wake cycles, which seriously affect the quality of life of the patients after surgery [5]. The occurrence of POCD in heart transplant patients not only increases the patient’s medical costs and prolongs the patient’s hospitalization, but also increases the patient’s mortality [6]. Therefore, in recent years, organ transplant physicians have become increasingly concerned about the occurrence of POCD after organ transplantation. Up to 40% of heart transplant patients develop cognitive impairment [7]. However, the neural mechanisms underlying cognitive impairment in heart transplant patients remain unclear.
In recent years, resting-state functional MRI (rs-fMRI) has been widely used in the study of the functional connectivity of the resting-state human brain [8]. Studies have shown that some brain regions or brain networks play an important role in human cognitive functions, such as the default mode network (DMN), which is not only involved in primary cognitive functions such as spatial location, sensation, and attention in the cognitive process [9], but is also closely related to higher cognitive functions such as social cognition, semantic memory, and logical thinking [10]. The application of some indicators in rs-fMRI to evaluate the differences in brain area activation and functional connectivity in patients with cognitive impairment is a hot research topic at this stage. Among them, VMHC is a method used to analyze the homotopic connectivity between a given voxel in the cerebral hemisphere and its mirror voxel in the contralateral hemisphere, which can reflect the functional connectivity of the brain in the resting state and is used to assess the endogenous spontaneous activity of neurons with the same origins in both cerebral hemispheres [11]. ReHo can reflect the time-series similarity between each voxel and its neighboring voxels [12]. The above metrics are effective methods for assessing functional connectivity and spontaneous activity in brain regions, but their application in evaluating impaired cognitive function in heart transplantation patients still needs to be further investigated and expanded. Therefore, the aim of this study is to apply VMHC and ReHo and combine them with cognition-related scales to provide an imaging basis for the pathogenesis of cognitive impairment in heart transplant patients.
2. Materials and Methods
2.1. Objects
Patients who underwent heart transplantation at Union Hospital of Huazhong University of Science and Technology from September 2021 to September 2023 were selected for the study. Inclusion criteria were (1) habitual right-handedness, (2) ability to communicate and understand questionnaires, (3) successful heart transplantation with an expected survival period of more than one month after discharge from the hospital, and (4) no preoperative cognitive impairment. Exclusion criteria included (1) a history of substance dependence, (2) organic brain diseases such as traumatic brain injury, epilepsy, or severe physical diseases, (3) contraindication to magnetic resonance examination (MRI), (4) joint organ transplantation, and (5) suffering from hereditary or congenital diseases. Community health volunteers were recruited as the control group during the same period. Inclusion criteria for the controls were (1) Han nationality, (2) right-handedness, and (3) no family history of mental illness. Exclusion criteria for the controls were contraindications to magnetic resonance examination. The enrollment was assisted by a cardiac surgeon with 8 years of experience, who collected basic information of all enrolled patients, such as gender, age, and years of education. All organs were donated voluntarily after death, in accordance with the Chinese Regulations on Human Organ Transplantation. No organs from death row inmates were used. All subjects or their guardians signed an informed consent form. A total of 68 patients and 57 controls were initially included. The study adhered to the Declaration of Helsinki and was approved by the Hospital Ethics Committee (approval number: 2022(0166-01)).
2.2. Cognitive Assessment
Cognitive function was assessed in all enrolled patients using the Mini-Mental State Examination (MMSE) and the Montreal Cognitive Assessment (MoCA). The MMSE measures general cognitive function and comprises six domains: orientation, registration, attention and calculation, recall, language, and visuospatial functioning. The maximum score for each domain ranges from 1 to 10, with a total possible score of 30, where higher scores indicate better general cognitive functioning [13]. The MoCA is a brief test of cognitive functioning and comprises seven domains: short-term memory, visuospatial functioning, executive functioning, attention, concentration, working memory, language, and orientation [14]. The test takes approximately ten minutes, with a total possible score of 30, where higher scores indicate better overall cognitive functioning.
2.3. MRI Data Acquisition
MRI data, including anatomical and functional images, were acquired using a Siemens Trio Tim 3.0T MRI system and a 32-channel head coil. Subjects were instructed to close their eyes, remain awake and relaxed, and wear headphones to minimize scanning noise. Foam pads were used to minimize head movement and prevent motion artifacts. Anatomical images were obtained using a high-resolution T1-weighted MP-RAGE sequence with 192 sagittal slices covering the whole brain (TR = 1900 ms; TE = 2.3 ms; TI = 900 ms; flip angle = 9°; voxel size = 0.3 × 0.3 × 0.8 mm3; FOV = 240 mm × 240 mm; slice thickness = 0.8 mm). Functional images were acquired using a gradient-echo EPI sequence with 240 volumes (TR = 2000 ms; TE = 30 ms; flip angle = 90°; voxel size = 2.4 × 2.4 × 2.4 mm3; FOV = 230 mm × 230 mm; slice thickness = 2.4 mm). Two radiologists independently reviewed the MR images for abnormalities, such as hemorrhage, ischemia, and tumors. Subjects with these abnormalities were excluded.
2.4. Data Preprocessing
Based on Matlab 2022b, the data were preprocessed using Data Processing Assistant for Resting-State fMRI Advanced edition (DPARSFA, http://www.rfmri.org/DPARSF (accessed on 10 January 2025)) software [15] with statistical parametric maps (SPM 12, http://www.fil.ion.ucl.ac.uk/spm (accessed on 10 January 2025)). The processing steps included (1) format conversion, which converted the DICOM raw data to a NIfTI format, (2) removal of the first 10 time points of the rs-fMRI data, (3) temporal layer correction, (4) head-motion correction, which removed subjects with head movements greater than 3 mm or rotations greater than 3° (three patients were excluded in the heart transplantation group, and four patients were excluded in the healthy control group), (5) spatial normalization (the head-movement-corrected functional images were aligned to the Montreal Neuroscience Institute standard space and resampled to voxel sizes of 3 mm × 3 mm × 3 mm), (6) de-linearization drift, which removes trends in nonneural activity, (7) removal of covariates, including cerebral white matter signals, cerebrospinal fluid signals, and the 24 head-movement parameters, and (8) spatial filtering, which was applied to the data from 0.01 to 0.08 Hz.
2.5. Calculation of Indicators
ReHo calculation was performed using DPARSF software (Version V5.0_200401). The time-series similarity between each voxel and its neighboring 26 voxels was assessed based on Kendall’s concordance coefficient (KCC), then the ReHo metrics were smoothed with a Gaussian kernel with a half-height and width of 6 mm × 6 mm × 6 mm, and finally, the results were normalized using Fisher-Z transformation to Z-values. The VMHC was calculated using DPARSF software (Version V5.0_200401). The Pearson correlation coefficients between mirror symmetry voxels in the whole brain were calculated to obtain the VMHC, and finally, the results were normalized to Z-values using Fisher-Z transformation.
2.6. Statistical Analysis
The demographic data of all patients were statistically analyzed along with the scale results using SPSS 27.0. Measurement information that conformed to a normal distribution was expressed as mean ± standard deviation ( ± s), and independent samples t-tests were used for comparison between groups. Count data were compared between groups using χ2 tests. The results of rs-fMRI indexes of the two groups were evaluated using the resting-state statistical analysis model (Specify 2nd-level) of SPM 12 software. Two independent samples t-tests were used to evaluate the ReHo and VMHC outcome brain maps of the two groups, with head movement, age, gender, and years of education as covariates, and the results were corrected by false discovery rates (FDRs), qualifying the voxel level at p < 0.001 and the cluster level at p < 0.05. AAL-90 templates were used for the brain regions with significant differences, and the MNI coordinates of the index peak points were extracted. The mean values of ReHo and VMHC of the brain regions with differences were extracted and analyzed by Pearson correlation with MMSE and MoCA scales, with differences considered statistically significant at p < 0.05.
3. Results
3.1. Demographics and Scale Results
A total of 68 heart transplant patients and 56 healthy controls were included in this study. The differences in age, gender, and years of education between the two groups of subjects were not statistically significant (p > 0.05). The MMSE and MoCA scale scores of the heart transplant group were lower than those of the control group, and the difference was statistically significant (MMSE: t = 4.028, p < 0.001; MoCA: t = 4.914, p < 0.001). There was a significant difference between the two groups of subjects in the six MoCA domains of visuospatial/executive (t = 7.175, p < 0.001), naming (t = 2.519, p =0.014), attention (t = 3.972, p < 0.001), language (t = 4.090, p < 0.001), abstraction (t = 5.988, p < 0.001), and memory (t = 9.729, p < 0.001), as shown in Table 1.

Table 1.
Comparison of basic data between two groups.
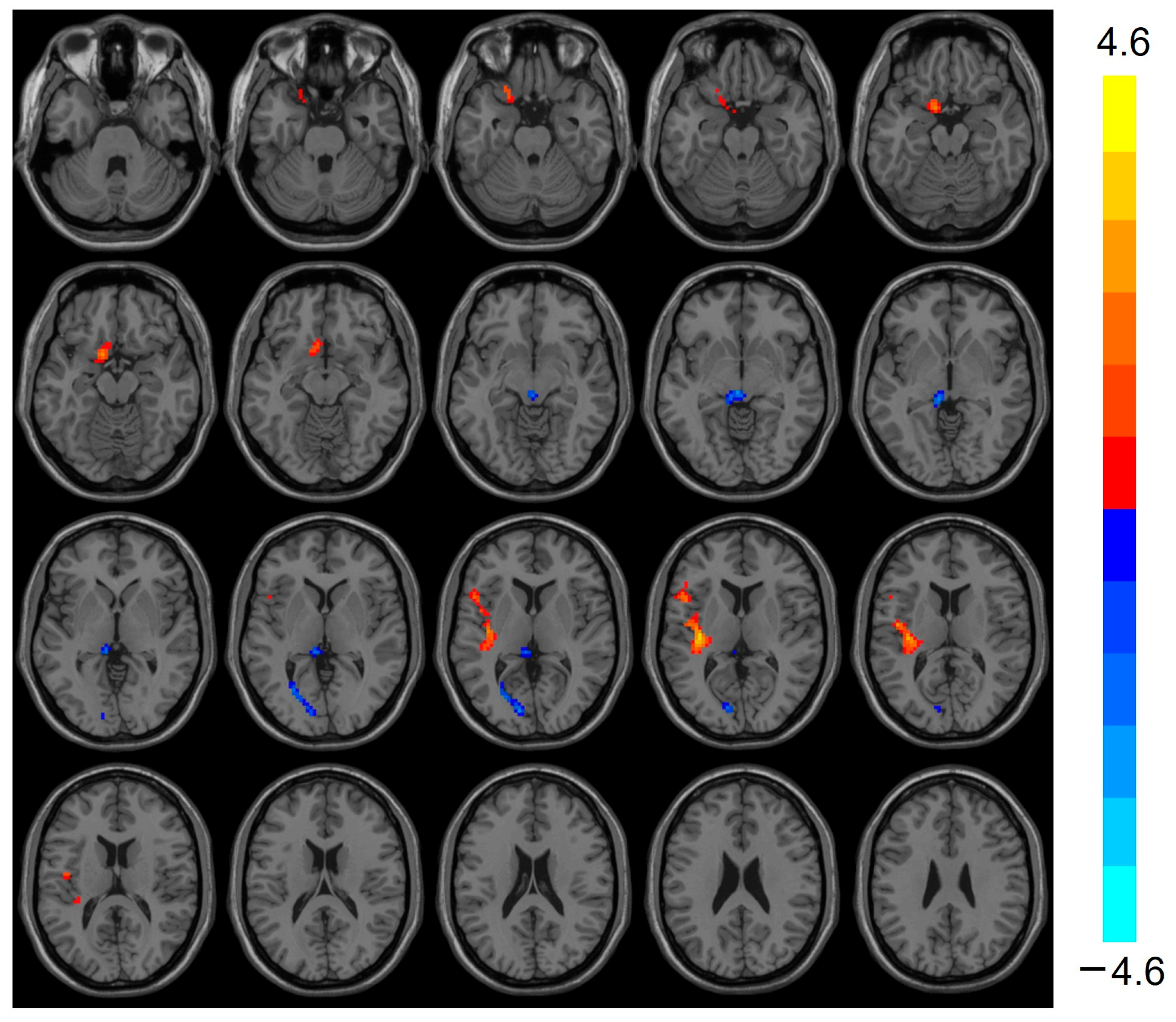
3.2. ReHo Analysis Results
Compared with the control group, the heart transplantation group exhibited reduced ReHo in the Frontal_Sup_R (t = −4.422, p < 0.001), Thalamus_L (t = −3.911, p < 0.001), and Calcarine_L (t = −3.640, p < 0.001), while the ReHo of Temporal_Sup_L was elevated (t = 4.609, p < 0.001) (see Table 2 and Figure 1).

Table 2.
Brain regions with differences in ReHo between groups.
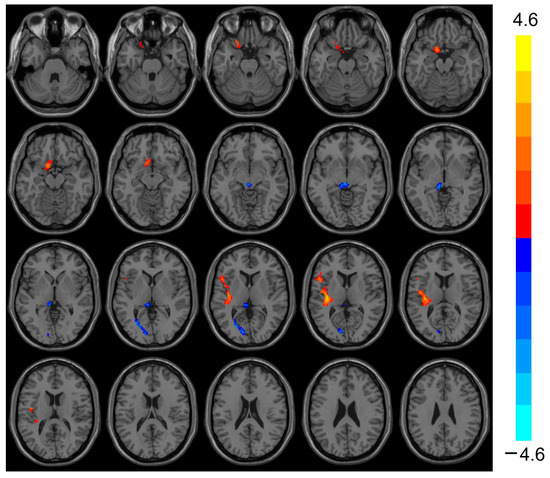
Figure 1.
Images show decreased ReHo for Frontal_Sup_R, Thalamus_L, and Calcarine_L in the heart transplantation group (blue) and increased ReHo for Temporal_Sup_L (red). Color bars on the right show t-values. ReHo, regional homogeneity.
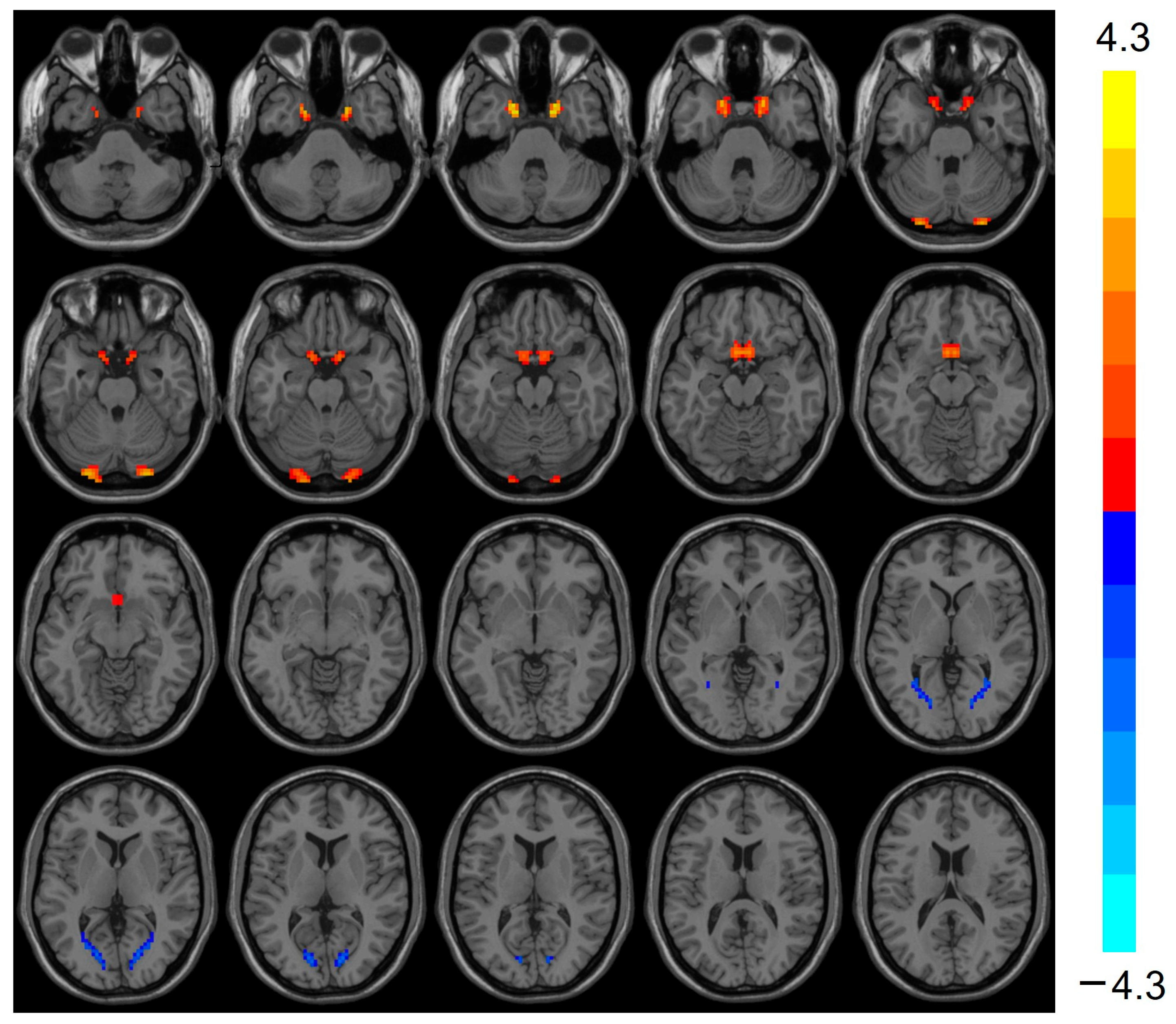
3.3. VMHC Analysis Results
VMHC was elevated (t = 3.803, p < 0.001) in the bilateral Cerebellum_Crus1 of the heart transplant group, while VMHC was reduced (t = −3.424, p < 0.001) in the bilateral calcarine, as shown in Table 3 and Figure 2.

Table 3.
Brain regions with differences in VMHC between groups.
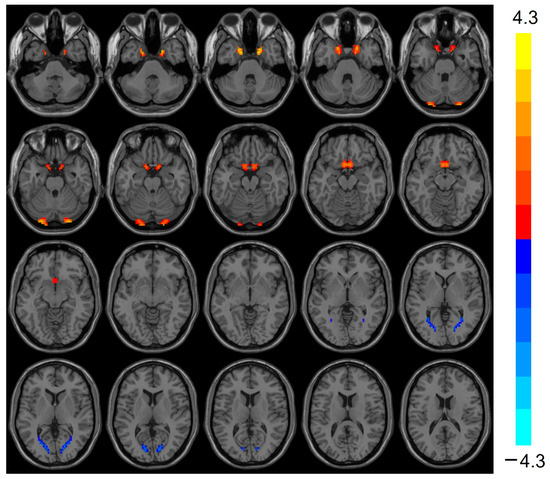
Figure 2.
VMHC values were elevated in the heart transplantation group in bilateral Cerebelum_Crus1 (red), whereas they were reduced in bilateral calcarine (blue). Color bars are t-values. VMHC, voxel-mirrored homotopic connectivity.
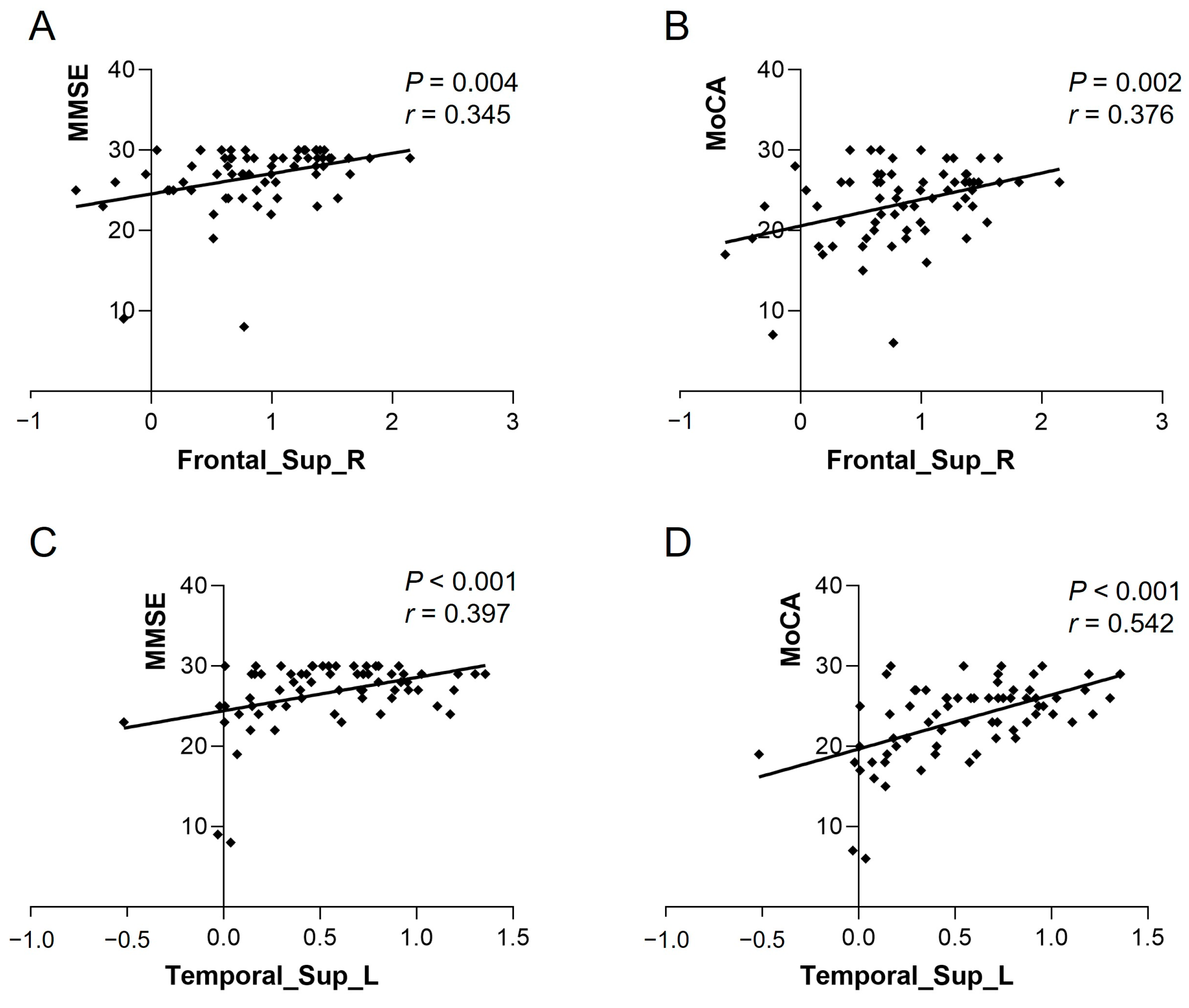
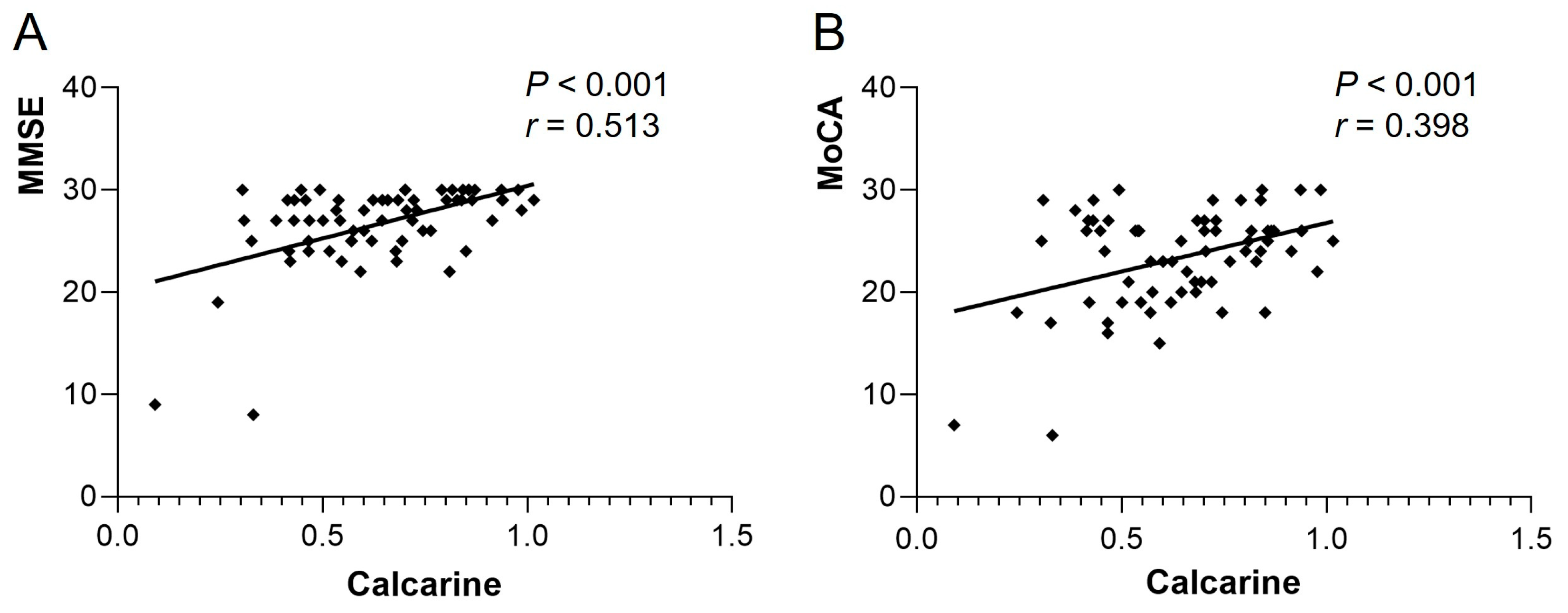
3.4. Correlation Analysis of Differential Brain Regions with Cognitive Scales
The ReHo of Frontal_Sup_R in the heart transplant group was positively correlated with MMSE (r = 0.345, p = 0.004) and MoCA (r = 0.376, p = 0.002). The ReHo of Temporal_Sup_L was also positively correlated with MMSE (r = 0.397, p < 0.001) and MoCA (r = 0.542, p < 0.001) (see Figure 3). The VMHC of bilateral calcarine in the patient group showed a positive correlation with MMSE (r = 0.513, p < 0.001) and MoCA (r = 0.398, p < 0.001) (see Figure 4). Other differential brain regions showed no significant correlation with MMSE and MoCA scale scores.
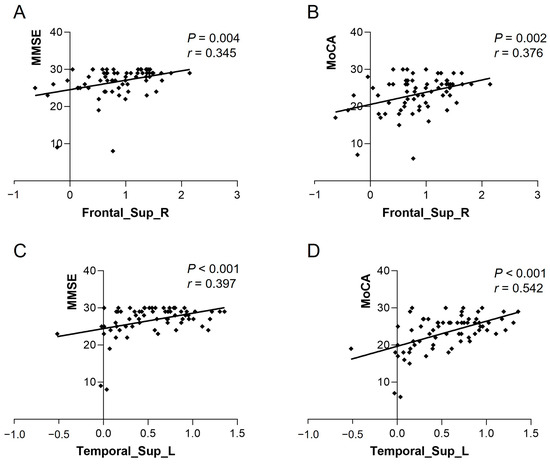
Figure 3.
ReHo values of Frontal_Sup_R in the heart transplant group were positively correlated with (A) MMSE (r = 0.345, p = 0.004) and (B) MoCA (r = 0.376, p = 0.002). ReHo values of Temporal_Sup_L were positively correlated with (C) MMSE (r = 0.397, p < 0.001) and (D) MoCA (r = 0.542, p < 0.001). ReHo, regional homogeneity; MoCA, Montreal Cognitive Assessment; MMSE, Mini-Mental State Examination.
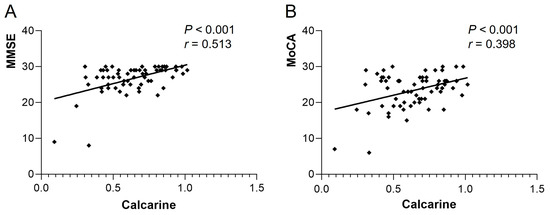
Figure 4.
VMHC of bilateral calcarine in the heart transplant group showed a positive correlation with (A) MMSE (r = 0.513, p < 0.001) and (B) MoCA (r = 0.398, p < 0.001). VMHC, voxel-mirrored homotopic connectivity; MoCA, Montreal Cognitive Assessment; MMSE, Mini-Mental State Examination.
4. Discussion
This study focused on the feasibility of applying rs-fMRI to evaluate cognitive impairment in heart transplant patients. We primarily utilized ReHo and VMHC analyses to assess the changes in functional connectivity and spontaneous brain activity between the cerebral hemispheres after heart transplantation and correlated these findings with MMSE and MoCA scales. The results demonstrated that the MMSE and MoCA scale scores were lower in the heart transplant group than in the control group. In the rs-fMRI results, several brain regions exhibited altered ReHo and VMHC in heart transplant patients, which were correlated with MMSE and MoCA scale scores. These findings may contribute to a better understanding of the neuropathophysiological mechanisms of cognitive dysfunction in heart transplant patients.
The MMSE and MoCA scales are the most widely used tools for evaluating cognitive function in clinical practice. In the present study, the reduced MMSE and MoCA scores in the heart transplant group indicated cognitive decline. Bucker et al. reported that approximately 40% of patients exhibited cognitive impairment at 3 years post-heart transplantation, primarily in domains such as processing speed, memory, language, and executive function [16]. Consistent with this finding, our study revealed cognitive impairment in six domains: visuospatial/executive function, naming, attention, language, abstraction, and memory. POCD is characterized by impaired memory, decreased information processing, and reduced attention, with a range of negative outcomes, including changes in mood and personality [17]. The one-year mortality rate after surgery is nearly twice as high in patients with POCD compared to those without POCD [18]. POCD is believed to involve pathological processes, including neuroinflammation, mitochondrial dysfunction, oxidative stress, blood–brain barrier (BBB) damage, neurotrophic support damage, and synaptic damage [19]. These molecular pathways are suspected to contribute to cognitive impairment after heart transplantation.
ReHo, calculated using Kendall’s concordance coefficient (KCC) to assess the consistency of adjacent voxels in the time series of rs-fMRI, indirectly reflects the synchronization of local spontaneous brain activities [20]. Previous studies have shown that patients with cognitive impairment exhibit altered spontaneous brain activity in the resting state. Zhang et al. found that ReHo in the medial prefrontal cortex and precuneus was significantly lower in patients with cognitive impairment compared to healthy subjects [21]. Liu et al. noted that ReHo in the right superior temporal gyrus and right middle temporal gyrus of patients with mild cognitive impairment (MCI) was significantly lower than that of healthy subjects [22]. In the present study, reduced ReHo in the Frontal_Sup_R, Thalamus_L, and Calcarine_L suggests disrupted local functional integration in these regions. The superior frontal gyrus is a crucial component of the prefrontal lobe, which is responsible for integrating internal and external environmental information, extracting environmental memories, and playing a central role in attention and executive function, and its decreased ReHo may directly contribute to the observed deficits in attention and abstraction tasks [23]. The thalamus acts as an information relay station for the brain and plays a key role in processing and transmitting sensory information [24]. It is also recognized as a critical node for coordinating cognitive functions. Its reduced ReHo could impair information transfer between cortical and subcortical regions, exacerbating memory and language deficits [25]. The calcarine sulcus belongs to the occipital cortex, which is involved in memory, speech, attention, and executive functions in addition to visual information processing as an important visual center [26]. This finding is generally consistent with our results, which showed that VMHC in heart transplant patients is significantly correlated with cognitive function. The resting-state brain activity in the occipital lobe is involved in the entire cognitive process beyond visuospatial structures. Conversely, we also found elevated ReHo in the Temporal_Sup_L in heart transplant patients. The superior temporal gyrus, which is part of the temporal lobe, contains the hippocampus and parahippocampal gyrus, which are associated with memory. The superior temporal gyrus also contains areas 41 and 42 and the transverse temporal gyrus, which form the auditory cortical area and are thought to be involved in cognitive processes and language function. Elevated ReHo in the superior temporal gyrus may reflect compensatory neural recruitment to mitigate language-related cognitive decline [27].
VMHC is a validated rs-fMRI evaluation method for quantifying the functional connectivity between the two cerebral hemispheres and is one of the most prominent features of the brain’s basic functional architecture. In pathological states, altered communication between the two cerebral hemispheres can significantly impact cognition and behavior [28]. In this study, VMHC was elevated in the bilateral Cerebellum_Crus1 and decreased in the bilateral calcarine in the heart transplant group. Decreased VMHC in the bilateral calcarine, a primary visual cortex, may indicate disrupted visual information processing, potentially explaining visuospatial deficits in patients. An increasing number of studies recognize that the cerebellum is not only involved in maintaining body balance, motor coordination, and eye movements [29] but also plays a significant role in sensory, cognitive, and emotional learning and regulation [30]. Elevated VMHC in the Cerebellum_Crus1 might indicate maladaptive plasticity in chronic cognitive impairment. Many studies have used fMRI to map motor and non-motor task processes and resting-state networks in the human cerebellar cortex [31]. Pagen et al. found that the functional connectivity of the cerebellum to the brain’s default mode network (DMN) was generally reduced in patients with amnestic mild cognitive impairment (MCI) [32]. The DMN is primarily responsible for the body’s cognitive control in the resting state and maintains inward thinking activity. In patients with Alzheimer’s disease, the DMN is initially disrupted by amyloid deposition caused by the disease process [33]. Both the cerebellum and the prefrontal lobe belong to the DMN. The reduced ReHo in the prefrontal lobe and elevated VMHC in the cerebellum in this study suggest that the DMN is damaged in heart transplant patients.
These alterations in ReHo and VMHC may stem from multiple pathological processes post-heart transplantation. Neuroinflammation and oxidative stress, common in post-transplant patients [19], could damage synaptic plasticity and neuronal synchronization, leading to reduced ReHo in frontal and thalamic regions. Additionally, chronic hypoperfusion due to cardiovascular instability may impair interhemispheric connectivity (VMHC), particularly in the occipital cortex. The cerebellum’s elevated VMHC might be driven by its role in compensating for cortical dysfunction through cerebellar–cortical loops [31], but prolonged overactivation could deplete neural resources, worsening cognitive fatigue.
In this study, there were significant correlations between the ReHo of Frontal_Sup_R, the ReHo of Temporal_Sup_L, and the VMHC of calcarine and the MMSE and MoCA scores in the heart transplantation group. We speculate that the pathogenesis of cognitive dysfunction in heart transplant patients may be related to these brain regions. Changes in the functional connectivity of these brain regions may be predictive of cognitive impairment in heart transplant patients. These findings have potential diagnostic and therapeutic implications. The ReHo and VMHC patterns may serve as neuroimaging biomarkers for early detection of cognitive decline in heart transplant patients. In addition, therapeutic strategies targeting specific brain regions are worth exploring such as, for example, the enhancement of thalamocortical connectivity through neuromodulation. Non-invasive techniques such as transcranial magnetic stimulation (TMS) of the prefrontal cortex have shown promise for improving executive function in other populations [34]. Monitoring changes in ReHo and VMHC in specific brain regions may be useful in assessing the effectiveness of interventions aimed at restoring cognitive control networks.
5. Limitations
Despite the importance of our findings, there are some limitations. Firstly, the sample size is relatively small, which may lead to biased results in differential brain regions, and the sample size will be continuously increased in subsequent studies. Secondly, the present study was cross-sectional, and it was not possible to determine the relationship between brain activity and the progression of cognitive impairment in heart transplant patients. Thirdly, most of the patients had received different types of medications before enrollment. These medications may interfere with the normal metabolism of the brain and thus have an effect on brain activity. Importantly, this study is exploratory and data-driven rather than driven by a specific, narrow research hypothesis. As such, the findings should be regarded as exploratory rather than confirmatory. The results highlight potential associations between VMHC, ReHo, and cognitive function in heart transplant patients, but they need to be replicated in larger, more diverse cohorts to validate their clinical relevance.
6. Conclusions
In summary, heart transplant patients exhibit significant cognitive decline and undergo a series of changes in functional brain activity. Using VMHC and ReHo can objectively and comprehensively reflect the changes in functional connectivity and spontaneous activity between the bilateral cerebral hemispheres. The positive correlation between the ReHo of Frontal_Sup_R, the ReHo of Temporal_Sup_L, and the VMHC of calcarine and cognitive function scales in heart transplant patients provides an imaging basis for further elucidating the pathogenesis of cognitive dysfunction in heart transplant patients. However, further research is needed to explore their potential as biomarkers for cognitive dysfunction in this population.
Author Contributions
Conceptualization, Q.Q. and X.Z.; methodology, W.F.; software, J.L. (Jue Lu); validation, X.G. and Q.Q.; resources, Z.L.; data curation, J.L. (Jia Liu); writing—original draft preparation, Q.Q.; writing—review and editing, J.L. (Jia Liu) and J.W.; funding acquisition, J.L. (Jia Liu) and J.W. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (Grant Nos. 82001801 and 82371945) and the Horizontal Cooperation Foundation of China (Grant No. 02.01.23061).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (2022(0166-01)).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| VMHC | voxel-mirrored homotopic connectivity. |
| ReHo | regional homogeneity |
| MMSE | Mini-Mental State Examination |
| MoCA | Montreal Cognitive Assessment |
| POCD | postoperative cognitive dysfunction |
| rs-fMRI | resting-state functional MRI |
| DMN | default mode network |
| KCC | Kendall’s concordance coefficient |
| MCI | mild cognitive impairment |
References
- Khush, K.K.; Hsich, E.; Potena, L.; Cherikh, W.S.; Chambers, D.C.; Harhay, M.O.; Hayes, D., Jr.; Perch, M.; Sadavarte, A.; Toll, A.; et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-eighth adult heart transplantation report—2021; Focus on recipient characteristics. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2021, 40, 1035–1049. [Google Scholar] [CrossRef] [PubMed]
- Velleca, A.; Shullo, M.A.; Dhital, K.; Azeka, E.; Colvin, M.; DePasquale, E.; Farrero, M.; García-Guereta, L.; Jamero, G.; Khush, K.; et al. The International Society for Heart and Lung Transplantation (ISHLT) guidelines for the care of heart transplant recipients. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2023, 42, e1–e141. [Google Scholar] [CrossRef]
- van Dijk, D.; Keizer, A.M.; Diephuis, J.C.; Durand, C.; Vos, L.J.; Hijman, R. Neurocognitive dysfunction after coronary artery bypass surgery: A systematic review. J. Thorac. Cardiovasc. Surg. 2000, 120, 632–639. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Lindsay, J.; Monsein, L.H.; Hill, P.C.; Corso, P.J. Silent brain injury after cardiac surgery: A review: Cognitive dysfunction and magnetic resonance imaging diffusion-weighted imaging findings. J. Am. Coll. Cardiol. 2012, 60, 791–797. [Google Scholar] [CrossRef] [PubMed]
- Guenther, U.; Hoffmann, F.; Dewald, O.; Malek, R.; Brimmers, K.; Theuerkauf, N.; Putensen, C.; Popp, J. Preoperative Cognitive Impairment and Postoperative Delirium Predict Decline in Activities of Daily Living after Cardiac Surgery-A Prospective, Observational Cohort Study. Geriatrics 2020, 5, 69. [Google Scholar] [CrossRef]
- Olotu, C. Postoperative neurocognitive disorders. Curr. Opin. Anaesthesiol. 2020, 33, 101–108. [Google Scholar] [CrossRef]
- Roman, D.D.; Holker, E.G.; Missov, E.; Colvin, M.M.; Menk, J. Neuropsychological functioning in heart transplant candidates. Clin. Neuropsychol. 2017, 31, 118–137. [Google Scholar] [CrossRef] [PubMed]
- Yan, W.; Palaniyappan, L.; Liddle, P.F.; Rangaprakash, D.; Wei, W.; Deshpande, G. Characterization of Hemodynamic Alterations in Schizophrenia and Bipolar Disorder and Their Effect on Resting-State fMRI Functional Connectivity. Schizophr. Bull. 2022, 48, 695–711. [Google Scholar] [CrossRef]
- Smallwood, J.; Bernhardt, B.C.; Leech, R.; Bzdok, D.; Jefferies, E.; Margulies, D.S. The default mode network in cognition: A topographical perspective. Nat. Rev. Neurosci. 2021, 22, 503–513. [Google Scholar] [CrossRef]
- Menon, V. 20 years of the default mode network: A review and synthesis. Neuron 2023, 111, 2469–2487. [Google Scholar] [CrossRef]
- Zuo, X.N.; Kelly, C.; Di Martino, A.; Mennes, M.; Margulies, D.S.; Bangaru, S.; Grzadzinski, R.; Evans, A.C.; Zang, Y.F.; Castellanos, F.X.; et al. Growing together and growing apart: Regional and sex differences in the lifespan developmental trajectories of functional homotopy. J. Neurosci. Off. J. Soc. Neurosci. 2010, 30, 15034–15043. [Google Scholar] [CrossRef] [PubMed]
- Zang, Y.; Jiang, T.; Lu, Y.; He, Y.; Tian, L. Regional homogeneity approach to fMRI data analysis. NeuroImage 2004, 22, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Honda, T.; Narazaki, K.; Chen, T.; Nofuji, Y.; Kumagai, S. Global cognitive performance and frailty in non-demented community-dwelling older adults: Findings from the Sasaguri Genkimon Study. Geriatr. Gerontol. Int. 2016, 16, 729–736. [Google Scholar] [CrossRef]
- Jia, X.; Wang, Z.; Huang, F.; Su, C.; Du, W.; Jiang, H.; Wang, H.; Wang, J.; Wang, F.; Su, W.; et al. A comparison of the Mini-Mental State Examination (MMSE) with the Montreal Cognitive Assessment (MoCA) for mild cognitive impairment screening in Chinese middle-aged and older population: A cross-sectional study. BMC Psychiatry 2021, 21, 485. [Google Scholar] [CrossRef]
- Yan, C.G.; Wang, X.D.; Zuo, X.N.; Zang, Y.F. DPABI: Data Processing & Analysis for (Resting-State) Brain Imaging. Neuroinformatics 2016, 14, 339–351. [Google Scholar] [CrossRef] [PubMed]
- Bürker, B.S.; Gude, E.; Gullestad, L.; Grov, I.; Relbo Authen, A.; Andreassen, A.K.; Havik, O.E.; Dew, M.A.; Fiane, A.E.; Haraldsen, I.R.; et al. Cognitive function among long-term survivors of heart transplantation. Clin. Transplant. 2017, 31, e13143. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Yang, W.; Xue, J.; Chen, J.; Liu, S.; Zhang, S.; Zhang, X.; Gu, X.; Dong, Y.; Qiu, P. Neuroinflammation: The central enabler of postoperative cognitive dysfunction. Biomed. Pharmacother. Biomed. Pharmacother. 2023, 167, 115582. [Google Scholar] [CrossRef]
- Leslie, M. The post-op brain. Science 2017, 356, 898–900. [Google Scholar] [CrossRef]
- Luo, A.; Yan, J.; Tang, X.; Zhao, Y.; Zhou, B.; Li, S. Postoperative cognitive dysfunction in the aged: The collision of neuroinflammaging with perioperative neuroinflammation. Inflammopharmacology 2019, 27, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Song, Y.; Yang, X.; Chen, S.; Ge, H.; Yan, Z.; Qi, W.; Yuan, Q.; Liang, X.; Lin, X.; et al. Functional and structural alterations of dorsal attention network in preclinical and early-stage Alzheimer’s disease. CNS Neurosci. Ther. 2023, 29, 1512–1524. [Google Scholar] [CrossRef]
- Zhang, Z.; Liu, Y.; Jiang, T.; Zhou, B.; An, N.; Dai, H.; Wang, P.; Niu, Y.; Wang, L.; Zhang, X. Altered spontaneous activity in Alzheimer’s disease and mild cognitive impairment revealed by Regional Homogeneity. NeuroImage 2012, 59, 1429–1440. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Jiang, H.; Wang, D.; Zhao, X.F. A study of regional homogeneity of resting-state Functional Magnetic Resonance Imaging in mild cognitive impairment. Behav. Brain Res. 2021, 402, 113103. [Google Scholar] [CrossRef] [PubMed]
- Alagapan, S.; Lustenberger, C.; Hadar, E.; Shin, H.W.; Fröhlich, F. Low-frequency direct cortical stimulation of left superior frontal gyrus enhances working memory performance. NeuroImage 2019, 184, 697–706. [Google Scholar] [CrossRef]
- Qiu, E.; Xing, X.; Wang, Y.; Tian, L. Altered functional connectivity of the thalamus and salience network in patients with cluster headache: A pilot study. Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol. 2024, 45, 269–276. [Google Scholar] [CrossRef]
- Hwang, K.; Bruss, J.; Tranel, D.; Boes, A.D. Network Localization of Executive Function Deficits in Patients with Focal Thalamic Lesions. J. Cogn. Neurosci. 2020, 32, 2303–2319. [Google Scholar] [CrossRef]
- He, X.; Zhang, Y.; Chen, J.; Xie, C.; Gan, R.; Wang, L.; Wang, L. Changes in theta activities in the left posterior temporal region, left occipital region and right frontal region related to mild cognitive impairment in Parkinson’s disease patients. Int. J. Neurosci. 2017, 127, 66–72. [Google Scholar] [CrossRef]
- Li, M.; Zheng, G.; Zheng, Y.; Xiong, Z.; Xia, R.; Zhou, W.; Wang, Q.; Liang, S.; Tao, J.; Chen, L. Alterations in resting-state functional connectivity of the default mode network in amnestic mild cognitive impairment: An fMRI study. BMC Med. Imaging 2017, 17, 48. [Google Scholar] [CrossRef]
- Tan, S.W.; Cai, G.Q.; Li, Q.Y.; Guo, Y.; Pan, Y.C.; Zhang, L.J.; Ge, Q.M.; Shu, H.Y.; Zeng, X.J.; Shao, Y. Interhemispheric Functional Connectivity Alterations in Diabetic Optic Neuropathy: A Resting-State Functional Magnetic Resonance Imaging Study. Diabetes Metab. Syndr. Obes. Targets Ther. 2021, 14, 2077–2086. [Google Scholar] [CrossRef]
- Hewitt, A.L.; Popa, L.S.; Ebner, T.J. Changes in Purkinje cell simple spike encoding of reach kinematics during adaption to a mechanical perturbation. J. Neurosci. Off. J. Soc. Neurosci. 2015, 35, 1106–1124. [Google Scholar] [CrossRef][Green Version]
- Cheron, G.; Servais, L.; Dan, B. Cerebellar network plasticity: From genes to fast oscillation. Neuroscience 2008, 153, 1–19. [Google Scholar] [CrossRef]
- Guell, X.; Schmahmann, J. Cerebellar Functional Anatomy: A Didactic Summary Based on Human fMRI Evidence. Cerebellum 2020, 19, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Pagen, L.H.G.; van de Ven, V.G.; Gronenschild, E.; Priovoulos, N.; Verhey, F.R.J.; Jacobs, H.I.L. Contributions of Cerebro-Cerebellar Default Mode Connectivity Patterns to Memory Performance in Mild Cognitive Impairment. J. Alzheimer’s Dis. 2020, 75, 633–647. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Sporns, O.; Saykin, A.J. The human connectome in Alzheimer disease—Relationship to biomarkers and genetics. Nat. Rev. Neurol. 2021, 17, 545–563. [Google Scholar] [CrossRef]
- Brunoni, A.R.; Moffa, A.H.; Fregni, F.; Palm, U.; Padberg, F.; Blumberger, D.M.; Daskalakis, Z.J.; Bennabi, D.; Haffen, E.; Alonzo, A.; et al. Transcranial direct current stimulation for acute major depressive episodes: Meta-analysis of individual patient data. Br. J. Psychiatry J. Ment. Sci. 2016, 208, 522–531. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).