The Impact of Artificial Intelligence in the Odyssey of Rare Diseases
Abstract
1. Introduction
- only small cohorts of patients are interested in purchasing these drugs, making them so-called orphan drugs because they are not competitive for pharmaceutical companies.
- difficulties in treatment because most rare diseases are caused by genetic errors and/or have a degenerative nature.
- significant percentages of patients do not respond to available therapies due to partial or complete loss of response.
2. Artificial Intelligence
- Classification: two or more classes are created with the input data, and the learning system aims to produce a model capable of assigning a class to each input.
- Regression: conceptually similar to classification, with the difference that the output is continuous.
- Clustering: data are divided into groups about which there is no prior knowledge.
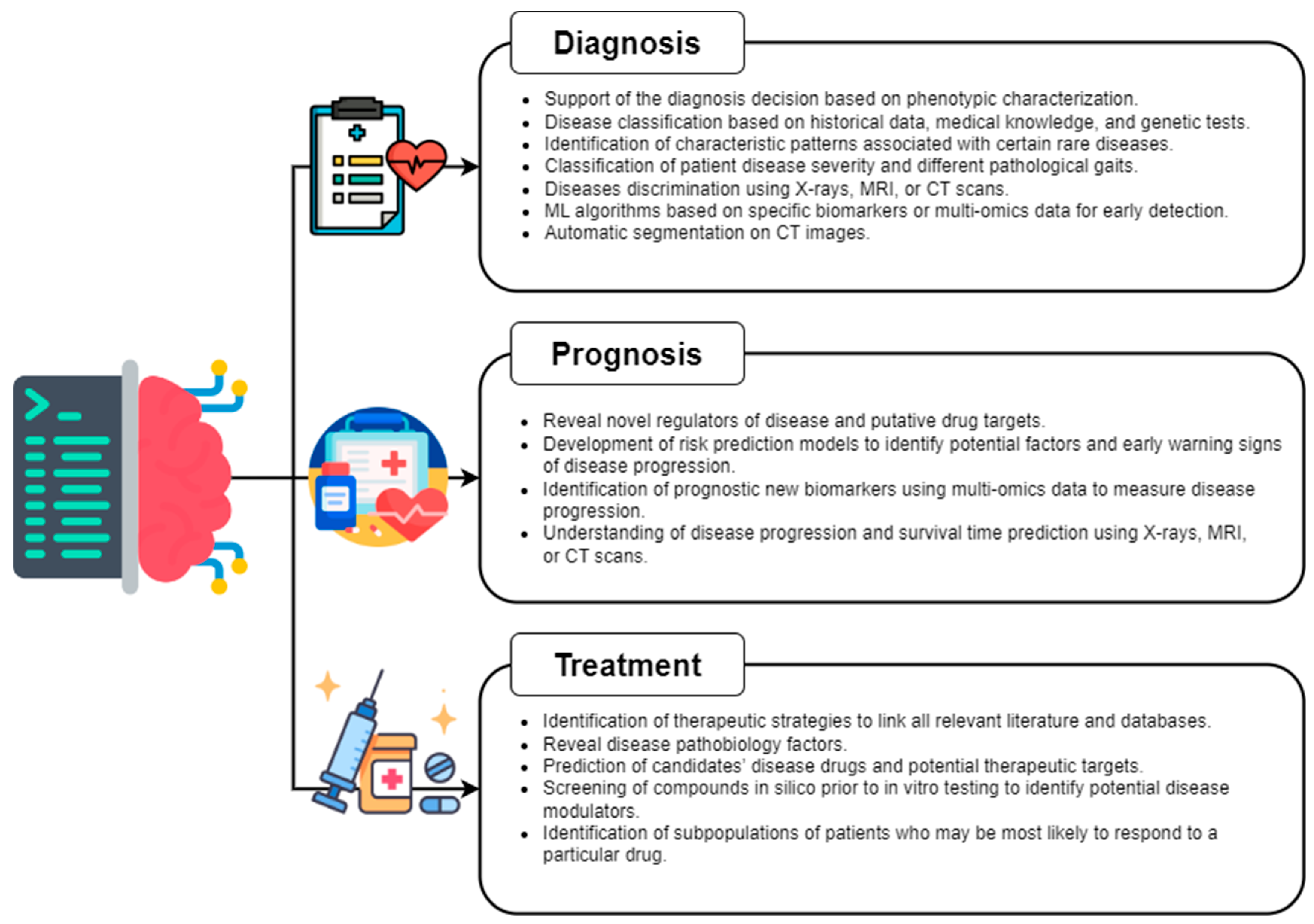
3. AI Application in Rare Diseases
3.1. Diagnosis
3.2. Prognosis
3.3. Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vickers, P.J. Challenges and Opportunities in The Treatment of Rare Diseases. Drug Discov. World 2013, 14, 9–16. [Google Scholar]
- Hughes, D.; Tunnage, B.; Yeo, S. Drugs for exceptionally rare diseases: Do they deserve special status for funding? QJM Int. J. Med. 2005, 98, 829–836. [Google Scholar] [CrossRef] [PubMed]
- Nguengang Wakap, S.; Lambert, D.M.; Olry, A.; Rodwell, C.; Gueydan, C.; Lanneau, V.; Murphy, D.; Le Cam, Y.; Rath, A. Estimating cumulative point prevalence of rare diseases: Analysis of the Orphanet database. Eur. J. Hum. Genet. 2020, 28, 165–173. [Google Scholar] [CrossRef] [PubMed]
- European Union. Regulation (EC) N°141/2000 of the European Parliament and of the Council of 16 December 1999 on Orphan Medicinal Products. 2000. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32000R0141 (accessed on 18 November 2022).
- National Institute of Health. Public Law 97–414 97th Congress. 1983. Available online: https://www.govinfo.gov/content/pkg/STATUTE-96/pdf/STATUTE-96-Pg2049.pdf (accessed on 14 December 2022).
- Richter, T.; Nestler-Parr, S.; Babela, R.; Khan, Z.M.; Tesoro, T.; Molsen, E.; Hughes, D.A. Rare Disease Terminology and Definitions—A Systematic Global Review: Report of the ISPOR Rare Disease Special Interest Group. Value Health 2015, 18, 906–914. [Google Scholar] [CrossRef] [PubMed]
- Stoller, J.K. The Challenge of Rare Diseases. Chest 2018, 153, 1309–1314. [Google Scholar] [CrossRef]
- Navarrete-Opazo, A.A.; Singh, M.; Tisdale, A.; Cutillo, C.M.; Garrison, S.R. Can you hear us now? The impact of health-care utilization by rare disease patients in the United States. Anesth. Analg. 2021, 23, 2194–2201. [Google Scholar] [CrossRef]
- Willmen, T.; Völkel, L.; Ronicke, S.; Hirsch, M.C.; Kaufeld, J.; Rychlik, R.P.; Wagner, A.D. Health economic benefits through the use of diagnostic support systems and expert knowledge. BMC Health Serv. Res. 2021, 21, 947. [Google Scholar] [CrossRef]
- NORD. Barriers to Rare Disease Diagnosis, Care and Treatment in the US: A 30-Year Comparative Analysis. 2020. Available online: https://rarediseases.org/wp-content/uploads/2020/11/NRD-2088-Barriers-30-Yr-Survey-Report_FNL-2.pdf (accessed on 18 November 2022).
- Mueller, T.; Jerrentrup, A.; Bauer, M.J.; Fritsch, H.W.; Schaefer, J.R. Characteristics of patients contacting a center for undiagnosed and rare diseases. Orphanet J. Rare Dis. 2016, 11, 81. [Google Scholar] [CrossRef]
- Tambuyzer, E.; Vandendriessche, B.; Austin, C.P.; Brooks, P.J.; Larsson, K.; Needleman, K.I.M.; Valentine, J.; Davies, K.; Groft, S.C.; Preti, R.; et al. Therapies for rare diseases: Therapeutic modalities, progress and challenges ahead. Nat. Rev. Drug Discov. 2019, 19, 93–111. [Google Scholar] [CrossRef]
- Hurvitz, N.; Azmanov, H.; Kesler, A.; Ilan, Y. Establishing a second-generation artificial intelligence-based system for improving diagnosis, treatment, and monitoring of patients with rare diseases. Eur. J. Hum. Genet. 2021, 29, 1485–1490. [Google Scholar] [CrossRef]
- Valdez, R.; Ouyang, L.; Bolen, J. Public Health and Rare Diseases: Oxymoron No More. Prev. Chronic Dis. 2016, 13, E05. [Google Scholar] [CrossRef] [PubMed]
- Alves, V.M.; Korn, D.; Pervitsky, V.; Thieme, A.; Capuzzi, S.J.; Baker, N.; Chirkova, R.; Ekins, S.; Muratov, E.N.; Hickey, A.; et al. Knowledge-based approaches to drug discovery for rare diseases. Drug Discov. Today 2021, 27, 490–502. [Google Scholar] [CrossRef] [PubMed]
- Baxter, K.; Horn, E.; Gal-Edd, N.; Zonno, K.; O’Leary, J.; Terry, P.F.; Terry, S.F. An End to the Myth: There Is No Drug Development Pipeline. Sci. Transl. Med. 2013, 5, 171cm1. [Google Scholar] [CrossRef] [PubMed]
- Kakkis, E.D.; O’Donovan, M.; Cox, G.; Hayes, M.; Goodsaid, F.; Tandon, P.K.; Furlong, P.; Boynton, S.; Bozic, M.; Orfali, M.; et al. Recommendations for the development of rare disease drugs using the accelerated approval pathway and for qualifying biomarkers as primary endpoints. Orphanet J. Rare Dis. 2015, 10, 16. [Google Scholar] [CrossRef]
- Pradhan, A.; Prabhu, S.; Chadaga, K.; Sengupta, S.; Nath, G. Supervised Learning Models for the Preliminary Detection of COVID-19 in Patients Using Demographic and Epidemiological Parameters. Information 2022, 13, 330. [Google Scholar] [CrossRef]
- Khanna, V.V.; Chadaga, K.; Sampathila, N.; Prabhu, S.; Chadaga, R.; Umakanth, S. Diagnosing COVID-19 using artificial intelligence: A comprehensive review. Netw. Model. Anal. Health Inform. Bioinform. 2022, 11, 25. [Google Scholar] [CrossRef]
- COVID-19 Mortality Prediction using Machine Learning: A Deep Forest Approach. In Proceedings of the 2022 International Conference on Distributed Computing, VLSI, Electrical Circuits and Robotics (DISCOVER), Shivamogga, India, 14–15 October 2022; pp. 245–250. [CrossRef]
- Ilan, Y. Second-Generation Digital Health Platforms: Placing the Patient at the Center and Focusing on Clinical Outcomes. Front. Digit. Health 2020, 2, 569178. [Google Scholar] [CrossRef]
- Sim, I.; Gorman, P.; Greenes, R.A.; Haynes, R.B.; Kaplan, B.; Lehmann, H.; Tang, P.C. Clinical Decision Support Systems for the Practice of Evidence-based Medicine. J. Am. Med. Inform. Assoc. 2001, 8, 527–534. [Google Scholar] [CrossRef]
- Porat, T.; Delaney, B.; Kostopoulou, O. The impact of a diagnostic decision support system on the consultation: Perceptions of GPs and patients. BMC Med. Inform. Decis. Mak. 2017, 17, 79. [Google Scholar] [CrossRef]
- Winther, O.; Svenstrup, D.; Henningsen, P.P.; Kristiásson, R.; Jørgensen, H.L. FindZebra-the search engine for difficult medical cases. Orphanet J. Rare Dis. 2014, 9, O5. [Google Scholar] [CrossRef]
- Girdea, M.; Dumitriu, S.; Fiume, M.; Bowdin, S.; Boycott, K.M.; Chénier, S.; Chitayat, D.; Faghfoury, H.; Meyn, M.S.; Ray, P.N.; et al. PhenoTips: Patient Phenotyping Software for Clinical and Research Use. Hum. Mutat. 2013, 34, 1057–1065. [Google Scholar] [CrossRef] [PubMed]
- Alves, R.; Piñol, M.; Vilaplana, J.; Teixidó, I.; Cruz, J.; Comas, J.; Vilaprinyo, E.; Sorribas, A.; Solsona, F. Computer-assisted initial diagnosis of rare diseases. PeerJ 2016, 4, e2211. [Google Scholar] [CrossRef]
- Ronicke, S.; Hirsch, M.C.; Türk, E.; Larionov, K.; Tientcheu, D.; Wagner, A.D. Can a decision support system accelerate rare disease diagnosis? Evaluating the potential impact of Ada DX in a retrospective study. Orphanet J. Rare Dis. 2019, 14, 69. [Google Scholar] [CrossRef]
- Lanar, S.; Acquadro, C.; Seaton, J.; Savre, I.; Arnould, B. To what degree are orphan drugs patient-centered? A review of the current state of clinical research in rare diseases. Orphanet J. Rare Dis. 2020, 15, 134. [Google Scholar] [CrossRef]
- Lee, J.; Liu, C.; Kim, J.; Chen, Z.; Sun, Y.; Rogers, J.R.; Chung, W.K.; Weng, C. Deep learning for rare disease: A scoping review. J. Biomed. Inform. 2022, 135, 104227. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, J.; Lehne, M.; Schepers, J.; Prasser, F.; Thun, S. The use of machine learning in rare diseases: A scoping review. Orphanet J. Rare Dis. 2020, 15, 145. [Google Scholar] [CrossRef] [PubMed]
- Mcculloch, W.S.; Pitts, W.H. A logical calculus of the ideas immanent in nervous activity. Bull. Math. Biophys. 1943, 5, 115–133. [Google Scholar] [CrossRef]
- Cunningham, P.; Cord, M.; Delany, S.J. Supervised Learning. In Machine Learning Techniques for Multimedia: Cognitive Technologies; Springer: Berlin/Heidelberg, Germany, 2008; pp. 21–49. [Google Scholar]
- Ghahramani, Z. Unsupervised learning. In Summer School on Machine Learning; Springer: Berlin/Heidelberg, Germany, 2004; pp. 72–112. [Google Scholar]
- Zhu, X.J. Semi-Supervised Learning Literature Survey. 2005. Available online: https://pages.cs.wisc.edu/~jerryzhu/pub/ssl_survey.pdf (accessed on 18 November 2022).
- Russel, S.; Norvig, P. Artificial Intelligence: A Modern Approach; Pearson Education Limited, Prentice Hall Press: Upper Saddle River, NJ, USA, 2016. [Google Scholar]
- Alzubi, J.; Nayyar, A.; Kumar, A. Machine Learning from Theory to Algorithms: An Overview. J. Phys. Conf. Ser. 2018, 1142, 012012. [Google Scholar] [CrossRef]
- HamediRad, M.; Chao, R.; Weisberg, S.; Lian, J.; Sinha, S.; Zhao, H. Towards a fully automated algorithm driven platform for biosystems design. Nat. Commun. 2019, 10, 5150. [Google Scholar] [CrossRef]
- Shen, F.; Liu, S.; Wang, Y.; Wang, L.; Afzal, N.; Liu, H. Leveraging Collaborative Filtering to Accelerate Rare Disease Diagnosis. AMIA Annu. Symp. Proc. 2018, 2017, 1554–1563. [Google Scholar]
- Jia, J.; Wang, R.; An, Z.; Guo, Y.; Ni, X.; Shi, T. RDAD: A Machine Learning System to Support Phenotype-Based Rare Disease Diagnosis. Front. Genet. 2018, 9, 587. [Google Scholar] [CrossRef]
- Rother, A.K.; Schwerk, N.; Brinkmann, F.; Klawonn, F.; Lechner, W.; Grigull, L. Diagnostic Support for Selected Paediatric Pulmonary Diseases Using Answer-Pattern Recognition in Questionnaires Based on Combined Data Mining Applications—A Monocentric Observational Pilot Study. PLoS ONE 2015, 10, e0135180. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, Y.; Wang, D.; Yuan, W.; Peng, D.; Mei, Q. Improving rare disease classification using imperfect knowledge graph. BMC Med. Inform. Decis. Mak. 2019, 19, 238. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Poon, S.K.; Vuong, K.; Sneddon, A.; Loy, C.T. A Deep Learning-Based Approach for Gait Analysis in Huntington Disease. Stud. Health Technol. Inform. 2019, 264, 477–481. [Google Scholar] [CrossRef]
- Mannini, A.; Trojaniello, D.; Cereatti, A.; Sabatini, A.M. A Machine Learning Framework for Gait Classification Using Inertial Sensors: Application to Elderly, Post-Stroke and Huntington’s Disease Patients. Sensors 2016, 16, 134. [Google Scholar] [CrossRef] [PubMed]
- Miranda, Â.; Lavrador, R.; Júlio, F.; Januário, C.; Castelo-Branco, M.; Caetano, G. Classification of Huntington’s disease stage with support vector machines: A study on oculomotor performance. Behav. Res. Methods 2015, 48, 1667–1677. [Google Scholar] [CrossRef] [PubMed]
- Odish, O.F.F.; Johnsen, K.; van Someren, P.; Roos, R.A.C.; van Dijk, J.G. EEG may serve as a biomarker in Huntington’s disease using machine learning automatic classification. Sci. Rep. 2018, 8, 16090. [Google Scholar] [CrossRef] [PubMed]
- Baggio, H.C.; Abos, A.; Segura, B.; Campabadal, A.; Uribe, C.; Giraldo, D.M.; Perez-Soriano, A.; Muñoz, E.; Compta, Y.; Junque, C.; et al. Cerebellar resting-state functional connectivity in Parkinson's disease and multiple system atrophy: Characterization of abnormalities and potential for differential diagnosis at the single-patient level. NeuroImage Clin. 2019, 22, 101720. [Google Scholar] [CrossRef]
- Abos, A.; Baggio, H.C.; Segura, B.; Campabadal, A.; Uribe, C.; Giraldo, D.M.; Perez-Soriano, A.; Muñoz, E.; Compta, Y.; Junque, C.; et al. Differentiation of multiple system atrophy from Parkinson’s disease by structural connectivity derived from probabilistic tractography. Sci. Rep. 2019, 9, 16488. [Google Scholar] [CrossRef]
- Kiryu, S.; Yasaka, K.; Akai, H.; Nakata, Y.; Sugomori, Y.; Hara, S.; Seo, M.; Abe, O.; Ohtomo, K. Deep learning to differentiate parkinsonian disorders separately using single midsagittal MR imaging: A proof of concept study. Eur. Radiol. 2019, 29, 6891–6899. [Google Scholar] [CrossRef]
- Yin, B.; Balvert, M.; van der Spek, R.A.A.; Dutilh, B.E.; Bohté, S.; Veldink, J.; Schönhuth, A. Using the structure of genome data in the design of deep neural networks for predicting amyotrophic lateral sclerosis from genotype. Bioinformatics 2019, 35, i538–i547. [Google Scholar] [CrossRef] [PubMed]
- Sarica, A.; Cerasa, A.; Valentino, P.; Yeatman, J.; Trotta, M.; Barone, S.; Granata, A.; Nisticò, R.; Perrotta, P.; Pucci, F.; et al. The corticospinal tract profile in amyotrophic lateral sclerosis. Hum. Brain Mapp. 2016, 38, 727–739. [Google Scholar] [CrossRef] [PubMed]
- Welsh, R.C.; Jelsone-Swain, L.M.; Foerster, B.R. The Utility of Independent Component Analysis and Machine Learning in the Identification of the Amyotrophic Lateral Sclerosis Diseased Brain. Front. Hum. Neurosci. 2013, 7, 251. [Google Scholar] [CrossRef] [PubMed]
- Palstrøm, N.B.; Rojek, A.M.; Møller, H.E.H.; Hansen, C.T.; Matthiesen, R.; Rasmussen, L.M.; Abildgaard, N.; Beck, H.C. Classification of Amyloidosis by Model-Assisted Mass Spectrometry-Based Proteomics. Int. J. Mol. Sci. 2021, 23, 319. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Carretero, R.; Olid-Velilla, M.; Perez-Torrella, D.; Torres-Pacho, N.; Darnaude-Ortiz, M.T.; Bustamate-Zuloeta, A.D.; Tenorio, J.A. Predictive modeling of hypophosphatasia based on a case series of adult patients with persistent hypophosphatasemia. Osteoporos. Int. 2021, 32, 1815–1824. [Google Scholar] [CrossRef]
- Nguyen, K.D.; Corben, L.A.; Pathirana, P.N.; Horne, M.K.; Delatycki, M.B.; Szmulewicz, D.J. An Instrumented Measurement Scheme for the Assessment of Upper Limb Function in Individuals with Friedreich Ataxia. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019. [Google Scholar] [CrossRef]
- Salvatore, C.; Cerasa, A.; Castiglioni, I.; Gallivanone, F.; Augimeri, A.; Lopez, M.; Arabia, G.; Morelli, M.; Gilardi, M.C.; Quattrone, A. Machine learning on brain MRI data for differential diagnosis of Parkinson's disease and Progressive Supranuclear Palsy. J. Neurosci. Methods 2014, 222, 230–237. [Google Scholar] [CrossRef]
- Abidin, A.Z.; Jameson, J.; Molthen, R.; Wismüller, A. Classification of micro-CT images using 3D characterization of bone canal patterns in human osteogenesis imperfecta. Proc. SPIE Int. Soc. Opt. Eng. 2017, 10134, 1013413. [Google Scholar] [CrossRef]
- Karthikeyan, S.; Ramkumar, G.; Aravindkumar, S.; Tamilselvi, M.; Ramesh, S.; Ranjith, A. A Novel Deep Learning-Based Black Fungus Disease Identification Using Modified Hybrid Learning Methodology. Contrast Media Mol. Imaging 2022, 2022, 4352730. [Google Scholar] [CrossRef]
- Masumoto, H.; Tabuchi, H.; Nakakura, S.; Ohsugi, H.; Enno, H.; Ishitobi, N.; Ohsugi, E.; Mitamura, Y. Accuracy of a deep convolutional neural network in detection of retinitis pigmentosa on ultrawide-field images. PeerJ 2019, 7, e6900. [Google Scholar] [CrossRef]
- Wang, T.; Lei, Y.; Tian, S.; Jiang, X.; Zhou, J.; Liu, T.; Dresser, S.; Curran, W.J.; Shu, H.; Yang, X. Learning-based automatic segmentation of arteriovenous malformations on contrast CT images in brain stereotactic radiosurgery. Med. Phys. 2019, 46, 3133–3141. [Google Scholar] [CrossRef]
- Kovacs, W.; Hsieh, N.; Roth, H.; Nnamdi-Emeratom, C.; Bandettini, W.P.; Arai, A.; Mankodi, A.; Summers, R.M.; Yao, J. Holistic segmentation of the lung in cine MRI. J. Med. Imaging 2017, 4, 041310. [Google Scholar] [CrossRef]
- Zhang, H.-W.; Zhou, P.; Wang, K.-Z.; Liu, J.-B.; Huang, Y.-S.; Tu, Y.-T.; Deng, Z.-H.; Zhu, X.-D.; Hang, Y.-L. Platelet proteomics in diagnostic differentiation of primary immune thrombocytopenia using SELDI-TOF-MS. Clin. Chim. Acta 2016, 455, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Mordenti, M.; Ferrari, E.; Pedrini, E.; Fabbri, N.; Campanacci, L.; Muselli, M.; Sangiorgi, L. Validation of a new multiple osteochondromas classification through Switching Neural Networks. Am. J. Med. Genet. Part A 2013, 161, 556–560. [Google Scholar] [CrossRef] [PubMed]
- Artoni, P.; Piffer, A.; Vinci, V.; LeBlanc, J.; Nelson, C.A.; Hensch, T.K.; Fagiolini, M. Deep learning of spontaneous arousal fluctuations detects early cholinergic defects across neurodevelopmental mouse models and patients. Proc. Natl. Acad. Sci. USA 2019, 117, 23298–23303. [Google Scholar] [CrossRef] [PubMed]
- Errington, N.; Iremonger, J.; Pickworth, J.A.; Kariotis, S.; Rhodes, C.J.; Rothman, A.M.; Condliffe, R.; Elliot, C.A.; Kiely, D.G.; Howard, L.S.; et al. A diagnostic miRNA signature for pulmonary arterial hypertension using a consensus machine learning approach. Ebiomedicine 2021, 69, 103444. [Google Scholar] [CrossRef] [PubMed]
- Iwasawa, K.; Suda, W.; Tsunoda, T.; Oikawa-Kawamoto, M.; Umetsu, S.; Takayasu, L.; Inui, A.; Fujisawa, T.; Morita, H.; Sogo, T.; et al. Dysbiosis of the salivary microbiota in pediatric-onset primary sclerosing cholangitis and its potential as a biomarker. Sci. Rep. 2018, 8, 5480. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Camino, A.; Hagag, A.M.; Wang, J.; Weleber, R.G.; Yang, P.; Pennesi, M.E.; Huang, D.; Li, D.; Jia, Y. Automated detection of preserved photoreceptor on optical coherence tomography in choroideremia based on machine learning. J. Biophotonics 2018, 11, e201700313. [Google Scholar] [CrossRef]
- Nodera, H.; Sogawa, K.; Takamatsu, N.; Hashiguchi, S.; Saito, M.; Mori, A.; Osaki, Y.; Izumi, Y.; Kaji, R. Texture analysis of sonographic muscle images can distinguish myopathic conditions. J. Med. Investig. 2019, 66, 237–247. [Google Scholar] [CrossRef]
- Shire. Rare Disease Impact Report: Insights from Patients and the Medical Community. 2013. Available online: https://globalgenes.org/wp-content/uploads/2013/04/ShireReport-1.pdf (accessed on 18 November 2022).
- Bohr, A.; Memarzadeh, K. The rise of artificial intelligence in healthcare applications. In Artificial Intelligence in Healthcare; Elsevier: Amsterdam, The Netherlands, 2020; pp. 25–60. [Google Scholar] [CrossRef]
- Bates, D.W.; Saria, S.; Ohno-Machado, L.; Shah, A.; Escobar, G. Big Data in Health Care: Using Analytics to Identify And Manage High-Risk and High-Cost Patients. Health Aff. 2014, 33, 1123–1131. [Google Scholar] [CrossRef]
- Rajkomar, A.; Dean, J.; Kohane, I. Machine Learning in Medicine. N. Engl. J. Med. 2019, 380, 1347–1358. [Google Scholar] [CrossRef]
- Marquardt, A.; Landwehr, L.-S.; Ronchi, C.L.; di Dalmazi, G.; Riester, A.; Kollmannsberger, P.; Altieri, B.; Fassnacht, M.; Sbiera, S. Identifying New Potential Biomarkers in Adrenocortical Tumors Based on mRNA Expression Data Using Machine Learning. Cancers 2021, 13, 4671. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.; Moon, S.; Jung, K.; Kim, S.; Kim, H.; Han, D.; Kim, J. Mass Spectrometry-Based Proteomic Discovery of Prognostic Biomarkers in Adrenal Cortical Carcinoma. Cancers 2021, 13, 3890. [Google Scholar] [CrossRef] [PubMed]
- Spiga, O.; Cicaloni, V.; Bernini, A.; Zatkova, A.; Santucci, A. ApreciseKUre: An approach of Precision Medicine in a Rare Disease. BMC Med. Inform. Decis. Mak. 2017, 17, 42. [Google Scholar] [CrossRef]
- Spiga, O.; Cicaloni, V.; Fiorini, C.; Trezza, A.; Visibelli, A.; Millucci, L.; Bernardini, G.; Bernini, A.; Marzocchi, B.; Braconi, D.; et al. Machine learning application for development of a data-driven predictive model able to investigate quality of life scores in a rare disease. Orphanet J. Rare Dis. 2020, 15, 46. [Google Scholar] [CrossRef]
- Spiga, O.; Cicaloni, V.; Dimitri, G.M.; Pettini, F.; Braconi, D.; Bernini, A.; Santucci, A. Machine learning application for patient stratification and phenotype/genotype investigation in a rare disease. Brief. Bioinform. 2021, 22, bbaa434. [Google Scholar] [CrossRef]
- Blasco, H.; Patin, F.; Descat, A.; Garçon, G.; Corcia, P.; Gelé, P.; Lenglet, T.; Bede, P.; Meininger, V.; Devos, D.; et al. A pharmaco-metabolomics approach in a clinical trial of ALS: Identification of predictive markers of progression. PLoS ONE 2018, 13, e0198116. [Google Scholar] [CrossRef]
- Huang, Z.; Zhang, H.; Boss, J.; Goutman, S.A.; Mukherjee, B.; Dinov, I.D.; Guan, Y. For the Pooled Resource Open-Access ALS Clinical Trials Consortium Complete hazard ranking to analyze right-censored data: An ALS survival study. PLOS Comput. Biol. 2017, 13, e1005887. [Google Scholar] [CrossRef] [PubMed]
- Gordon, J.; Lerner, B. Insights into Amyotrophic Lateral Sclerosis from a Machine Learning Perspective. J. Clin. Med. 2019, 8, 1578. [Google Scholar] [CrossRef]
- Wang, J.; Kothalkar, P.V.; Kim, M.; Bandini, A.; Cao, B.; Yunusova, Y.; Campbell, T.F.; Heitzman, D.; Green, J.R. Automatic prediction of intelligible speaking rate for individuals with ALS from speech acoustic and articulatory samples. Int. J. Speech-Lang. Pathol. 2018, 20, 669–679. [Google Scholar] [CrossRef]
- van der Burgh, H.K.; Schmidt, R.; Westeneng, H.-J.; de Reus, M.A.; Berg, L.H.V.D.; Heuvel, M.P.V.D. Deep learning predictions of survival based on MRI in amyotrophic lateral sclerosis. NeuroImage Clin. 2016, 13, 361–369. [Google Scholar] [CrossRef]
- Lauraitis, A.; Maskeliūnas, R.; Damaševičius, R. ANN and Fuzzy Logic Based Model to Evaluate Huntington Disease Symptoms. J. Healthc. Eng. 2018, 2018, 4581272. [Google Scholar] [CrossRef]
- Mason, S.L.; Daws, R.; Soreq, E.; Johnson, E.B.E.B.; Scahill, R.; Tabrizi, S.J.S.J.; Barker, R.A.; Hampshire, A. Predicting clinical diagnosis in Huntington's disease: An imaging polymarker. Ann. Neurol. 2018, 83, 532–543. [Google Scholar] [CrossRef] [PubMed]
- Asadi, H.; Kok, H.K.; Looby, S.; Brennan, P.; O'Hare, A.; Thornton, J. Outcomes and Complications After Endovascular Treatment of Brain Arteriovenous Malformations: A Prognostication Attempt Using Artificial Intelligence. World Neurosurg. 2016, 96, 562–569. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-L.; Zhao, X.-A.; Ng, S.-H.; Lu, C.-S.; Lin, Y.-C.; Cheng, J.-S.; Tsai, C.-C.; Wang, J.-J. Prediction of the Clinical Severity of Progressive Supranuclear Palsy by Diffusion Tensor Imaging. J. Clin. Med. 2019, 9, 40. [Google Scholar] [CrossRef]
- Zhutovsky, P.; Vijverberg, E.G.; Bruin, W.B.; Thomas, R.M.; Wattjes, M.P.; Pijnenburg, Y.A.; van Wingen, G.A.; Dols, A. Individual Prediction of Behavioral Variant Frontotemporal Dementia Development Using Multivariate Pattern Analysis of Magnetic Resonance Imaging Data. J. Alzheimer's Dis. 2019, 68, 1229–1241. [Google Scholar] [CrossRef]
- An, K.; Zhou, J.-B.; Xiong, Y.; Han, W.; Wang, T.; Ye, Z.-Q.; Wu, Y.-D. Computational Studies of the Structural Basis of Human RPS19 Mutations Associated with Diamond-Blackfan Anemia. Front. Genet. 2021, 12, 650897. [Google Scholar] [CrossRef]
- Pande, A.; Mohapatra, P.; Nicorici, A.; Han, J.J.; Altini, M.; Voos, M. Machine Learning to Improve Energy Expenditure Estimation in Children with Disabilities: A Pilot Study in Duchenne Muscular Dystrophy. JMIR Rehabil. Assist. Technol. 2016, 3, e7. [Google Scholar] [CrossRef] [PubMed]
- Eaton, J.E.; Vesterhus, M.; McCauley, B.M.; Atkinson, E.J.; Schlicht, E.M.; Juran, B.D.; Gossard, A.A.; LaRusso, N.F.; Gores, G.J.; Karlsen, T.H.; et al. Primary Sclerosing Cholangitis Risk Estimate Tool (PREsTo) Predicts Outcomes of the Disease: A Derivation and Validation Study Using Machine Learning. Hepatology 2018, 71, 214–224. [Google Scholar] [CrossRef]
- Robinson, G.A.; Peng, J.; Dönnes, P.; Coelewij, L.; Naja, M.; Radziszewska, A.; Wincup, C.; Peckham, H.; Isenberg, D.A.; Ioannou, Y.; et al. Disease-associated and patient-specific immune cell signatures in juvenile-onset systemic lupus erythematosus: Patient stratification using a machine-learning approach. Lancet Rheumatol. 2020, 2, e485–e496. [Google Scholar] [CrossRef]
- Chou, F.-S.; Ghimire, L.V. Identification of prognostic factors for pediatric myocarditis with a random forests algorithm-assisted approach. Pediatr. Res. 2020, 90, 427–430. [Google Scholar] [CrossRef]
- Chou, F.-S.; Ghimire, L.V. Machine Learning for Mortality Prediction in Pediatric Myocarditis. Front. Pediatr. 2021, 9, 644922. [Google Scholar] [CrossRef] [PubMed]
- Tabor, H.K.; Goldenberg, A. What Precision Medicine Can Learn from Rare Genetic Disease Research and Translation. AMA J. Ethics 2018, 20, 834–840. [Google Scholar] [CrossRef]
- Foksinska, A.; Crowder, C.M.; Crouse, A.B.; Henrikson, J.; Byrd, W.E.; Rosenblatt, G.; Patton, M.J.; He, K.; Tran-Nguyen, T.K.; Zheng, M.; et al. The precision medicine process for treating rare disease using the artificial intelligence tool mediKanren. Front. Artif. Intell. 2022, 5, 910216. [Google Scholar] [CrossRef]
- Bakkar, N.; Kovalik, T.; Lorenzini, I.; Spangler, S.; Lacoste, A.; Sponaugle, K.; Ferrante, P.; Argentinis, E.; Sattler, R.; Bowser, R. Artificial intelligence in neurodegenerative disease research: Use of IBM Watson to identify additional RNA-binding proteins altered in amyotrophic lateral sclerosis. Acta Neuropathol. 2017, 135, 227–247. [Google Scholar] [CrossRef]
- Chen, Y.; Argentinis, J.E.; Weber, G. IBM Watson: How Cognitive Computing Can Be Applied to Big Data Challenges in Life Sciences Research. Clin. Ther. 2016, 38, 688–701. [Google Scholar] [CrossRef]
- Cao, H.; Zhang, L.; Jin, B.; Cheng, S.; Wei, X.; Che, C. Enriching limited information on rare diseases from heterogeneous networks for drug repositioning. BMC Med. Inform. Decis. Mak. 2021, 21, 304. [Google Scholar] [CrossRef] [PubMed]
- Klein, J.J.; Baker, N.C.; Foil, D.H.; Zorn, K.M.; Urbina, F.; Puhl, A.C.; Ekins, S. Using Bibliometric Analysis and Machine Learning to Identify Compounds Binding to Sialidase-1. ACS Omega 2021, 6, 3186–3193. [Google Scholar] [CrossRef]
- Zorn, K.; Lingerfelt, M.; Clark, A.; Ekins, S. Assay Central: A new approach to compiling Big Data and preparing machine learning models for drug repurposing. In Proceedings of the American Chemical Society National Meeting, Washington, DC, USA, 23 August 2017. [Google Scholar] [CrossRef]
- Wolfe, J.M.; Fadzen, C.M.; Choo, Z.-N.; Holden, R.L.; Yao, M.; Hanson, G.J.; Pentelute, B.L. Machine Learning to Predict Cell-Penetrating Peptides for Antisense Delivery. ACS Cent. Sci. 2018, 4, 512–520. [Google Scholar] [CrossRef]
- Esteban-Medina, M.; Peña-Chilet, M.; Loucera, C.; Dopazo, J. Exploring the druggable space around the Fanconi anemia pathway using machine learning and mechanistic models. BMC Bioinform. 2019, 20, 370. [Google Scholar] [CrossRef]
- Taniguchi, T.; D'Andrea, A.D. Molecular pathogenesis of Fanconi anemia: Recent progress. Blood 2006, 107, 4223–4233. [Google Scholar] [CrossRef]
- Spiga, O.; Cicaloni, V.; Visibelli, A.; Davoli, A.; Paparo, M.; Orlandini, M.; Vecchi, B.; Santucci, A. Towards a Precision Medicine Approach Based on Machine Learning for Tailoring Medical Treatment in Alkaptonuria. Int. J. Mol. Sci. 2021, 22, 1187. [Google Scholar] [CrossRef] [PubMed]
| Disease | Methods | Data Type | Sample Size | Model Performance | References |
|---|---|---|---|---|---|
| Huntington disease | ANN | footstep pressure data | 180 | ACC: 89% | [42] |
| SVM | gait data | 15 (post stroke patients), 17 (HD patients), 10 (Controls) | ACC: 90.5% | [43] | |
| SVM | eye tracking data | 22 (Controls), 14 (pre-HD patients), 14 (HD patients) | ACC: 73.47%, TPR: 74.31%, TNR: 72.64% pre-HD vs. Controls ACC: 81.84%, TPR: 76.19%, TNR: 87.48% HD vs. Controls ACC: 83.54%, TPR: 92.62%, TNR: 74.45 % pre-HD vs. HD | [44] | |
| BM | quantitative electroencephalography data | 26 (preHD patients), 25 (Controls) | TNR: 83%, TPR: 83%, ACC: 83%. | [45] | |
| Multiple system atrophy | SVM | MRI data | 30 (MSA patients), 62 (PD patients), 59 (Controls) | ACC: 77.17% | [46] |
| SVM | MRI data | 31 MSA patients, 65 PD patients, 54 (Controls) | ACC: 78% | [47] | |
| ANN | MRI data | 125 (PD patients), 98 (PSP patients), 54 (MSA-P patients), 142 (Controls) | PD ACC: 96.8%, AUC: 0.995 PSP ACC: 93.7%, AUC: 0.982 MSA-P ACC: 95.2%, AUC: 0.990 Controls ACC: 98.4%, AUC: 1.000 | [48] | |
| Amyotrophic lateral sclerosis | ANN | whole-genome data | 4511 (ALS patients), 7397 (Controls) | ACC: 77% | [49] |
| RF | brain MRI data | 24 (ALS patients), 24 (Controls) | ACC: 80% | [50] | |
| SVM | fMRI data | 32 (ALS patients), 31 (Controls) | ACC: 71% | [51] | |
| Amyloidosis | SVM | proteomics data | 75 (amyloid positive), 78 (Controls) | ACC: 96–99% | [52] |
| Hypophosphatasia | SVM | clinical data | 23 (HPP patients), 22 (Controls) | ACC: 90%, TPR: 87%, TNR: 93%, AUC: 0.936 | [53] |
| Friedreich ataxia | SVM | kinematic data | 30 (Friedreich patients), 14 (Controls) | ACC: 91%, TPR: 90%, TNR: 93%, AUC: 0.91 | [54] |
| Progressive supranuclear palsy | SVM | MRI data | 28 (PSP patients), 28 (PD patients), 28 (Controls) | ACC: 85.8%, TPR: 86%, TNR: 86% PD vs. Controls ACC: 89.1%, TPR: 89.5%, TNR: 89.1% PSP vs. Controls PSP vs. PD 84.7 87.5 83.8 | [55] |
| Osteogenesis imperfecta | SVM | μCT images | 21 (specimens of 13 OI patients), 19 (specimens from 15 Controls) | AUC: 96% | [56] |
| Mucormycosis disease | ANN | eye photographs | Not clear | ACC: 99.5% | [57] |
| Retinitis pigmentosa | ANN | ultrawide-field images | 150 (RP patients), 223 (Controls) | AUC: 0.998, TPR: 99.3%, TNR: 99.1% of the ultrawide-field pseudocolor group AUC: 1.000, TPR: 100%, TNR: 99.5% of the ultrawide-field autofluorescence | [58] |
| Cerebral arteriovenous malformation | ANN | Brain CT images | 80 | DSC: 85.2% TPR: 88% TNR: 99% | [59] |
| Duchenne muscular dystrophy | ANN | cine MRI data | 15 (Duchenne patients), 16 (Controls) | DSC: 97.2 for the sagittal view DSC: 96.1 for the axial view DSC: 96.6 for the coronal view | [60] |
| Immune thrombocytopenic purpura | ANN | proteomics data | 64 (pITP patients), 70 (sITP patients), 82 (Controls) | TPR: 87.5%, TNR 69.7%, ACC: 75.0% | [61] |
| Multiple osteochondromas | ANN | clinical data | 96 (class I), 137 (class II), 56 (class III) | Class I ACC: 94% Class II ACC: 80% Class III ACC: 79% | [62] |
| Rett syndrome | ANN | heart rate variation data | 35 (Rett patients), 40 (Controls) | ACC: 88% | [63] |
| Pulmonary arterial hypertension | EL | microRNA expression data | 64 (PAH patients), 43 (Controls) | TPR: 91%, TNR: 64%, ACC: 81%, AUC: 0.85 | [64] |
| Primary sclerosing cholangitis | RF | bacterial 16S rRNA gene sequence data | 24 (PSC patients), 16 (UC patients), 24 (Controls) | PSC AUC: 0.7423 UC AUC: 0.8756 | [65] |
| Choroideremia | RF | OCT/OCTA data | 16 (eyes with choroideremia), 5 (Controls eyes) | J: 0.876 ± 0.066 | [66] |
| Dermatomyositis | RF | sonographic muscle images | 11 (IBM patients), 19 (DM1 patients), 21 (PM-DM patients) | ACC: 78.4% | [67] |
| Disease | Methods | Data Type | Sample Size | Model Performance | References |
|---|---|---|---|---|---|
| Adrenocortical carcinoma | clustering, RF | mRNA expression data | 79 | ACC: 96% | [72] |
| DT | differentially expressed proteins | 117 | [73] | ||
| Alkaptonuria | XGBoost, k-NN | genetic, biochemical, histopathological, clinical, therapeutic resources, and QoL scores | 129 | RAE: 0.25, R2: 0.94 | [75] |
| custering | 112 | [76] | |||
| Amyotrophic lateral sclerosis | RF, SVM | metabolomics data | 38 (treated), 36 (placebo) | TPR: 71.4%, TNR: 71.4%, PPV: 71.4%, NPV: 70.0% | [77] |
| LASSO, RF | a subset of the PRO-ACT dataset (survival and clinical data) | 6565 | C-index: 0.7355 | [78] | |
| RF, XGBoost, BM, DT | a subset of the PRO-ACT dataset | 3772 | ACC: 71–84.7% | [79] | |
| GBoost, SVM | speech acoustic and articulatory data | 1832 | R2: 0.712, RMSE: 37.562 | [80] | |
| ANN | Clinical and MRI data | 135 | ACC: 84.4%. | [81] | |
| Huntington disease | ANN, FLS | finger-tapping tests data | 3032 | R2: 0.98, MSE: 0.08 | [82] |
| SVM, EL | Neuroimaging data | 19 (preHD), 21(Controls) | F1: 74% | [83] | |
| Cerebral arteriovenous malformation | ANN, SVM, Log Reg | clinical and imaging data | 199 | ACC: 97.5% | [84] |
| Progressive supranuclear palsy | LASSO, Lin Reg | Imaging data | 53 | R2: 0.892 | [85] |
| Behavioral variant of frontotemporal dementia | SVM | clinical and structural MRI data | 73 | ACC: 72–82%, TPR: 67–79%, TNR; 77–88%, AUC: 0.80–0.9 | [86] |
| Diamond-Blackfan anemia | SVM | structural data of missense mutation | 29 (positive samples), 30 (negative samples) | ACC: 95%, TPR: 90%, TNR; 98% F1: 94% | [87] |
| Duchenne muscular dystrophy | EL | inertial sensor (accelerometer) data | 7 | RMSE: 0.017 | [88] |
| Primary sclerosing cholangitis | GBoost | clinical and laboratory data | 509 | C-index: 0.90 | [89] |
| Juvenile-onset systemic lupus erythematosus | RF | Immunophenotyping data | 67 (jSLE), 39 (Controls) | ACC: 86·8% | [90] |
| Pediatric myocarditis | RF | Diagnoses/procedures data from the Kids’ Inpatient Database | 7241 | CI: 95% | [91] |
| RF, Log Reg | 4144 | TPR: 89.9% TNR: 85.8%, ACC: 87.9% | [92] |
| Disease | Methods | Data Type | Sample Size | Model Performance | References |
|---|---|---|---|---|---|
| Amyotrophic lateral sclerosis | IBM Watson® | RNA-binding proteins | 1478 | AUC: 0.935 | [95] |
| Multiple diseases, exp. Gaucher disease | ANN | disease, gene, and drug data | 7000 | Hits@10: 0.454, MRR 0.231 | [97] |
| Sialidosis | BM | disease targets and accessible bioactivity data | 57 | AUC: 0.737, PPV: 34.5%, TPR: 91%, TNR: 58.7%, F1: 50% | [98] |
| Duchenne muscular dystrophy | RF | PMO activity data | 64 | ACC:72%, PPV:75%, TPR:69% | [100] |
| Fanconi anemia | EL | gene expression data | >11,000 | R2: 0.62–0.97 | [101] |
| Alkaptonuria | RF | genetic, biochemical, histopathological, clinical, therapeutic resources, and QoL scores | 129 | ACC: 70% | [103] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Visibelli, A.; Roncaglia, B.; Spiga, O.; Santucci, A. The Impact of Artificial Intelligence in the Odyssey of Rare Diseases. Biomedicines 2023, 11, 887. https://doi.org/10.3390/biomedicines11030887
Visibelli A, Roncaglia B, Spiga O, Santucci A. The Impact of Artificial Intelligence in the Odyssey of Rare Diseases. Biomedicines. 2023; 11(3):887. https://doi.org/10.3390/biomedicines11030887
Chicago/Turabian StyleVisibelli, Anna, Bianca Roncaglia, Ottavia Spiga, and Annalisa Santucci. 2023. "The Impact of Artificial Intelligence in the Odyssey of Rare Diseases" Biomedicines 11, no. 3: 887. https://doi.org/10.3390/biomedicines11030887
APA StyleVisibelli, A., Roncaglia, B., Spiga, O., & Santucci, A. (2023). The Impact of Artificial Intelligence in the Odyssey of Rare Diseases. Biomedicines, 11(3), 887. https://doi.org/10.3390/biomedicines11030887







