What Are the Factors Associated with Nonadherence to Medications in Patients with Chronic Diseases?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Data Analysis
2.4. Sample Size Calculations
3. Results
3.1. Demographic Characteristics of the Participants
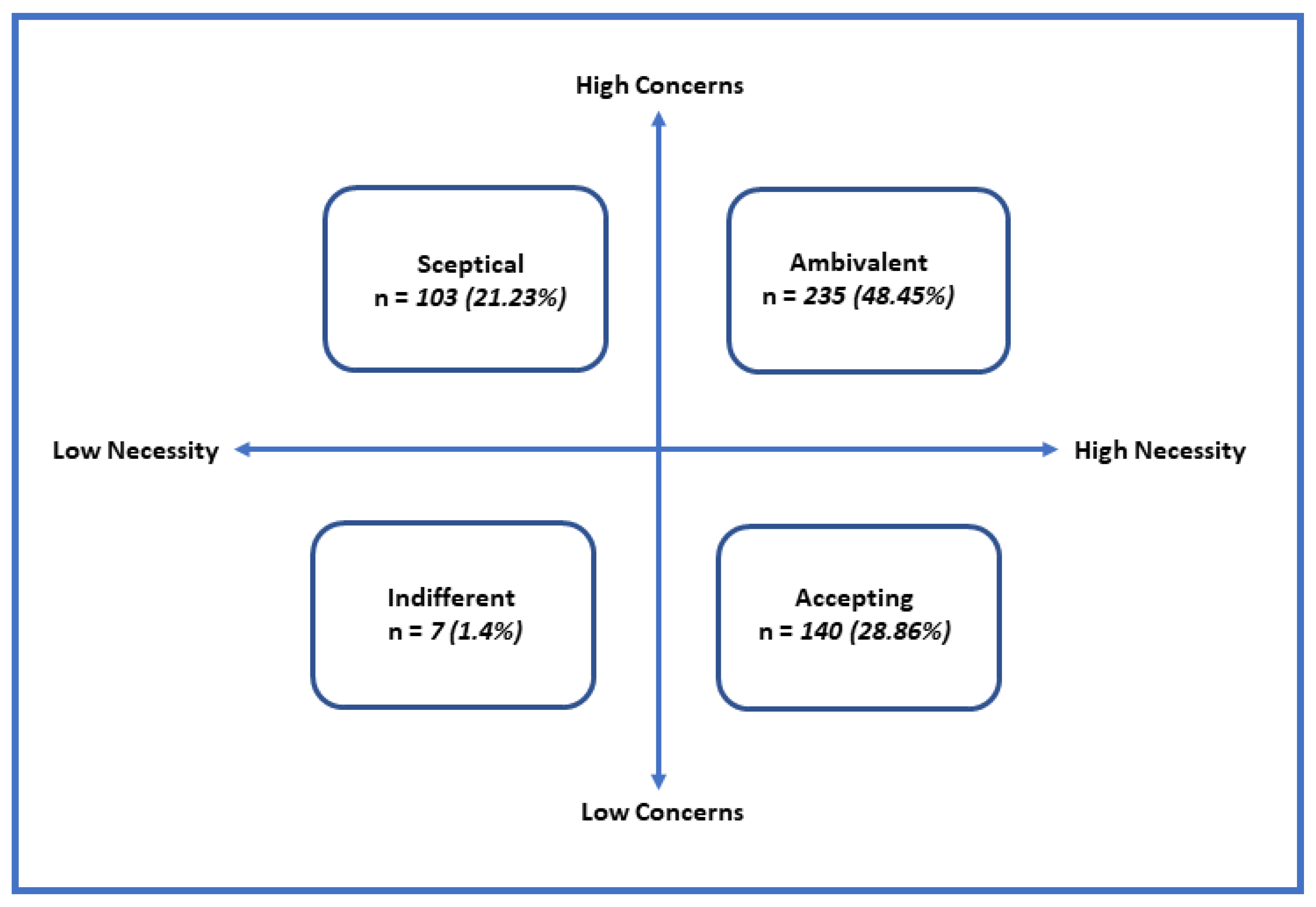
3.2. MARS-5 and BMQ-Reported Responses Portrayals
3.3. Logistic Regression Model
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jaul, E.; Barron, J. Age-Related Diseases and Clinical and Public Health Implications for the 85 Years Old and Over Population. Front. Public Health 2017, 5, 335. [Google Scholar] [CrossRef]
- Maher, R.L.; Hanlon, J.; Hajjar, E.R. Clinical consequences of polypharmacy in elderly. Expert Opin. Drug Saf. 2014, 13, 57–65. [Google Scholar] [CrossRef]
- Yap, A.F.; Thirumoorthy, T.; Kwan, Y.H. Medication adherence in the elderly. J. Clin. Gerontol. Geriatr. 2016, 7, 64–67. [Google Scholar] [CrossRef]
- Bussell, J.K.; Cha, E.S.; Grant, Y.E.; Schwartz, D.D.; Young, L.A. Ways health care providers can promote better medication adherence. Clin. Diabetes 2017, 35, 171–177. [Google Scholar] [CrossRef]
- McHorney, C.A.; Victor Spain, C.; Alexander, C.M.; Simmons, J. Validity of the adherence estimator in the prediction of 9-month persistence with medications prescribed for chronic diseases: A prospective analysis of data from pharmacy claims. Clin. Ther. 2009, 31, 2584–2607. [Google Scholar] [CrossRef] [PubMed]
- Cutler, R.L.; Fernandez-Llimos, F.; Frommer, M.; Benrimoj, C.; Garcia-Cardenas, V. Economic impact of medication non-adherence by disease groups: A systematic review. BMJ Open Sci. 2018, 8, e016982. [Google Scholar] [CrossRef]
- Gast, A.; Mathes, T. Medication adherence influencing factors—An (updated) overview of systematic reviews. Syst. Rev. 2019, 8, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Peral, P.; Conejo-Cerón, S.; Fernández, A.; Berenguera, A.; Martínez-Andrés, M.; Pons-Vigués, M.; Motrico, E.; Rodríguez-Martín, B.; Bellón, J.A.; Rubio-Valera, M. Primary care patients’ perspectives of barriers and enablers of primary prevention and health promotion—A meta-ethnographic synthesis. PLoS ONE 2015, 10, e0125004. [Google Scholar]
- UN Jordan. United Nations Sustainable Development Framework United Nations Jordan. 2019. Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/Annual-Results-Report-Jordan-2019-UNSDF-Final.pdf (accessed on 10 May 2021).
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Gatt, I.; West, L.M.; Calleja, N.; Briffa, C.; Cordina, M. Psychometric properties of the belief about medicines questionnaire (BMQ) in the Maltese language. Pharm. Pract. 2017, 1, 15. [Google Scholar] [CrossRef]
- Horne, R.; Albert, A.; Boone, C. Relationship between beliefs about medicines, adherence to treatment, and disease activity in patients with rheumatoid arthritis under subcutaneous anti-TNFα therapy. Patient Prefer. Adher. 2018, 12, 1099–1111. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; Chapman, S.C.E.; Parham, R.; Freemantle, N.; Forbes, A.; Cooper, V. Understanding patients’ adherence-related Beliefs about Medicines prescribed for long-term conditions: A meta-analytic review of the Necessity-Concerns Framework. PLoS ONE 2013, 8, e80633. [Google Scholar]
- Alsous, M.; Alhalaiqa, F.; Farha, R.A.; Jalil, M.A.; Mcelnay, J.; Horne, R. Reliability and validity of Arabic translation of Medication Adherence Report Scale (MARS) and Beliefs about Medication Questionnaire (BMQ)-specific for use in children and their parents. PLoS ONE 2017, 12, e0171863. [Google Scholar] [CrossRef]
- Nazer, L.H.; Tuffaha, H. Health care and pharmacy practice in Jordan. Can. J. Hosp. Pharm. 2017, 70, 150. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; Weinman, J.; Hankins, M. The beliefs about medicines questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychol. Health 1999, 14, 1–24. [Google Scholar] [CrossRef]
- Kutner, M.; Nachtsheim, C.; Neter, J. Applied Linear Statistical Models, 4th ed.; McGraw-Hill: New York, NY, USA, 2004. [Google Scholar]
- Green, S.B. How Many Subjects Does It Take to Do a Regression Analysis? Multivar. Behav. Res. 1991, 26, 499–510. [Google Scholar] [CrossRef] [PubMed]
- Veehof, L.J.G.; Meyboom-De Jong, B.; Haaijer-Ruskamp, F.M. Polypharmacy in the elderly—A literature review. Eur. J. Gen. Pract. 2000, 6, 98–106. [Google Scholar] [CrossRef]
- Park, H.Y.; Seo, S.A.; Yoo, H.; Lee, K. Medication adherence and beliefs about medication in elderly patients living alone with chronic diseases. Patient Prefer. Adher. 2018, 12, 175–181. [Google Scholar] [CrossRef]
- Coleman, C.I.; Limone, B.; Sobieraj, D.M.; Lee, S.; Roberts, M.S.; Kaur, R.; Alam, T. Dosing frequency and medication adherence in chronic disease. J. Manag. Care Pharm. 2012, 18, 527–539. [Google Scholar] [CrossRef]
- Goette, A.; Hammwöhner, M. How important it is for therapy adherence to be once a day? Eur. Heart J. 2016, 18, I7–I12. [Google Scholar] [CrossRef]
- Ajibola, S.S.; Timothy, F.O. The Influence of National Health Insurance on Medication Adherence Among Outpatient Type 2 Diabetics in Southwest Nigeria. J. Patient Exp. 2018, 5, 114–119. [Google Scholar] [CrossRef]
- Iuga, A.O.; McGuire, M.J. Adherence and health care costs. Risk Manag. Healthc. Policy 2014, 7, 35–44. [Google Scholar] [PubMed]
- Aziz, H.; Hatah, E.; Makmor Bakry, M.; Islahudin, F. How payment scheme affects patients’ adherence to medications? A systematic review. Patient Prefer. Adher. 2016, 10, 837–850. [Google Scholar]
- Gillespie, C.W.; Morin, P.E.; Tucker, J.M.; Purvis, L. Medication Adherence, Health Care Utilization, and Spending among Privately Insured Adults with Chronic Conditions in the United States, 2010–2016. Am. J. Med. 2020, 133, 690–704.e19. [Google Scholar] [CrossRef] [PubMed]
- Olorunfemi, O.; Ojewole, F. Medication belief as correlate of medication adherence among patients with diabetes in Edo State, Nigeria. Nurs. Open 2019, 6, 197–202. [Google Scholar] [CrossRef]
- Glombiewski, J.A.; Nestoriuc, Y.; Rief, W.; Glaesmer, H.; Braehler, E. Medication adherence in the general population. PLoS ONE 2012, 7, e50537. [Google Scholar] [CrossRef]
- Wei, L.; Champman, S.; Li, X.; Li, X.; Li, S.; Chen, R.; Bo, N.; Chater, A.; Horne, R. Beliefs about medicines and non-adherence in patients with stroke, diabetes mellitus and rheumatoid arthritis: A cross-sectional study in China. BMJ Open 2017, 7, e017293. [Google Scholar] [CrossRef]
- Sjölander, M.; Eriksson, M.; Glader, E.L. The association between patients’ beliefs about medicines and adherence to drug treatment after stroke: A cross-sectional questionnaire survey. BMJ Open 2013, 3, e003551. [Google Scholar] [CrossRef]
- Al-Qerem, W.; Jarab, A.; Badinjki, M.; Hyassat, D.; Qarqaz, R. Exploring variables associated with medication non-adherence in patients with type 2 diabetes mellitus. PLoS ONE 2021, 16, e0256666. [Google Scholar] [CrossRef]
- Figueiras, M.; Marcelino, D.S.; Claudino, A.; Cortes, M.A.; Maroco, J.; Weinman, J. Patients’ illness schemata of hypertension: The role of beliefs for the choice of treatment. Psychol. Health 2010, 25, 507–517. [Google Scholar] [CrossRef]
- Alefishat, E.; Jarab, A.S.; Al-Qerem, W.; Abu-Zaytoun, L. Factors Associated with Medication Non-Adherence in Patients with Dyslipidemia. Healthcare 2021, 7, 813. [Google Scholar] [CrossRef] [PubMed]
- Manteuffel, M.; Williams, S.; Chen, W.; Verbrugge, R.R.; Pittman, D.G.; Steinkellner, A. Influence of patient sex and gender on medication use, adherence, and prescribing alignment with guidelines. J. Women’s Health 2014, 23, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.L.; Lee, W.L.; Liang, T.; Liao, I.C. Factors associated with gender differences in medication adherence: A longitudinal study. J. Adv. Nurs. 2014, 70, 2031–2040. [Google Scholar] [CrossRef] [PubMed]
- Braverman, J.; Dedier, J. Predictors of medication adherence for African American patients diagnosed with hypertension. Ethn. Dis. 2009, 19, 396. [Google Scholar]
- Basheti, I.A.; El Hait, S.S.; Qunaibi, E.A.; Aburuz, S.; Bulatova, N. Associations between patient factors and medication adherence: A Jordanian experience. Pharm. Pract. 2016, 14, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ji, N.J.; Hong, Y.P. Effect of income level on adherence to antidepressant treatment in first onset depression outpatients. PLoS ONE 2020, 15, e0238623. [Google Scholar] [CrossRef]
- Kim, S.J.; Kwon, O.D.; Han, E.B.; Lee, C.M.; Oh, S.W.; Joh, H.K.; Oh, B.; Kwon, H.; Cho, B.; Choi, H.C. Impact of number of medications and age on adherence to antihypertensive medications: A nationwide population-based study. Medicine 2019, 98, e17825. [Google Scholar] [CrossRef]
- Al Qasem, A.; Smith, F.; Cliffold, S. Adherence to medication among chronic patients in Middle Eastern countries: Review of studies. EMHJ-East. Mediterr. Health J. 2011, 17, 356–363. [Google Scholar] [CrossRef]
- Srivastava, K.; Arora, A.; Kataria, A.; Cappelleri, J.; Sadosky, A.; Peterson, A.M. Impact of reducing dosing frequency on adherence to oral therapies: A literature review and meta-analysis. Patient Prefer. Adher. 2013, 20, 419–434. [Google Scholar]
- Tarutani, S.; Kikuyama, H.; Ohta, M.; Kanazawa, T.; Okamura, T.; Yoneda, H. Association between medication adherence and duration of outpatient treatment in patients with schizophrenia. Psychiatry Investig. 2016, 13, 413. [Google Scholar] [CrossRef]
| Sample Characteristics | Adhered Frequency (%) or Mean (SD) | Non-Adhered Frequency (%) or Mean (SD) | Total Frequency (%) or Mean (SD) |
|---|---|---|---|
| Gender | |||
| Male | 80 (32.5%) | 166 (76.5%) | 246 (50.7%) |
| Female | 75 (21.4%) | 164 (68.6%) | 239 (49.3 %) |
| Age | 57.34 (13.95) | 57.05 (12.27) | 57.14 (12.81) |
| Educational level | |||
| Illiterate a | 8 (50.0%) | 8 (50.0%) | 16 (3.3%) |
| Primary Education | 11 (20.0%) | 44 (80.0%) | 55 (11.3%) |
| Secondary Education | 54 (41.5%) | 76 (58.5%) | 49 (10.1%) |
| High School | 76 (58.5%) | 54 (41.5%) | 130 (26.8%) |
| Bachelor’s Degree | 59 (30.1%) | 137 (69.9%) | 196 (40.4%) |
| Master’s Degree | 9 (33.3%) | 18 (66.7%) | 27 (5.6) |
| PhD | 3 (75%) | 9 (75%) | 12 (2.5) |
| Income level | |||
| Low b | 16 (29.6%) | 38 (70.4%) | 57 (11.8%) |
| Intermediate c | 115 (30.7%) | 259(69.3%) | 374 (77.1%) |
| High d | 24 (42.1%) | 33 (57.9) | 54 (11.1%) |
| Diseases | |||
| Hypertension | 58 (33.5%) | 115 (66.5%) | 173 (35.7%) |
| Diabetes | 46 (29.5%) | 110 (70.5%) | 156 (32.2%) |
| Cardiovascular | 29 (33.0%) | 59 (67.0%) | 88 (18.1%) |
| Asthma | 17 (32.7%) | 35 (67.3%) | 52 (10.7%) |
| Daily frequency of taking medications | 3.00 (1.35) | 3.78 (2.02) | 3.53(1.87) |
| Ensured | |||
| Yes | 67 (22.3%) | 234 (77.7%) | 301 (62.1%) |
| No | 88 (47.8%) | 96 (52.2%) | 184 (87.9%) |
| Medication Adherence Report Scale | Frequency (%) | Mean (SD) | |
|---|---|---|---|
| I forget to take them | Always | 18 (3.7) | 3.21 (1.10) |
| Often | 116 (23.9) | ||
| Sometimes | 180 (37.1) | ||
| Rarely | 87 (17.9) | ||
| Never | 84 (17.3) | ||
| I change the dose | Always | 8 (1.6) | 3.46 (1.10) |
| Often | 91 (18.8) | ||
| Sometimes | 176 (36.3) | ||
| Rarely | 91 (18.8) | ||
| Never | 119 (24.5) | ||
| I stop taking them for a while | Always | 13 (2.7) | 3.39 (1.13) |
| Often | 93 (19.2) | ||
| Sometimes | 194 (40) | ||
| Rarely | 63 (13) | ||
| Never | 122 (25.2) | ||
| I decide to skip a dose | Always | 6 (1.2) | 3.51 (1.12) |
| Often | 89 (18.4) | ||
| Sometimes | 178 (36.7) | ||
| Rarely | 78 (16.1) | ||
| Never | 134 (27.6) | ||
| I take medications less than instructed | Always | 15 (3.1) | 3.49 (1.14) |
| Often | 77 (15.9) | ||
| Sometimes | 182 (37.5) | ||
| Rarely | 77 (15.9) | ||
| Never | 134 (27.6) | ||
| Statement | Agree/Strongly Agree N (%) | Mean (SD) |
|---|---|---|
| Specific necessity | 3.67 (0.71) | |
| 1—My health, at present, depends on my medicine | 417 (86) | 4.05 (0.94) |
| 2—My life would be impossible without my medicine | 406 (83.7) | 3.75 (0.86) |
| 3—Without my medicine, I would be very sick | 296 (61) | 3.58 (0.89) |
| 4—My health in the future will depend on my medicine | 199 (41) | 3.33 (0.76) |
| 5—My medicine protects me from becoming wore | 275 (59.7) | 3.62 (0.84) |
| Specific concerns | 3.28 (0.84) | |
| 1—Having to take medicine worries me | 137 (28.2) | 3.02 (0.90) |
| 2—I sometimes worry about the long-term effects of my medicine | 296 (61.1) | 3.37 (0.98) |
| 3—My medicines are a mystery to me | 246 (50.7) | 3.24 (0.95) |
| 4—My medicine disrupts my life | 264 (54.4) | 3.13 (1.10) |
| 5—I sometimes worry about becoming too dependent on my medicine | 229 (47.2) | 3.32 (0.90) |
| 6—This medicine gives me unfavorable side effects | 313 (64.5) | 3.59 (0.97) |
| Significant Variables * | B | p-Value | Odds Ratio | Confidence Interval of 95% | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Necessity score | 1.44 | <0.01 | 4.22 | 2.59 | 6.87 |
| Concerns score | −0.32 | 0.02 | 0.73 | 0.56 | 0.95 |
| Frequency of taking medications | −0.30 | <0.01 | 0.74 | 0.65 | 0.84 |
| Medical insurance | |||||
| Ensured | −1.37 | <0.01 | 0.26 | 0.16 | 0.40 |
| Not ensured | Reference | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Bawab, A.Q.; Al-Qerem, W.; Abusara, O.; Alkhatib, N.; Mansour, M.; Horne, R. What Are the Factors Associated with Nonadherence to Medications in Patients with Chronic Diseases? Healthcare 2021, 9, 1237. https://doi.org/10.3390/healthcare9091237
Al Bawab AQ, Al-Qerem W, Abusara O, Alkhatib N, Mansour M, Horne R. What Are the Factors Associated with Nonadherence to Medications in Patients with Chronic Diseases? Healthcare. 2021; 9(9):1237. https://doi.org/10.3390/healthcare9091237
Chicago/Turabian StyleAl Bawab, Abdel Qader, Walid Al-Qerem, Osama Abusara, Nimer Alkhatib, Maha Mansour, and Robert Horne. 2021. "What Are the Factors Associated with Nonadherence to Medications in Patients with Chronic Diseases?" Healthcare 9, no. 9: 1237. https://doi.org/10.3390/healthcare9091237
APA StyleAl Bawab, A. Q., Al-Qerem, W., Abusara, O., Alkhatib, N., Mansour, M., & Horne, R. (2021). What Are the Factors Associated with Nonadherence to Medications in Patients with Chronic Diseases? Healthcare, 9(9), 1237. https://doi.org/10.3390/healthcare9091237







