Association of Continuity of General Practitioner Care with Utilisation of General Practitioner and Specialist Services in China: A Mixed-Method Study
Abstract
:1. Introduction
2. Materials and Methods
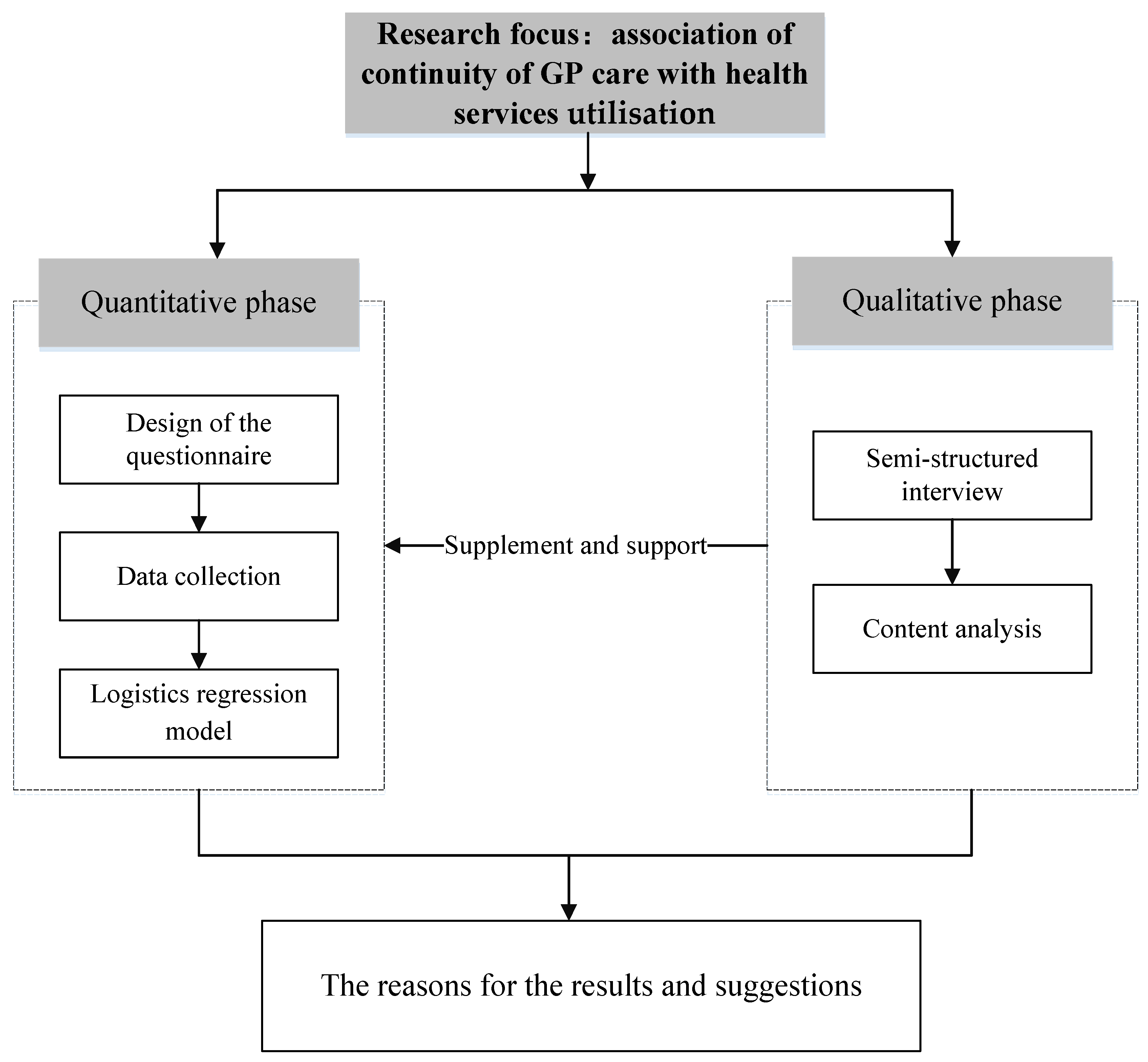
2.1. Study Design
2.2. Quantitative Phase
2.2.1. Data Collection and Subjects
2.2.2. Measurements
Outcome Variables
Measurement of COC
Other Covariates
2.2.3. Statistical Analysis
2.3. Qualitative Phase
2.3.1. Sampling and Interviews
2.3.2. Content Analysis
3. Results
3.1. Quantitative Findings
3.2. Qualitative Findings
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yip, W.C.; Hsiao, W.C.; Chen, W. Early appraisal of China’s huge and complex health-care reforms. Lancet 2012, 379, 833–842. [Google Scholar] [CrossRef]
- Li, X.; Lu, J.; Hu, S.; Cheng, K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Xu, D.R.; Yip, W.; Zhang, H. The primary health-care system in China. Lancet 2017, 390, 2584. [Google Scholar] [CrossRef]
- Zhao, Y.; Lin, J.; Qiu, Y. Demand and Signing of General Practitioner Contract Service among the Urban Elderly: A Population-Based Analysis in Zhejiang Province, China. Int. J. Environ. Res. Public Health 2017, 14, 356. [Google Scholar] [CrossRef] [Green Version]
- Kong, X.; Yang, Y. The current status and challenges of community general practitioner system building in China. Q. J. Med. 2015, 108, 89–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shu, Z.; Wang, Z.; Chen, R.; Li, M.; Lou, J.; Huang, X.; Wu, J.; Jing, L. Allocation and development of the general practitioner workforce in China from 2012 to 2015: A literature review. Lancet 2017, 390, S91. [Google Scholar] [CrossRef]
- Shuang, W.; Fu, X.; Liu, Z.; Bing, W.; Tang, Y.; Feng, H.; Jian, W. General practitioner education reform in China: Most undergraduate medical students do not choose general practitioner as a career under the 5+3 model. Health Prof. Educ. 2017, 4, S2452301116301237. [Google Scholar]
- Liu, Q.; Wang, B.; Kong, Y. China’s primary health-care reform. Lancet 2011, 377, 2064–2066. [Google Scholar] [CrossRef]
- Yip, W.; Fu, H.; Chen, A.T.; Zhai, T.; Jian, W.; Xu, R.; Pan, J.; Hu, M.; Zhou, Z.; Chen, Q.; et al. 10 years of health-care reform in China: Progress and gaps in Universal Health Coverage. Lancet 2019, 394, 1192–1204. [Google Scholar] [CrossRef]
- Shu, Z.; Wang, L.; Sun, X. An evaluation of the effects of general practitioner–supported patient noncommunicable diseases control model in Shanghai, China. Int. J. Health Plan. Manag. 2019, 34, 1–13. [Google Scholar] [CrossRef]
- Yin, J.; Wei, X.; LI, H. Assessing the impact of general practitioner team service on perceived quality of care among patients with non-communicable diseases in China: A natural experimental study. Int. J. Qual. Health Care 2016, 8, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waibel, S.; Henao, D.; Aller, M.-B.; Vargas, I.; Vázquez, M.-L. What do we know about patients’ perceptions of continuity of care? A meta-synthesis of qualitative studies. Int. J. Qual. Health Care 2012, 24, 39–48. [Google Scholar] [CrossRef] [Green Version]
- Reid, R.J.; Haggerty, J.; McKendry, R. Defusing the Confusion: Concepts and Measures of Continuity of Healthcare; Canadian Health Services Research Foundation: Ottawa, ON, Canada, 2002. [Google Scholar]
- Van Walraven, C.; Oake, N.; Jennings, A.; Forster, A.J. The association between continuity of care and outcomes: A systematic and critical review. J. Eval. Clin. Pract. 2010, 16, 947–956. [Google Scholar] [CrossRef] [PubMed]
- Saultz, J.W.; Albedaiwi, W. Interpersonal Continuity of Care and Patient Satisfaction: A Critical Review. Ann. Fam. Med. 2004, 2, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Servellen, G.V.; Fongwa, M.; D’Errico, E.M. Continuity of care and quality care outcomes for people experiencing chronic conditions: A literature review. Nurs. Health Sci. 2010, 8, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Lei, L.; Intrator, O.; Intrator, O.; Fortinsky, R.H.; Cai, S. Continuity of care and health care cost among community-welling older adult veterans living with dementia. Health Serv. Res. 2020, 56, 378–388. [Google Scholar] [CrossRef]
- Saultz, J.W.; Lochner, J. Interpersonal Continuity of Care and Care Outcomes: A Critical Review. Ann. Fam. Med. 2005, 3, 159–166. [Google Scholar] [CrossRef] [Green Version]
- Wu, D.; Lam, T.P. At a crossroads: Family medicine education in China. Acad. Med. 2017, 92, 185–191. [Google Scholar] [CrossRef] [Green Version]
- Dan, W.; Wang, Y.; Lam, K.F.; Hesketh, T. Health system reforms, violence against doctors and job satisfaction in the medical profession: A cross-sectional survey in Zhejiang Province, Eastern China. BMJ Open 2014, 4, e006431. [Google Scholar]
- Hansen, A.H.; Kristoffersen, A.E.; Lian, O.S.; Halvorsen, P.A. Continuity of GP care is associated with lower use of complementary and alternative medical providers: A population-based cross-sectional survey. BMC Health Serv. Res. 2014, 14, 629. [Google Scholar] [CrossRef] [Green Version]
- Maccallum, R.C.; Widaman, K.F.; Zhang, S.; Hong, S. Sample Size in Factor Analysis. Psychol. Methods 1999, 4, 84–99. [Google Scholar] [CrossRef]
- Uijen, A.A.; Schellevis, F.G.; Wj, V.D.B.; Mokkink, H.G.; Van Weel, C.; Schers, H.J. Nijmegen Continuity Questionnaire: Development and testing of a questionnaire that measures continuity of care. J. Clin. Epidemiol. 2011, 64, 1391–1399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aller, M.B.; Vargas, I.; Garciasubirats, I.; Coderch, J.; Colomés, L.; Llopart, J.R.; Ferran, M.; Sánchezpérez, I.; Vázquez, M.L. A tool for assessing continuity of care across care levels: An extended psychometric validation of the CCAENA questionnaire. Int. J. Integr. Care 2013, 13, e050. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carver, C.S. You want to measure coping but your protocol’ too long: Consider the brief cope. Int. J. Behav. Med. 1997, 4, 92. [Google Scholar] [CrossRef] [PubMed]
- Hill, M.C.; Tiedeman, C.R. Evaluating Model Fit. In Effective Groundwater Model Calibration: With Analysis of Data, Sensitivities, Predictions, and Uncertainty; John Wiley & Sons: Hoboken, NJ, USA, 2005. [Google Scholar]
- Cho, K.H.; Lee, S.G.; Jun, B.; Jung, B.Y.; Kim, J.H.; Park, E.C. Effects of continuity of care on hospital admission in patients with type 2 diabetes: Analysis of nationwide insurance data. BMC Health Serv. Res. 2015, 15, 107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uijen, A.A.; Heinst, C.W.; Schellevis, F.G.; van den Bosch, W.J.; van de Laar, F.A.; Terwee, C.B.; Schers, H.J. Measurement Properties of Questionnaires Measuring Continuity of Care: A Systematic Review. PLoS ONE 2012, 7, e42256. [Google Scholar] [CrossRef]
- Marta-Beatriz, A.; Ingrid, V.; Sina, W.; Jordi, C.; Inma, S.P.; Lluís, C.; Ramon, L.J.; Manel, F.; Luisa, V.M. A comprehensive analysis of patients’ perceptions of continuity of care and their associated factors. Int. J. Qual. Health Care J. Int. Soc. Qual. Health Care 2013, 25, 291–299. [Google Scholar]
- Weitzman, E.A. Analyzing qualitative data with computer software. Health Serv. Res. 1999, 34, 1241–1263. [Google Scholar] [PubMed]
- Strauss, A.L.; Corbin, J.M. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory; Sage: Thousand Oaks, CA, USA, 2014; Volume 36, p. 129. [Google Scholar]
- Bernard, H.R.; Ryan, G.W. Analyzing Qualitative Data: Systematic Approaches; Sage: Thousand Oaks, CA, USA, 2010. [Google Scholar]
- Jalil, A.; Zakar, R.; Zakar, M.Z.; Fischer, F. Patient satisfaction with doctor-patient interactions: A mixed methods study among diabetes mellitus patients in Pakistan. BMC Health Serv. Res. 2017, 17, 155. [Google Scholar] [CrossRef] [Green Version]
- Agarwal, G.; Crooks, V.A. The nature of informational continuity of care in general practice. Br. J. Gen. Pract. 2008, 58, 17–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koirala, N. Trust and Communication in a Doctor Patient Relationship. Birat J. Health Sci. 2020, 4, 770. [Google Scholar] [CrossRef]
- Ionescu-Ittu, R.; M Cc Usker, J.; Ciampi, A.; Vadeboncoeur, A.M.; Roberge, D.; Larouche, D.; Verdon, J.; Pineault, R. Continuity of primary care and emergency department utilization among elderly people. Can. Med Assoc. J. 2007, 177, 1362. [Google Scholar] [CrossRef] [Green Version]
- Waibel, S.; Vargas, I.; Aller, M.B.; Coderch, J.; Farré, J.; Vázquez, M. Continuity of clinical management and information across care levels: Perceptions of users of different healthcare areas in the Catalan national health system. BMC Health Serv. Res. 2016, 16, 466. [Google Scholar] [CrossRef] [Green Version]
- Chen, Q.; Zhang, X.; Gu, J.; Wang, T.; Zhang, Y.; Zhu, S. General practitioners’ hypertension knowledge and training needs: A survey in Xuhui district, Shanghai. BMC Fam. Pract. 2013, 14, 16–26. [Google Scholar] [CrossRef] [Green Version]
- Fung, C.S.C.; Wong, C.K.H.; Fong, D.Y.T.; Lee, A.; Lam, C.L.K. Having a family doctor was associated with lower utilization of hospital-based health services. BMC Health Serv. Res. 2015, 15, 42. [Google Scholar] [CrossRef] [Green Version]
- Haggerty, J.L.; Reid, R.J.; Freeman, G.K.; Starfield, B.H.; Adair, C.E.; McKendry, R. Continuity of care: A multidisciplinary review. BMJ 2003, 327, 1219–1221. [Google Scholar] [CrossRef] [Green Version]
- Schulman, B.A. Active patient orientation and outcomes in hypertensive treatment: Application of a socio-organizational perspective. Med. Care 1979, 17, 267–280. [Google Scholar] [CrossRef] [PubMed]
- Liu, H. Is There a Problem of Excessive Medical Treatment Issues in China? From the Perspective of Medical Service Efficiency Measurement of Urban Hospitals in Provincial Regions. J. Soc. Sci. 2015, 12, 65–75. [Google Scholar]
- Dai, H.; Fang, L.; Malouin, R.A.; Huang, L.; Liu, G. Family Medicine Training in China. Fam. Med. 2013, 45, 341–344. [Google Scholar] [PubMed]
- Negri, A.; Zamin, C.; Parisi, G.; Paladino, A.; Andreoli, G. Analysis of General Practitioners’ Attitudes and Beliefs about Psychological Intervention and the Medicine-Psychology Relationship in Primary Care: Toward a New Comprehensive Approach to Primary Health Care. Healthcare 2021, 9, 613. [Google Scholar] [CrossRef]
| Dimension | Items |
|---|---|
| IC | 1. I know the GP very well |
| 2. I believe that the GP knows my previous medical history very well | |
| 3. I believe the GP knows my living environment very well | |
| 4. I believe the GP knows my daily activities very well | |
| 5. I believe the GP knows a general level of my health very well | |
| MC | 6. I feel comfortable consulting the GP about my doubts or health problems |
| 7. During the consultation process, the GP can inquire about my physical condition carefully | |
| 8. The GP is very clear about what kind of treatment is most effective for me | |
| RC | 9. I can contact the GP easily when needed |
| 10. I go to visit the same GP every time I become sick | |
| 11. The GP can provide services in my home, such as home visits or home care beds | |
| 12. The GP can communicate with me and teach me health knowledge |
| Characteristics of Respondents | n | % |
|---|---|---|
| Gender | ||
| Male | 249 | 39.9 |
| Female | 375 | 60.1 |
| Age (years) | ||
| 18–25 | 128 | 20.5 |
| 26–35 | 278 | 44.6 |
| 36–45 | 112 | 17.9 |
| 46–55 | 57 | 9.1 |
| ≥56 | 49 | 7.9 |
| Education | ||
| Primary school or below | 24 | 3.8 |
| Junior high school | 57 | 9.1 |
| High school | 156 | 25.0 |
| Bachelor’s degree | 262 | 42.0 |
| Graduate degree or above | 125 | 20.0 |
| Household income per capita (¥RMB) | ||
| <3000 | 39 | 6.3 |
| 3000– | 162 | 26.0 |
| 5000– | 153 | 24.5 |
| 8000– | 101 | 16.2 |
| 10,000≤ | 169 | 27.1 |
| Marital status | ||
| Single | 138 | 22.1 |
| Married | 447 | 71.6 |
| Other | 39 | 6.3 |
| Medical insurance | ||
| Uninsured | 58 | 9.3 |
| Insured | 566 | 90.7 |
| Chronic diseases | ||
| Yes | 114 | 18.3 |
| No | 510 | 81.7 |
| Self-rated health status | ||
| Bad | 49 | 7.8 |
| Fair | 292 | 46.8 |
| Good | 283 | 45.4 |
| IC | ||
| Low | 353 | 56.6 |
| High | 271 | 43.4 |
| MC | ||
| Low | 321 | 51.4 |
| High | 303 | 48.6 |
| RC | ||
| Low | 360 | 57.7 |
| High | 264 | 42.3 |
| Intention to Visit GP | GP Visits | Specialist Visits | ||||
|---|---|---|---|---|---|---|
| No | Yes | Mean | SD * | Mean | SD | |
| IC | ||||||
| Low | 258 | 95 | 0.60 | 1.08 | 0.59 | 0.90 |
| High | 142 | 129 | 0.68 | 1.15 | 0.63 | 1.09 |
| p | <0.001 | <0.001 | 0.488 | |||
| MC | ||||||
| Low | 240 | 81 | 0.79 | 1.37 | 0.64 | 1.02 |
| High | 160 | 143 | 1.15 | 1.56 | 0.49 | 0.83 |
| p | <0.001 | <0.001 | 0.036 | |||
| RC | ||||||
| Low | 266 | 94 | 0.60 | 0.95 | 0.55 | 0.98 |
| High | 124 | 130 | 1.32 | 1.25 | 0.45 | 0.73 |
| p | <0.001 | <0.001 | 0.099 | |||
| Characteristics | Intention to Visit GP | GP Visits | Specialist Visits | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR * | 95% CI * | p | β | 95% CI | p | β | 95% CI | p | |
| IC (ref. = low) | |||||||||
| High | 3.583 | 1.828–7.024 | <0.001 | 0.418 | 0.100–0.735 | 0.010 | 0.128 | −0.277–0.533 | 0.535 |
| MC (ref. = low) | |||||||||
| High | 0.924 | 0.436–1.959 | 0.837 | −0.030 | −0.412–0.352 | 0.878 | −0.438 | −0.874–−0.001 | 0.037 |
| RC (ref. = low) | |||||||||
| High | 1.758 | 0.843–3.666 | 0.132 | 0.446 | 0.089–0.804 | 0.014 | −0.142 | −0.637–0.243 | 0.381 |
| Gender (ref. = male) | |||||||||
| Female | 0.929 | 0.627–1.375 | 0.711 | −0.053 | −0.233–0.128 | 0.569 | −0.009 | −0.234–0.215 | 0.935 |
| Age (ref. = 18–25) | |||||||||
| 26–35 | 1.769 | 0.868–3.604 | 0.116 | 0.509 | 0.127–0.891 | 0.009 | 0.044 | −0.401–0.490 | 0.846 |
| 36–45 | 2.666 | 1.171–6.161 | 0.020 | 0.541 | 0.106–0.975 | 0.015 | 0.224 | −0.261–0.710 | 0.366 |
| 46–55 | 3.589 | 1.358–9.488 | 0.010 | 0.804 | 0.328–1.279 | 0.001 | −0.106 | −0.702–0.491 | 0.728 |
| ≥56 | 4.096 | 1.338–12.538 | 0.013 | 0.656 | 0.571–1.542 | 0.001 | 0.065 | −0.562–0.692 | 0.839 |
| Education (ref. = primary school or below) | |||||||||
| Junior high school | 0.909 | 0.289–2.861 | 0.870 | −0.236 | −0.646–0.174 | 0.259 | −0.410 | −1.152–0.331 | 0.278 |
| High school | 0.627 | 0.212–1.849 | 0.397 | −0.157 | −0.551–0.237 | 0.434 | 0.342 | −0.300–0.984 | 0.296 |
| Bachelor’s degree | 0.523 | 0.176–1.554 | 0.244 | −0.152 | −0.564–0.260 | 0.471 | 0.241 | −0.416–0.898 | 0.472 |
| Graduate degree or above | 0.513 | 0.160–1.640 | 0.260 | −0.386 | −0.851–0.080 | 0.104 | 0.417 | −0.268–1.102 | 0.233 |
| Income (ref. ≤ 3000) | |||||||||
| 3000– | 0.362 | 0.162–0.809 | 0.013 | 0.664 | 0.233–1.095 | 0.003 | 0.759 | 0.090–1.428 | 0.026 |
| 5000– | 0.297 | 0.131–0.676 | 0.004 | 0.544 | 0.087–1.001 | 0.020 | 0.543 | −0.146–1.232 | 0.122 |
| 8000– | 0.316 | 0.132–0.759 | 0.010 | 0.564 | 0.078–1.050 | 0.023 | 0.544 | −0.167–1.255 | 0.134 |
| ≥10,000 | 0.154 | 0.065–0.367 | 0.000 | 0.561 | 0.095–1.027 | 0.018 | 0.940 | 0.256–1.625 | 0.007 |
| Marital status (ref. = Single) | |||||||||
| Married | 0.510 | 0.259–1.006 | 0.052 | −0.022 | −0.363–0.318 | 0.898 | 0.223 | −0.179–0.333 | 0.295 |
| Other | 0.381 | 0.135–1.078 | 0.069 | −0.405 | −0.866–0.055 | 0.084 | 0.222 | −0.307–0.461 | 0.446 |
| Medical insurance (ref. = Uninsured) | |||||||||
| Insured | 0.608 | 0.323–1.144 | 0.123 | 0.118 | −0.231–0.466 | 0.509 | 0.406 | −0.077–0.888 | 0.099 |
| Chronic diseases (ref. = no) | |||||||||
| Yes | 0.913 | 0.494–1.685 | 0.770 | 0.364 | 0.114–0.614 | 0.004 | 0.549 | 0.253–0.844 | 0.001 |
| Self-rated health status (ref. = bad) | |||||||||
| Fair | 0.807 | 0.376–1.732 | 0.582 | −0.464 | −0.733–−0.195 | 0.001 | −0.330 | −0.677–0.017 | 0.063 |
| Good | 0.953 | 0.439–2.071 | 0.903 | −0.619 | −0.905–0.333 | 0.000 | −0.378 | −0.739—0.016 | 0.041 |
| Domains | Associated Themes | Example of Verbatim Transcript |
|---|---|---|
| Service capabilities | Effective treatment (20 interviewees) | “…When I get sick, I go to a tertiary hospital, because the treatment is very effective, and the general practitioners in the community are not technical…” “…The diagnosis and treatment skills of general practitioners are not as good as those of specialists in tertiary hospitals, so I still choose tertiary hospitals…” |
| Working experience and education of GPs (18 interviewees) | “…Most of the general practitioners’ academic qualifications are college or undergraduate qualifications, and the level of education is generally low…, but the qualifications of specialists in tertiary hospitals are mostly Ph.D.” “…Many general practitioners are very young and have no experience, so I have no confidence in their skills. I am afraid that there will be misdiagnosis and missed diagnosis…” | |
| Accuracy of diagnosis (16 interviewees) | “…Community health service centres lack a lot of medical equipment, and some laboratory tests cannot be done…, Only essential medicines are provided, and other medicines cannot be used…” | |
| Doctor–patient interaction | Doctor–patient communication (19 interviewees) | “…For some minor illnesses, I usually visit a GP because he has time to communicate with me and tell me what I should pay attention to in my daily life…” |
| Doctor–patient familiarity (17 interviewees) | “…I signed a GP as my family doctor. He often visits for follow-up visits, so he knows my situation well. So, it’s very convenient for me to visit GP…” | |
| Doctor–patient trust (14 interviewees) | “…I am a hypertensive patient and often come to community health service centres. I know general practitioners very well. They will prescribe different drugs for me according to my blood pressure. Currently my blood pressure is controlled very well, I trust them very much… Sometimes they followed up regularly and give some guidance on diet and drug use” | |
| Time provision | Waiting time (15 interviewees) | “…The community health service centre is very close to my home. It is very convenient for me to come here to see a general practitioner. At the same time, it’s not like a tertiary hospital where you have to wait in line for a long time…” |
| Service time (12 interviewees) | “…General practitioners also provide me with service lasting at least 15 min of and ask me carefully about my condition, but specialists in tertiary hospitals spend about 5 min each time…” |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, T.; Wang, X. Association of Continuity of General Practitioner Care with Utilisation of General Practitioner and Specialist Services in China: A Mixed-Method Study. Healthcare 2021, 9, 1206. https://doi.org/10.3390/healthcare9091206
Zhang T, Wang X. Association of Continuity of General Practitioner Care with Utilisation of General Practitioner and Specialist Services in China: A Mixed-Method Study. Healthcare. 2021; 9(9):1206. https://doi.org/10.3390/healthcare9091206
Chicago/Turabian StyleZhang, Tao, and Xiaohe Wang. 2021. "Association of Continuity of General Practitioner Care with Utilisation of General Practitioner and Specialist Services in China: A Mixed-Method Study" Healthcare 9, no. 9: 1206. https://doi.org/10.3390/healthcare9091206






