Rehabilitation Process Issues and Functional Performance after Total Hip and Knee Replacement
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
- (i)
- They underwent THR or TKR surgery between 1 January 2015 and 30 June 2016, at Research Institute of Traumatology, Orthopedics and Neurosurgery of Saratov State Medical University;
- (ii)
- They were diagnosed with unilateral coxarthrosis (M16) or gonarthrosis (M17);
- (iii)
- They were over 18 years of age.
- (i)
- Their contact information in medical records was absent or outdated;
- (ii)
- They could not be reached by phone calls;
- (iii)
- They did not respond to all questions of the survey.
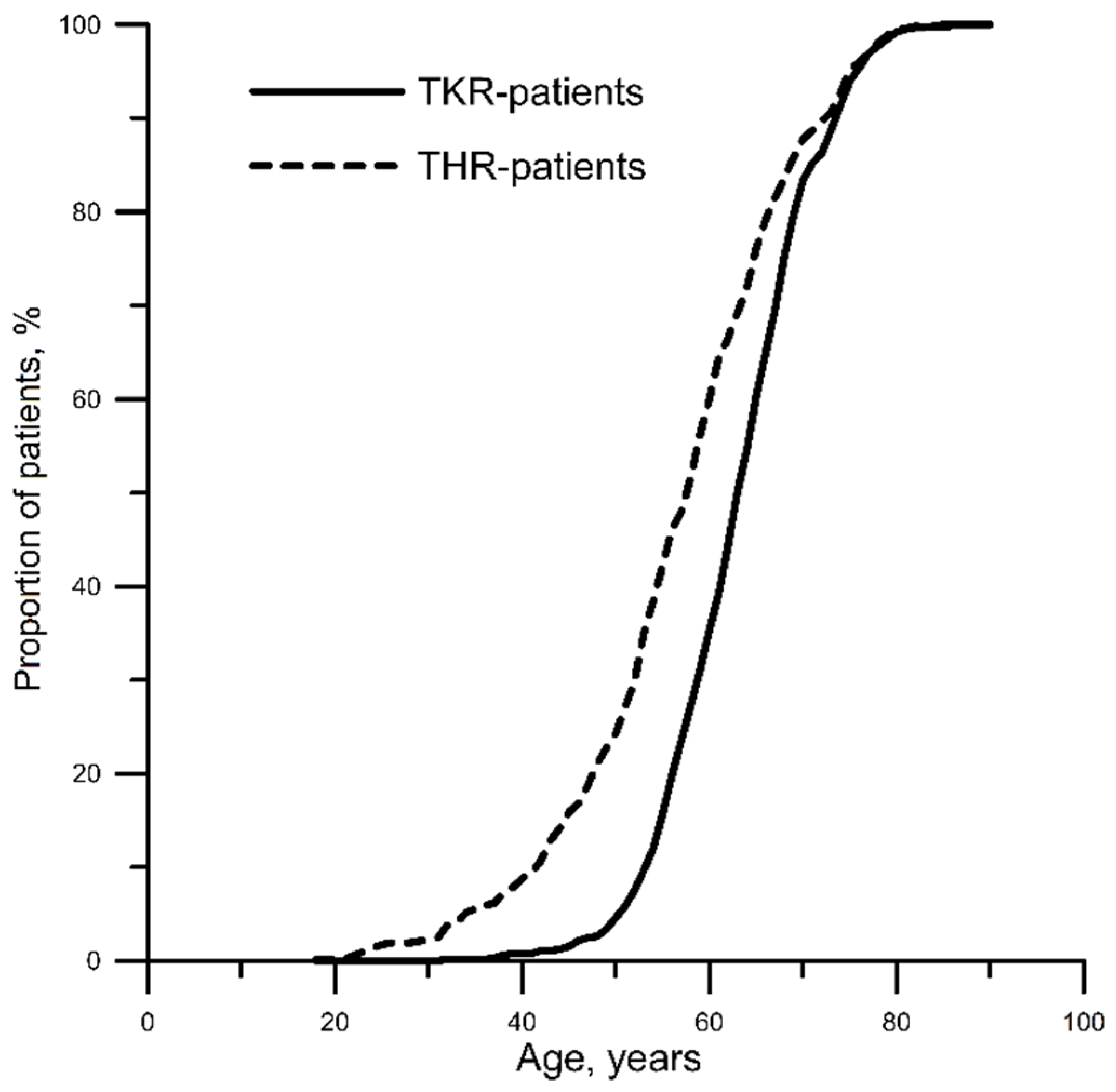
2.2. Participants
2.3. Questionnaire Survey
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Woolf, A.D.; Pfleger, B. Burden of major musculoskeletal conditions. Bull. World Health Organ. 2003, 81, 646–656. [Google Scholar]
- Storheim, K.; Zwart, J.A. Musculoskeletal disorders and the Global Burden of Disease study. Ann. Rheum. Dis. 2014, 73, 949–950. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Litwic, A.; Edwards, M.H.; Dennison, E.M. Cooper Cyrus. Epidemiology and burden of osteoarthritis. Br. Med. Bull. 2013, 105, 185–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conaghan, P.G.; Dickson, J.; Grant, R.L. Guideline Development Group. Care and Management of Osteoarthritis in Adults: Summary of NICE Guidance. BMJ 2008, 336, 502–503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Clinical Guideline Centre (UK). Osteoarthritis: Care and Management in Adults; National Institute for Health and Care Excellence (UK): London, UK, 2014. [Google Scholar]
- Nelson, A.E.; Allen, K.D.; Golightly, Y.M.; Goode, A.P.; Jordan, J.M. A systematic review of recommendations and guidelines for the management of osteoarthritis: The chronic osteoarthritis management initiative of the U.S. bone and joint initiative. Semin. Arthritis Rheum. 2014, 43, 701–712. [Google Scholar] [CrossRef] [PubMed]
- Kremers, M.H.; Larson, D.R.; Crowson, C.S.; Kremers, W.K.; Washington, R.E.; Steiner, C.A.; Jiranek, W.A.; Berry, D.J. Prevalence of total hip and knee replacement in the United States. J. Bone Jt. Surg. Am. 2015, 97, 1386–1397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hunt, L.P.; Blom, A.; Wilkinson, J.M. An analysis of 30-day mortality after weekend versus weekday elective joint arthroplasty in England and Wales: A cohort study using the National Joint Registry Dataset. Bone Jt. J. 2017, 99, 1618–1628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torre, M.; Romanini, E.; Zanoli, G.; Carrani, E.; Luzi, I.; Leone, L.; Leone, L.; Bellino, S. Monitoring outcome of joint arthroplasty in Italy: Implementation of the National Registry. Joints 2017, 5, 70–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van der Wees, P.J.; Wammes, J.J.; Akkermans, R.P.; Koetsenruijter, J.; Westert, G.P.; van Kampen, A.; Hannink, G.; de Waal-Malefijt, M.; Schreurs, B.W. Patient-reported health outcomes after total hip and knee surgery in a Dutch University Hospital Setting: Results of twenty years clinical registry. BMC Musculoskelet. Disord. 2017, 18, 97. [Google Scholar] [CrossRef] [Green Version]
- Tikhilov, R.M.; Kornilov, N.N.; Kulyaba, T.A.; Fil’, A.S.; Drozdova, P.V.; Petukhov, A.I. Comparative analysis of knee replacement registers (review). Travmatol. Ortop. Ross. 2014, 2, 112–121. [Google Scholar] [CrossRef] [Green Version]
- Zagorodniy, N.V. Joint replacement in the Russian Federation. In Proceedings of the Research and Practice Conference Vreden Readings, Saint-Petersburg, Russia, 26–28 September 2013; Available online: http://vredenreadings.org/arc/28/Zagorodny.pdf (accessed on 2 December 2020).
- Goryannaya, N.A.; Ishekova, N.I.; Popov, V.V.; Bondarenko, E.G. Change of patients’ quality of life after hip replacement at the first stage of rehabilitation. Hum. Ecol. 2017, 1, 41–44. [Google Scholar] [CrossRef]
- Asilova, S.U.; Ruzibaev, D.R. Medical-and-social examination and rehabilitation of patients and disabled persons after the hip total arthroplasty. Geniy Ortop. 2015, 2, 36–39. [Google Scholar] [CrossRef]
- Norkin, I.A.; Baratov, A.V.; Akimova, T.N.; Yushina, B.S.; Vegele, L.S. The traumatological orthopedic service of Region: Problems and goals. Zdr. Ross. Fed. 2014, 58, 12–17. [Google Scholar]
- Shubnjakov, I.I.; Tihilov, R.M.; Nikolaev, N.S.; Grigoricheva, L.G.; Ovsjankin, A.V.; Chernyj, A.Z.; Drozdova, P.V.; Denisov, A.O.; Veber, E.V.; Kuz’mina, I.V. Epidemiology of primary hip endoprosthesis on the basis of the data of the register of arthroplasty RSRITO named after R. R. Vreden. Traumatol. Orthop. Russ. 2017, 23, 81–101. [Google Scholar] [CrossRef] [Green Version]
- Resources and Activities of Health Care Organizations. Key Indicators of Health Care. Part VI, 2019. Russian. Available online: https://www.rosminzdrav.ru/ministry/61/22/stranitsa-979/statisticheskie-i-informatsionnye-materialy/statisticheskiy-sbornik-2018-god (accessed on 2 November 2020).
- Sandakov, J.P.; Kochubej, A.V.; Chernjahovskij, O.B.; Kochubej, V.V. Evaluation of polyclinic rehabilitation after joint endoprosthesis. Probl. Soc. Hyg. Health Care Med Hist. 2020, 28, 101–105. [Google Scholar]
- Zagorodniy, N.V.; Elkin, D.V.; Banetskiy, M.V.; Sharkeev, V.N.; Grebchenko, N.V.; Kurnikov, D.A. Medium-term results of femoral component of implants “Implant-Elit” by MATI-Medtech use in clinical practice at cementless fixation. Acta Biomed. Sci. 2006, 4, 104–109. [Google Scholar]
- Wong, N.M.R.; Cheung, W.L.; Ng, C.K.; Wong, K.K.; Lau, S.W.; Hung, T. A new multi-disciplinary rehabilitation outcome checklist for the rehabilitation of total knee and total hip replacement patients. J. Orthop. Trauma Rehabil. 2013, 17, 40–45. [Google Scholar] [CrossRef] [Green Version]
- Woolhead, G.M.; Donovan, J.L.; Dieppe, P.A. Outcomes of total knee replacement: A qualitative study. Rheumatology 2005, 44, 1032–1037. [Google Scholar] [CrossRef] [Green Version]
- Stavrev, V.P.; Ilieva, E.M. The holistic approach to rehabilitation of patients after total hip joint replacement. Folia Med. (Plovdiv) 2003, 45, 16–21. [Google Scholar]
- Desai, A.S.; Dramis, A.; Board, T.N. Leg length discrepancy after total hip arthroplasty: A review of literature. Curr. Rev. Musculoskelet. Med. 2013, 6, 336–341. [Google Scholar] [CrossRef] [Green Version]
- Fedonnikov, A.S. Communication with patients and colleagues in rehabilitation process: Needs, expectations and responsibility of the orthopedic surgeons. Russ. Open Med. J. 2019, 8, e0306. [Google Scholar] [CrossRef] [Green Version]
- Fedonnikov, A.; Andriyanova, E.; Grishechkina, N. Online communication-based rehabilitation management for patients with replaced joints: Experience and opportunities. Archiv EuroMedica 2020, 10, 91–94. [Google Scholar] [CrossRef]
- Lingard, E.A.; Verven, S.; Katz, J.N. Management and care of patients undergoing total knee arthroplasty: Variations across different health care settings. Arthritis Care Res. 2000, 13, 129–136. [Google Scholar] [CrossRef]
- Mahomed, N.N.; Lau, J.T.C.; Lin, M.K.S.; Zdero, R.; Davey, J.R. Significant variation exists in home care services following total joint arthroplasty. J. Rheumatol. 2004, 31, 973–975. [Google Scholar]
- Mauer, K.A.; Abrahams, E.B.; Arslanian, C.; Schoenly, L.; Taggart, H.M. National practice patterns for the care of the patient with total joint replacement. Orthop. Nurs. 2002, 21, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Canadian Institute for Health Information. Hip and Knee Replacements in Canada—Canadian Joint Replacement Registry (CJRR) 2008–2009 Annual Report; CIHI: Ottawa, ON, Canada, 2009. [Google Scholar]
- Donabedian, A. The definition of quality and approaches to its assessment. In Explorations in Quality Assessment and Monitoring; Health Administration Press: Ann Arbor, MI, USA, 1980; Volume 1, pp. 95–99. [Google Scholar]
- Breugem, S.J.; Haverkamp, D. Anterior knee pain after a total knee arthroplasty: What can cause this pain? World J. Orthop. 2014, 5, 163–170. [Google Scholar] [CrossRef]
- Kastyro, I.V.; Torshin, V.I.; Drozdova, G.A.; Popadyuk, V.I. Acute pain intensity in men and women after septoplasty. Russ. Open Med. J. 2017, 6, e0305. [Google Scholar] [CrossRef] [Green Version]
- Edelen, M.O.; Saliba, D. Correspondence of verbal descriptor and numeric rating scales for pain intensity: An item response theory calibration. J. Gerontol. A Biol. Sci. Med. Sci. 2010, 65, 778–785. [Google Scholar] [CrossRef] [Green Version]
- Carr, E.C.J.; Mann, E.M. Pain: Creative Approaches to Effective Management; Macmillan Publishers Ltd.: Basingstoke, UK, 2000. [Google Scholar]
- Turk, D.C.; Melzack, R. Handbook of Pain Assessment, 2nd ed.; Guilford Press: New York, NY, USA, 2001. [Google Scholar]
| Time Elapsed after the Surgery, Months | THR-Patients (n = 523) | TKR-Patients (n = 650) | p-Value |
|---|---|---|---|
| Under 3 | 4.2 (2.7–6.3) | 5.6 (4.0–7.7) | 0.27 |
| 3–6 | 8.0 (5.8–10.7) | 8.9 (6.8–11.4) | 0.58 |
| 6–12 | 25.1 (21.4–29.1) | 28.0 (24.6–31.6) | 0.27 |
| Over 12 | 62.7 (58.4–66.9) | 57.5 (53.6–61.3) | 0.07 |
| No. | Survey Results | THR Patients (n = 523) | TKR Patients (n = 650) | p-Value |
|---|---|---|---|---|
| Local orthopedic postsurgical monitoring | ||||
| 1.1.1. | Regular (after 3, 6, 12 months; annually afterwards *) visits to a local orthopedic surgeon | 73.2 (69.2–77.0) | 66.5 (62.7–70.1) | 0.01 |
| 1.1.2. | Irregular visits to a local orthopedic surgeon | 17.4 ( 14.3–20.9) | 19.4 (16.4–22.7) | 0.38 |
| 1.1.3. | No local orthopedic monitoring | 9.2 (6.9–12.0) | 13.6 (11.1–16.5) | 0.02 |
| 1.1.4. | Other | 0.2 (0.01–1.1) | 0.5 (0.1–1.4) | 0.40 |
| Communication with local health authorities | ||||
| 1.2.1. | Feedback from regional health services representative offering a rehabilitation course | 8.6 (6.3–11.3) | 8.8 (6.7–11.3) | 0.90 |
| 1.2.2. | Voluntary visits to a local orthopedic surgeon | 74.2 (70.2–77.9) | 68.7 (65.0–72.3) | 0.04 |
| 1.2.3. | Voluntary consultation with the orthopedic surgeon who performed the surgery | 7.6 (5.5–10.2) | 10.6 (8.3–13.2) | 0.08 |
| 1.2.4. | Absence of both communication with healthcare system representative and actual rehabilitation | 9.4 (7.0–12.2) | 11.7 (9.3–14.4) | 0.21 |
| 1.2.5. | Other | 0.2 (0.01–1.1) | 0.2 (0.01–0.9) | 1.00 |
| Evaluation of postsurgical rehabilitation process at the place of residence | ||||
| 1.3.1. | Entirely satisfied | 71.5 (67.4–75.3) | 71.8 (68.2–75.2) | 0.91 |
| 1.3.2. | Overall, the evaluation of rehabilitation process is positive; however, it needs improvement | 8.2 (6.0–10.9) | 8.6 (6.6–11.0) | 0.81 |
| 1.3.3. | Absolutely dissatisfied | 19.1 (15.8–22.7) | 18.6 (15.7–21.8) | 0.83 |
| 1.3.4. | Evaluation is impossible (choosing 1.2.4) | 1.1 (0.4–2.4) | 0.9 (0.3–2.0) | 0.73 |
| No. | Survey Results | THR Patients (n = 78) | TKR Patients (n = 99) | p-Value |
|---|---|---|---|---|
| 1.3.3.1. | Absence of a local orthopedic surgeon | 21.8 (13.2–32.6) | 30.3 (21.5–40.4) | 0.21 |
| 1.3.3.2. | Lack of time for visiting a local orthopedic surgeon | 10.3 (4.6–19.3) | 10.1 (5.0–17.8) | 0.97 |
| 1.3.3.3. | Poor healthcare quality (no result after visiting a local orthopedic surgeon) | 26.9 (17.5–38.1) | 30.3 (21.5–40.4) | 0.62 |
| 1.3.3.4. | Other | 41.0 (30.0–52.7) | 29.3 (20.6–39.3) | 0.11 |
| No. | Survey Results | THR Patients (n = 523) | TKR Patients (n = 650) | p-Value |
|---|---|---|---|---|
| Chronic pain evaluation | ||||
| 2.1.1.1. | No pain | 56.4 (52.0–60.7) | 47.0 (43.1–50.9) | <0.01 |
| 2.1.1.2. | Mild, annoying pain | 25.1 (21.4–29.1) | 26.2 ( 22.9–29.8) | 0.67 |
| 2.1.1.3. | Nagging, uncomfortable pain | 14.2 (11.3–17.5) | 20.7 (17.7–24.0) | <0.01 |
| 2.1.1.4. | Distressing, miserable pain | 3.1 (1.8–5.0) | 4.0 ( 2.6–5.8) | 0.41 |
| 2.1.1.5. | Intense, horrible pain | 0.8 (0.2–2.0) | 1.5 (0.7–2.8) | 0.27 |
| 2.1.1.6. | Worst possible, unbearable pain | 0.4 (0.1–1.4) | 0.6 (0.2–1.6) | 0.63 |
| Evaluation of physical activity, limb function and anatomic changes | ||||
| Ability to walk | ||||
| 2.2.1.1. | Unable to walk | 2.1 (1.1–3.7) | 3.8 (2.5–5.6) | 0.09 |
| 2.2.1.2. | Able to walk with extra support (cane, crutches) | 40.5 (36.3–44.9) | 44.0 (40.1–47.9) | 0.23 |
| 2.2.1.3. | Able to walk independently | 57.4 (53.0–61.7) | 52.2 (48.3–56.1) | 0.08 |
| Range of walking without rest | ||||
| 2.2.2.1. | Able to move inside the house | 14.5 (11.6–17.8) | 19.8 (16.8–23.1) | 0.02 |
| 2.2.2.2. | Able to reach nearby facilities | 29.6 (25.7–33.7) | 31.5 (27.9–35.2) | 0.48 |
| 2.2.2.3. | Able to walk several blocks | 31.2 (27.3–35.4) | 27.5 (24.1–31.1) | 0.17 |
| 2.2.2.4. | Able to walk unassisted within the residential district | 24.7 (21.1–28.6) | 21.2 (18.1–24.6) | 0.16 |
| Anatomical and functional changes of the limb | ||||
| 2.2.3.1. | Joint excursion (motion range) is restricted | 26.0 (22.3–30.0) | 31.1 (27.6–34.8) | 0.06 |
| 2.3.1.1. | No difference in limb lengths | 72.9 (68.9–76.7) | 78.2 (74.8–81.3) | 0.04 |
| 2.3.2.1. | No limb deformations | 93.9 (91.5–95.8) | 91.7 (89.3–93.7) | 0.15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fedonnikov, A.S.; Andriyanova, E.A.; Kiselev, A.R.; Norkin, I.A. Rehabilitation Process Issues and Functional Performance after Total Hip and Knee Replacement. Healthcare 2021, 9, 1126. https://doi.org/10.3390/healthcare9091126
Fedonnikov AS, Andriyanova EA, Kiselev AR, Norkin IA. Rehabilitation Process Issues and Functional Performance after Total Hip and Knee Replacement. Healthcare. 2021; 9(9):1126. https://doi.org/10.3390/healthcare9091126
Chicago/Turabian StyleFedonnikov, Alexander S., Elena A. Andriyanova, Anton R. Kiselev, and Igor A. Norkin. 2021. "Rehabilitation Process Issues and Functional Performance after Total Hip and Knee Replacement" Healthcare 9, no. 9: 1126. https://doi.org/10.3390/healthcare9091126
APA StyleFedonnikov, A. S., Andriyanova, E. A., Kiselev, A. R., & Norkin, I. A. (2021). Rehabilitation Process Issues and Functional Performance after Total Hip and Knee Replacement. Healthcare, 9(9), 1126. https://doi.org/10.3390/healthcare9091126







