Understanding the Role of External Facilitation to Drive Quality Improvement for Stroke Care in Hospitals
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population
2.3. QI Intervention Description
2.4. Data Collection
2.5. Clinical Indicator Data to Assess Quality Improvement Effects
2.6. Calculation of Composite Score
2.7. Data Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vestergaard, A.S.; Ehlers, L.H. A Health Economic Evaluation of Stroke Prevention in Atrial Fibrillation: Guideline Adherence versus the Observed Treatment Strategy Prior to 2012 in Denmark. Pharmacoeconomics 2015, 33, 967–979. [Google Scholar] [CrossRef]
- Brien, E.C.; Wu, J.; Zhao, X.; Schulte, P.J.; Fonarow, G.C.; Hernandez, A.F.; Schwamm, L.H.; Peterson, E.D.; Bhatt, D.L.; Smith, E.E.; et al. Healthcare Resource Availability, Quality of Care, and Acute Ischemic Stroke Outcomes. J. Am. Heart Assoc. 2017, 6, e003813. [Google Scholar] [CrossRef] [Green Version]
- Cadilhac, D.A.; Lannin, N.A.; Anderson, C.S.; Kim, J.; Andrew, N.; Kilkenny, M.; Shehata, S.; Grabsch, B.; Levi, C.; Faux, S.; et al. The Australian Stroke Clinical Registry Annual Report 2015; The Florey Institute of Neuroscience and Mental Health, 2016; Report No 7, pages 42. [Google Scholar]
- Grimshaw, J.M.; Eccles, M.P.; Walker, A.E.; Thomas, R.E. Changing physicians’ behavior: What works and thoughts on getting more things to work. J. Contin. Educ. Health Prof. 2002, 22, 237–243. [Google Scholar] [CrossRef]
- Forsner, T.; Hansson, J.; Brommels, M.; Wistedt, A.Å.; Forsell, Y. Implementing clinical guidelines in psychiatry: A qualitative study of perceived facilitators and barriers. BMC Psychiatry 2010, 10, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Cadilhac, D.A.; Carter, R.C.; Thrift, A.G.; Dewey, H.M. Why invest in a national public health program for stroke?: An example using Australian data to estimate the potential benefits and cost implications. Health Policy 2007, 83, 287–294. [Google Scholar] [CrossRef]
- Grimshaw, J.M.; Eccles, M.P.; Lavis, J.N.; Hill, S.J.; Squires, J.E. Knowledge translation of research findings. Implement. Sci. 2012, 7, 1–17. [Google Scholar] [CrossRef]
- Cochrane Effective Practice and Organization of Care Group. Data Collection Checklist. 2002. Available online: http://www.epoc.cochrane.org/ (accessed on 25 April 2016).
- Grimshaw, J.; Eccles, M.; Tetroe, J. Implementing clinical guidelines: Current evidence and future implications. J. Contin. Educ. Health Prof. 2004, 24, S31–S37. [Google Scholar] [CrossRef] [PubMed]
- Squires, J.E.; Sullivan, K.; Eccles, M.P.; Worswick, J.; Grimshaw, J.M. Are multifaceted interventions more effective than single-component interventions in changing health-care professionals’ behaviours? An overview of systematic reviews. Implement. Sci. 2014, 9, 152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitson, A.L.; Rycroft-Malone, J.; Harvey, G.; McCormack, B.; Seers, K.; Titchen, A. Evaluating the successful implementation of evidence into practice using the PARiHS framework: Theoretical and practical challenges. Implement. Sci. 2008, 3, 1. [Google Scholar] [CrossRef]
- Gozdzik, A. Applying the PARiHS framework in a knowledge dissemination initiative. CANNT J. J. ACITN 2013 2013, 3, 48–50. [Google Scholar]
- Stetler, C.B.; Legro, M.W.; Rycroft-Malone, J.; Bowman, C.; Curran, G.; Guihan, M.; Hagedorn, H.; Pineros, S.; Wallace, C.M. Role of “external facilitation” in implementation of research findings: A qualitative evaluation of facilitation experiences in the Veterans Health Administration. Implement. Sci. 2006, 1, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Bornbaum, C.C.; Kornas, K.; Peirson, L.; Rosella, L.C. Exploring the function and effectiveness of knowledge brokers as facilitators of knowledge translation in health-related settings: A systematic review and thematic analysis. Implement. Sci. 2015, 10, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cadilhac, D.A.; Grimley, R.; Kilkenny, M.F.; Andrew, N.E.; Lannin, N.A.; Hill, K.; Grabsch, B.; Levi, C.R.; Thrift, A.G.; Faux, S.G.; et al. Multicenter, Prospective, Controlled, Before-and-After, Quality Improvement Study (Stroke123) of Acute Stroke Care. Stroke 2019, 50, 1525–1530. [Google Scholar] [CrossRef] [PubMed]
- Cadilhac, D.A.; Andrew, N.E.; Kilkenny, M.F.; Hill, K.; Grabsch, B.; Lannin, N.A.; Thrift, A.G.; Anderson, C.S.; Donnan, G.A.; Middleton, S.; et al. Improving quality and outcomes of stroke care in hospitals: Protocol and statistical analysis plan for the Stroke123 implementation study. Int. J. Stroke 2018, 13, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Andrew, N.E.; Middleton, S.; Grimley, R.; Anderson, C.S.; Donnan, G.A.; Lannin, N.A.; Stroil-Salama, E.; Grabsch, B.; Kilkenny, M.F.; Squires, J.E.; et al. Hospital organizational context and delivery of evidence-based stroke care: A cross-sectional study. Implement. Sci. 2019, 14, 6. [Google Scholar] [CrossRef] [Green Version]
- Speroff, T.; O’Connor, G.T. Study Designs for PDSA Quality Improvement Research. Qual. Manag. Healthc. 2004, 13, 17–32. [Google Scholar] [CrossRef] [Green Version]
- Donnelly, P.; Kirk, P. Use the PDSA model for effective change management. Educ. Prim. Care 2015, 26, 279–281. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Academic Press: New York, NY, USA, 1988. [Google Scholar]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. Br. Med. J. 2014, 348, g1687. [Google Scholar] [CrossRef] [Green Version]
- Bidassie, B.; Williams, L.S.; Woodward-Hagg, H.; Matthias, M.S.; Damush, T.M. Key components of external facilitation in an acute stroke quality improvement collaborative in the Veterans Health Administration. Implement. Sci. 2015, 10, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Schwamm, L.H.; Fonarow, G.C.; Reeves, M.J.; Pan, W.; Frankel, M.R.; Smith, E.E.; Ellrodt, G.; Cannon, C.P.; Liang, L.; Peterson, E.; et al. Get With the Guidelines–Stroke Is Associated With Sustained Improvement in Care for Patients Hospitalized With Acute Stroke or Transient Ischemic Attack. Circulation 2009, 119, 107–115. [Google Scholar] [CrossRef] [Green Version]
- Cadilhac, D.A.; Andrew, N.E.; Stroil Salama, E.; Hill, K.; Middleton, S.; Horton, E.; Meade, I.; Kuhle, S.; Nelson, M.R.; Grimley, R.; et al. Improving discharge care: The potential of a new organisational intervention to improve discharge after hospitalisation for acute stroke, a controlled before–after pilot study. BMJ Open 2017, 7, e016010. [Google Scholar] [CrossRef] [PubMed]



| Type of Information |
|---|
| Number of contacts the external facilitators had with the relevant clinicians and hospital staff |
| Mode of contact (e.g., telephone, face-to-face, email) |
| Contact time in minutes for telephone and face-to-face contacts |
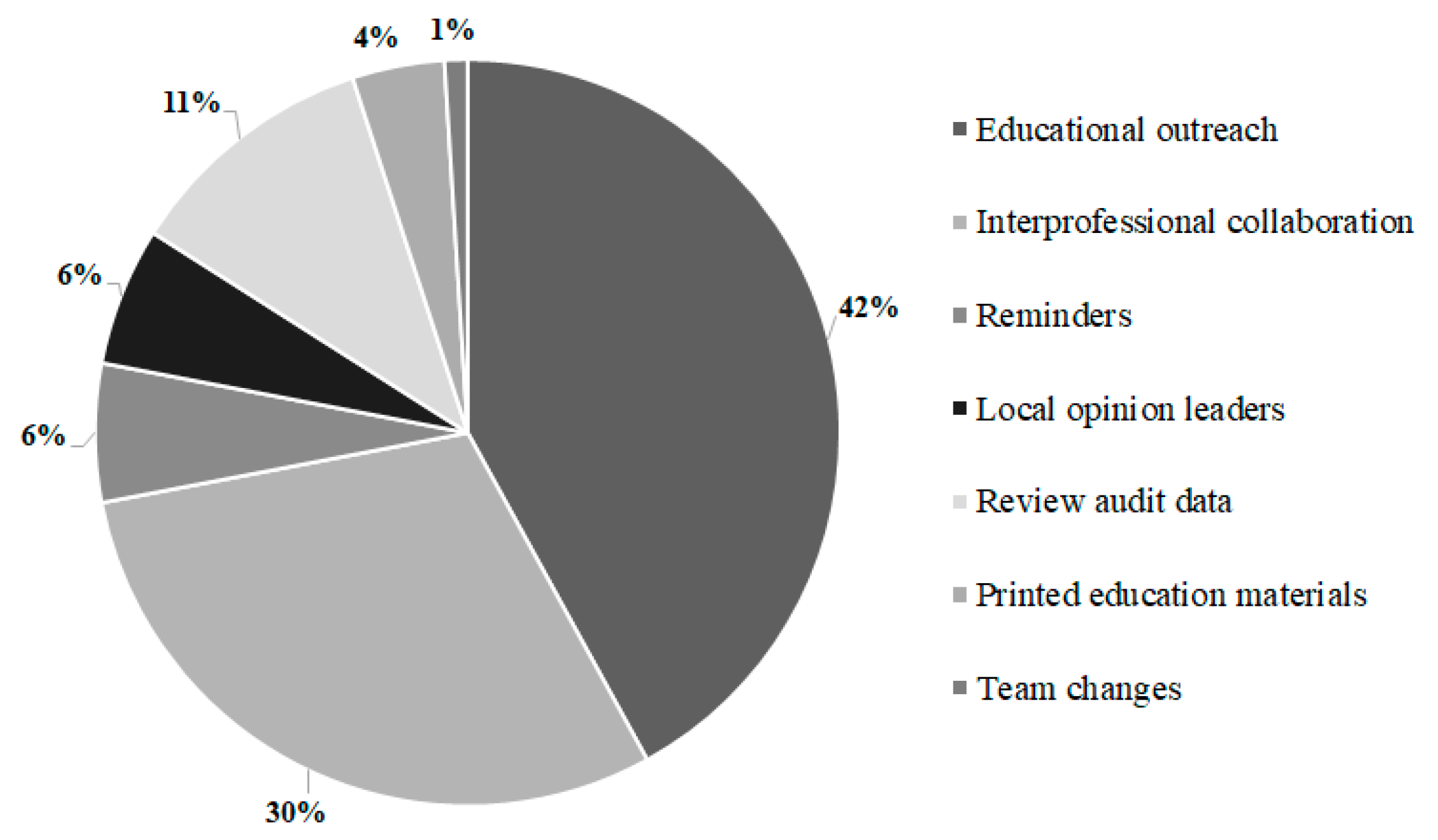
| Professional behavior change support type provided (e.g., reminders, educational outreach) * |
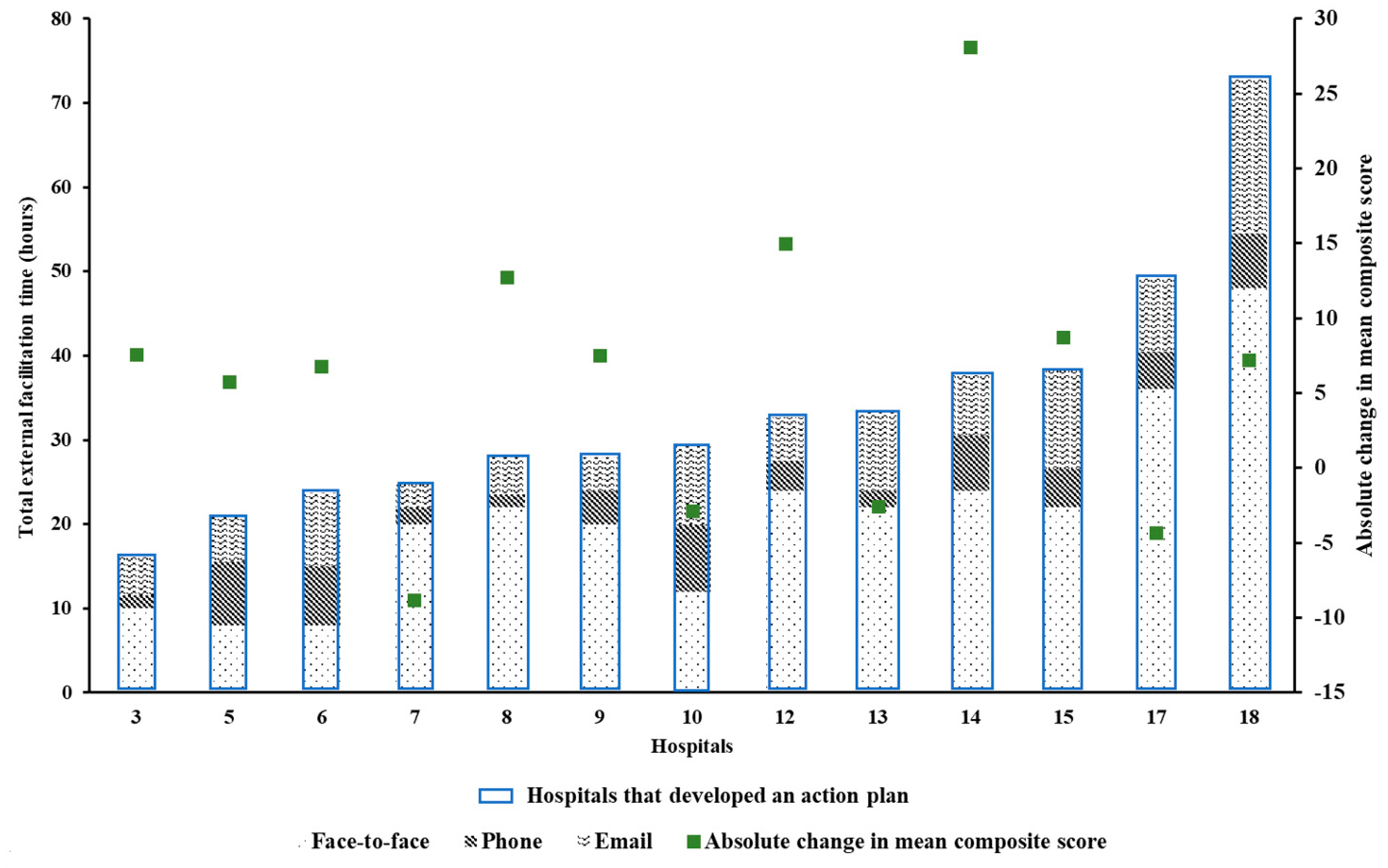
| Action plan initiated by staff at participating hospitals (Yes/No) |
| Hospitals accessing their AuSCR data (by downloading online live reports)—Yes or No |
| Mode of Contact | Measure | All Hospitals N = 19 | Hospitals that Developed an Action Plan N = 14 | Hospitals That Did Not Develop an Action Plan N = 5 | p Value | Hedge’s g |
|---|---|---|---|---|---|---|
| Face-to-face | Median (Q1, Q3) | 20 (10, 24) | 21 (10, 24) | 10 (10, 12) | 0.243 | N/A |
| Mean (± SD) | 19 (11) | 20 (11) | 14 (10) | 0.300 | 0.557 | |
| Telephone | Median (Q1, Q3) | 5 (3, 7) | 5 (3, 7) | 3 (3, 6) | 0.676 | N/A |
| Mean (± SD) | 5 (2) | 5 (2) | 4 (3) | 0.411 | 0.440 | |
| Median (Q1, Q3) | 6 (4, 9) | 7 (4, 9) | 5 (5, 8) | 0.817 | N/A | |
| Mean (± SD) | 7 (4) | 7 (4) | 7 (3) | 0.859 | 0 | |
| Total | Median (Q1, Q3) | 22 (15, 29) | 29 (24, 38) | 20 (16, 31) | 0.308 | N/A |
| Mean (± SD) | 30 (14) | 32 (15) | 25 (10) | 0.350 | 0.501 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thayabaranathan, T.; Andrew, N.E.; Grimley, R.; Stroil-Salama, E.; Grabsch, B.; Hill, K.; Cadigan, G.; Purvis, T.; Middleton, S.; Kilkenny, M.F.; et al. Understanding the Role of External Facilitation to Drive Quality Improvement for Stroke Care in Hospitals. Healthcare 2021, 9, 1095. https://doi.org/10.3390/healthcare9091095
Thayabaranathan T, Andrew NE, Grimley R, Stroil-Salama E, Grabsch B, Hill K, Cadigan G, Purvis T, Middleton S, Kilkenny MF, et al. Understanding the Role of External Facilitation to Drive Quality Improvement for Stroke Care in Hospitals. Healthcare. 2021; 9(9):1095. https://doi.org/10.3390/healthcare9091095
Chicago/Turabian StyleThayabaranathan, Tharshanah, Nadine E. Andrew, Rohan Grimley, Enna Stroil-Salama, Brenda Grabsch, Kelvin Hill, Greg Cadigan, Tara Purvis, Sandy Middleton, Monique F. Kilkenny, and et al. 2021. "Understanding the Role of External Facilitation to Drive Quality Improvement for Stroke Care in Hospitals" Healthcare 9, no. 9: 1095. https://doi.org/10.3390/healthcare9091095
APA StyleThayabaranathan, T., Andrew, N. E., Grimley, R., Stroil-Salama, E., Grabsch, B., Hill, K., Cadigan, G., Purvis, T., Middleton, S., Kilkenny, M. F., Cadilhac, D. A., & on behalf of the Stroke123 Investigators and AuSCR Consortium. (2021). Understanding the Role of External Facilitation to Drive Quality Improvement for Stroke Care in Hospitals. Healthcare, 9(9), 1095. https://doi.org/10.3390/healthcare9091095








