Health Issues Due to the Global Prevalence of Sedentariness and Recommendations towards Achieving a Healthier Behaviour
Abstract
1. Introduction
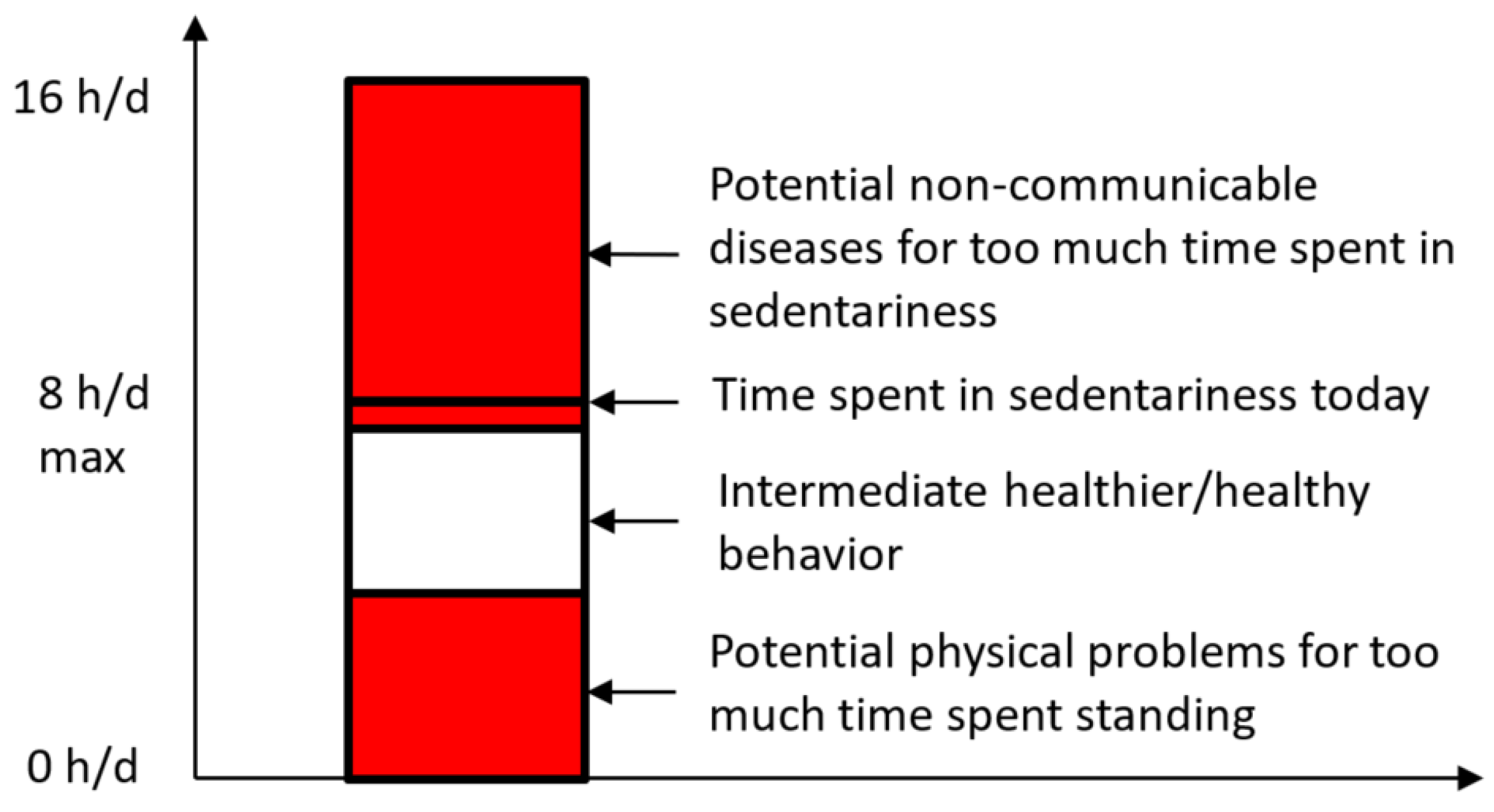
2. Sedentariness as a Subconscious, Dangerous, Non-Communicable Disease
3. Recommendations for Public Health Implications
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andersen, L.B.; Mota, J.; Di Pietro, L. Update on the global pandemic of physical inactivity. Lancet 2016, 388, 1255–1256. [Google Scholar] [CrossRef]
- Sallis, J.F.; Haskell, W.L.; Wood, P.D.; Fortmann, S.P.; Rogers, T.; Blair, S.N.; Paffenbarger, R.S., Jr. Physical activity assessment methodology in the Five-City Project. Am. J. Epidemiol. 1985, 121, 91–106. [Google Scholar] [CrossRef] [PubMed]
- Sujatha, T.; Shatrugna, V.; Venkataramana, Y.; Begum, N. Energy expenditure on household, childcare and occupational activities of women from urban poor households. Br. J. Nutr. 2000, 83, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; Olds, T.; Tremblay, M.S. Public health guidelines on sedentary behaviour are important and needed: A provisional benchmark is better than no benchmark at all. Br. J. Sports Med. 2020, 54, 308–309. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, E.; Ekelund, U.; Ding, D.; Hamer, M.; Bauman, A.E.; Lee, I.-M. Is the time right for quantitative public health guidelines on sitting? A narrative review of sedentary behaviour research paradigms and findings. Br. J. Sports Med. 2019, 53, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.A. Sick of sitting. Diabetologia 2015, 58, 1751–1758. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M.; on behalf of SBRN Terminology Consensus Project Participants. Sedentary Behavior Research Network (SBRN)–Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.W.; Popkin, B. Time Use and Physical Activity: A Shift Away from Movement across the Globe. Obes. Rev. 2012, 13, 659–680. [Google Scholar] [CrossRef] [PubMed]
- Belzunegui-Eraso, A.; Erro-Garcés, A. Teleworking in the Context of the COVID-19 Crisis. Sustainability 2020, 12, 3662. [Google Scholar] [CrossRef]
- Coenen, P.; Parry, S.; Willenberg, L.; Shi, J.W.; Romero, L.; Blackwood, D.M.; Healy, G.N.; Dunstan, D.W.; Straker, L.M. Associations of prolonged standing with musculoskeletal symptoms—A systematic review of laboratory studies. Gait Posture 2017, 58, 310–318. [Google Scholar] [CrossRef]
- Baker, R.; Coenen, P.; Howie, E.; Lee, J.; Williamson, A.; Straker, L. A detailed description of the short-term musculoskeletal and cognitive effects of prolonged standing for office computer work. Ergonomics 2018, 61, 877–890. [Google Scholar] [CrossRef] [PubMed]
- Bergouignan, A.; Legget, K.T.; De Jong, N.; Kealey, E.; Nikolovski, J.; Groppel, J.L.; Jordan, C.; O’Day, R.; Hill, J.O.; Bessesen, D.H. Effect of frequent interruptions of prolonged sitting on self-perceived levels of energy, mood, food cravings and cognitive function. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 113. [Google Scholar] [CrossRef] [PubMed]
- Raichlen, D.A.; Pontzer, H.; Zderic, T.W.; Harris, J.A.; Mabulla, A.Z.P.; Hamilton, M.T.; Wood, B.M. Sitting, squatting, and the evolutionary biology of human inactivity. Proc. Natl. Acad. Sci. USA 2020, 117, 7115–7121. [Google Scholar] [CrossRef]
- Smith, L.; Hamer, M.; Ucci, M.; Marmot, A.; Gardner, B.; Sawyer, A.; Wardle, J.; Fisher, A. Weekday and weekend patterns of objectively measured sitting, standing, and stepping in a sample of office-based workers: The active buildings study. BMC Public Health 2015, 15, 9. [Google Scholar] [CrossRef] [PubMed]
- Hadgraft, N.T.; Healy, G.N.; Owen, N.; Winkler, E.A.H.; Lynch, B.M.; Sethi, P.; Eakin, E.G.; Moodie, M.; LaMontagne, A.D.; Wiesner, G.; et al. Office workers’ objectively assessed total and prolonged sitting time: Individual-level correlates and worksite variations. Prev. Med. Rep. 2016, 4, 184–191. [Google Scholar] [CrossRef]
- Owen, N.; Healy, G.N.; Dempsey, P.C.; Salmon, J.; Timperio, A.; Clark, B.K.; Goode, A.D.; Koorts, H.; Ridgers, N.D.; Hadgraft, N.T.; et al. Sedentary Behavior and Public Health: Integrating the Evidence and Identifying Potential Solutions. Annu. Rev. Public Health 2020, 41, 265–287. [Google Scholar] [CrossRef]
- Wang, X.; Li, Y.; Fan, H. The associations between screen time-based sedentary behavior and depression: A systematic review and meta-analysis. BMC Public Health 2019, 19, 1524. [Google Scholar] [CrossRef] [PubMed]
- Carson, V.; Wong, S.L.; Winkler, E.; Healy, G.N.; Colley, R.C.; Tremblay, M.S. Patterns of sedentary time and cardiometabolic risk among Canadian adults. Prev. Med. 2014, 65, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Gibson, A.-M.; Muggeridge, D.J.; Hughes, A.R.; Kelly, L.; Kirk, A. An examination of objectively-measured sedentary behavior and mental well-being in adults across week days and weekends. PLoS ONE 2017, 12, e0185143. [Google Scholar] [CrossRef]
- Hamer, M.; Coombs, N.; Stamatakis, E. Associations between objectively assessed and self-reported sedentary time with mental health in adults: An analysis of data from the Health Survey for England. BMJ Open 2014, 4, e004580. [Google Scholar] [CrossRef] [PubMed]
- Healy, G.N.; Matthews, C.E.; Dunstan, D.W.; Winkler, E.A.H.; Owen, N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-06. Eur. Heart J. 2011, 32, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Loyen, A.; Clarke-Cornwell, A.M.; Anderssen, S.A.; Hagströmer, M.; Sardinha, L.B.; Sundquist, K.; Ekelund, U.; Steene-Johannessen, J.; Baptista, F.; Hansen, B.H.; et al. Sedentary Time and Physical Activity Surveillance Through Accelerometer Pooling in Four European Countries. Sports Med. 2017, 47, 1421–1435. [Google Scholar] [CrossRef] [PubMed]
- Matthews, C.E.; Chen, K.Y.; Freedson, P.S.; Buchowski, M.S.; Beech, B.M.; Pate, R.R.; Troiano, R.P. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am. J. Epidemiol. 2008, 167, 875–881. [Google Scholar] [CrossRef]
- Vallance, J.K.; Winkler, E.A.H.; Gardiner, P.A.; Healy, G.N.; Lynch, B.M.; Owen, N. Associations of objectively-assessed physical activity and sedentary time with depression: NHANES (2005–2006). Prev. Med. 2011, 53, 284–288. [Google Scholar] [CrossRef]
- Alomari, M.A.; Khabour, O.F.; Alzoubi, K.H. Changes in Physical Activity and Sedentary Behavior Amid Confinement: The BKSQ-COVID-19 Project. Risk Manag. Healthc. Policy 2020, 13, 1757–1764. [Google Scholar] [CrossRef]
- Gupta, N.; Hallman, D.M.; Mathiassen, S.E.; Aadahl, M.; Jørgensen, M.B.; Holtermann, A. Are temporal patterns of sitting associated with obesity among blue-collar workers? A cross sectional study using accelerometers. BMC Public Health 2016, 16, 148. [Google Scholar] [CrossRef] [PubMed]
- Parry, S.; Straker, L. The contribution of office work to sedentary behaviour associated risk. BMC Public Health 2013, 13, 296. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.-M.; Lancet Physical Activity Series 2 Executive Committe; Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef]
- Magnon, V.; Vallet, G.T.; Auxiette, C. Sedentary Behavior at Work and Cognitive Functioning: A Systematic Review. Front. Public Health 2018, 6, 239. [Google Scholar] [CrossRef]
- Paterson, C.; Fryer, S.; Zieff, G.; Stone, K.; Credeur, D.P.; Gibbs, B.B.; Padilla, J.; Parker, J.K.; Stoner, L. The Effects of Acute Exposure to Prolonged Sitting, With and Without Interruption, on Vascular Function Among Adults: A Meta-analysis. Sports Med. 2020, 50, 1929–1942. [Google Scholar] [CrossRef] [PubMed]
- Stanczykiewicz, B.; Banik, A.; Knoll, N.; Keller, J.; Hohl, D.H.; Rosińczuk, J.; Luszczynska, A. Sedentary behaviors and anxiety among children, adolescents and adults: A systematic review and meta-analysis. BMC Public Health 2019, 19, 459. [Google Scholar] [CrossRef] [PubMed]
- Pruimboom, L. Physical inactivity is a disease synonymous for a non-permissive brain disorder. Med. Hypotheses 2011, 77, 708–713. [Google Scholar] [CrossRef] [PubMed]
- Kar, G.; Hedge, A. Effects of Sitting and Standing Work Postures on Short-Term Typing Performance and Discomfort. SAGE J. 2016, 60, 460–464. [Google Scholar] [CrossRef]
- Loh, R.; Stamatakis, E.; Folkerts, D.; Allgrove, J.E.; Moir, H.J. Effects of Interrupting Prolonged Sitting with Physical Activity Breaks on Blood Glucose, Insulin and Triacylglycerol Measures: A Systematic Review and Meta-analysis. Sports Med. 2020, 50, 295–330. [Google Scholar] [CrossRef]
- Levine, J.A. Health-chair reform: Your chair: Comfortable but deadly. Diabetes 2010, 59, 2715–2716. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Boerema, S.T.; van Velsen, L.; Vollenbroek, M.M.; Hermens, H.J. Pattern measures of sedentary behaviour in adults: A literature review. Digit. Health 2020, 6. [Google Scholar] [CrossRef] [PubMed]
- Gardner, B.; Smith, L.; Lorencatto, F.; Hamer, M.; Biddle, S.J.H. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol. Rev. 2016, 10, 89–112. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Chau, J.Y.; Grunseit, A.C.; Chey, T.; Stamatakis, E.; Brown, W.J.; Matthews, C.E.; Bauman, A.E.; van der Ploeg, H.P. Daily Sitting Time and All-Cause Mortality: A Meta-Analysis. PLoS ONE 2013, 8, e80000. [Google Scholar] [CrossRef]
- Dunstan, D.W.; Howard, B.; Healy, G.N.; Owen, N. Too much sitting—A health hazard. Diabetes Res. Clin. Pract. 2012, 97, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Pitanga, F.J.G.; Beck, C.C.; Pitanga, C.P.S.; Pitanga, F.J.G.; Beck, C.C.; Pitanga, C.P.S. Physical Activity and Reducing Sedentary Behavior during The Coronavirus Pandemic. Arq. Bras. Cardiol. 2020, 114, 1058–1060. [Google Scholar] [CrossRef]
- Rangul, V.; Sund, E.R.; Mork, P.J.; Røe, O.D.; Bauman, A. The associations of sitting time and physical activity on total and site-specific cancer incidence: Results from the HUNT study, Norway. PLoS ONE 2018, 13, e0206015. [Google Scholar] [CrossRef] [PubMed]
- Patterson, R.; McNamara, E.; Tainio, M.; de Sá, T.H.; Smith, A.D.; Sharp, S.J.; Edwards, P.; Woodcock, J.; Brage, S.; Wijndaele, K. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: A systematic review and dose response meta-analysis. Eur. J. Epidemiol. 2018, 33, 811–829. [Google Scholar] [CrossRef]
- Chastin, S.F.M.; Dontje, M.L.; Skelton, D.A.; Čukić, I.; Shaw, R.J.; Gill, J.M.R.; Greig, C.A.; Gale, C.R.; Deary, I.J.; Der, G.; et al. Systematic comparative validation of self-report measures of sedentary time against an objective measure of postural sitting (activPAL). Int. J. Behav. Nutr. Phys. Act. 2018, 15, 21. [Google Scholar] [CrossRef]
- Sanders, J.P.; Loveday, A.; Pearson, N.; Edwardson, C.; Yates, T.; Biddle, S.J.H.; Esliger, D.W. Devices for Self-Monitoring Sedentary Time or Physical Activity: A Scoping Review. J. Med. Internet Res. 2016, 18, e90. [Google Scholar] [CrossRef] [PubMed]
- Beckwith, C. Utilizing Wearable Activity Trackers in the Intervention of Sedentary Lifestyles. In Proceedings of the Academic Festival 2021, Fairfield, CT, USA, 5 May 2021; Available online: https://digitalcommons.sacredheart.edu/acadfest/2021/all/15 (accessed on 3 August 2021).
- Aldenaini, N.; Alqahtani, F.; Orji, R.; Sampalli, S. Trends in Persuasive Technologies for Physical Activity and Sedentary Behavior: A Systematic Review. Front. Artif. Intell. 2020, 3, 7. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; König, L.M.; Reiterer, H. A Smartphone App to Support Sedentary Behavior Change by Visualizing Personal Mobility Patterns and Action Planning (SedVis): Development and Pilot Study. JMIR Form. Res. 2021, 5, e15369. [Google Scholar] [CrossRef]
- Gill, J.M.R.; Hawari, N.S.A.; Maxwell, D.J.; Louden, D.; Mourselas, N.; Bunn, C.; Gray, C.M.; van der Ploeg, H.P.; Hunt, K.; Martin, A.; et al. Validation of a Novel Device to Measure and Provide Feedback on Sedentary Behavior. Med. Sci. Sports Exerc. 2018, 50, 525–532. [Google Scholar] [CrossRef]
- Karakolis, T.; Callaghan, J.P. The impact of sit-stand office workstations on worker discomfort and productivity: A review. Appl. Ergon. 2014, 45, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, D.; Mama, Y.; Algom, D. Stand by Your Stroop: Standing Up Enhances Selective Attention and Cognitive Control. Psychol. Sci. 2017, 28, 1864–1867. [Google Scholar] [CrossRef]
- Smith, K.C.; Davoli, C.C.; Knapp, W.H.; Abrams, R.A. Standing enhances cognitive control and alters visual search. Atten. Percept. Psychophys. 2019, 81, 2320–2329. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.; Mallick, K.; Monforte, J.; Foster, C. Disability, the communication of physical activity and sedentary behaviour, and ableism: A call for inclusive messages. Br. J. Sports Med. 2021. [Google Scholar] [CrossRef]
- Landais, L.L.; Damman, O.C.; Schoonmade, L.J.; Timmermans, D.R.M.; Verhagen, E.A.L.M.; Jelsma, J.G.M. Choice architecture interventions to change physical activity and sedentary behavior: A systematic review of effects on intention, behavior and health outcomes during and after intervention. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 47. [Google Scholar] [CrossRef]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Venema, T.A.G.; Kroese, F.M.; De Ridder, D.T.D. I’m still standing: A longitudinal study on the effect of a default nudge. Psychol. Health 2018, 33, 669–681. [Google Scholar] [CrossRef]
- Finch, L.E.; Tomiyama, A.J.; Ward, A. Taking a Stand: The Effects of Standing Desks on Task Performance and Engagement. Int. J. Environ. Res. Public Health 2017, 14, 939. [Google Scholar] [CrossRef]
- Habib, S.H.; Saha, S. Burden of non-communicable disease: Global overview. Diabetes Metab. Syndr. Clin. Res. Rev. 2010, 4, 41–47. [Google Scholar] [CrossRef]
| Study | Objective Time Spent per Day in Sedentariness | Countries in Which the Study Was Performed |
|---|---|---|
| Smith et al. (2015) | 10.6 h/d | England |
| Hamer, Coombs and Stamatakis (2014) | 9.64 h/d | England |
| Loyen et al. (2017) | 8.83 h/d | England, Norway, Portugal, and Sweden |
| Gibson, Muggeridge, Hughes, Kelly and Kirk (2017) | 9.5 h/d | Scotland |
| Vallance et al. (2011) | 8.5 h/d 1 | Canada |
| Carson et al. (2014) | 10.8 h/d | Canada |
| Healy, Matthews, Dunstan, Winkler and Owen (2011) | 8.44 h/d | United States of America |
| Matthews et al. (2008) | 8.53 h/d | United States of America |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bonnet, C.T.; Barela, J.A. Health Issues Due to the Global Prevalence of Sedentariness and Recommendations towards Achieving a Healthier Behaviour. Healthcare 2021, 9, 995. https://doi.org/10.3390/healthcare9080995
Bonnet CT, Barela JA. Health Issues Due to the Global Prevalence of Sedentariness and Recommendations towards Achieving a Healthier Behaviour. Healthcare. 2021; 9(8):995. https://doi.org/10.3390/healthcare9080995
Chicago/Turabian StyleBonnet, Cédrick T., and Jose A. Barela. 2021. "Health Issues Due to the Global Prevalence of Sedentariness and Recommendations towards Achieving a Healthier Behaviour" Healthcare 9, no. 8: 995. https://doi.org/10.3390/healthcare9080995
APA StyleBonnet, C. T., & Barela, J. A. (2021). Health Issues Due to the Global Prevalence of Sedentariness and Recommendations towards Achieving a Healthier Behaviour. Healthcare, 9(8), 995. https://doi.org/10.3390/healthcare9080995






